Abstract
Objectives:
Esophageal instillation of capsaicin enhances secondary peristalsis, but the γ-aminobutyric acid receptor type B (GABA-B) agonist baclofen inhibits secondary peristalsis. This study aimed to investigate whether baclofen could influence heartburn perception and secondary peristalsis subsequent to capsaicin infusion in healthy adults.
Methods:
Secondary peristalsis was performed by slow and rapid mid-esophagus air injections in 15 healthy subjects. Two different sessions including esophageal infusion of capsaicin-containing red pepper sauce (0.84 mg) following pre-treatment with placebo or baclofen were randomly performed to test the effects on heartburn perception and secondary peristalsis.
Results:
The intensity of heartburn symptom subsequent to capsaicin infusion was significantly greater after pre-treatment of baclofen as compared with the placebo (P=0.03). Baclofen significantly increased the threshold volume of secondary peristalsis to slow air injections subsequent to esophageal capsaicin infusion (P<0.001). Baclofen significantly increased the threshold volume of secondary peristalsis to rapid air injections subsequent to esophageal capsaicin infusion (P<0.01). The frequency of secondary peristalsis subsequent to capsaicin infusion was significantly decreased with baclofen as compared with the placebo (P<0.002). Baclofen had no effect on any of the peristaltic parameters of secondary peristalsis subsequent to capsaicin infusion.
Conclusions:
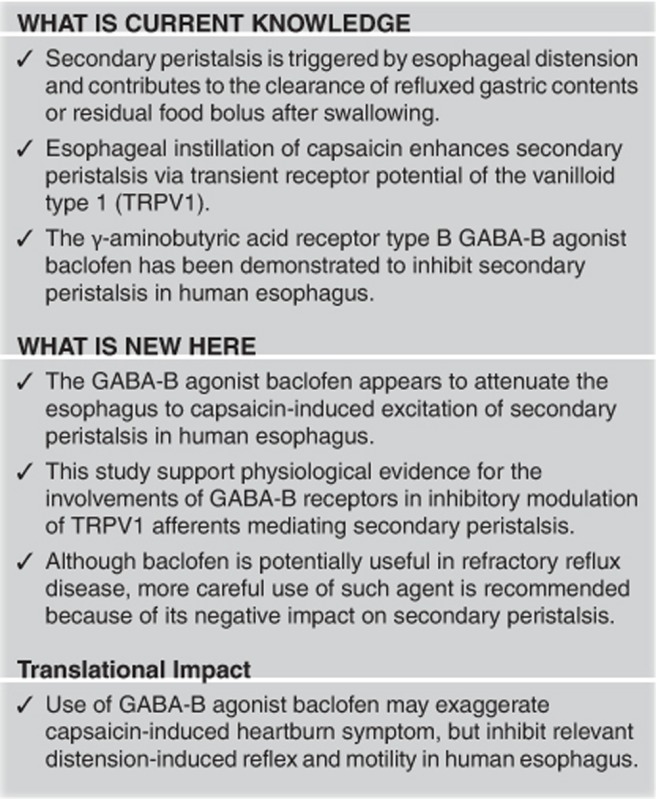
The GABA-B agonist baclofen appears to attenuate the esophagus to capsaicin-induced excitation of secondary peristalsis in healthy adults. Our study suggests the inhibitory modulation for GABA-B receptors on capsaicin-sensitive afferents mediating secondary peristalsis in human esophagus.
