Abstract
Living in disorganized neighborhoods characterized by high levels of poverty, crime, violence, and deteriorating buildings has been associated with increased alcohol consumption and mental health problems. Data drawn from the Seattle Social Development Project (N=790), a theory-driven longitudinal study originating in Seattle, WA, were used to estimate trajectories of Alcohol Use Disorder (AUD) symptoms from age 21 to 39. Time-varying measures of neighborhood disorganization, psychological distress, and sociodemographic factors were associated with deviations from average AUD symptoms at each wave. Results indicated that, on average, AUD symptoms decreased as individuals got older. Living in more disorganized neighborhoods and experiencing psychological distress was associated with increased AUD symptoms after accounting for average reductions from AUD symptoms over time and time-varying measures of relevant sociodemographic factors. Results of mediation analysis suggested that psychological distress is a mechanism by which disorganized neighborhoods increased risk of AUD from age 21 to 39.
Keywords: neighborhood disorganization, alcohol use disorder, psychological distress, latent growth curve
Problem Drinking and Mental Health Problems
Excessive alcohol use has been closely linked to a range of health issues including mental health problems such as anxiety, depression, violence and sexual assault, motor vehicle crashes, and multiple physical health problems including heart disease, cancer, and stroke (Centers for Disease Control and Prevention, 2016; Gutjahr, Gmel, & Rehm, 2001). Approximately 88,000 annual deaths in America are attributed to alcohol-related causes and economic estimates of the alcohol-related costs of health care, mortality, and reduced worker productively reached $249 billion for 2010 (National Insitute on Alcohol Abuse and Alcoholism, 2016; Sacks, Gonzales, Bouchery, Tomedi, & Brewer, 2015). Research suggests causal relationships between heavy alcohol consumption and at least 60 different diseases (Connor, Haber, & Hall, 2016).
The term Alcohol Use Disorder (AUD) is used to collectively describe diagnoses of either alcohol abuse or dependence as defined by the Diagnostic and Statistical Manual of Mental Disorders (4th Edition)(DSM-IV, American Psychological Association, 1994). For 2013, epidemiological studies estimated that 7 to 13 percent of adults age 18 and older meet diagnostic criteria for AUD in the past year (Grant et al., 2015; Substance Abuse and Mental Health Services Administration, 2014). Over a lifetime, approximately 29 percent of adults in the United States are estimated to experience AUD, yet many never receive treatment for AUD (Connor et al., 2016; Grant et al., 2015). Epidemiological surveillance has consistently shown higher rates of AUD for males and decreases in prevalence of AUD with age (Delker, Brown, & Hasin, 2016; Grant et al., 2004a; Grant et al., 2015). Peak prevalence of AUD occurs between ages 18 and 25 with recent rates of 15–18% in the United States (Hedden, 2015; Rehm et al., 2014). Binge drinking among young adults is viewed by many researchers as a normative behavior peaking in the early 20s (Schulenberg, O’Malley, Bachman, Wadsworth, & Johnston, 1996) that tends to wane as individuals grow older and take on more significant adult roles in work and family life (Connor et al., 2016). Young adults who develop mild alcohol problems often later reduce drinking below problem levels when they transition to adult roles (Connor et al., 2016).
Epidemiological and longitudinal studies have documented high rates of comorbidity among substance use, anxiety, and depressive disorders (Burns & Teesson, 2002; Grant et al., 2004b; Jones et al., 2016; Regier et al., 1990) that may suggest the presence of a common etiology (Hasin, Stinson, Ogburn, & Grant, 2007). Analyses of nationally representative data from the United States, Australia, and the Netherlands have all found similar results suggesting that those meeting diagnostic criteria for an anxiety or depressive disorder have roughly twice the odds of experiencing a co-occurring AUD compared to those not experiencing anxiety or depression (Boschloo et al., 2011; Burns & Teesson, 2002; Grant et al., 2004b). While multiple factors may independently impact anxiety, depression, or AUD, comorbid disorders are hypothesized to develop through shared antecedents such as exposure to adverse environments or events paired with cognitive vulnerability to stress (Brady & Sinha, 2005; Hankin & Abramson, 2001; Keyes, Hatzenbuehler, & Hasin, 2011). Exposure to adverse environments or events can overwhelm individual coping skills, harm neurobiological functioning, increase cognitive vulnerability to stress, escalate risk for psychological distress, and, in turn, risk of AUD (Hankin & Abramson, 2001; Pollack, 2004). It has been well-documented that, faced with exposure to repeated stressful experiences or acute instances of stress, individuals with reduced coping skills are at increased risk for developing AUD or relapsing into AUD (Brady & Sinha, 2005; Witkiewitz & Marlatt, 2004). Furthermore, those experiencing psychological distress may use alcohol as a coping strategy to regulate distress (Holahan, Moos, Holahan, Cronkite, & Randall, 2001, 2003).
Neighborhoods, Mental Health, and Alcohol Use
Studies examining the role of neighborhood contexts, mental health, and substance use are often built upon socioecological models of human behavior posited by Bronfenbrenner (1977). Socioecological models of health behavior suggest that individual-level factors alone are insufficient for understanding health behaviors and that larger social environments such as neighborhoods contextualize both positive and negative health behaviors at the individual-level (Diez Roux & Mair, 2010; Wilson, 1987). Socioecological theories are regularly applied to substance use and mental health research to warrant examination of both structural features of neighborhoods as well as social processes occurring within neighborhoods (Galea, Nandi, & Vlahov, 2004; Sampson, Morenoff, & Gannon-Rowley, 2002). Systematic reviews have found that studies examining associations between neighborhood socioeconomic disadvantage and alcohol use are yet to produce consistent results (Bryden, Roberts, Petticrew, & McKee, 2013; Jackson, Denny, & Ameratunga, 2014; Karriker-Jaffe, 2011, 2013). While prevalence of alcohol use and misuse tend to cluster geographically, areas with both lower and higher levels of socioeconomic advantage appear to be related to increased alcohol use depending on the study design, methods, type of alcohol use being measured, and population considered (Karriker-Jaffe, 2011). Multiple studies have shown that disorganized neighborhoods categorized by concentrated poverty, high levels of crime, violence, or physical deterioration are associated with heavy drinking (Hill & Angel, 2005; Kuipers, van Poppel, van den Brink, Wingen, & Kunst, 2012) and alcohol or substance use disorders (Martin-Storey et al., 2013; Stockdale et al., 2007; Winstanley et al., 2008). Neighborhood disorganization has been found to be largely a function of neighborhood socioeconomic disadvantage (Herrenkohl, Hawkins, Abbott, & Guo, 2002) and a key mediator in the relationship between neighborhood socioeconomic disadvantage and substance use problems (Martin-Storey et al., 2013; Stockdale et al., 2007).
