Abstract
Ankylosing spondylitis is a chronic inflammatory disease that mainly affects axial joints and the changes in the vertebrae cause typical kyphotic posture. In patients with ankylosing spondylitis, the postural changes, including cervical flexion, decreased lumbar lordosis, posterior rotation of pelvis, hip extension, knee flexion, and plantar flexion of ankle along with kyphosis, may occur in the upcoming terms of the disease and may negatively affect balance. Joint and eye involvements; muscular, vestibular and proprioceptional changes can also affect balance. This review evaluates the ankylosing spondylitis-equilibrium relationship together with posture and other parameters of balance.
Keywords: Ankylosing spondylitis, balance, posture
Öz
Ankilozan spondilit temel olarak aksiyal eklemleri etkileyen kronik inflamatuar bir hastalıktır ve omurgadaki değişiklikler tipik kifotik posture sebep olur. Ankilozan spondilitli hastalarda kifozla birlikte servikal fleksiyon, azalmış lomber lordoz, pelvisin posterior rotasyonu, kalça ekstansiyonu, diz fleksiyonu, ayak bilek plantar fleksiyonunu içeren postural değişiklikler dengeyi olumsuz etkileyebilir. Postur ile birlikte eklem ve göz tutulumları, vestibular ve proprioseptif değişiklikler de ayrıca dengeyi etkileyebilir. Bu derlemede ankilozan spondilit denge ilişkisini posturle birlikte dengenin diğer parametreleriyle de ele alınmıştır.
Keywords: Ankilozan spondilit, denge, postür
Introduction
Ankylosing spondylitis (AS) is a chronic inflammatory disease that mainly affects axial joints and may cause limitations in spinal mobility [1]. As the disease progresses, the changes in the vertebrae cause typical kyphotic posture [2]. There is also pain and limitation in joint range of motion due to peripheral joint involvement and enthesis.
Balance disorders in AS may develop as a result of postural changes, muscle shortness, atrophy, joint involvement secondary to the disease, and movement limitations due to pain [3].
Parameters such as pain, function, spinal mobility, stiffness, fatigue, and patient global assessment were proposed for evaluation of patients in the core set of criteria described by the Assessment of Spondyloarthritis International Society and there is no recommendation for assessing equilibrium. There is limited number of studies on balance with AS patients in the literature. Many of these studies focused on the postural features of patients with AS [4].
In this review, the association between AS and balance is discussed in regard to muscle strength, proprioception, and vestibular and visual changes together with posture.
Discussion
Balance is defined as postural adaptation to changes in the gravity center at times of rest and activity [5]. It requires the coordination of visual, auditory, proprioceptive, and neuromuscular systems along with the central nervous system [6]. Balance plays an important role in maintaining daily activities. The musculoskeletal system may be exposed to trauma after falling in people with balance problems. Also, the fear of falling and sequelae development cause activity restriction and reduce the quality of life [7].
Posture
In patients with AS, postural changes, including cervical flexion, decreased lumbar lordosis, posterior rotation of pelvis, hip extension, knee flexion, and plantar flexion of ankle along with kyphosis, may occur in the upcoming terms of the disease and may negatively affect balance [2, 3]. The most evident characteristic among these patients is spinal kyphosis, which causes the forward and backward displacement of the gravity center in the sagittal plane. Other body parts develop a number of compensatory changes to keep the gravity center within the borders of the supporting surface. When spinal ankyloses occurs, only the moving lower extremity joints can compensate for the displacement of the gravity center [8].
In the study by Bot et al. [8] on four patients with advanced kyphosis, they stated that thoracic kyphosis causes the forward and downward displacement of the spine weight center. Some compensatory movements may develop only in the lower extremities in order to maintain balance due to the ankylosis of the spine. In patients who were observed in different postural positions over the force platform, hip extension, knee flexion, and ankle plantar flexion were observed. The patients were observed in different postures including loose, erect, and maximum hip extension in a standing position. Among these postures, they suggested that the compensation was provided primarily by knee flexion and plantar flexion of ankle and that the hip was in continuous maximal extension since only 1–6 degree of change occurred in the hip extension.
