Abstract
Background: Severe burns have been shown to be a risk factor for developing intra-abdominal hypertension (IAH). Fluid resuscitation practices used in burns management further predispose patients to intra-abdominal hypertension. The mortality associated with IAH in severe burns is estimated to be more than 74.5% once organ dysfunction occurs. Despite 95% of all burns occurring in Low and Middle income countries (LMIC), there is paucity of published data on this topic in sub-Saharan Africa. Objectives: To determine the prevalence, incidence, organ dysfunction and mortality of intra-abdominal hypertension among severe burns patients. Methods: A prospective cohort study was conducted over a 6 months period in the Burns Unit of Mulago National Referral Hospital. Patients of all age groups with burns ≥25% and 20% in adults and children respectively were recruited and followed up for 7 days or until death occurred. Patients with burns older than 48 hours were excluded. The outcome variables were intra-abdominal pressure, organ dysfunction and seven day mortality. Results: Of all the 335 burns patients admitted, 64 patients met the inclusion criteria. The overall prevalence of IAH was 57.8% while the prevalence in the children and adults was 54.5% and 61.3% respectively. The incidence of IAH was 13.1 cases/100 person days with the incidence in adults being twice that of the children. The one week mortality of patients with IAH was 82.6% with the risk of dying being 3.34 (p=0.0035) and seven day survival being less than 50%. Conclusion: One in two patients with severe burns exceeding 20% or 25% in children or adults respectively developed IAH. Adults had a higher prevalence and incidence of IAH. Mortality associated with IAH exceeded 80%.
Keywords: Intra-abdominal hypertension, severe burns, abdominal compartment syndrome, sub-Saharan Africa, Uganda, Africa, outcome, mortality
Introduction
Intra-abdominal hypertension (IAH) has been recognised as a contributor to burns morbidity and mortality. As a result, there is growing interest in the field of intra-abdominal hypertension in severe burns and its impact on patient care and outcome.
Severe burns can cause intra-abdominal hypertension either as a result of the burn eschar on the abdominal wall or as an unwanted consequence of the aggressive fluid resuscitation during the resuscitative phase of burn management [1].
Severe third degree trunk burns result in restrictive thoraco-abdominal eschars which greatly limit the abdominal wall compliance resulting in intra-abdominal hypertension. Aggressive fluid resuscitation regimens especially the Parkland formula often result in excessive fluid administration causing “fluid creep”. This results in excessive fluid extravasation into the peritoneal cavity and as such causes intra-abdominal hypertension [2,3]. The marked inflammatory response to burns affects the peritoneal absorptive capacity as well as leads to bowel oedema further worsening the IAH [4,5].
Intra-abdominal hypertension results in multiple organ dysfunction, often affecting the cardiovascular, renal and respiratory systems [6,7].
The prevalence of IAH has been shown to be as high as 64.7-74.5% in the severely burned patients [1]. The incidence is also as high as 56 cases per 100 person days [8] with an associated mortality of 74.6% once Abdominal Compartment Syndrome (ACS) develops [1].
Despite 95% of all burns occurring in Low and Middle Income Countries (LMIC) [9] and burns being a major contributor to trauma related deaths in Uganda [10] and east Africa [11]. There is paucity of literature on IAH in severe burns especially in sub-Saharan Africa and as a result, there are no standard screening or management protocols in most burns ICUs in the sub-Saharan African region. Current practices in our burns Unit involve crude methods such as abdominal girth measurements and abdominal wall tenseness which carry a sensitivity of less than 40% when combined [12]. Intra-abdominal pressure measurement is affordable and easily adoptable even in low resource settings as demonstrated by studies that have been done in patients undergoing emergency surgery in the East African region [13,14].
The purpose of this study was to determine the prevalence and incidence of IAH and its outcome in the form of organ dysfunction and seven day mortality in patients with severe burns in Mulago Hospital Burns Unit.
Methods
Study setting and design
A prospective cohort study was conducted in Mulago National Referral Hospital (MNRH), burns unit from the 1st August 2016 to 15th January 2017 following approval by the Makerere University College of Health Sciences School of Medicine Research Ethics Committee (Reference number 2016-069). This is the largest burns unit in Uganda with a 50 bed capacity and a 9 bed ICU. It’s the national referral centre for patients with severe burns with an annual admission close to 600 burns patients of which about 120 are severe.