Introduction
Secondary peristalsis is triggered by esophageal distension and contributes to maintain esophageal clearance of refluxed gastric contents1 or residual food bolus after swallowing. Secondary peristalsis can be reliably generated by intraesophageal air injection, balloon distension, or water infusion.2 Studies on secondary peristalsis have been well demonstrated regarding its reproducibility, physiological characteristics, and clinical implication.2, 3, 4, 5, 6 Secondary peristalsis in the striated muscle is controlled by central mechanisms with vagal afferents, which in turn leads to sequential vagal efferent discharge to the striated musculature of the proximal esophagus,7 whereas that in the smooth muscle part of the esophagus is mainly controlled by an intrinsic neuromuscular reflex with a purely myogenic contractile origin.8 The triggering of secondary peristalsis depends on a vagal afferent pathway which requires esophageal mucosal and intramuscular mechanoreceptors.9, 10
γ-Aminobutyric acid (GABA) is an important inhibitory neurotransmitter within the central nervous system, and GABA receptors type B (GABA-B) are abundant in both the central and enteric nervous systems.11 Inhibitory GABA-B receptors are located in vagal afferents in the dorsal medulla,11 which can inhibit transmitter release in vagal nuclei.12 The GABA-B receptor agonist baclofen is thought to exert suppression of reflexes controlling respiration13 and gastric relaxation.14 Applying GABA-B receptor agonist inhibits mechanotransduction in primary sensory endings.15 Baclofen has been further demonstrated to inhibit transient lower esophageal sphincter relaxations in animal and human models.16, 17, 18 It has been demonstrated that the GABA-B receptor agonist baclofen, a single 40-mg dose orally, has been further demonstrated to inhibit secondary peristalsis in human esophagus.19
Capsaicin from red pepper has been used for evaluating chemonociception in human and animal studies.20 Its effects are believed to occur by activating the polymodal transient receptor potential of the vanilloid type 1 (TRPV1), which is located on nociceptive afferent neurons21 and can be activated by numerous stimuli.22, 23, 24, 25, 26 Short-term application of capsaicin stimulates the TRPV1 receptor, thereby inducing burning pain, while prolonged capsaicin exposure produces desensitization of sensory neurons and attenuates their sensitivity to noxious stimuli.20 We have shown in human esophagus that activation of TRPV1 receptors enhances mechanosensitivity and contractility of secondary peristalsis.27
Although diverse effects on secondary peristalsis are demonstrated by application of GABA-B agonist baclofen and TRPV1 activation with capsaicin,19, 27 it remains unclear whether GABA-B receptor activation can modulate esophageal heartburn perception and secondary peristalsis subsequent to direct esophageal instillation with capsaicin. The aim of this study was therefore to characterize the effects of GABA-B agonist baclofen on perception of heartburn and distension-induced esophageal reflex subsequent to esophageal capsaicin infusion in healthy volunteers. Specifically, it was hypothesized that acute administration of baclofen may change capsaicin excited sensorimotor characteristics of secondary peristalsis using rapid or slow air esophageal distension.
Methods
Subjects
We studied 15 healthy volunteers (7 women; mean age 26.9, range 21–38 years) enrolled from the community by advertisement. None of the participants had any history of esophageal symptoms or chronic illness. They did not take any prokinetic medication or have frequent consumption of red chili pepper as their diet (at least three times a week) before this study. All the participants gave written informed consent before the study, which was approved by the Research Ethics Committee of Hualien Tzu Chi Hospital, Taiwan.
Esophageal manometry
We recorded intraluminal pressures with a Koenigsberg 4-channel probe with 4.5 mm in diameter (Sandhill Scientific, Highlands Ranch, CO). The manometric assembly was designed with one circumferential solid-state pressure sensor at 5 cm and three unidirectional pressure sensors at 10, 20, and 25 cm from the tip. The infusion port was located in the mid-esophagus between 15 and 20 cm from the tip. The catheter was passed through the nose of fasting subjects in the supine position into the esophagus up to a depth of 60 cm. We performed stationary pull-through technique to allow most distal sensor in the high-pressure zone of the lower esophageal sphincter. Intraluminal pressures were continuously recorded and stored on the computer during the entire study period. Swallowing event was monitored by the most proximal channel of the catheter, which was located in the pharynx for differentiating primary and secondary peristalsis.
Study design
Secondary peristalsis was recorded 10 min after the infusion of capsaicin-containing red pepper sauce on two separate occasions, in which all participants had a pre-treatment (90 min ahead) with oral baclofen (40 mg) and placebo with double-blind in randomized order. Capsaicin-containing red pepper sauce including 5 ml of red pepper sauce (Tabasco; McIIhenny Company, Avery Island, LA), diluted with 15 ml of saline was infused into the mid-esophagus via the manometric catheter at a rate of 10 ml/min. Subjective symptoms (nausea, heartburn, stick, and pain) was evaluated with a visual analog scale score (0–100) shortly after each session of the infusion. The total amount of pure capsaicin included in the infused red pepper sauce suspension (5 ml of Tabasco) was 0.84 mg.27, 28
Secondary peristalsis was performed first by a slow air injection (0.25 ml/s) into the esophagus via an automatic pump connected to the infusion port of the manometric assembly. We determined the amount of volume tested for slow injection of air with the pump machine. Secondary peristalsis was then generated by rapid air injection, in which we started at 1-ml volume and gradually increased the volume by 1-ml increments until the presence of a secondary peristalsis or the injected volume reached 20 ml. The threshold volumes for both slow and rapid air injections were determined as the lowest injection volume for triggering a secondary peristaltic event.29 Then, the frequency of secondary peristalsis and relevant manometric parameters was measured by ten 10 ml boluses of air injections within 0.5 s to determine the effectiveness of secondary peristaltic response (%). The peristaltic response was judged to occur with an interval of 20 s, during which each subject avoided spontaneous swallowing. At the end of 20 s, they were allowed to have a dry swallow to clear any residual air and reduce the desire to swallow before the next distension. The frequency (%) was therefore calculated as the number of secondary peristaltic responses/10 × 100/100.