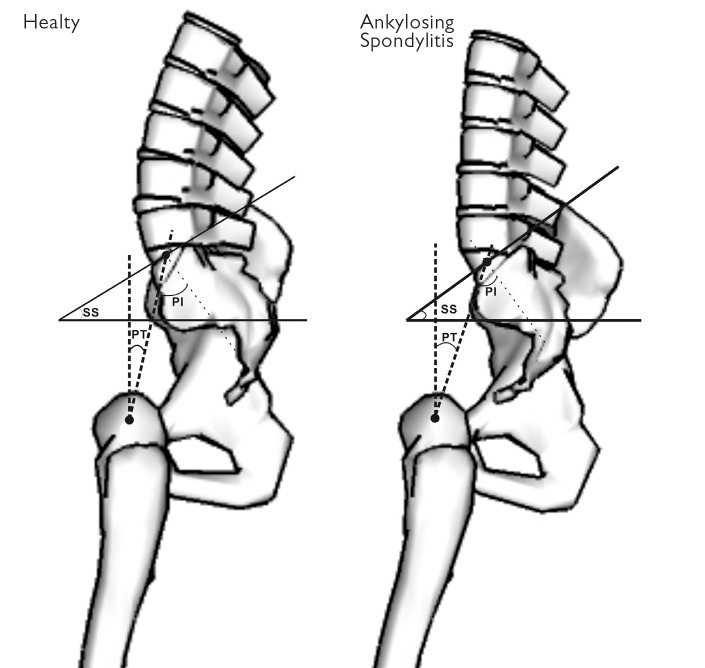
There are also studies in which sagittal changes in the spine were examined in detail. In a study in which sagittal measurements of 40 patients were taken, the sacral slope (the angle between the line passing from the sacral end plate and the horizontal line that is drawn parallel to the floor), pelvic tilt (the angle formed by the line passing from the head of the femur and the line connecting the middle of the sacral plateau), pelvic incidence (the angle between the perpendicular line drawn to the sacral endplate and the line connecting the midpoint of the sacral plateau and hip axis), and lumbar lordosis showed significant differences. In the patients with AS, pelvic tilt was higher whereas pelvic incidence was lower [9].The authors also stated that these findings indicated a vertical sacrum, posterior deviation of hip, and thus a deviant pelvis position [9]. For normal balance of the spine, pelvic tilt should be smaller than half of the pelvic incidence and the sacral slope should be bigger than half of the pelvic incidence [10]. The results of these studies suggest that the increase in pelvic tilt and decrease in pelvic incidence might have a negative effect on balance (Figure 1).
Figure 1.
Sagittal angular measurements
PI: pelvic incidence; PT: pelvic tilt; SS: sacral slope
Another problem developed by the anteflexion posture that causes the increase in dorsal kyphosis is the restriction of gazing at the opposite side. It is known that this situation causes difficulty in daily activities such as driving, communication, and personal care [8, 11]. According to Bot et al. [8], hip extension and posterior rotation of the pelvis may occur to increase the field of vision.
There are also studies in which technological auxiliary devices were used for assessing balance. There are some studies that were conducted with force platforms [2, 8, 12] and some with balance devices [11, 13] (Table 1). These studies reported an increased incidence of balance disorders in patients with AS compared to healthy subjects, though this difference was not detected in the study by Aydog et al. [11]. The authors reported that the tragus wall distance was an indicator of dorsal kyphosis and advanced disease. The presence of only three patients in whom this distance was more than 30 cm might have affected the results or the spinal postural changes may have been compensated for by the lower extremities as hypothesized previously by Bot et al. [8]. However, in another study conducted with the same model device, only one patient with tragus wall distance longer than 30 cm was included and it was shown that the anteroposteri-or, mediolateral, and mean balance values were all negatively affected [13]. However, the use of different model devices makes it difficult to compare the assessments and analyses between studies.
Table 1.