Informed consent was obtained from all the adult patients or parents of children. For children above 7 years of age, assent was obtained.
Study population and participants
Adults were defined as any one 18 years and above while children being anyone below 18 years. All patients with burns exceeding 25% in adults or 20% in children were recruited. Patients with burns older than 48 hours, poly-trauma, morbid obesity or pregnancy were excluded (See Figure 1).
Figure 1.
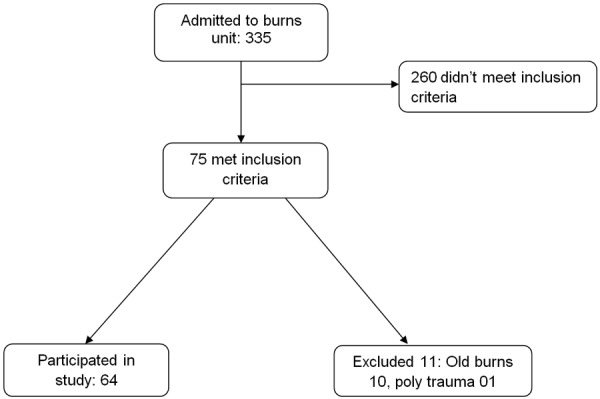
Patient flow chart.
Study variables and study procedure
Once a patient was included and informed consent obtained, they were recruited and followed up for seven days. At admission, demographic data, baseline burn characteristics such as TBSA, degree of burns, presence of inhalation injuries and the presence of a thoraco-abdominal eschar were obtained. Monitoring parameters were also obtained and included a baseline BP, pulse rate, respiratory rate, SPO2, blood samples for electrolytes, kidney function, prescribed fluid volume. The intra-abdominal pressure (IAP) was obtained as the mean of three measurements taken three minutes apart. Intra-abdominal hypertension (IAH) was defined as a reading ≥12 mmHg in adults and ≥10 mmHg in children while Abdominal Compartment Syndrome (ACS) was defined as IAP of ≥20 mmHg or ≥10 mmHg with evidence on new onset organ dysfunction in adults and children respectively. The primary and secondary outcome variables were mortality and organ dysfunction respectively and these were assessed on the seventh day. For mortality, the day death occurred was recorded. Organ dysfunction was defined as in Table 1 below.
Table 1.
Definition of organ dysfunction
| Organ dysfunction (Both) | Parameter 1 | Parameter 2 |
|---|---|---|
| Renal | Creatinine >106 µmol/L | Urine output <25 ml/hr |
| Cardiovascular | MAP <60 mmHg | Heart rate >100/min |
| Respiratory | SPO2 <90% | Respiratory rate >20/min |
| Neurological | Drop of more than 2 points from admission GCS |
Study procedure; Intra-abdominal pressure measurement
The World Society of Abdominal Compartment Syndrome guidelines were followed. An intra-abdominal pressure monitoring system (Unomedical a/s Convatec Company UnoMeterTM Abdo PressureTM ref number 158100110190) was used to measure the intra-abdominal pressure. The intra-abdominal pressure was measured at admission, second day and on the fifth day. The measurements were taken with the patient lying supine on a completely flat bed, the iliac crest junction with the mid axillary line was used as the zero reference point, and the readings taken at the end of expiration after a clear meniscal swing with breathing had been obtained. Three readings three minutes apart were taken and the average reading computed. The first reading was taken 3 minutes following instillation of the saline into the manometer to give ample time to the detrusor spasm reflex to resolve.
Statistical analysis
Statistical analysis was done with STATA version 13.0. The variables were reported as means, percentages with their standard deviations and confidence intervals respectively.
The prevalence was reported as the percentage of patients who had IAH on admission, day two and day five as well as an overall prevalence while the incidence was reported as cases per 100 person days of follow-up.
Mortality of IAH was the proportion of patients with IAH who died during the 7 days of follow up while organ dysfunction was the proportion of patients who had organ dysfunction on the second day and on day seven. The chi-square test was used to determine the relative risk of mortality in IAH. Bivariate analysis was done using chi-square of some predictor variables to assess their relationship with IAH. Significance was set at a p-value <0.05%.
Kaplan-Meier survival analysis was also done to compare survival in the patients that had IAH and those that did not.