Data analysis
Secondary peristalsis was considered to be complete if the pressure wave of ≧12 mm Hg was noted in the proximal esophagus and ≧25 mm Hg in the distal esophagus with normal propagation.2 The minimal latency of wave onset between two recording channels was 0.5 s. A failed peristalsis was defined as either a pressure wave of <12 mm Hg in the proximal esophagus or <25 mm Hg in the distal esophagus, or synchronous pressure waves occurring at two or more recording channels. Secondary peristalsis was analyzed in the same manner for during slow and rapid injections.2
Statistical analysis
The normality of all data was evaluated by D'Agostino's K-squared test. All data were expressed with mean±s.e.m. and compared with a paired t-test. Visual analog scale scores of subjective symptoms were determined and compared after capsaicin infusion between baclofen and the placebo. Symptom perception and esophageal threshold volumes of air injected during slow and rapid air injections were compared between baclofen and the placebo. Data for frequency of secondary peristaltic response were analyzed and compared using the Wilcoxon's signed-rank test and were present as median with interquartile range in parentheses. Data for peristaltic wave amplitude and duration of contraction were calculated and compared for middle and distal esophagus. A P value of <0.05 was accepted as indicating statistical significance. Statistical analyses were performed with SPSS 19.0 for Windows (SPSS, Chicago, IL).
Sample size calculation
According to the data that had shown differences in distension threshold volume with intraesophageal air injection19, 27 and esophageal peristaltic amplitudes of secondary peristalsis,19, 27 we determined at least 12 cases were required to achieve a power of 80% and α of 0.05, which is considered as statistically significant difference.
Results
Symptom perception and esophageal sensitivity subsequent to capsaicin infusion after pre-treatment with baclofen vs. the placebo
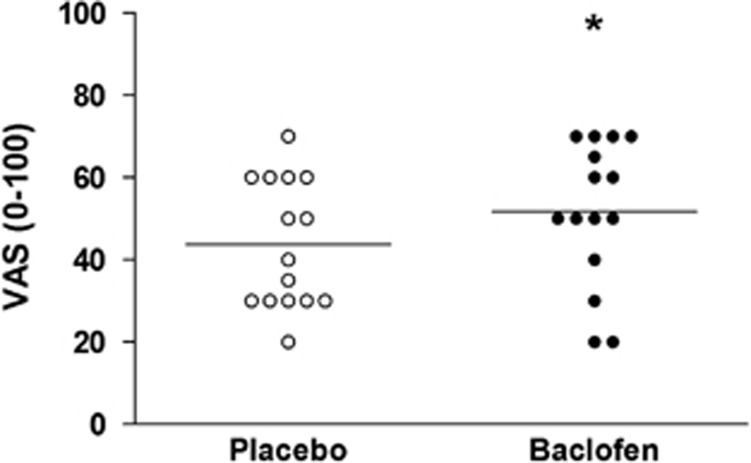
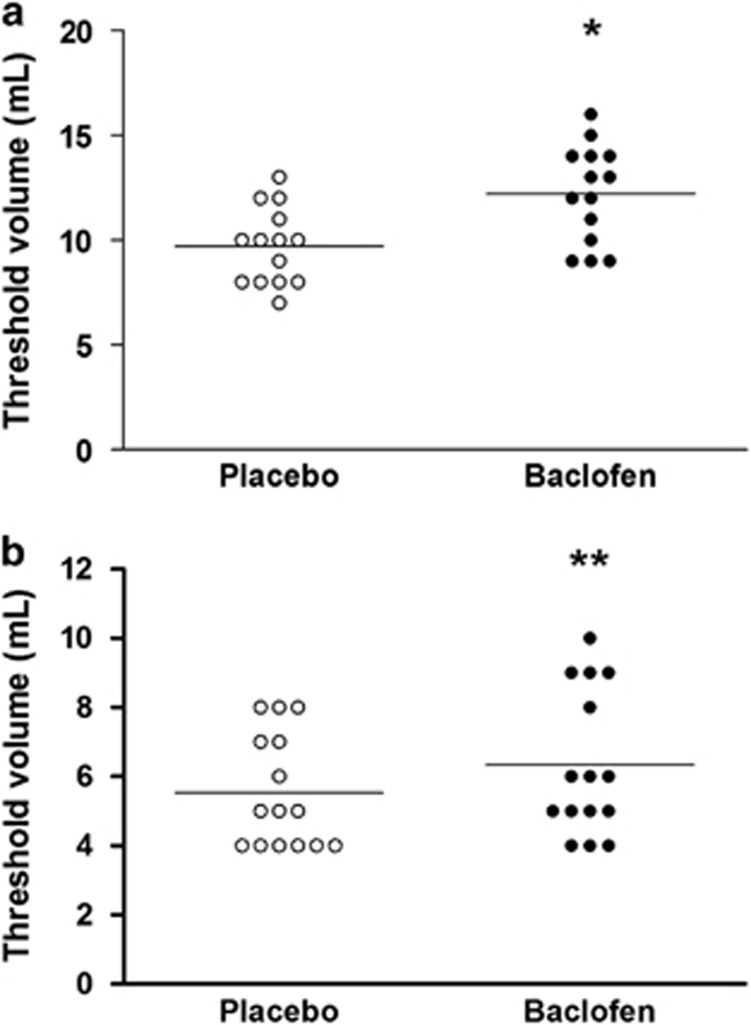
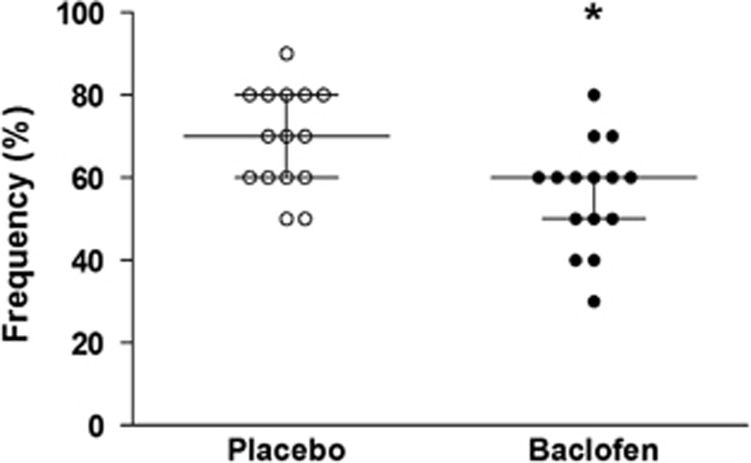
The heartburn symptom scale subsequent to capsaicin infusion was significantly greater after pre-treatment of baclofen as compared with the placebo (52±5 vs. 44±4, P=0.03) (Figure 1). The threshold volume of secondary peristalsis during slow air injection subsequent to capsaicin infusion was significantly increased by pre-treatment with baclofen when compared with the placebo (12.2±0.6 vs. 9.7±0.5 ml, P<0.001) (Figure 