AS-Balance studies with devices
| Studies | Sawacha et al. [12] | Murray et al. [27] | Batur et al. [28] | Aydog et al. [11] | Vergara et al. [2] | Durmus et al. [13] |
|---|---|---|---|---|---|---|
| Subjects | 12 healthy, 12 AS | 30 AS(mild, moderate, severe) | 34 healthy, 34 AS | 35 healthy, 70 AS | 17 healthy, 16 AS | 50 healthy, 64 AS (tragus to wall distance<15 cm Group I and≥15 cm Group II) |
| Clinical assessment | BASMI, BASDAI, BASFI, manual muscle strength test, ROM | Schober test, tragus to wall, chest expansion | Schober test, hand to ground distance, tragus to wall distance, occiput to wall distance, BASMI, Berg Balance Scale, Functional Reach Test, Lateral Reach Test. | BASMI | BASDAI, BASMI, BASFI, Ankylosing Spondylitis Quality of Life Index (ASQoL), patient global assessment, total and nocturnal back pain scores | BASMI, BASDAI, BASFI, Chest expansion, fingertip-to-floor distance, occiput to wall distance |
| Instrumental assessment | Six cameras stereophotogrammetric system (60–120 Hz, BTS S.r.l., Padova, Italy) synchronized with a Bertec force plate (FP4060-10, 960 Hz) | Sway magnetometry | Kinesthetic Ability Trainer 3000 (KAT-3000, Med-Fit Systems Inc., Fallbrook, CA, USA). Postural sway was calculated by using the Emed®-X (Novel GmbH, Munich, Germany) system | Biodex Stability System (Biodex Medical Systems, Shirley, NY, USA). | Two AMTI force platforms (Model OR6-7; Advanced Mechanical Technologies, Inc, Watertown, MA, USA) for ground reaction forces. VICON motion analysis system (VICON Motion Systems, Oxford, UK,128 Hz) for force plate data | Biodex Stability System (Biodex, Inc., Shirley, NY) |
| Summary result |
|
|
|
|
|
|
AS: ankylosing spondylitis; BASMI: bath ankylosing spondylitis metrology index; BASDAI: bath ankylosing spondylitis disease activity index; BASFI: bath ankylosing spondylitis functional index; ROM: range of motion
Peripheral joints
Postural and structural changes can also be seen in peripheral joints. In a study that examined the characteristics of patients with AS, involvement one or more peripheral joints was detected in 65.7% of patients. It was reported that the vast majority of them were in the lower extremities and that they presented asymmetric patterns. Enthesis may also affect joint structures and are often observed around the Achilles tendon [14]. Although it is suggested that the lower extremity joints may contribute to the preservation of the compensatory balance in relation to changes in the spinal column [8], it should be considered that arthritis and enthesis may occur in the lower extremity joints and this may affect adaptation.
Muscles
Muscle structures are also important in the preservation of posture. Hip and knee joints tend to extend while the ankle joints tend to dorsiflex. When patients with AS were compared with healthy populations, a reduction in the strength of the quadriceps was found in several studies with different methods such as isokinetic tests [15] and quantitative surface electro neuro myography [16]. It is known that there is a tendency for knee flexion and ankle plantar flexion posture in the patients with AS; but plan tarflexor muscle strength reduction was found in an isokinetic test assessment study [17].
Proprioception
Another factor that affects balance is proprioception. In a study with mild AS patients, there was no worsening in the proprioception of the spine as the disease progressed [18]. Çınar et al. [19] reported that a tandem Romberg test with closed eyes was an indicator of proprioception and significant impairment was detected in patients with AS compared to healthy subjects. However, the proprioceptive change may also occur in peripheral joints. In a study conducted with osteoarthritis patients, there was increased impairment in knee proprioception compared to healthy volunteers [20]. It is known that joint effusion has negative effects on proprioception [21]. Although active disease state is often excluded in balance studies of AS, there may be subclinical effusion and degeneration in the peripheral joints.