Results
Characteristics of the study participants
During the study period, 335 patients were admitted to the burns unit, of these 75 met the inclusion criteria but 11 were excluded. Of those excluded, 10 had burns older than 48 hours and one had poly-trauma. In total of 64 patients were included in this study (See Figure 1). The patients demographic and baseline burn characteristics are summarised in Table 2. The mean age was 16.95 (±15.2) and 33 (51.6%) of these were below the age of 18 years and the average total burn surface area (TBSA) was 43.2% (±20.2).
Table 2.
A table showing the characteristics of the study participants
| Variable | N (percentage) or Mean ± SD |
|---|---|
| Age category | |
| Below 18 years | 33 (51.6) |
| Above 18 years | 31 (48.4) |
| Sex | |
| Female | 29 (45.3) |
| Male | 35 (54.7) |
| Level of education | |
| Primary | 24 (37.5) |
| Secondary | 11 (17.2) |
| Tertiary | 2 (3.1) |
| None | 27 (42.2) |
| Degree of burns | |
| Second degree burns | 10 (15.6) |
| Third degree burns | 18 (28.1) |
| Fourth degree burns | 3 (4.7) |
| Mixed burns | 33 (51.6) |
| Thoraco-abdominal eschar | |
| None | 3 (4.7) |
| Circumferential | 10 (15.6) |
| Partial | 51 (79.7) |
| Total burn surface area | 43.2±20.2 |
| Inhalation burns | 29 (45.3) |
| Nature or agent causing burns | |
| Flame burns | 30 (47.6) |
| Scalds | 28 (44.4) |
| Chemical | 2 (3.2) |
| Electrical | 3 (4.8) |
| Fluid status at 48 hours | N (95% CI) |
| Overloaded | 41.4 (22.3-60.4) |
| Not overloaded | 36.8 (13-60.7) |
Prevalence and incidence of intra-abdominal hypertension
The overall period prevalence of intra-abdominal hypertension was 57.8% with the prevalence in the adults being 61.3% and children being 54.5%. The point prevalence at admission, second day and fifth day was 21.9%, 40.7% and 50% respectively. The point prevalence in the age subgroups is not significantly different (See Table 3).
Table 3.
Prevalence and incidence of intra-abdominal hypertension
| Prevalence | Percentage (95%, CI) | |||||
|
|
||||||
| At admission | Day two | 5th day | Period prevalence | |||
|
| ||||||
| Overall IAH | ||||||
| IAH present | 21.9 (11.5-32.3) | 40.7 (27.2-54.3) | 50 (32.9-67.0) | 57.8 (45.14-69.5) | ||
| Children | ||||||
| IAH present | 15.2 (2.2-28.1) | 40.6 (22.6-58.6) | 50 (26.44-73.56) | 54.5 (36.8-71.2) | ||
| Adults | ||||||
| IAH present | 29 (12.1-46) | 40.9 (18.6-63.2) | 50 (24.96-75.04) | 61.3 (42.4-77.3) | ||
|
| ||||||
| Incidence | N (Cases per 100 person days) | |||||
|
|
||||||
| At day 2 | Between day 2 and 5 | Overall 5 day | ||||
|
| ||||||
| Overall incidence | 17.4 | 4.4 | 13.1 | |||
| Incidence by age group | ||||||
| Children | 16 | 4.8 | 8 | |||
| Adults | 18.9 | 3.97 | 16.7 | |||
The overall incidence of IAH was 13.1 cases per 100 person days. The incidence is higher in the first two days at 17.4 cases per 100 person days but declined over the next five days. In the children’s group, the two day incidence was 16 cases per 100 person days being lower than in the adult group which was at 18.9 cases/100 person days. Overall the incidence is higher in the adults than the children’s group (See Table 3).
Mortality of IAH
The overall mortality of IAH was 82.6% with the mortality in the age sub groups not differing much. See Table 4. A patient with IAH was 3.34 times at risk of mortality as compared to one without IAH (p=0.0035), see Table 5.
Table 4.
Mortality of intra-abdominal hypertension in severe burns
| Variables | Percentage (95%, CI) | |
|---|---|---|
| Overall mortality | 82.6 | 59.7-93.8 |
| Children | 81.8 | 42.0-96.5 |
| Adults | 83.3 | 45.7-96.7 |
Table 5.