A clearer picture emerges from the research literature regarding associations between neighborhood socioeconomic disadvantage and anxiety, depression, or other indicators of psychological distress (see Truong and Ma (2006) for a systematic review and Hill and Mamion (2013) for a recent theoretical discussion). Similar to results from studies examining alcohol use, mental health researchers have identified neighborhood disorganization as an important mediator of the relationship between neighborhood socioeconomic disadvantage and increased psychological distress (Casciano & Massey, 2012; Kim, 2010; Ross & Mirowsky, 2001). Both empirical and theoretical work has suggested that the accumulation of fear and stress, which are normative psychological responses to exposure to disorganized and unsafe neighborhoods, are a mechanism by which disorganized neighborhoods impact mental health (Casciano & Massey, 2012; Hill & Maimon, 2013; Mirowsky & Ross, 2003; Ross & Mirowsky, 2001; Sampson et al., 2002; Stockdale et al., 2007).
Three studies are of particular relevance for the current investigation. Stockdale and colleagues (2007) study identified significant cross-sectional associations among neighborhood disorganization and comorbid alcohol, drug, and other mental health disorders among adults. Models from their study considering anxiety and depression separately from substance abuse disorders (SUD) found effects of neighborhood violence on anxiety and depression but not on SUD (Stockdale et al., 2007). A second study by Buu and colleagues (2007) considered data from fathers with AUD at two time points over 12 years. Respondents living in more disadvantaged neighborhoods exhibited more symptoms of AUD 12 years later after accounting for baseline AUD symptoms and other sociodemographic controls. We located only one study examining neighborhood disorganization, anxiety, depression, and problem drinking over time among adults. Hill and Angel (2005) examined data from approximately 2,400 low-income women with children across two waves of data. Employing a single-item ordinal measure of how often individuals were intoxicated in the past 12 months (never = 0, once or twice = 1, several times =2, often = 3), Hill and Angel found an association between neighborhood disorganization and increased drinking that was fully mediated by anxiety and depression after controlling for a range of sociodemographic factors. The current study is built upon the work of these authors, as well as many others, to examine the longitudinal trajectory of AUD symptoms across adulthood and associations with time-varying measures of neighborhood disorganization, psychological distress, and sociodemographic factors.
Hypotheses
Based on our review of the literature, we expect that, on average, individuals will show reduced symptoms of AUD from age 21 to 39. We also hypothesize that women will exhibit fewer AUD symptoms. We expect that individuals living in more disorganized neighborhoods will likely exhibit higher AUD symptoms across adulthood after controlling for sociodemographic factors. Finally, we hypothesize that psychological distress will mediate the association between neighborhood disorganization and AUD symptoms.
Methods
Sample
Data were drawn from the Seattle Social Development Project (SSDP), a longitudinal, theory-driven study originating in 18 Seattle elementary schools that over-represented high crime neighborhoods. SSDP began conducting in-person interviews in 1985 with 808 students in the 5th grade when most participants were 10 years old (M = 10.3, SD = .52). The 808 respondents accounted for 77% of 1,053 5th grade students invited to participate in the study. Retention rates for the participating sample ranged from 88% to 96% of the still living sample across the six waves of data employed in this study. Of the longitudinal sample, 49% were female, 46% were European American, 24% were African American, 21% were Asian American and 9% were Native American. Participants without data on AUD symptoms at any wave from age 21 to 39 were excluded from the analysis (N=18). The analytic sample for this study employed prospectively gathered data across six waves from ages 21 through 39 from 790 participants.
Measures
Descriptive statistics for measures included in the analysis are shown in Table 1.
Table 1.
Sample descriptive statistics
| Age 21 | Age 24 | Age 27 | Age 30 | Age 33 | Age 39 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||||
| Min | Max | M | SD | M | SD | M | SD | M | SD | M | SD | M | SD | |
| Alcohol Use Disorder (AUD) symptoms | 0 | 11 | 1.26 | 1.81 | 1.09 | 1.78 | .92 | 1.84 | .80 | 1.73 | .78 | 1.86 | .55 | 1.55 |
| No AUD symptoms | 0 | 1 | 52% | 57% | 68% | 71% | 74% | 81% | ||||||
| Psychological Distressa | 0 | 1 | 22% | 17% | 16% | 14% | 13% | 17% | ||||||
| Anxiety | 0 | 1 | 6% | 8% | 6% | 6% | 6% | 11% | ||||||
| Depression | 0 | 1 | 20% | 13% | 13% | 12% | 10% | 11% | ||||||
| Neighborhood Disorganization | 1 | 4 | 1.65 | .62 | 1.59 | .59 | 1.55 | .58 | 1.54 | .57 | 1.56 | .64 | 1.63 | .64 |
| Educational Attainmentb | 1 | 3 | 1.85 | .38 | 2.04 | .59 | 2.12 | .56 | 2.15 | .58 | 2.17 | .58 | 2.23 | .55 |
| Household Incomec | 1 | 6 | 1.47 | .83 | 3.02 | 1.56 | 3.10 | 1.61 | 3.17 | 1.60 | 3.70 | 1.68 | 3.74 | 1.84 |
| Married | 0 | 1 | 9% | 23% | 30% | 40% | 42% | 51% | ||||||
| Parenthood | 0 | 1 | 27% | 43% | 50% | 59% | 67% | 79% | ||||||
| Female | 0 | 1 | 49% | - | - | - | - | - | ||||||
| African American | 0 | 1 | 26% | - | - | - | - | - | ||||||
| Asian American | 0 | 1 | 22% | - | - | - | - | - | ||||||
| Native American | 0 | 1 | 5% | - | - | - | - | - | ||||||
| European American | 0 | 1 | 47% | - | - | - | - | - | ||||||
Notes. M = mean, SD = standard deviation.
indicated by a probable diagnosis of anxiety or depression;
1 = less than high school, 2 = high school diploma or GED, 3 = college degree or higher;
1 = less than $20,000, 6 = greater than $100,000 household income annually.
Alcohol Use Disorder
Past year AUD symptoms were measured as the sum of criteria for alcohol abuse or dependence met by respondents in the past year. Eleven diagnostic symptoms defined by the DSM-IV (American Psychological Association, 1994) were evaluated at each wave using a modified version of the Diagnostic Interview Schedule (DIS; McGee et al., 1990; Robins, Helzer, Croughan, Williams, & Spitzer, 1981). These symptoms included inability to fulfill life role obligations due to alcohol use, recurrent alcohol-related legal problems, alcohol use in dangerous situations, repeated social problems due to alcohol use, and physical or mental health problems resulting from alcohol consumption. Internal consistency for AUD items (Cronbach’s α) for each wave ranged from .75 to .84. We employed a count measure of AUD symptoms as our dependent variable throughout this study to capture both individuals with a diagnosable AUD and those engaging in subclinical levels of problem drinking. Similar strategies have been used by other studies and higher symptoms counts are considered indicative of more severe drinking problems (Buu et al., 2007; Goldstein et al., 2015; Lee, Kosterman, McCarty, Hill, & Hawkins, 2012).
