Abstract
Purpose
Determine whether certain patterns of objectively measured physical activity (PA) are associated with the risk factors for or the diagnosis of the metabolic syndrome (MS).
Design
Latent class analysis, including the assessment of the associations between latent PA classes and the risk factors for MS.
Setting
Random sample from throughout the United States (US) using data from 2003–2004 National Health and Nutrition Examination Survey.
Subjects
A total of 3,458 adult, civilian, non-institutionalized US citizens.
Measures
Daily minutes of moderate-to-vigorous PA across a 7-day week, based on accelerometer measurements, as well ashigh blood pressure, blood glucose levels, triglyceride levels, and body mass index, along with low levels of high density lipoproteins, using clinical cut points.
Results
Membership in the more active PA classes was consistently associated with lower odds of all of the risk factors for the MS. However, when participants were categorized into quartiles of the coefficient of variation of PA across 7 days, few differences were seen in any of the risk factors.
Conclusion
Accumulating the total recommended amount of PA for a week is consistently associated with positive health profiles, and more PA than the recommended amounts may suggest. However, the manner in which this activity is accumulated, either spread over most days of the week or compressed into just a couple of days, may have similar associations with the risk factors for the MS.
Keywords: accelerometer, latent class analysis, moderate-to-vigorous physical activity, metabolic syndrome
Indexing Key Words: Format: research, Research Purpose: modeling/relationship testing, Study design: quasi-experimental, Outcome measure: morbidity, Setting: state/national, Health focus: fitness/physical activity, Strategy: policy, Target population age: adults, Target population circumstances: education/ income level and race/ethnicity
Purpose
The last several decades have produced a substantial body of literature indicating the health benefits of physical activity (PA), including reduced risk of all-cause mortality, coronary heart disease (CHD), and CHD risk factors.1 Recent review articles also separate the benefits of physical activity into preventive and palliative effects on disease and disease progression.2, 3 Nevertheless, the prevalence of PA in the United States continues to be suboptimal among most as work and daily activities become more sedentary.4, 5 In 2004, the National Center for Health Statistics reported that 32.2% of adults were obese,6 as defined by a body mass index (BMI) (calculated as weight in kilograms divided by height in meters squared) of 30 or higher. Extreme obesity (BMI ≥ 40.0), which in 1990 only affected 0.5% of men and 1.2% of women, now affects 2.8% of men and 6.9% of women.6, 7
According to the National Cholesterol Education Program’s Adult Treatment Panel III report (ATP III), these two factors (overweight/obesity and physical inactivity), along with genetic factors, are the primary root causes of the metabolic syndrome (MS), which described as a constellation of CHD risk factors of metabolic origin.8 This syndrome and its risk factors have become “a coequal partner to cigarette smoking as contributors to premature coronary heart disease.”8 As such, the ATP III report indicated that treating the MS is one of the most important clinical goals for reducing the risk of CHD, second in importance only to the primary goal of controlling high levels of low density lipoproteins.8
From a clinical perspective, the diagnosis of the metabolic syndrome requires at least three of the following: large waist circumference, low levels of high-density lipoprotein (HDLs), and elevated blood pressure (BP) and triglyceride and fasting glucose levels.8 Congruent with this diagnosis and the importance that PA is believed to play in the development of the syndrome, research articles report negative associations between PA and hypertension, diabetes mellitus, obesity, high triglyceride levels, and low HDL levels, which are components of the clinical definition of the MS.1, 2, 9, 10
Many of these associations, however, may be somewhat transient in nature. For example, higher levels of insulin-mediated glucose uptake have been demonstrated for up to 48 hours after exercise, but the levels return to normal after 5 days.11 Similarly, during bouts of PA, triglycerides are hydrolyzed by lipoprotein lipase into glycerol and fatty acids, which are used as energy for muscle contractions. Lipoprotein lipase activity has been shown to increase during bouts of PA, but this increased activity only lasts up to 48 hours after acute endurance exercise.12 Investigations have also shown that immediately following bouts of exercise there is a reduction in systemic vascular resistance while cardiac output returns to lower levels, leading to periods of hypotension.13 These periods can last for 2 hours among healthy individuals but up to 12 hours among individuals with hypertension.14
Given the relatively short term effects of PA on some of the risk factors for the MS, those who demonstrate regular activity patterns across a 7-day week would be associated cross-sectionally with fewer diagnoses of the MS compared with individuals with irregular activity. Therefore, using 7 days of accelerometer data from the 2003–2004 National Health and Nutrition Examination Survey (NHANES),15 the purpose of this analysis was to use latent class analysis (LCA) to determine the whether certain patterns of objectively measured PA among adults in this sample are disproportionately associated with any of the risk factors for or the diagnosis of the MS.