The risk of mortality in patients with IAH
| Variable | Died | Alive | Risk ratio | 95% CI | p-value |
|---|---|---|---|---|---|
|
|
|||||
| N | |||||
| Overall IAP | |||||
| IAH | 19 | 18 | 3.34 | 1.25-8.67 | 0.0035 |
| No IAH | 4 | 22 | |||
| Admission IAP | 23 | 40 | |||
| IAH | 10 | 4 | 2.69 | 1.51-4.77 | 0.0021 |
| No IAH | 13 | 36 | 1 | ||
| 2nd day IAP | 14 | 40 | |||
| IAH | 10 | 12 | 3.64 | 1.31-10.13 | 0.0066 |
| No IAH | 4 | 28 | 1 | ||
Footnotes: IAP: Intra-abdominal pressure, IAH: Intra-abdominal hypertension.
Kaplan Meier survival analysis
In Figure 2, survival analysis was done comparing the IAH group against the non IAH group. Overall we see a significantly poor seven day survival in the IAH group of less than 50%. On the contrary the non-IAH group had a far better seven day survival estimate of about 80%.
Figure 2.
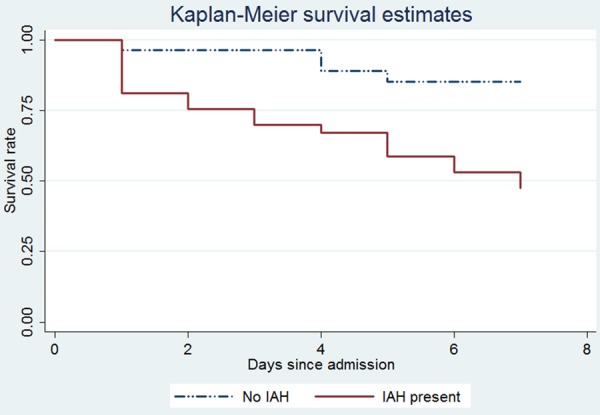
Kaplan Meier survival estimate in relation to the presence or absence of intra-abdominal hypertension.
Organ dysfunction
At day two, the respiratory system had the highest proportion of dysfunction at 26.4% while at 7 days, the most affected was the renal system with 42.2% of the patients having renal dysfunction. The least affected system was the neurological system having only 2% on day two and 1% on day 7. On the second day, 7 (13.2%) patients fitted the description of abdominal compartment syndrome (ACS) while 10% met the criterion for ACS on seventh day.
Overall the risk of a patient with IAH developing organ dysfunction was high. The risk of a patient with IAH at two days developing respiratory and cardiovascular derangements was 2.03 and 2.6 respectively while that of developing renal failure was 1.1 as seen in Table 6. However these values were not statistically significant.
Table 6.
Bivariate analysis of predictor and secondary outcome variables of IAH
| Variable | IAH | No IAH | RR (95% CI) | P value |
|---|---|---|---|---|
| Age | ||||
| Below 18 | 13 | 19 | 0.71 (0.41-1.22) | |
| 18 and above | 13 | 9 | 1 | 0.218 |
| Eschar | ||||
| Present | 21 | 4 | 24.4 (3.5-168.4) | 0.0001 |
| No eschar | 1 | 28 | ||
| Fluids | ||||
| Not overloaded | 10 | 9 | 1 | |
| Overloaded | 16 | 13 | 1.04 (0.61-1.79) | 0.862 |
| Cardiovascular Derangements | ||||
| 48 hours | 4 | 3 | 2.03 (0.5-8.1) | 0.309 |
| 7 days | 2 | 3 | 2.1 (0.39-11.1) | 0.370 |
| Respiratory derangements | ||||
| 48 hours | 8 | 6 | 2.23 (0.79-6.23) | 0.104 |
| 7 days | 2 | 6 | 1.4 (0.41-4.72) | 0.588 |
| Renal derangements | ||||
| 48 hours | 3 | 4 | 1.1 (0.27-4.46) | 0.88 |
| 7 days | 2 | 2 | 2.9 (0.48-17.2) | 0.24 |
| Neurological derangements | ||||
| 7 days | 2 | 2 | 4.2 (0.48-36.56) | 0.15 |
For organ dysfunction at 7 days, the risk of a patient who had IAH at 48 hours developing organ dysfunction at 7 days was 2.1, 1.4, 4.2 and 2.9 for cardiovascular, respiratory, neurological and renal derangements respectively.