2a). Similarly, the threshold volume of secondary peristalsis during rapid air injection subsequent to capsaicin infusion was significantly increased by pre-treatment with baclofen as compared with the placebo (6.3±0.5 vs. 5.5±0.4 ml, P<0.01) (Figure 2b). Compared with pre-treatment with the placebo, the frequency of secondary peristalsis during rapid air injection after capsaicin infusion was significantly decreased by pre-treatment with baclofen (70% (60–80%) vs. 60% (50–60%), P=0.002) (Figure 3).
Figure 1.
Effects of baclofen on heartburn symptom subsequent to capsaicin infusion. The visual analog scale (VAS) score for heartburn symptom as induced by capsaicin infusion was significantly increased after pre-treatment of baclofen when compared with the placebo (*P=0.03). Values are expressed as mean±s.e.m. Line represents the mean value.
Figure 2.
Effects of baclofen on threshold volumes of secondary peristalsis subsequent to capsaicin infusion. (a) The threshold volume of secondary peristalsis subsequent to capsaicin infusion was significantly increased after pre-treatment with baclofen when compared with the placebo during rapid air injection (*P<0.001). (b) The threshold volume of secondary peristalsis subsequent to capsaicin infusion was significantly increased after pre-treatment with baclofen when compared with the placebo during rapid slow injection (**P<0.01). Values are expressed as mean±s.e.m. Line represents the mean value.
Figure 3.
Effect of baclofen on the frequency of secondary peristalsis subsequent to capsaicin infusion. Baclofen significantly decreased the frequency of secondary peristalsis subsequent to capsaicin infusion as compared with the placebo (P=0.002). Values are expressed as median with interquartile range.
Motility characteristics of secondary peristalsis subsequent to capsaicin infusion after pre-treatment with baclofen vs. the placebo
There was no significant difference in the pressure wave amplitude of secondary peristalsis during slow air injection after capsaicin infusion between pre-treatment with baclofen and the placebo (P=0.49, middle; P=0.2, distal) (Table 1). The pressure wave amplitude of secondary peristalsis during rapid air injections was also similar after capsaicin infusion between pre-treatment with baclofen and the placebo (P=0.42, middle; P=0.17, distal) (Table 1). No difference was found in the durations of secondary peristaltic waves during slow or rapid air injection subsequent to capsaicin infusion between pre-treatment with baclofen and the placebo (Table 1).