In LCA analysis, a specified number of classes are requested a priori. Then, LCA finds the requested number of best-fitting underlying activity patterns using the indicators of these classes (in this case, the daily minutes of moderate-to-vigorous PA [MVPA] across 7 days of a week). New developments in LCA methods allow for simultaneous assessment of the associations between these derived patterns of PA and the risk factors for the MS.
Determining whether certain patterns of PA are associated with the MS could help target interventions for individuals who do not accumulate physical activity in an optimal way. For example, while the current recommendations are to be moderately active at least 30 minutes on most, and preferably all days of the week,15, 16 a large portion of the population has employment that requires them to be sedentary for most of the day throughout the workweek. This would potentially allow for greater time during the weekend for activity. If this pattern of PA is insufficient, then interventions incorporating activity during the typical workweek would be important. Conversely, it may be that a significant amount of PA only on the weekend (a “weekend warrior”) is sufficient for desired health benefits. This analysis was thus performed to help fill in these very important gaps in our understanding of the importance of PA.
Because it was unknown a priori what patterns would be found, a secondary analysis was also performed to directly assess the associations between regular PA and the clinical diagnosis of and the risk factors for the MS. Participants were classified into quartiles of the coefficients of variation (CVs) based on their minutes of MVPA across the 7 days. A low CV would indicate that an individual accumulated his or her minutes of MVPA consistently during the week, while a high CV would indicate days of high and low MVPA accumulation, similar to a weekend warrior. The quartiles of CV were then used to assess whether the variation in the accumulated MVPA was associated with the MS.
METHODS
Sample
We analyzed data from the 2003–2004 NHANES, an ongoing health survey with a target population of civilian noninstitutionalized citizens from throughout the United States. The survey consists of two principle components. The first component is an interview, from which the basic demographic information for our present analysis was obtained, including race/ethnicity, gender, education and income levels, and age. In the 2003–2004 NHANES,15 persons with low-incomes, Mexican-Americans, African-Americans, and those aged 12 to 19 years and 60 years or older were oversampled.
The second component of the survey is a physical examination. Most participants agreed to the physical examination, during which the various health measures for our analysis were assessed, including BP, levels of blood lipids and fasting blood glucose, and height and weight for the calculation of BMI. In addition, the 2003–2004 NHANES collected 7 consecutive days of accelerometry measurements among all ambulatory participants 6 years and older who agreed to wear the monitor for a week.