In Table 6, bivariate analysis was done for some independent variables and important is the presence of a thoracoabdominal eschar whose risk of developing intra-abdominal hypertension was 24.4 with a p-value of 0.0001. Age (p=0.218) was not shown to have significant impact on development of IAH in our study.
Discussion
We set out to find the prevalence, incidence, organ dysfunction and mortality of intra-abdominal hypertension in patients with severe burns. We found that atleast 1 in 2 patients developed IAH and the mortality of these patients with IAH was high with an associated less than 50% seven day survival.
Prevalence of intra-abdominal hypertension
Our findings concur with existing literature that the prevalence of IAH is high. From Strang’s systematic review which assessed studies from developed countries, the prevalence ranged from 64.7-78% which is slightly higher than our study findings [1]. However Strang’s review only looked at studies in the adult participants. The prevalence in the adult patients in our study was 61.3% which is fairly close to his findings. Another explanation for the higher prevalence in burn centres in developed countries from which his results were obtained could be that these centres potentially save patients who would otherwise not survive in a low resource ICU like our study setting. This being due to the fairly more efficient emergency and referral systems as well as more advanced ICU’s in the developed countries.
Overall, theoretical knowledge states that the children group is at higher risk of developing IAH [1,15] however this has not been backed by evidence as there is no paper comparing the two age groups to the best of my knowledge. Contrary to the above presumption, our findings revealed that there was no significant difference in prevalence of IAH in the children and adult sub-groups.
The prevalence of IAH at admission was far greater in the patients that had abdominal eschars as compared to those without (p=0.0001). This demonstrates the impact of the presence of a thoraco-abdominal eschar and concurs with existing knowledge about its causative role in IAH development.
The prevalence of IAH was also higher among the fluid overloaded patients, being 35% in the patients who got fluid overload in the first 48 hours. This finding as similar to other studies [16,17] and demonstrates that fluid overload in the resuscitative phase predisposes to development of IAH. However the difference from our study wasn’t that significant (p=0.705). This could be due to the small study sample size.
Incidence of intra-abdominal hypertension
The overall five day incidence was 13.1 cases/100 person days. However on stratification for the age subgroups, the incidence was higher in the adults being 16.7 cases per 100 person days. In the children group the incidence was half that of the adult subgroup.
The incidence was highest in the first two days, being 17.4 cases per 100 person days. This concurs with the fact that patients tend to receive aggressive fluid resuscitation in the first two days using the Parkland’s formula.
This IAH that occurs in the subsequent days following admission usually occurs as a component of the phenomenon of “fluid creep” which has been described to occur in severe burns following aggressive fluid resuscitation [2,3].
When compared to other studies, the incidence in our study population is lower. One study reported the incidence to be 56 cases per 100 person days [8] while another reported the cumulative incidence and not the incidence rate [18]. Mechanical ventilation is one risk factor for IAH that was present in the two studies above while in our study, none of the patients were mechanically ventilated. This could explain the lower incidence in our study. Just like prevalence, no prospective study had been done to compare incidence in adults and children groups to the best of my knowledge. From our study, the incidence was highest in the adult population with the incidence in children being half of that of the adults sub-group. This could be explained by the fact that most burns is adults had high burn percentages and deeper burns due to nature of aetiology being flames while the majority of burns in children were scalds causing second degree burns. However the incidence in the subsequent days following the resuscitative period was slightly higher in the children. This could be explained by the fact that children were more likely to receive excess fluid and hence be predisposed to “fluid creep”.
Mortality of intra-abdominal hypertension
The mortality in the IAH group was 82.6% and this did not differ markedly in the age subgroups with a slightly higher mortality in the adults. The findings are similar to findings in other studies where mortality is seen to exceed 71.4% [1,18,19].
Overall, the relative risk of dying if a patient had IAH was 3.34 (p=0.0035) and further demonstrated the significant impact of IAH on mortality in severe burns and concurs with other findings [1,8].