Table 1. Effects of baclofen on motility parameters of secondary peristalsis subsequent to capsaicin infusion.
|
Slow distension |
P value |
Rapid distension |
P value | |||
|---|---|---|---|---|---|---|
| Placebo | Baclofen | Placebo | Baclofen | |||
| Pressure waves (mm Hg) | ||||||
| Middle | 46.7 (5.3) | 64.8 (13.20) | 0.49 | 58.7 (7.6) | 63.7 (8.3) | 0.42 |
| Distal | 101.2 (6.8) | 97.9 (8.5) | 0.2 | 86.1 (7.3) | 99.8 (9.3) | 0.17 |
| Duration (s) | ||||||
| Middle | 3.5 (0.8) | 2.9 (0.5) | 0.33 | 2.5 (0.2) | 2.5 (0.3) | 0.82 |
| Distal | 3.4 (0.9) | 3.9 (0.8) | 0.68 | 2.9 (0.2) | 2.9 (0.3) | 0.86 |
Discussion
The major findings of this study are that the GABA-B agonist, baclofen, inhibited secondary peristaltic response and increased the threshold volumes of secondary peristalsis subsequent to esophageal capsaicin infusion by both slow and rapid air injections. In addition, the perception of heartburn subsequent to capsaicin infusion appears to be greater after the application of baclofen. Furthermore, baclofen decreased the effectiveness of secondary peristalsis as induced by abrupt air injection. In accordance with prior work,19 baclofen did not change any of peristalsis activities of secondary peristalsis subsequent to capsaicin infusion during either slow or rapid air injection.
In this study, we noticed that subjective perception of heartburn after capsaicin infusion was significantly greater with baclofen than the placebo. In prior study using red pepper sauce containing capsaicin, it was demonstrated that direct intraesophageal instillation of capsaicin with a dose equivalent to 0.84 mg can provoke typical heartburn symptom in non-gastroesophageal reflux disease (GERD) healthy volunteers.27 Our new finding in this work is that baclofen appears to exaggerate the intensity of heartburn symptom after esophageal capsaicin infusion in healthy volunteers. Although previous work has demonstrated inhibitory mechanotransduction within gastroesophageal vagal mechanoreceptors through GABA-B agonist,15 our study may indicate that baclofen may in some way influence the chemosensitivity of mucosa afferents while TRPV1 receptors receive direct activation by capsaicin infusion inside the esophagus.30 The explanation for such finding is yet unclear, but can be possibly attributed to the notion that a recent study has shown that activation of TRPV1 also triggers endogenous GABA release from peripheral nerve endings, which serves as a modulator of nociceptor sensitization in the periphery.31 Consequently, sensitization of TRPV1 by capsaicin has been widely accepted as important characteristics for this receptor,20, 32 but it is still unclear whether the receptor may become further sensitized after the application of baclofen or activation of GABA-B receptors.
In addition to earlier study showing inhibitory effects of GABA-B receptor agonist on esophageal mechanosensitivity in response to distension-induced secondary peristalsis, distension thresholds of secondary peristalsis subsequent to capsaicin were attenuated by baclofen regardless of the type of esophageal stimuli. Inhibitor effects of GABA-B receptors on transmitter release from sensory fibers have been extensively studied. By releasing inhibiting transmitters from central afferent terminals in the spinal cord or medullary vagal nuclei,12, 33 GABA-B receptor agonists are able to inhibit somatomotor,33 respiratory,34 cardiovascular,35 and gastrointestinal reflexes.14 In addition, GABA-B receptors in the periphery have been demonstrated to inhibit transmitter release from intrinsic neurons in the myenteric plexus inside either the gut36 or peripheral axon collaterals of extrinsic primary afferent fibers.37
In this work, most of secondary peristaltic parameters subsequent to capsaicin infusion were comparable between baclofen and the placebo. It is well established that esophageal peristalsis origins from successive contraction of circular muscle in conjunction with longitudinal muscle. Between these muscle layers is myenteric plexus that modulates esophageal peristalsis, which is also influenced by complex interactions among the peripheral muscle part of the esophagus, the enteric nervous system, and central nervous system.38 In addition, motility characteristics of secondary peristalsis are also affected by a number of physiological factors including bolus characteristics and subject position, etc.39, 40, 41 The change in these parameters are therefore likely to be influenced by local neuromuscular reflexes as well as by vagovagal reflexes,38 although activation of GABA-B receptor can decrease acetylcholine release from preganglionic vagal receptors potentiating motor activities.42 Therefore, similar to our previous findings,19 the effect of baclofen on peristaltic parameter of secondary peristalsis subsequent to capsaicin infusion may be limited. Alternately, the activation of GABA-B agonist by baclofen may solely trigger a localized response instead of a complete activation of the whole peristaltic neural pathway together with motility events.