Risk Factors for the MS
For analysis purposes, all of the variables were categorized according to their relevant clinical cut points. Hypertensive status was classified based on the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure.18 Thus, normotensive was based on a systolic BP (SBP) of less than 120 mm Hg and a diastolic BP (DBP) of less than 80 mm Hg. Pre-hypertension was based on a SBP of 120–139 mm Hg or a DBP of 80–89 mm Hg. Hypertension was based on a SBP of 140 mm Hg or higher or a DBP of 90 mm Hg or higher or if the participant was taking medication for hypertension. A fasting blood glucose of 126 mg/dL or higher was considered the clinical cut point for the diagnosis of diabetes mellitus,19 as well as whether the participant was taking insulin or pills for high blood glucose levels. Clinical categories used to classify triglycerides and HDLs were based on the National Cholesterol Education Program’s cut-points.8 Thus, normal triglycerides levels were less than 150 mg/dL, borderline-high triglycerides were 150 to 199 mg/dL, and high triglycerides were 200 mg/dL or higher (or taking medication for high cholesterol). An individual’s HDL level was categorized as low (high risk) if below 40 mg/dL or he or she was taking cholesterol medication. BMI was based on the standard calculation of weight in kilograms divided by standing height in meters squared. According to the cut points published by the National Heart, Blood and Lung Institute,20 BMI was categorized into the following four categories: underweight (<18.5), normal (18.5–24.9), overweight (25–29.9), and obese (≥30). Finally, for the purposes of this analysis, participants were classified as having the MS if they fell into the highest risk category of these of these risk factors.
The analysis software treats the risk factor variables as ordinal, not simply categorical, which we did not feel reflected the true relationship for the associations for the four BMI categories, specifically comparing the odds for the lowest BMI category to the next three higher BMI categories. In addition, because only 42 participants fell into the lightest BMI category, they were excluded, leading to a modeling strategy that we believe was more appropriate given the model assumptions and the sample size requirements needed for the associations between the activity classes and the risk factors.
Measuring PA With Accelerometry
Accelerometers are small, electronic devices that record the acceleration of change of bodily motion either in one dimension (usually the vertical plane), three dimensions, or omnidirectionally. They are particularly useful in measuring physical activity because they eliminate the potential for recall bias, social desirability bias, and are not dependent on literacy. NHANES 2003–200415 used the ActiGraph model 7164 accelerometer (Health One Technology, Fort Walton Beach, Florida) to collect information on participants’ PA. This lightweight uniaxial monitor is a technically reliable instrument, both within and across monitors.21 NHANES15 used 1-minute epochs to assign a “count” value, which is a relative measure of the changes in momentum that occurred during these periods, which may then be translated into an estimate of PA intensity.
Moderate PA Cut Points Based on Calibration Studies
The accelerometer cut point used by this study to translate the count value into an estimate of MVPA was based on a strategy that has been adopted by NHANES researchers.22 This strategy used a weighted average of several cut points that have been published from previous prediction equations for adults.23–26 Each study reported a cut point for MVPA; the cut points were then weighted by their sample size to arrive at an n-weighted average cut point of 2020 counts/min for MVPA.
Accumulating Minutes of MVPA
There are many potential strategies for assigning to an individual a level of PA based on his or her accelerometer data. The present study credited an individual for every minute that their accelerometer registered a count higher than the given 2020 MVPA cut point. Then, for each of the 7 days, a person was assigned a total number of minutes of MVPA.
Imputation of missing daily minutes of MVPA
The NHANES15 accelerometry data was quite complete in terms of the total number of participants (>99.8%) providing all 7 days of data. However, within each day there may be extended periods of zero counts, indicating either a nonwearing period or a period with no detectable movement. Periods consisting of one hour or more of consecutive zeros were treated as missing data. In addition, periods of monitor malfunctioning were also considered missing data (e.g., 10 minutes of identical consecutive nonzero count values). Occasional missing accelerometry data within a participant’s 7-day record was then imputed using the expectation maximization algorithm, an iterative imputation technique which uses the values of an individual’s other, non-missing data as predictors to estimate the expected value of the total minutes of MVPA for each missing segment of time.22
Self-Reported Variables
Gender was recorded at the time of interview, as was age, which was assigned a truncated value of 85 years for those older than 85 years. Race/ethnicity and country of origin questions were recoded into the following categories: (1) Mexican-American, (2) other Hispanic, (3) non-Hispanic black, (4) non-Hispanic white, and (5) other race/ethnicity, including multiracial. Education level was categorized as less than high school, high school or GED, and more than high school. The poverty income ratio was recorded as a ratio of the self-reported family income to the poverty threshold based on family size. The smallest value of zero indicated no family income, while the highest value is truncated at five, indicating a family income at least five times the poverty threshold for family size.