Vestibular system
There are studies that reported increased frequency of vestibular pathologies in patients with AS, which may be due to an intra labyrinthical autoimmune process or ischemia [22]. In a study that evaluated patients with psoriatic arthritis, which is another typeof spondyloarthritis, the frequency of bilateral symmetrical hearing loss and abnormal vestibular test results were higher than in the control group [23]. However sensorineural dysfunction was shown in vasculitis and diseases in which autoimmune mechanisms are predominant, such as systemic lupus erythematosus [23]; vestibular dysfunction in the patients with spondyloarthritis appears to be a topic that is open to investigation.
Visual system
The visual system provides the strongest support to the vestibular system and even the smallest defects in the visual system can negatively affect balance [24]. The most discussed issue in the literature is the restriction of gaze due to decreased spinal motion in patients with advanced kyphosis and cervical involvement [8].
However, when evaluated in terms of ocular findings, typical ocular involvement in AS is anterior uveitis and mechanical ptosis. Also, superficial epithelial keratitis, episcleritis, scleritis, and corneal ulcer rarely occur. Especially long-lasting and uncontrolled attacks can lead to the spread of inflammation to the posterior segment and to decreases in vision [25].
The effect of visual status on balance in AS has been investigated quite rarely. In a study investigating the effect of visual inputs on the postural control of patients with AS, measurements were taken on a baropodometric platform (FDM-S, Zebris, Germany) in healthy subjects when the eyes were closed and open. The most striking result in the computer-aided measurements was observed in the frequency bandwidth. The increase in frequency bandwidth indicates an increase in the efficacy of posture graphic motor commands, which provide rapid control of oscillations in the foot pressure center. The visual input changes between AS and healthy subjects were similar for almost all parameters but no difference was observed in frequency bandwidth in the anteroposterior direction in the individuals with AS. When the eyes were closed, the oscillations were wide and were low velocity in the anteroposterior direction for healthy subjects, and they were rapid and had high amplitude in the patients with AS. The researchers surmised that the patients with AS were more likely to rely on visual input for sustaining the balance and that there was increased worsening in balance compared to healthy subjects when their eyes were closed [26]. The authors suggested that this change, which occurred without pathology in the central nervous system or visual pathway, could indicate impaired motor control or problems in the feedback mechanisms from lower extremity muscles.
In another study evaluating visual input, visual frontal panel pressure center was increased on the force platform (AMTI, Model OR6-7; Advanced Mechanical Technologies, Inc., Watertown, MA, USA) in patients with AS. The authors suggested that the confidence in visual input may be increased due to the somatosensory or vestibular pathologies in AS patients [2].
In conclusion, AS is a disease that mainly involves axial joints and may also influences other systems. These impairments may have negative effects on balance. Considering that balance may be affected by visual, vestibular, and proprioceptive changes in addition to skeletal muscle structures, more multidimensional studies on the association between AS and balance are needed.
Footnotes