Psychological Distress
Generalized anxiety disorder (GAD) and major depressive episode (MDE) were assessed at each wave using the DIS. To create a single dichotomous measure of psychological distress, participants were first classified with MDE if they reported at least five out of nine potential symptoms and at least three of those symptoms disrupted daily life. Symptoms included changes in weight or appetite, sleep difficulties, moving or talking slowly, fatigue, difficulty concentrating or making decisions, guilt or worthlessness, and thoughts of suicide or death spanning most days for at least two weeks in the past year. Next, participants were classified with GAD if they endorsed at least two out of six potential symptoms concerning problems with irritability, recurrent worrying, and distractibility spanning most days for at least two weeks in the past year and disrupting daily life. At each wave, the correlation between anxiety and depression ranged from .32 to .40. Similar to other studies, those meeting criteria for a likely MDE or GAD were coded as 1 (or 0 otherwise) (Stockdale et al., 2007). Theoretical work (Mirowsky & Ross, 2003) in conjunction with our own sensitivity tests (results not shown) supported combining anxiety and depression into a single measure of psychological distress.
Neighborhood Disorganization
A self-report measure of neighborhood disorganization was represented by the mean of seven items that assessed the extent to which crime or drug dealing, shootings or knifings, fights, gangs, undesirable neighbors, graffiti, and empty or abandoned buildings described the respondent’s neighborhood. Each item offered the same response options (1=YES!, 2=yes, 3=no, 4=NO!), scale internal consistency across waves ranged from .87 to .93, and items were standardized within each year prior to analysis. Similar measures of neighborhood disorganization have been employed in other studies (Herrenkohl et al., 2002; Sampson et al., 2002).
Sociodemographic Factors
Multiple studies have shown that sociodemographic factors including education, marital status, income, and parenthood are associated with alcohol consumption. Currently being married and parenting children have consistently shown protective effects against problem drinking (Dawson, Grant, Chou, & Pickering, 1995; Miller-Tutzauer, Leonard, & Windle, 1991; O Malley, 2004). While higher socioeconomic status (SES) as measured by income and educational attainment has often been associated with increased alcohol consumption (Dawson et al., 1995; Moore et al., 2005; Van Oers, Bongers, Van de Goor, & Garretsen, 1999), higher SES is also consistently related to decreased problem drinking (Van Oers et al., 1999) and diagnoses of alcohol dependence (Gilman et al., 2008; Hasin et al., 2007; Keyes & Hasin, 2008). For the SSDP sample, educational attainment was assessed at each wave with an ordinal variable coded as 1 for less than high school completion, 2 for high school diploma or GED, and 3 for completion of a 4 year college degree or higher. Current marital status was assessed at each wave with 1 indicating married and 0 indicating not married. A six category measure of household income broken into $20,000 increments was assessed at each wave and measures were standardized within wave prior to analysis. Parenthood was measured at each wave as a current biological or adoptive parent and coded with current parenthood equal to 1.
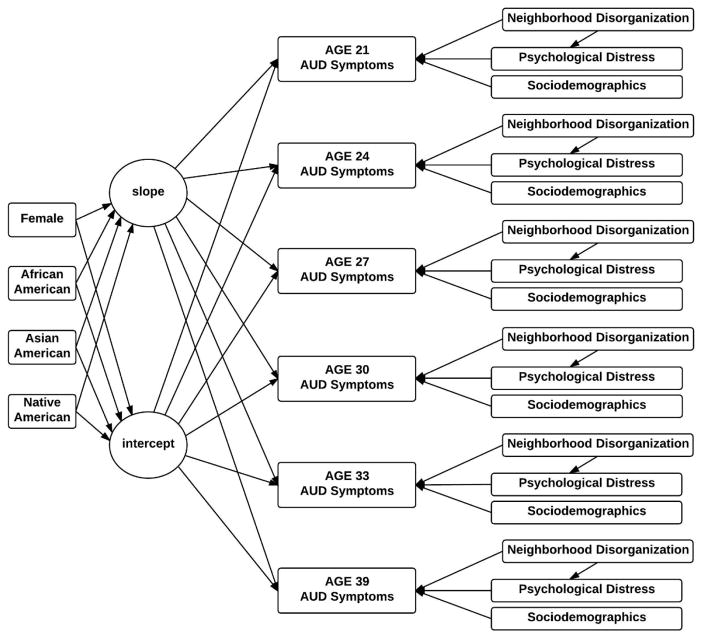
Analytic Strategy
Latent growth curve modeling provides an established method of examining change in substance use over time and is flexible enough to allow for individual differences in initial levels of substance use, rates of change over time, and deviation from average levels of use at each time point (Curran & Hussong, 2003). Deviation from average levels of substance use can be examined by simultaneously estimating the growth curve and regressing predictors on the indicators constituting the growth parameters (Hussong, Curran, Moffitt, Caspi, & Carrig, 2004). Figure 1 presents a conceptual diagram including time-fixed and time-varying covariates. An initial unconditional model estimated the average trajectory of AUD symptoms from ages 21 to 39 and found a statistically significant mean and variance of the growth parameters (i.e., intercept and slope) warranting further examination of time-fixed and time-varying covariates. Model 1 included time-fixed covariates for gender and ethnicity as well as time-varying measures of educational attainment, marital status, household income, and parenthood status predicting AUD symptoms controlling for average growth in AUD symptoms. Models 2 and 3 included neighborhood disorganization and psychological distress respectively as time-varying predictors of AUD symptoms. Model 4 examined indirect effects of psychological distress as a mediator of the association between neighborhood disorganization and AUD symptoms independent of time-fixed and time-varying sociodemographic factors. All models constrained the association of time-varying covariates with AUD symptoms to estimate their average association across adulthood and the same procedure was employed for the mediation model. Models with time-varying covariates constrained over time consistently showed better fit compared to those with covariates free to vary across time. Model fit was compared across models using sample size adjusted BIC (Curran & Hussong, 2003) and a reduction of five or more in BIC was considered an improvement model fit (Singer & Willett, 2003).
Figure 1.
Path diagram for negative binomial latent growth curve of alcohol use disorder (AUD) symptoms with time-varying measures of neighborhood disorganization, psychological distress, and sociodemographic factors. Psychological distress was tested as a mediator between neighborhood disorganization and AUD symptoms. Covariance between the slope and intercept and covariances among exogenous predictors not shown.
Missing data were handled via multiple imputation (Asparouhov & Muthén, 2010). Data were present for over 93% of possible data points (33,863 out of 36,340) across 46 variables used in these analyses. Forty datasets were created and subsequently analyzed using the multiple imputation and latent growth modeling procedures in Mplus version 7.1 (Muthén & Muthén, 2006). All reported model results employ the MLR estimator for robust standard errors and are averaged across 40 datasets using Rubin’s rules (Rubin, 1987). Commonly used model fit indices (e.g. CFI, RMSEA) are not available for negative binomial latent growth curves using the MLR estimator (Muthén & Muthén, 2006). Initial results of an unconditional growth model showed over-dispersion on measures of AUD symptoms warranting the use of a negative binomial distribution. Given the preponderance of zeros for counts of AUD symptoms at each time point and the potential for non-linear growth, we also examined zero-inflated negative binomial latent growth models and the inclusion of a quadratic growth term. These specifications did not alter our substantive findings and, as a result, parameter estimates and model fit statistics from negative binomial growth curves without a quadratic term are reported in Table 2. Some SSDP participants received a social development intervention during elementary school (Hawkins et al., 1992). Sensitivity tests controlling for the intervention on all paths in Model 4 did not show any substantive changes to the findings reported in Table 2.