The seven-day survival of patients with IAH is markedly lower than 50% compared to greater than 80% in non-IAH group. This when compared to Wises’ 28 day survival analysis reveals similar findings and further emphasises that IAH has a poor survival whether at seven days or even at longer follow up of 28 days [18].
Organ dysfunction in intra-abdominal hypertension
Organ dysfunction due to intra-abdominal hypertension is varied. Commonly the renal and cardiovascular systems are the most affected [7,8,20]. In our study, the respiratory system was the most affected organ system at 48 hours (26.4%). The presence of IAH markedly reduces the functional residual capacity which results in inadequate ventilation. The risk of developing respiratory dysfunction was twice in IAH patients than in non IAH patients. See Table 6.
On the 7th day, renal dysfunction was the most prevalent organ dysfunction occurring in 57.8% of IAH patients and having a relative risk of 2.9. However these findings were not statistically significant in all the organs. These findings do not differ from other studies which also demonstrated high risk of developing organ dysfunction in patients with IAH however without statistical significance in their findings [8]. This could be due to confounders like inhalational injuries, systemic inflammatory response syndrome and pain all of which can independently affect organ function and could not be stratified against in our study. To correctly diagnose inhalation injuries required bronchoscopy which in our setting wasn’t available and as a result this could have contributed to confounding for respiratory dysfunction.
Strengths and limitations of the study
Our study is the first documented prospective study comparing outcome in children and adults at least to the best of my knowledge. This study also is the first prospective study conducted in low income countries particularly sub-Saharan Africa.
To avoid user bias, only the principal investigator and his research assistant took the measurements.
The limitations included the fact that intra-abdominal pressures were taken on three occasions during the study. That is on admission, day two and day five, skipping day three and four. This does not affect prevalence on the given days but may have had an effect of a lower period prevalence in the follow up period. Secondly studies conducted in high income countries involved continuous monitoring which was most likely more accurate than point measurements as was the case in our study. This may have resulted in under estimation of the prevalence of IAH and could explain why our findings were slightly lower than findings in other centres.
Conclusion
One in two patients with severe burns exceeding 20% or 25% in children or adults respectively developed IAH. Seven day mortality associated with IAH exceeded 80%. Adults were more likely to develop IAH and had a higher mortality than children.
Recommendation
The Burns Unit needs to design protocols for screening, monitoring and management of IAH. Due to the high mortality associated with IAH, interventional studies need to be carried out to assess the available and recommended treatment alternatives.
Acknowledgements
I wish to acknowledge the nursing team of the burns and plastic unit of Mulago Hospital for all the assistance they rendered. I also wish to acknowledge Dr. Luyimbaazi Julius and the staff of Nyakibale hospital for the support offered during preparing this manuscript.
Disclosure of conflict of interest
None.
References
- 1.Strang SG, Van Lieshout EM, Breederveld RS, Van Waes OJ. A systematic review on intra-abdominal pressure in severely burned patients. Burns. 2014;40:9–16. doi: 10.1016/j.burns.2013.07.001. [DOI] [PubMed] [Google Scholar]
- 2.Saffle JI. The phenomenon of “fluid creep” in acute burn resuscitation. J Burn Care Res. 2007;28:382–395. doi: 10.1097/BCR.0B013E318053D3A1. [DOI] [PubMed] [Google Scholar]
- 3.James E, Hayes M, McCabe P, Williams G, Takata M, Vizcaychipi MP. Fluid creep in burn resuscitation: the tide has not yet turned. Critical Care. 2012;16:1–189. [Google Scholar]