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - A.U., I.S.; Design - A.U., I.S.; Supervision - A.U, I.S.; Resources - A.U., I.S.; Materials - A.U. ; Data Collection and/or Processing - A.U., I.S.; Analysis and/or Interpretation - A.U., ; Literature Search - A.U., ; Writing Manuscript - A.U:, I.S.; Critical Review - A.U., I.S.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Zochling J, van der Heijde D, Burgos-Vargas R, et al. ASAS/EULAR recommendations for the management of ankylosing spondylitis. Ann Rheum Dis. 2006;65:442–52. doi: 10.1136/ard.2005.041137. https://doi.org/10.1136/ard.2005.041129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vergara ME, O’Shea FD, Inman RD, Gage WH. Postural control is altered in patients with ankylosing spondylitis. Clin Biomech. 2012;27:334–40. doi: 10.1016/j.clinbiomech.2011.10.016. https://doi.org/10.1016/j.clinbiomech.2011.10.016. [DOI] [PubMed] [Google Scholar]
- 3.Pompeu JE, Romano RSL, Pompeu SMAA, et al. Static and dynamic balance in subjects with ankylosing spondylitis: literature review. Rev Bras Reumatol. 2012;52:413–6. https://doi.org/10.1590/S0482-50042012000300010. [PubMed] [Google Scholar]
- 4.Sieper J, Rudwaleit M, Baraliakos X, et al. The Assessment of SpondyloArthritis international Society (ASAS) handbook: a guide to assess spondyloarthritis. Ann Rheum Dis. 2009;68:ii1–44. doi: 10.1136/ard.2008.104018. [DOI] [PubMed] [Google Scholar]
- 5.Nichols DS, Glenn TM, Hutchinson KJ. Changes in the mean center of balance during balance testing in young adults. Phys Ther. 1995;75:699–706. doi: 10.1093/ptj/75.8.699. https://doi.org/10.1093/ptj/75.8.699. [DOI] [PubMed] [Google Scholar]
- 6.Fredman ML, Berk BZ. Medikal Management of Geriatric Rehabilitation. Toronto: Rehabilitation Medicine; 1998. pp. 384–420. [Google Scholar]
- 7.Scheffer AC, Schuurmans MJ, van Dijk N, van der Hooft T, de Rooij SE. Fear of falling: measurement strategy, prevalence, risk factors and consequences among older persons. Age Ageing. 2008;37:19–24. doi: 10.1093/ageing/afm169. https://doi.org/10.1093/ageing/afm169. [DOI] [PubMed] [Google Scholar]
- 8.Bot SD, Caspers M, Van Royen BJ, Toussaint HM, Kingma I. Biomechanical analysis of posture in patients with spinal kyphosis due to ankylosing spondylitis: a pilot study. Rheumatology. 1999;38:441–3. doi: 10.1093/rheumatology/38.5.441. https://doi.org/10.1093/rheumatology/38.5.441. [DOI] [PubMed] [Google Scholar]
- 9.Lee JS, Suh KT, Kim JI, Goh TS. Analysis of sagittal balance of ankylosing spondylitis using spinopelvic parameters. Clinical Spine Surgery. 2014;27:94–8. doi: 10.1097/BSD.0b013e31829186c1. https://doi.org/10.1097/BSD.0b013e31829186c1. [DOI] [PubMed] [Google Scholar]
- 10.Özer AF, Kaner T. Omurgada Sagital Denge. J Turk Neurosurgery. 2013;23:13–8. [Google Scholar]
- 11.Aydog E, Depedibi R, Bal A, Eksioglu E, Unlü E, Cakci A. Dynamic postural balance in ankylosing spondylitis patients. Rheumatology (Oxford) 2006;45:445–8. doi: 10.1093/rheumatology/kei192. [DOI] [PubMed] [Google Scholar]
- 12.Sawacha Z, Carraro E, Del Din S, et al. Biomechanical assessment of balance and posture in subjects with ankylosing spondylitis. Journal of neuroengineering and rehabilitation. 2012;9:63. doi: 10.1186/1743-0003-9-63. https://doi.org/10.1186/1743-0003-9-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Durmus B, Altay Z, Ersoy Y, Baysal O, Dogan E. Postural stability in patients with ankylosing spondylitis. Disabil Rehabil. 2010;32:1156–62. doi: 10.3109/09638280903428310. https://doi.org/10.3109/09638280903428310. [DOI] [PubMed] [Google Scholar]
- 14.Aggarwal R, Malaviya AN. Clinical characteristics of patients with ankylosing spondylitis in India. Clin Rheumatol. 2009;28:1199–205. doi: 10.1007/s10067-009-1227-7. https://doi.org/10.1007/s10067-008-1049-z. [DOI] [PubMed] [Google Scholar]