Table 2.
Results of latent growth curves predicting Alcohol Use Disorder (AUD) symptoms
| Independent Variable | Dedependent Variable | Model 1 | Model 2 | Model 3 | Model 4 |
|---|---|---|---|---|---|
| Time-varying Covariates | Est. (SE) | Est. (SE) | Est. (SE) | Est. (SE) | |
| Educational Attainmenta | AUD | −.30 (.08) *** | −.27 (.08) *** | −.26 (.08) *** | −.26 (.08) *** |
| Psy. Distress | −.11 (.06) | ||||
| Marriedb | AUD | −.42 (.09) *** | −.41 (.09) *** | −.38 (.09) *** | −.38 (.09) *** |
| Psy. Distress | −.25 (.07) ** | ||||
| Household Incomec | AUD | −.05 (.03) | −.05 (.03) | −.04 (.03) | −.04 (.03) |
| Psy. Distress | −.09 (.02) *** | ||||
| Parenthoodb | AUD | −.18 (.10) | −.18 (.10) | −.19 (.10) * | −.19 (.10) * |
| Psy. Distress | .06 (.07) | ||||
| Neighborhood Disorganizationc | AUD | .17 (.04) *** | .15 (.04) *** | .15 (.04) *** | |
| Psy. Distress | .16 (.03) *** | ||||
| Psychological Distressb | AUD | .46 (.07) *** | .46 (.07) *** | ||
| Mediation Analysesd | |||||
| Indirect Path | AUD | .08 (.03) *** | |||
| Total Path | AUD | .22 (.04) *** | |||
| Time-fixed Covariates | |||||
| Female | Intercept | −.89 (.11) *** | −.88 (.11) *** | −.91 (.11) *** | −.91 (.11) *** |
| Slope | −.03 (.01) * | −.03 (.01) * | −.03 (.01) * | −.03 (.01) * | |
| Psy. Distress | .28 (.12) *** | ||||
| African American | Intercept | −.28 (.15) | −.33 (.14) | −.35 (.14) | −.35 (.14) |
| Slope | .00 (.02) | .00 (.02) | .00 (.02) | .00 (.02) | |
| Psy. Distress | .00 (.16) | ||||
| Asian American | Intercept | −.25 (.14) | −.26 (.14) | −.27 (.14) | −.27 (.14) |
| Slope | −.04 (.02) | −.03 (.02) | −.03 (.02) | −.03 (.02) | |
| Psy. Distress | −.06 (.) | ||||
| Native American | Intercept | .59 (.17) ** | .55 (.17) ** | .53 (.16) ** | .53 (.16) ** |
| Slope | −.01 (.03) | −.02 (.03) | −.02 (.03) | −.02 (.03) | |
| Psy. Distress | .09 (.14) | ||||
| Table 3.3 (continued) | |||||
| AUD Intercept & Slope | |||||
| AUD | Intercept | .92 (.18) *** | .89 (.17) *** | .79 (.17) *** | .79 (.17) *** |
| Slope | −.08 (.01) *** | −.08 (.01) *** | −.08 (.01) *** | −.08 (.01) *** | |
| Residual Variance | Intercept | 1.03 (.13) *** | .96 (.13) *** | .86 (.13) *** | .86 (.13) *** |
| Slope | .01 (.00) *** | .01 (.00) *** | .01 (.00) *** | .01 (.00) *** | |
| Intercept & Slope Covariance | .03 (.01) ** | .03 (.01) ** | .03 (.01) ** | .03 (.01) ** | |
| BICe | 9462 (9498) | 9444 (9463) | 9402 (9416) | 13545 (13596) | |
Notes : N=790;
p<.05,
p<.01,
p<.001;
Est. = unstandardized estimate; SE = standard error; Psy. Disress = psychological distress; estimates are constrained to be equal from age 21 to 39; all ethnicity variables are compared to European Americans.
1 = less than high school, 2 = high school completion, 3 = college degree or higher;
variables coded as 0 | 1 with 1 indicating the variable name;
variables were standardized with mean = 0 and SD = 1 within year prior to analysis;
Indirect Path indicates the estimate of Neighborhood Disorganization through Psychological Distress to AUD and Total Path indicates the sum of the Direct and Indirect Paths from Neighborhood Disorganization to AUD;
BIC in parentheses indicates fit for a model with time-varying predictors unconstrained over time.
Results
Results of descriptive analyses and Models 1 through 4 are found in Tables 1 and 2 respectively. Correlations among constructs are presented in the appendix. Among the SSDP sample, approximately 21% of 21–30 year olds met criteria for a DSM-IV AUD diagnosis in the past year while national estimates place the prevalence of AUD diagnoses in the past year at 16% for 18–29 year olds (Hasin et al., 2007) and 18% for 18 to 25 year olds (Hedden, 2015). Differences may reflect lack of diagnostic data in the SSDP sample for individuals under age 21. Approximately 30% of the SSDP sample (n=240) never displayed any symptoms of AUD. Results of the unconditional growth model confirmed that individuals reduced their problem drinking on average from age 21 to 39. The unconditional model also found heterogeneity across individuals in both AUD symptoms at age 21 and rates of decrease in AUD symptoms through the 30s as indicated by significant variance in the intercept (Est. = 1.35, p < .001) and slope (Est. = .01, p<.001) of the latent growth curve respectively. The variance of the slope and intercept remained significant across all models indicating variability in trajectories of AUD symptoms across individuals. A positive and significant covariance between intercept and slope parameters indicated that individuals with higher counts of AUD symptoms at age 21 tended to reduce problem drinking more slowly across adulthood. The covariance between the intercept and slope remained positive and significant across all models.
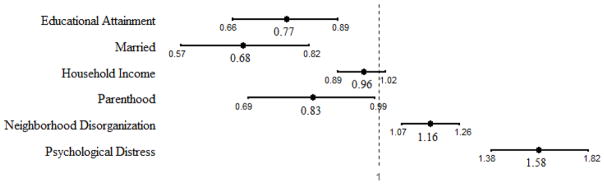
Model 1 found that, as expected, women showed lower initial counts of AUD symptoms at age 21 and significantly quicker reductions in problem drinking through the 30s compared to men after accounting for educational attainment, marital status, household income, and parenthood. Native Americans had a higher number of AUD symptoms at age 21 when compared to European Americans but no difference in the rate of decline. On average, married individuals and those with higher levels of educational attainment showed significantly fewer AUD symptoms across adulthood after accounting for average slope of AUD symptoms over time and other sociodemographic factors. Model 2 included a time-varying measure of neighborhood disorganization. Higher levels of neighborhood disorganization were associated with increased AUD symptoms after accounting for average change in AUD symptoms and sociodemographic factors. Model 3 included a time-varying measure of psychological distress and found it to be associated with increased AUD symptoms across adulthood after accounting for all other factors included in the model. With the inclusion of psychological distress in Model 3, parenthood emerged as a significant predictor of fewer AUD symptoms while results from Models 1 and 2 showed only trend level associations (p < .1) for parenthood. Figure 2 provides a comparison of associations between time-varying covariates and AUD symptoms.