The therapeutic implication of baclofen has been demonstrated in human esophagus with its major advantage in reducing transient lower esophageal sphincter relaxations and increasing lower esophageal sphincter pressure in healthy adults and patients with gastroesophageal reflux disease;18, 43 however, other work failed to show its clinical role in patients with duodenal reflux and associated reflux symptoms despite acid suppression therapy.44 In this work, we demonstrated that baclofen significantly attenuated distension thresholds subsequent to capsaicin infusion with also inhibiting the frequency of secondary peristalsis. The mechanism for current findings is possibly explained by the notion that direct involvement of GABA-B receptors in inhibitory modulation at the sensory receptive field was disclosed by Page et al.,15 who confirmed that GABA-B receptors inhibited mechanotransduction in primary sensory endings. The clinical implication for this study may not support to consider its utility in treating gastroesophageal reflux disease in that baclofen is likely to attenuate esophageal mechanosensitivity relevant to capsaicin exciting secondary peristalsis as induced by abrupt esophageal distension. Moreover, baclofen adversely exaggerates perception of heartburn following capsaicin infusion, which also contradicts previously established clinical role in treating gastroesophageal reflux disease and alleviating reflux symptoms.43 As secondary peristalsis might be important for acid clearance when voluntary swallowing is suppressed,45 our work may support previous findings by suggesting careful use of GABA-B receptor agonists for treating reflux disease in terms of potentially negative impact on secondary peristalsis, especially in patients with significant erosive gastroesophageal reflux disease who are more vulnerable to have impaired secondary peristalsis.5, 46
Our study has some limitations that need to be acknowledged. First, although we have used current dose of baclofen 40 mg to detect the effects of GABA-B receptors activation in vivo for TRPV1 mediating heartburn perception and modulating secondary peristalsis, it remains to be determined whether such dosage is desirable to produce optimal effects for addressing our hypothesis. Second, the manometry with fewer channel in this work is less sensitive than applying high-resolution impedance and manometry for better physiological data of esophageal peristalsis. Finally, the time interval between baclofen administration and capsaicin infusion is of another concern. The time frame we used is based on prior work using 90 min as an interval.19 It is unclear whether ideal time frame for achieving observable effects can be more accurate; however, the findings of the hypothesis are achieved and such concern is less important and beyond our main scope.
In summary, the administration of baclofen attenuates the mechanosensitivity of distension-induced secondary peristalsis subsequent to esophageal excitation with capsaicin infusion. Despite no changes in motility aspects of secondary peristalsis, the administration of baclofen provokes greater heartburn perception relevant to capsaicin infusion in healthy adults without any history of reflux disease. Our study provides novel physiological evidence for the involvements of GABA-B receptors in inhibitory modulation of capsaicin-induced excitation of secondary peristalsis. Although baclofen has been potentially recommended to be useful in a subset of gastroesophageal reflux disease patients with refractory symptoms,47 our work may suggest more careful use of such agent in term of its negative impact on secondary peristalsis.
Study Highlights
Footnotes
Guarantor of the article: Chien-Lin Chen, MD, PhD.
Specific author contributions: Data collection, design of the work, and drafting the work: L.W.Y. and C.L.C.; analysis and interpretation of data: J.S.H., L.T.T., C.H.Y.; approved the final version of the submitted work: all the authors.
Financial support: This study was supported by a grant, TCRD 105-08, from Hualien Tzu Chi Hospital, Buddhist Tzu Chi Medical Foundation, Hualien, Taiwan.
Potential competing interests: None.