- 15.O’Dwyer T, O’Shea F, Wilson F. Decreased health-related physical fitness in adults with ankylosing spondylitis: a cross-sectional controlled study. Physiotherapy. 2016;102:202–9. doi: 10.1016/j.physio.2015.05.003. https://doi.org/10.1016/j.physio.2015.05.003. [DOI] [PubMed] [Google Scholar]
- 16.Hopkins GO, McDougall J, Mills KR, Isenberg DA, Ebringer A. Muscle changes in ankylosing spondylitis. Rheumatology. 1983;22:151–7. doi: 10.1093/rheumatology/22.3.151. https://doi.org/10.1093/rheumatology/22.3.151. [DOI] [PubMed] [Google Scholar]
- 17.Sahin N, Ozcan E, Baskent A, Karan A, Ekmeci O, Kasikcioglu E. Isokinetic evaluation of ankle muscle strength and fatigue in patients with ankylosings pondylitis. Eur J Phys Rehabil Med. 2011;47:399–405. [PubMed] [Google Scholar]
- 18.Swinkels A, Dolan P. Spinal position sense and disease progression in ankylosing spondylitis: a longitudinal study. Spine (Phila Pa 1976) 2004;29:1240–5. doi: 10.1097/00007632-200406010-00014. https://doi.org/10.1097/00007632-200406010-00014. [DOI] [PubMed] [Google Scholar]
- 19.Çınar E, Akkoç Y, Karapolat H, Durusoy R, Keser G. Postural deformities: potential morbidities to cause balance problems in patients with ankylosing spondylitis? Eur J Rheumatol. 2016;3:5–9. doi: 10.5152/eurjrheum.2015.15104. https://doi.org/10.5152/eurjrheum.2015.15104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hassan BS, Mockett S, Doherty M. Static postural sway, proprioception, and maximal voluntary quadriceps contraction in patients with knee osteoarthritis and normal control subjects. Ann Rheum Dis. 2001;60:612–8. doi: 10.1136/ard.60.6.612. https://doi.org/10.1136/ard.60.6.612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cho YR, Hong BY, Lim SH, et al. Effects of joint effusion on proprioception in patients with knee osteoarthritis: a single-blind, randomized controlled clinical trial. Osteoarthritis Cartilage. 2011;19:22–8. doi: 10.1016/j.joca.2010.10.013. https://doi.org/10.1016/j.joca.2010.10.013. [DOI] [PubMed] [Google Scholar]
- 22.Amor-Dorado JC, Barreira-Fernández MP, Vázquez-Rodríguez TR, Miranda-Filloy JA, Llorca J, González-Gay MA. Benign paroxysmal positional vertigo and clinical test of sensory interaction and balance in ankylosing spondylitis. Otol Neurotol. 2011;32:278–83. doi: 10.1097/MAO.0b013e3182016534. https://doi.org/10.1097/MAO.0b013e3182016534. [DOI] [PubMed] [Google Scholar]
- 23.Amor-Dorado JC, Barreira-Fernandez MP, Pina T, Vázquez-Rodríguez TR, Llorca J, González-Gay MA. Investigations into audiovestibular manifestations in patients with psoriatic arthritis. J Rheumatol. 2014;41:2018–26. doi: 10.3899/jrheum.140559. https://doi.org/10.3899/jrheum.140559. [DOI] [PubMed] [Google Scholar]
- 24.Soyuer F, İsmailoğulları S. Aging and Balance. Turkish journal of cerebrovascular diseases. 2009;15:1–5. [Google Scholar]
- 25.Oltulu R, Erkoç HY, Şatırtav G, Okka M. Clinical course and signs in patients with uveitis associated with ankylosing spondylitis. Dicle Medical Journal. 2013;40:418–21. [Google Scholar]
- 26.De Nunzio AM, Iervolino S, Zincarelli C, et al. Ankylosing spondylitis and posture control: the role of visual input. Biomed Res Int. 2015;2015:948674. doi: 10.1155/2015/948674. https://doi.org/10.1155/2015/948674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Murray HC, Elliott C, Barton SE, Murray A. Do patients with ankylosin spondylitis have poorer balance than normal subjects? Rheumatology. 2000;39:497–500. doi: 10.1093/rheumatology/39.5.497. [DOI] [PubMed] [Google Scholar]
- 28.Batur EB, Karataş GK. Do postural changes affect balance in patients with ankylosing spondylitis? J Rehabil Med. 2017;49:437–40. doi: 10.2340/16501977-2230. [DOI] [PubMed] [Google Scholar]