Figure 2.
Count ratios and 95% confidence intervals (CIs) from Model 3 for time-varying covariates predicting alcohol use disorder (AUD) symptoms from age 21 to 39 after controlling for average trajectory of AUD symptom severity, gender, and ethnicity. CIs fully above 1 indicate that variable is significantly associated with increased AUD symptoms and CIs fully below 1 indicate that variable is significantly associated fewer AUD symptoms. Confidence intervals crossing 1 indicate a non-significant association.
Mediational analyses in Model 4 found a significant indirect effect of neighborhood disorganization through psychological distress after accounting for all other factors in the model and controlling for sociodemographic differences in psychological distress. Women showed an increased likelihood of psychological distress compared to men across adulthood. Higher household income and being currently married were associated with reduced psychological distress over time. In Model 4, neighborhood disorganization maintained a significant direct effect on AUD symptoms across adulthood and no other changes in the substantive interpretation of coefficients for time-fixed or time-varying covariates were noted. Psychological distress accounted for approximately one third of the total association between neighborhood disorganization and AUD symptoms.
Discussion
The current study is the first to consider trajectories of problem drinking and the role of neighborhood contexts across nearly 20 years of adulthood. While other studies have considered individual components of this study, we are aware of no other studies incorporating neighborhood disorganization, psychological distress, and sociodemographic factors into a longitudinal model of problem drinking severity. These features of the analysis reported here provide an opportunity to address important questions across multiple domains of inquiry.
We sought to understand risk and promotive factors associated with increased severity of AUD symptoms above and beyond average reductions in AUD severity over time. Most importantly, our results provide evidence that individuals living in more disorganized neighborhoods are at increased risk of psychological distress and more severe AUD net of educational attainment, household income, marital status, parenthood, gender, and ethnicity. Consistent with reports by others, individuals on average engaged in less problem drinking as they moved through adulthood (Delker et al., 2016; Grant et al., 2004a; Grant et al., 2015; Hasin et al., 2007). We also observed heterogeneity in initial starting levels of AUD at age 21 and rates of change for AUD over time. As suggested by other researchers (Connor et al., 2016), individuals with lower initial levels of AUD at age 21 reduced their problem drinking more quickly. We noted lower levels of AUD among women (Dawson et al., 1995; Hasin et al., 2007) at age 21 as well as more rapid reductions in AUD symptoms across adulthood. Similar to AUD symptoms, we also found that psychological distress was significantly associated with lower educational status and currently being unmarried. Unlike for AUD symptoms, lower household income and being female were significantly associated with increased risk of psychological distress. The latter associations between psychological distress, household income, and gender have been found in nationally representative studies (Grant et al., 2005; Kessler et al., 2003). This study has replicated and extended results of previous studies and has found that the hypothesized interrelationships between neighborhood disorganization, psychological distress, and AUD symptom severity extends across the 30s, contributing to the substantial societal costs associated with problem drinking (Sacks et al., 2015).
Our results suggest implications for practitioners seeking to understanding and ameliorate the potential impacts of disorganized neighborhoods on psychological distress and AUD symptoms. First, our findings add evidence to suggestions by other researchers that regular exposure to crime, drug selling, violence, and deteriorating infrastructure in one’s neighborhood may create a shared risk for anxiety, depression, and heavy alcohol use (Hill & Maimon, 2013). These results support calls for treatment of anxiety or depressive disorders to be provided to individuals diagnosed with an AUD as needed (Grant et al., 2004b). We should, however, consider any treatment suggestions in context for those living in more disorganized neighborhoods. Given that residents of disorganized neighborhoods are likely to experience accumulated impacts of stress, they may particularly benefit from trauma-informed models of health care (Butcher, Galanek, Kretschmar, & Flannery, 2015). Trauma-informed care recognizes that symptoms of mental health disorders may represent adaptive coping strategies operating in response to previous experiences. See Butler, Critelli and Rinfrette (2011) for recent discussion of trauma-informed mental health care and service delivery models. A second treatment-oriented contextual issue is found in consistent reports that residents of socioeconomically disadvantaged neighborhoods contend with reduced health care service availability, lower service utilization rates, increased likelihood of experiencing unmet health care needs, and decreased likelihood of receiving preventive care (Kirby & Kaneda, 2005; Lurie & Dubowitz, 2007; O’Campo, Salmon, & Burke, 2009). Coordinated federal, state, and local policy efforts are needed to not only increase the safety and quality of poor neighborhoods (Brooks-Gunn, Duncan, & Aber, 1997; Wilson, 1987), but also to address disparities in health care service availability and utilization in disadvantaged neighborhoods (see Almgren (2012) for an extensive discussion on the topic).
The current findings in conjunction with consistent documentation of comorbid diagnoses of anxiety, depression, and AUD (Hasin et al., 2007; Regier et al., 1990) suggest that the links between neighborhood disadvantage and problem drinking are likely mediated in part by exposure to stressful environments, accumulated stress, and psychological distress. It is important to keep in mind, however, the substantial challenges faced by individuals and families seeking to migrate out of socioeconomically disadvantaged or disorganized neighborhoods (Massey, 2013; Sharkey, 2013). These challenges may be further exacerbated by the presence of anxiety, depression, or AUD. While lack of individual and family economic resources undoubtedly deter residential and social mobility, poor mental health or substance abuse problems among residents of disadvantaged neighborhoods may add to mobility limitations (Massey, 2013).
Despite the range of findings suggesting the impact of neighborhood contexts on individual-level outcomes, some additional limitations should be noted regarding the complexity and direction of these relationships. First, we suspect that reciprocal relationships may exist among the time-varying factors considered by this study. Examining the within time associations of AUD symptoms and neighborhood disorganization, psychological distress, and sociodemographic factors over time does not warrant causal claims regarding the direction of our findings. In particular, individuals suffering from significant psychological distress may potentially perceive and report higher levels of neighborhood disorganization (Hill & Maimon, 2013). In addition, analyses were limited to a non-representative sample originating from a single U.S. city; as such, caution should be taken in generalizing these findings to other populations. Future studies that utilize systematic social observations of neighborhood disorganization may offer a promising avenue to help improve our understanding of the relationships among neighborhood disorganization, psychological distress, and problem drinking (Sampson et al., 2002). As scholars have hypothesized that family or individual-level socioeconomics may function to mediate or moderate relationships between neighborhood contexts and mental health or alcohol use problems (Cerdá, Diez-Roux, Tchetgen, Gordon-Larsen, & Kiefe, 2010; Hill & Maimon, 2013), we think future studies seeking to refine our understanding of how, when, and for whom neighborhood factors, psychological distress, substance use disorders, and sociodemographic factors are associated can provide important insights for etiology, treatment, and preventive intervention (Sharkey & Faber, 2014).