References
- Helm JF, Dodds WJ, Pelc LR et al. Effect of esophageal emptying and saliva on clearance of acid from the esophagus. N Engl J Med 1984; 310: 284–288. [DOI] [PubMed] [Google Scholar]
- Schoeman MN, Holloway RH. Stimulation and characteristics of secondary oesophageal peristalsis in normal subjects. Gut 1994; 35: 152–158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pandolfino JE, Shi G, Zhang Q et al. Absence of a deglutitive inhibition equivalent with secondary peristalsis. Am J Physiol Gastrointest Liver Physiol 2005; 288: G671–G676. [DOI] [PubMed] [Google Scholar]
- Schoeman MN, Holloway RH. Secondary oesophageal peristalsis in patients with non-obstructive dysphagia. Gut 1994; 35: 1523–1528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schoeman MN, Holloway RH. Integrity and characteristics of secondary oesophageal peristalsis in patients with gastro-oesophageal reflux disease. Gut 1995; 36: 499–504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sifrim D, Janssens J. Secondary peristaltic contractions, like primary peristalsis, are preceded by inhibition in the human esophageal body. Digestion 1996; 57: 73–78. [DOI] [PubMed] [Google Scholar]
- Hwang K. Mechanism of transportation of the content of the esophagus. J Appl Physiol 1954; 6: 781–796. [DOI] [PubMed] [Google Scholar]
- Paterson WG, Hynna-Liepert TT, Selucky M. Comparison of primary and secondary esophageal peristalsis in humans: effect of atropine. Am J Physiol 1991; 260: G52–G57. [DOI] [PubMed] [Google Scholar]
- Kravitz JJ, Snape WJ Jr., Cohen S. Effect of thoracic vagotomy and vagal stimulation on esophageal function. Am J Physiol 1978; 234: E359–E364. [DOI] [PubMed] [Google Scholar]
- Lang IM, Medda BK, Shaker R. Mechanisms of reflexes induced by esophageal distension. Am J Physiol Gastrointest Liver Physiol 2001; 281: G1246–G1263. [DOI] [PubMed] [Google Scholar]
- Bowery NG, Pratt GD. GABAB receptors as targets for drug action. Arzneimittelforschung 1992; 42: 215–223. [PubMed] [Google Scholar]
- Brooks PA, Glaum SR, Miller RJ et al. The actions of baclofen on neurones and synaptic transmission in the nucleus tractus solitarii of the rat in vitro. J Physiol 1992; 457: 115–129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bolser DC, Aziz SM, DeGennaro FC et al. Antitussive effects of GABAB agonists in the cat and guinea-pig. Br J Pharmacol 1993; 110: 491–495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andrews PL, Bingham S, Wood KL. Modulation of the vagal drive to the intramural cholinergic and non-cholinergic neurones in the ferret stomach by baclofen. J Physiol 1987; 388: 25–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Page AJ, Blackshaw LA. GABA(B) receptors inhibit mechanosensitivity of primary afferent endings. J Neurosci 1999; 19: 8597–8602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blackshaw LA, Staunton E, Lehmann A et al. Inhibition of transient LES relaxations and reflux in ferrets by GABA receptor agonists. Am J Physiol 1999; 277: G867–G874. [DOI] [PubMed] [Google Scholar]
- Lehmann A, Antonsson M, Bremner-Danielsen M et al. Activation of the GABA(B) receptor inhibits transient lower esophageal sphincter relaxations in dogs. Gastroenterology 1999; 117: 1147–1154. [DOI] [PubMed] [Google Scholar]
- Lidums I, Lehmann A, Checklin H et al. Control of transient lower esophageal sphincter relaxations and reflux by the GABA(B) agonist baclofen in normal subjects. Gastroenterology 2000; 118: 7–13. [DOI] [PubMed] [Google Scholar]
- Chen CL, Liu TT, Yi CH. Control of esophageal distension-induced secondary peristalsis by the GABA(B) agonist baclofen in humans. Neurogastroenterol Motil 2011; 23: 612–e250. [DOI] [PubMed] [Google Scholar]
- Holzer P. Capsaicin: cellular targets, mechanisms of action, and selectivity for thin sensory neurons. Pharmacol Rev 1991; 43: 143–201. [PubMed] [Google Scholar]
- Caterina MJ, Schumacher MA, Tominaga M et al. The capsaicin receptor: a heat-activated ion channel in the pain pathway. Nature 1997; 389: 816–824. [DOI] [PubMed] [Google Scholar]
- Hwang SW, Cho H, Kwak J et al. Direct activation of capsaicin receptors by products of lipoxygenases: endogenous capsaicin-like substances. Proc Natl Acad Sci USA 2000; 97: 6155–6160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szallasi A, Di Marzo V. New perspectives on enigmatic vanilloid receptors. Trends Neurosci 2000; 23: 491–497. [DOI] [PubMed] [Google Scholar]