Primary Analysis
Of the 10,122 participants who completed the physical examination during 2003–2004, we excluded those under age 20 based on the previous accelerometer calibration studies for adults, which generally assessed those at least 20 years old or older.24 This left 5041 participants. Not all participants in the physical examination agreed to complete the accelerometer portion of the study, leaving 4252 participants. An additional 450 participants were excluded because they did not provide responses to their education level or household income or because they had no days of valid accelerometer data with which to impute the other, missing days. A lack of valid accelerometer data was caused by either not wearing the accelerometer (indicated by consecutive zeros) or because the accelerometer malfunctioned. This left 3802 participants. In the end, 344 were removed for missing height, weight, HDL levels, or BP, leaving a final population of 3458. For the analysis of triglyceride and fasting blood glucose levels, which were only collected among participants in the morning examination, only 1620 were available for analysis. There were no differences in the distributions of either the sociodemographic characteristics or the relevant risk factors (BP, blood glucose, and BMI) comparing those who sat for the morning examination and those who participated in the afternoon examination (p > .05 for all, χ2 test and t-test).
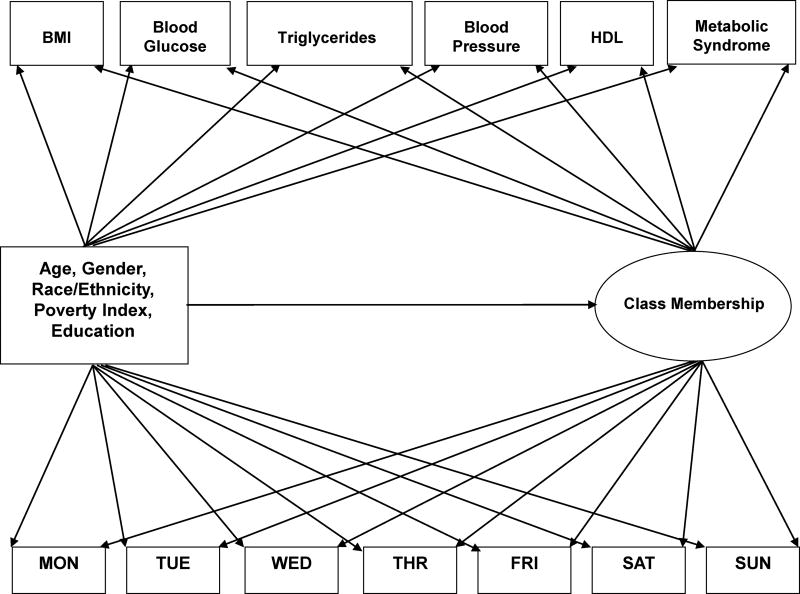
Using the survey procedures of SAS (SAS Institute, Cary, North Carolina), the distribution of each of the risk factors were produced, along with their sample-weighted number, sample weighted percent and SE. Readers may refer to our earlier paper for an in depth description of the statistical foundations of the LCA modeling as well as an overall description of the LCA modeling strategy employed.25 Figure 1 provides a structural equation representation of the model. In this depiction, the latent classes are defined based on the patterns of PA across the 7 days of the week. The sociodemographic characteristics are used to help predict membership in the derived activity classes, and at the same time the sociodemographic characteristics have been allowed to have a direct influence on the indicators of class and the six biological markers of health. Finally, the classes derived from the levels of PA across the 7 days are used as a categorical indicator for predicting the risk factors.
Figure 1.
Structural Equation Model for the Prediction of The Latent Classes of Physical Activity as Well as the Associations Between The Latent Classes and the Risk Factors.