Acknowledgments
Data collection for this study was supported by grants from the National Institute on Drug Abuse (5R01DA003721 and 5R01DA033956). Partial support was provided a National Poverty Research Center Dissertation Fellowship awarded by the Institute for Research on Poverty at the University of Wisconsin–Madison with funding from the Office of the Assistant Secretary for Planning and Evaluation, U.S. Department of Health and Human Services, Cooperative Agreement number AE00103. Partial support was also provided by a Eunice Kennedy Shriver National Institute of Child Health and Human Development research infrastructure grant, No. R24HD042828; and training grant No. T32HD007543 to the Center for Studies in Demography and Ecology at the University of Washington. The opinions and conclusions expressed herein are solely those of the author and should not be construed as representing the opinions or policy of any agency of the Federal government.
Table 1.
Average correlations from age 21 to 39
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | ||
|---|---|---|---|---|---|---|---|---|
|
|
||||||||
| AUD Symptoms | 1 | .61 | ||||||
| Pscyholgical Distress | 2 | .10 | .46 | |||||
| NH Disorganization | 3 | .16 | .12 | .55 | ||||
| Education | 4 | −.13 | −.10 | −.18 | .86 | |||
| Married | 5 | −.13 | −.09 | −.13 | .11 | .55 | ||
| Household Income | 6 | −.09 | −.14 | −.19 | .26 | .17 | .59 | |
| Parenthood | 7 | −.05 | .06 | .06 | −.27 | .12 | −.18 | .73 |
| Female | 8 | −.20 | .09 | −.04 | .10 | .04 | −.10 | .14 |
| African American | 9 | .00 | .08 | .16 | −.17 | −.19 | −.25 | .21 |
| Native American | 10 | .14 | .04 | .07 | −.15 | −.02 | −.06 | .09 |
| Asian American | 11 | −.07 | −.08 | −.11 | .17 | .08 | .18 | −.07 |
Notes. N=790; AUD = alcohol use disorder, NH = neighborhood.
References
- Almgren GR. Health care politics, policy and services: a social justice analysis. Springer Publishing Company; 2012. [Google Scholar]
- American Psychological Association. Diagnostic and statistical manual of mental disorders (DSM-IV) American Psychiatric Association; 1994. [Google Scholar]
- Asparouhov T, Muthén B. MPlus Web Notes. 2010. Multiple imputation with Mplus. [Google Scholar]
- Boschloo L, Vogelzangs N, Smit JH, van den Brink W, Veltman DJ, Beekman AT, Penninx BW. Comorbidity and risk indicators for alcohol use disorders among persons with anxiety and/or depressive disorders: findings from the Netherlands Study of Depression and Anxiety (NESDA) Journal of affective disorders. 2011;131(1):233–242. doi: 10.1016/j.jad.2010.12.014. [DOI] [PubMed] [Google Scholar]
- Brady KT, Sinha R. Co-occurring mental and substance use disorders: the neurobiological effects of chronic stress. American Journal of Psychiatry. 2005;162(8):1483–1493. doi: 10.1176/appi.ajp.162.8.1483. [DOI] [PubMed] [Google Scholar]
- Bronfenbrenner U. Toward an experimental ecology of human development. American psychologist. 1977;32(7):513. [Google Scholar]
- Brooks-Gunn J, Duncan G, Aber JL. Neighborhood poverty, Volume 2: Policy implications in studying neighborhoods. Russell Sage Foundation; 1997. [Google Scholar]
- Bryden A, Roberts B, Petticrew M, McKee M. A systematic review of the influence of community level social factors on alcohol use. Health & place. 2013;21:70–85. doi: 10.1016/j.healthplace.2013.01.012. [DOI] [PubMed] [Google Scholar]
- Burns L, Teesson M. Alcohol use disorders comorbid with anxiety, depression and drug use disorders: Findings from the Australian National Survey of Mental Health and Well Being. Drug and alcohol dependence. 2002;68(3):299–307. doi: 10.1016/s0376-8716(02)00220-x. [DOI] [PubMed] [Google Scholar]
- Butcher F, Galanek JD, Kretschmar JM, Flannery DJ. The impact of neighborhood disorganization on neighborhood exposure to violence, trauma symptoms, and social relationships among at-risk youth. Social science & medicine. 2015;146:300–306. doi: 10.1016/j.socscimed.2015.10.013. [DOI] [PubMed] [Google Scholar]
- Butler LD, Critelli FM, Rinfrette ES. Trauma-informed care and mental health. Directions in Psychiatry. 2011;31(3):197–212. [Google Scholar]
- Buu A, Mansour M, Wang J, Refior SK, Fitzgerald HE, Zucker RA. Alcoholism effects on social migration and neighborhood effects on alcoholism over the course of 12 years. Alcoholism: Clinical and Experimental Research. 2007;31(9):1545–1551. doi: 10.1111/j.1530-0277.2007.00449.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casciano R, Massey DS. Neighborhood disorder and anxiety symptoms: New evidence from a quasi-experimental study. Health & place. 2012;18(2):180–190. doi: 10.1016/j.healthplace.2011.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Fact Sheets - Alcohol Use and Your Health. 2016 Retrieved from http://www.cdc.gov/alcohol/pdfs/alcoholyourhealth.pdf.