- Tominaga M, Caterina MJ, Malmberg AB et al. The cloned capsaicin receptor integrates multiple pain-producing stimuli. Neuron 1998; 21: 531–543. [DOI] [PubMed] [Google Scholar]
- Trevisani M, Smart D, Gunthorpe MJ et al. Ethanol elicits and potentiates nociceptor responses via the vanilloid receptor-1. Nat Neurosci 2002; 5: 546–551. [DOI] [PubMed] [Google Scholar]
- Zygmunt PM, Petersson J, Andersson DA et al. Vanilloid receptors on sensory nerves mediate the vasodilator action of anandamide. Nature 1999; 400: 452–457. [DOI] [PubMed] [Google Scholar]
- Chen CL, Liu TT, Yi CH et al. Effects of capsaicin-containing red pepper sauce suspension on esophageal secondary peristalsis in humans. Neurogastroenterol Motil 2010; 22: e312–e313. [DOI] [PubMed] [Google Scholar]
- Lee KJ, Vos R, Tack J. Effects of capsaicin on the sensorimotor function of the proximal stomach in humans. Aliment Pharmacol Ther 2004; 19: 415–425. [DOI] [PubMed] [Google Scholar]
- Chen CL, Szczesniak MM, Cook IJ. Oesophageal bolus transit and clearance by secondary peristalsis in normal individuals. Eur J Gastroenterol Hepatol 2008; 20: 1129–1135. [DOI] [PubMed] [Google Scholar]
- Matthews PJ, Aziz Q, Facer P et al. Increased capsaicin receptor TRPV1 nerve fibres in the inflamed human oesophagus. Eur J Gastroenterol Hepatol 2004; 16: 897–902. [DOI] [PubMed] [Google Scholar]
- Hanack C, Moroni M, Lima Wanessa C et al. GABA blocks pathological but not acute TRPV1 pain signals. Cell 2015; 160: 759–770. [DOI] [PubMed] [Google Scholar]
- Szallasi A, Blumberg PM. Vanilloid (capsaicin) receptors and mechanisms. Pharmacol Rev 1999; 51: 159–212. [PubMed] [Google Scholar]
- Capaday C. The effects of baclofen on the stretch reflex parameters of the cat. Exp Brain Res 1995; 104: 287–296. [DOI] [PubMed] [Google Scholar]
- Trippenbach T. Baclofen-induced block of the Hering–Breuer expiratory-promoting reflex in rats. Can J Physiol Pharmacol 1995; 73: 706–713. [DOI] [PubMed] [Google Scholar]
- Silva-Carvalho L, Dawid-Milner MS, Spyer KM. The pattern of excitatory inputs to the nucleus tractus solitarii evoked on stimulation in the hypothalamic defence area in the cat. J Physiol 1995; 487: 727–737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minocha A, Galligan JJ. Excitatory and inhibitory responses mediated by GABAA and GABAB receptors in guinea pig distal colon. Eur J Pharmacol 1993; 230: 187–193. [DOI] [PubMed] [Google Scholar]
- Santicioli P, Tramontana M, Del Bianco E et al. GABAA and GABAB receptors modulate the K(+)-evoked release of sensory CGRP from the guinea pig urinary bladder. Life Sci 1991; 48: PL69–PL72. [DOI] [PubMed] [Google Scholar]
- Park H, Conklin JL. Neuromuscular control of esophageal peristalsis. Curr Gastroenterol Rep 1999; 1: 186–197. [DOI] [PubMed] [Google Scholar]
- Dooley CP, Schlossmacher B, Valenzuela JE. Effects of alterations in bolus viscosity on esophageal peristalsis in humans. Am J Physiol 1988; 254: G8–11. [DOI] [PubMed] [Google Scholar]
- Janssens J, Valembois P, Hellemans J et al. Studies on the necessity of a bolus for the progression of secondary peristalsis in the canine esophagus. Gastroenterology 1974; 67: 245–251. [PubMed] [Google Scholar]
- Janssens J, Valembois P, Vantrappen G et al. Is the primary peristaltic contraction of the canine esophagus bolus-dependent? Gastroenterology 1973; 65: 750–756. [PubMed] [Google Scholar]
- Blackshaw LA IV. GABA<sub>B</sub> receptors in the brain–gastroesophageal axis. Am J Physiol 2001; 281: G311–G315. [DOI] [PubMed] [Google Scholar]
- Zhang Q, Lehmann A, Rigda R et al. Control of transient lower oesophageal sphincter relaxations and reflux by the GABA(B) agonist baclofen in patients with gastro-oesophageal reflux disease. Gut 2002; 50: 19–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koek GH, Sifrim D, Lerut T et al. Effect of the GABA(B) agonist baclofen in patients with symptoms and duodeno-gastro-oesophageal reflux refractory to proton pump inhibitors. Gut 2003; 52: 1397–1402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orr WC, Johnson LF, Robinson MG. Effect of sleep on swallowing, esophageal peristalsis, and acid clearance. Gastroenterology 1984; 86: 814–819. [PubMed] [Google Scholar]
- Holloway RH. Esophageal body motor response to reflux events: secondary peristalsis. Am J Med 2000; 108 (Suppl 4a): 20S–26S. [DOI] [PubMed] [Google Scholar]
- Sifrim D, Zerbib F. Diagnosis and management of patients with reflux symptoms refractory to proton pump inhibitors. Gut 2012; 61: 1340–1354. [DOI] [PubMed] [Google Scholar]