- 4.Ivatury R, Diebel L. Intra-abdominal hypertension and the splanchnic bed. Abdominal compartment syndrome. Georgetown: Landes Bioscience. 2006:129–137. [Google Scholar]
- 5.Doty JM, Oda J, Ivatury RR, Blocher CR, Christie GE, Yelon JA, Sugerman HJ. The effects of hemodynamic shock and increased intra-abdominal pressure on bacterial translocation. J Trauma. 2002;52:13–7. doi: 10.1097/00005373-200201000-00005. [DOI] [PubMed] [Google Scholar]
- 6.Berry N, Fletcher S. Abdominal compartment syndrome. Continuing education in anaesthesia. Critical Care & Pain. 2012 [Google Scholar]
- 7.Mohmand H, Goldfarb S. Renal dysfunction associated with intra-abdominal hypertension and the abdominal compartment syndrome. J Am Soc Nephrol. 2011;22:615–21. doi: 10.1681/ASN.2010121222. [DOI] [PubMed] [Google Scholar]
- 8.Ruiz-Castilla M, Barret JP, Sanz D, Aguilera J, Serracanta J, Garcia V, Collado JM. Analysis of intra-abdominal hypertension in severe burned patients: the Vall d’Hebron experience. Burns. 2014;40:719–724. doi: 10.1016/j.burns.2013.09.021. [DOI] [PubMed] [Google Scholar]
- 9.Mock CPM, Peden M, Krug E. Geneva: a WHO plan for burn prevention and care. In World Health Organisation. 2008 [Google Scholar]
- 10.Kobusingye O, Guwatudde D, Lett R. Injury patterns in rural and urban Uganda. Inj Prev. 2001;7:46–50. doi: 10.1136/ip.7.1.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Outwater AH, Ismail H, Mgalilwa L, Justin Temu M, Mbembati NA. Burns in Tanzania: morbidity and mortality, causes and risk factors: a review. Int J Burns Trauma. 2013;3:18–29. [PMC free article] [PubMed] [Google Scholar]
- 12.Cheatham ML, Safcsak K. Intraabdominal pressure: a revised method for measurement. J Am Coll Surg. 1998;186:594–595. doi: 10.1016/s1072-7515(98)00122-7. [DOI] [PubMed] [Google Scholar]
- 13.Kuteesa J, Kituuka O, Namuguzi D, Ndikuno C, Kirunda S, Mukunya D, Galukande M. Intraabdominal hypertension; prevalence, incidence and outcomes in a low resource setting; a prospective observational study. World J Emerg Surg. 2015;10:57. doi: 10.1186/s13017-015-0051-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Muturi A, Ndaguatha P, Ojuka D, Kibet A. Prevalence and predictors of intra-abdominal hypertension and compartment syndrome in surgical patients in critical care units at Kenyatta national hospital. BMC Emerg Med. 2017;17:10. doi: 10.1186/s12873-017-0120-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hobson KG, Young KM, Ciraulo A, Palmieri TL, Greenhalgh DG. Release of abdominal compartment syndrome improves survival in patients with burn injury. J Trauma. 2002;53:1129–1133. doi: 10.1097/00005373-200212000-00016. [DOI] [PubMed] [Google Scholar]
- 16.Oda J, Yamashita K, Inoue T, Harunari N, Ode Y, Mega K, Aoki Y, Noborio M, Ueyama M. Resuscitation fluid volume and abdominal compartment syndrome in patients with major burns. Burns. 2006;32:151–154. doi: 10.1016/j.burns.2005.08.011. [DOI] [PubMed] [Google Scholar]
- 17.Ivy ME, Atweh NA, Palmer J, Possenti PP, Pineau M, D’Aiuto M. Intra-abdominal hypertension and abdominal compartment syndrome in burn patients. J Trauma. 2000;49:387–391. doi: 10.1097/00005373-200009000-00001. [DOI] [PubMed] [Google Scholar]
- 18.Wise R, Jacobs J, Pilate S, Jacobs A, Peeters Y, Vandervelden S, Van Regenmortel N, De Laet I, Schoonheydt K, Dits H, Malbrain ML. Incidence and prognosis of intra-abdominal hypertension and abdominal compartment syndrome in severely burned patients: pilot study and review of the literature. Anaesthesiol Intensive Ther. 2016;48:95–109. doi: 10.5603/AIT.a2015.0083. [DOI] [PubMed] [Google Scholar]
- 19.Sanchez-Sanchez M, Garcia-de-Lorenzo A, Herrero E, Asensio MJ, Galvan B, Cachafeiro L. Prevalence of intra-abdominal hypertension (IAH) among patients with severe burns. Burns. 2014;40:533. doi: 10.1016/j.burns.2013.10.014. [DOI] [PubMed] [Google Scholar]
- 20.Ridings PC, Bloomfield GL, Blocher CR, Sugerman HJ. Cardiopulmonary effects of raised intra-abdominal pressure before and after intravascular volume expansion. J Trauma. 1995;39:1071–1075. doi: 10.1097/00005373-199512000-00010. [DOI] [PubMed] [Google Scholar]