- Cerdá M, Diez-Roux AV, Tchetgen ET, Gordon-Larsen P, Kiefe C. The relationship between neighborhood poverty and alcohol use: estimation by marginal structural models. Epidemiology (Cambridge, Mass) 2010;21(4):482. doi: 10.1097/EDE.0b013e3181e13539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connor JP, Haber PS, Hall WD. Alcohol use disorders. The Lancet. 2016;387(10022):988–998. doi: 10.1016/S0140-6736(15)00122-1. [DOI] [PubMed] [Google Scholar]
- Curran PJ, Hussong AM. The use of latent trajectory models in psychopathology research. Journal of abnormal psychology. 2003;112(4):526. doi: 10.1037/0021-843X.112.4.526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson DA, Grant BF, Chou SP, Pickering RP. Subgroup variation in US drinking patterns: results of the 1992 national longitudinal alcohol epidemiologic study. Journal of substance abuse. 1995;7(3):331–344. doi: 10.1016/0899-3289(95)90026-8. [DOI] [PubMed] [Google Scholar]
- Delker E, Brown Q, Hasin DS. Alcohol consumption in demographic subpopulations: an epidemiologic overview. Alcohol research: current reviews. 2016;38(1):7. doi: 10.35946/arcr.v38.1.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diez Roux AV, Mair C. Neighborhoods and health. Annals of the New York Academy of Sciences. 2010;1186(1):125–145. doi: 10.1111/j.1749-6632.2009.05333.x. [DOI] [PubMed] [Google Scholar]
- Galea S, Nandi A, Vlahov D. The social epidemiology of substance use. Epidemiologic reviews. 2004;26(1):36–52. doi: 10.1093/epirev/mxh007. [DOI] [PubMed] [Google Scholar]
- Gilman S, Breslau J, Conron K, Koenen K, Subramanian S, Zaslavsky A. Education and race-ethnicity differences in the lifetime risk of alcohol dependence. Journal of epidemiology and community health. 2008;62(3):224–230. doi: 10.1136/jech.2006.059022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstein RB, Chou SP, Smith SM, Jung J, Zhang H, Saha TD, … Grant BF. Nosologic comparisons of DSM-IV and DSM-5 alcohol and drug use disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions–III. Journal of studies on alcohol and drugs. 2015;76(3):378–388. doi: 10.15288/jsad.2015.76.378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Dawson DA, Stinson FS, Chou SP, Dufour MC, Pickering RP. The 12-month prevalence and trends in DSM-IV alcohol abuse and dependence: United States, 1991–1992 and 2001–2002. Drug and alcohol dependence. 2004a;74(3):223–234. doi: 10.1016/j.drugalcdep.2004.02.004. [DOI] [PubMed] [Google Scholar]
- Grant BF, Goldstein RB, Saha TD, Chou SP, Jung J, Zhang H, … Huang B. Epidemiology of DSM-5 alcohol use disorder: results from the National Epidemiologic Survey on Alcohol and Related Conditions III. JAMA psychiatry. 2015;72(8):757–766. doi: 10.1001/jamapsychiatry.2015.0584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Hasin DS, Stinson FS, Dawson DA, Ruan WJ, Goldstein RB, … Huang B. Prevalence, correlates, co-morbidity, and comparative disability of DSM-IV generalized anxiety disorder in the USA: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Psychological medicine. 2005;35(12):1747–1759. doi: 10.1017/S0033291705006069. [DOI] [PubMed] [Google Scholar]
- Grant BF, Stinson FS, Dawson DA, Chou SP, Dufour MC, Compton W, … Kaplan K. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: Results from the national epidemiologic survey on alcohol and related conditions. Archives of general psychiatry. 2004b;61(8):807–816. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- Gutjahr E, Gmel G, Rehm J. Relation between average alcohol consumption and disease: an overview. European addiction research. 2001;7(3):117–127. doi: 10.1159/000050729. [DOI] [PubMed] [Google Scholar]
- Hankin BL, Abramson LY. Development of gender differences in depression: An elaborated cognitive vulnerability–transactional stress theory. Psychological bulletin. 2001;127(6):773. doi: 10.1037/0033-2909.127.6.773. [DOI] [PubMed] [Google Scholar]
- Hasin DS, Stinson FS, Ogburn E, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Archives of general psychiatry. 2007;64(7):830–842. doi: 10.1001/archpsyc.64.7.830. [DOI] [PubMed] [Google Scholar]
- Hawkins JD, Catalano RF, Morrison DM, O’Donnell J, Abbott RD, Day LE. The Seattle Social Development Project: effects of the first four years on protective factors and problem behaviors. Paper presented at the An earlier version of this chapter was presented at the Society for Research in Child Development; Kansas City, Missouri. Apr 1989.1992. [Google Scholar]
- Hedden SL. Behavioral health trends in the United States: results from the 2014 National Survey on Drug Use and Health. 2015. [Google Scholar]
- Herrenkohl TI, Hawkins JD, Abbott RD, Guo J. Correspondence between youth report and census measures of neighborhood context. Journal of Community Psychology. 2002;30(3):225–233. [Google Scholar]
- Hill TD, Angel RJ. Neighborhood disorder, psychological distress, and heavy drinking. Social science & medicine. 2005;61(5):965–975. doi: 10.1016/j.socscimed.2004.12.027. [DOI] [PubMed] [Google Scholar]
- Hill TD, Maimon D. Handbook of the sociology of mental health. Springer; 2013. Neighborhood context and mental health; pp. 479–501. [Google Scholar]
- Holahan CJ, Moos RH, Holahan CK, Cronkite RC, Randall PK. Drinking to cope, emotional distress and alcohol use and abuse: a ten-year model. Journal of studies on alcohol. 2001;62(2):190–198. doi: 10.15288/jsa.2001.62.190. [DOI] [PubMed] [Google Scholar]
- Holahan CJ, Moos RH, Holahan CK, Cronkite RC, Randall PK. Drinking to cope and alcohol use and abuse in unipolar depression: a 10-year model. Journal of abnormal psychology. 2003;112(1):159. [PubMed] [Google Scholar]
- Hussong AM, Curran PJ, Moffitt TE, Caspi A, Carrig MM. Substance abuse hinders desistance in young adults’ antisocial behavior. Development and psychopathology. 2004;16(4):1029–1046. doi: 10.1017/s095457940404012x. [DOI] [PubMed] [Google Scholar]
- Jackson N, Denny S, Ameratunga S. Social and socio-demographic neighborhood effects on adolescent alcohol use: A systematic review of multi-level studies. Social science & medicine. 2014;115:10–20. doi: 10.1016/j.socscimed.2014.06.004. [DOI] [PubMed] [Google Scholar]
- Jones TM, Hill KG, Epstein M, Lee JO, Hawkins JD, Catalano RF. Understanding the interplay of individual and social–developmental factors in the progression of substance use and mental health from childhood to adulthood. Development and psychopathology. 2016;28(03):721–741. doi: 10.1017/S0954579416000274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karriker-Jaffe KJ. Areas of disadvantage: A systematic review of effects of area-level socioeconomic status on substance use outcomes. Drug and alcohol review. 2011;30(1):84–95. doi: 10.1111/j.1465-3362.2010.00191.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karriker-Jaffe KJ. Neighborhood socioeconomic status and substance use by US adults. Drug and alcohol dependence. 2013;133(1):212–221. doi: 10.1016/j.drugalcdep.2013.04.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Koretz D, Merikangas KR, … Wang PS. The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R) Jama. 2003;289(23):3095–3105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- Keyes KM, Hasin DS. Socio-economic status and problem alcohol use: The positive relationship between income and the DSM-IV alcohol abuse diagnosis. Addiction. 2008;103(7):1120–1130. doi: 10.1111/j.1360-0443.2008.02218.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keyes KM, Hatzenbuehler ML, Hasin DS. Stressful life experiences, alcohol consumption, and alcohol use disorders: the epidemiologic evidence for four main types of stressors. Psychopharmacology. 2011;218(1):1–17. doi: 10.1007/s00213-011-2236-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim J. Neighborhood disadvantage and mental health: The role of neighborhood disorder and social relationships. Social science research. 2010;39(2):260–271. [Google Scholar]
- Kirby JB, Kaneda T. Neighborhood socioeconomic disadvantage and access to health care. Journal of health and social behavior. 2005;46(1):15–31. doi: 10.1177/002214650504600103. [DOI] [PubMed] [Google Scholar]
- Kuipers MA, van Poppel MN, van den Brink W, Wingen M, Kunst AE. The association between neighborhood disorder, social cohesion and hazardous alcohol use: a national multilevel study. Drug and alcohol dependence. 2012;126(1):27–34. doi: 10.1016/j.drugalcdep.2012.04.008. [DOI] [PubMed] [Google Scholar]
- Lee JO, Kosterman R, McCarty CA, Hill KG, Hawkins JD. Can patterns of alcohol use disorder in young adulthood help explain gender differences in depression? Comprehensive psychiatry. 2012;53(8):1071–1077. doi: 10.1016/j.comppsych.2012.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lurie N, Dubowitz T. Health disparities and access to health. Jama. 2007;297(10):1118–1121. doi: 10.1001/jama.297.10.1118. [DOI] [PubMed] [Google Scholar]
- Martin-Storey A, Ruttle PL, Temcheff CE, Serbin LA, Stack DM, Ledingham JE, Schwartzman AE. Longitudinal and concurrent pathways to alcoholism: The importance of perception of neighborhood disorder. Journal of Community Psychology. 2013;41(2):156–174. [Google Scholar]
- Massey DS. Inheritance of poverty or inheritance of place? The emerging consensus on neighborhoods and stratification. SAGE Publications Sage CA; Los Angeles, CA: 2013. [Google Scholar]
- McGee R, Feehan M, Williams S, Partridge F, Silva PA, Kelly J. DSM-III disorders in a large sample of adolescents. Journal of the American Academy of Child & Adolescent Psychiatry. 1990;29(4):611–619. doi: 10.1097/00004583-199007000-00016. [DOI] [PubMed] [Google Scholar]
- Miller-Tutzauer C, Leonard KE, Windle M. Marriage and alcohol use: a longitudinal study of “maturing out”. Journal of studies on alcohol. 1991;52(5):434–440. doi: 10.15288/jsa.1991.52.434. [DOI] [PubMed] [Google Scholar]
- Mirowsky J, Ross CE. Social causes of psychological distress. Transaction Publishers; 2003. [Google Scholar]
- Moore AA, Gould R, Reuben DB, Greendale GA, Carter MK, Zhou K, Karlamangla A. Longitudinal patterns and predictors of alcohol consumption in the United States. American Journal of Public Health. 2005;95(3):458–464. doi: 10.2105/AJPH.2003.019471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus Version 7 user’s guide. Los Angeles, CA: Muthén & Muthén; 2006. [Google Scholar]
- National Insitute on Alcohol Abuse and Alcoholism. Alcohol Facts and Statistics. 2016. [Google Scholar]
- O Malley PM. Maturing out of problematic alcohol use. Alcohol research and Health. 2004;28(4):202. [Google Scholar]
- O’Campo P, Salmon C, Burke J. Neighbourhoods and mental well-being: what are the pathways? Health & place. 2009;15(1):56–68. doi: 10.1016/j.healthplace.2008.02.004. [DOI] [PubMed] [Google Scholar]
- Pollack MH. Comorbid anxiety and depression. The Journal of clinical psychiatry. 2004;66:22–29. [PubMed] [Google Scholar]
- Regier DA, Farmer ME, Rae DS, Locke BZ, Keith SJ, Judd LL, Goodwin FK. Comorbidity of mental disorders with alcohol and other drug abuse: results from the Epidemiologic Catchment Area (ECA) study. Jama. 1990;264(19):2511–2518. [PubMed] [Google Scholar]
- Rehm J, Dawson D, Frick U, Gmel G, Roerecke M, Shield KD, Grant B. Burden of disease associated with alcohol use disorders in the United States. Alcoholism: Clinical and Experimental Research. 2014;38(4):1068–1077. doi: 10.1111/acer.12331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robins LN, Helzer JE, Croughan J, Williams JB, Spitzer RL. NIMH diagnostic interview schedule: Version III. Rockville, MD: National Institute of Mental Health; 1981. [Google Scholar]
- Ross CE, Mirowsky J. Neighborhood disadvantage, disorder, and health. Journal of health and social behavior. 2001:258–276. [PubMed] [Google Scholar]
- Rubin DB. Multiple imputation for nonresponse in surveys. New York: John Wiley & Sons; 1987. [Google Scholar]
- Sacks JJ, Gonzales KR, Bouchery EE, Tomedi LE, Brewer RD. 2010 national and state costs of excessive alcohol consumption. American journal of preventive medicine. 2015;49(5):e73–e79. doi: 10.1016/j.amepre.2015.05.031. [DOI] [PubMed] [Google Scholar]
- Sampson RJ, Morenoff JD, Gannon-Rowley T. Assessing” neighborhood effects”: Social processes and new directions in research. Annual review of sociology. 2002:443–478. [Google Scholar]
- Schulenberg J, O’Malley PM, Bachman JG, Wadsworth KN, Johnston LD. Getting drunk and growing up: trajectories of frequent binge drinking during the transition to young adulthood. Journal of studies on alcohol. 1996;57(3):289–304. doi: 10.15288/jsa.1996.57.289. [DOI] [PubMed] [Google Scholar]
- Sharkey P. Stuck in place: Urban neighborhoods and the end of progress toward racial equality. University of Chicago Press; 2013. [Google Scholar]
- Sharkey P, Faber JW. Where, when, why, and for whom do residential contexts matter? Moving away from the dichotomous understanding of neighborhood effects. Annual review of sociology. 2014;40:559–579. [Google Scholar]
- Singer JD, Willett JB. Applied longitudinal data analysis: Modeling change and event occurrence. Oxford university press; 2003. [Google Scholar]
- Stockdale SE, Wells KB, Tang L, Belin TR, Zhang L, Sherbourne CD. The importance of social context: neighborhood stressors, stress-buffering mechanisms, and alcohol, drug, and mental health disorders. Social science & medicine. 2007;65(9):1867–1881. doi: 10.1016/j.socscimed.2007.05.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results from the 2013 National Survey on Drug Use and Health-Detailed Tables. Rockville, MD: 2014. [PubMed] [Google Scholar]
- Truong KD, Ma S. A systematic review of relations between neighborhoods and mental health. Journal of Mental Health Policy and Economics. 2006;9(3):137. [PubMed] [Google Scholar]
- Van Oers J, Bongers I, Van de Goor L, Garretsen H. Alcohol consumption, alcohol-related problems, problem drinking, and socioeconomic status. Alcohol and alcoholism. 1999;34(1):78–88. doi: 10.1093/alcalc/34.1.78. [DOI] [PubMed] [Google Scholar]
- Wilson W. Truly Disadvantaged: The Inner City, the Underclass, and Public Policy. 1987. [Google Scholar]
- Winstanley EL, Steinwachs DM, Ensminger ME, Latkin CA, Stitzer ML, Olsen Y. The association of self-reported neighborhood disorganization and social capital with adolescent alcohol and drug use, dependence, and access to treatment. Drug and alcohol dependence. 2008;92(1):173–182. doi: 10.1016/j.drugalcdep.2007.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witkiewitz K, Marlatt GA. Relapse prevention for alcohol and drug problems: that was Zen, this is Tao. American psychologist. 2004;59(4):224. doi: 10.1037/0003-066X.59.4.224. [DOI] [PubMed] [Google Scholar]