Given this strategy (classes predicting the multiple risk factors), the ordinal variables representing the risk factors are assumed to follow an ordered polytomous logistic regression.26 Thresholds, analogous to intercept parameters, are established above which a subject is assumed to fall into the next higher category of the ordinal variable.27 With this model structure, the exponentiated difference between the thresholds of any two classes may be interpreted as the odds ratio (OR) that a member of one class falls above the ordinal category, compared to the odds that a member of the other class falls above the ordinal category.26,27
The least active class was used as the referent class. Odds ratios for each of the risk factors in each class were calculated with respect to this lowest activity class. The ORs were based on comparing the thresholds of the highest level of each ordinal variable.
Secondary analysis
The current PA recommendations call for 30 minutes of PA on most days of the week.16 Because for the secondary analysis we were primarily interested in whether the regularity of PA is associated with the MS, we only included those participants meeting the current PA recommendations in order to remove the possibility that any associations found would be driven by the underlying level of activity. By defining “most days of the week” as 5 days, then only participants who accumulated at least 150 minutes of MVPA over the 7 days were selected. Critical for this analysis, however, was that we allowed these 150 minutes to be accumulated in any way (e.g. 2 days of 75 minutes of MVPA and not just on days of ≥30 minutes). A total of 1392 participants from the final study population accumulated 150 minutes of PA in this way, while 710 were available for analysis of the triglycerides and 692 for blood glucose because of the reduced population who participated in the morning exam. Finally, 643 were available for the analysis of the MS.
Among this population, participants were classified into quartiles of the CVs based on the minutes of MVPA across the 7 days. The CV quartiles were then regressed on the each of the risk factors, adjusting for the sociodemographic variables, in order to assess whether “how” the participants accumulated their MVPA was associated with the MS or its risk factors.
Results
The frequency distributions of the five risk factors and the metabolic syndrome are given in Table 1. Thirty-four percent of the population was classified as having hypertension or taking medicine for hypertension. Only 6.4% of the population was classified as having high blood glucose or taking medication for blood glucose levels. Roughly one-third of the population fell into each of the three BMI categories, while 26.9% had low HDL levels and 28.3% had high triglycerides levels. Overall, almost 20% of the population was classified as having the MS.
Table 1.
Unweighted Frequency, Sample Weighted Frequency, and Sample Weighted Percentage (SE) Of the Categorized Risk Factors for the Metabolic Syndrome Among the Final Study Population.
| Risk Factors / Metabolic Syndrome | N | Weighted N |
Weighted % |
SE of % |
|---|---|---|---|---|
| JNC 7 Classification of BP with Meds | ||||
| Normal | 1,197 | 81,306,738 | 39.6 | 1.5 |
| Pre-Hypertension | 817 | 54,802,015 | 26.7 | 1.2 |
| Hypertension or medication | 1,444 | 69,175,916 | 33.7 | 1.3 |
| Blood Glucose (mg/dL) | ||||
| < 126 | 1,481 | 192,160,947 | 93.6 | 0.8 |
| >= 126 or insulin or pills | 139 | 13,106,621 | 6.4 | 0.8 |
| BMI (kg/m2) | ||||
| 18.5–24.9 | 1,029 | 65,678,847 | 32.0 | 1.3 |
| 25.0–29.9 | 1,264 | 72,172,568 | 35.2 | 1.4 |
| 30+ | 1,165 | 67,433,254 | 32.8 | 1.4 |
| HDL (mg/dL) | ||||
| ≥ 40 | 2,452 | 150,049,559 | 73.1 | 1.3 |
| < 40 or medication | 1,006 | 55,235,110 | 26.9 | 1.3 |
| Triglycerides (mg/dL) | ||||
| Normal (<150) | 910 | 124,488,133 | 60.6 | 1.8 |
| Borderline High (150–199) | 207 | 22,642,237 | 11.0 | 1.0 |
| High (≥ 200 or medication) | 503 | 58,137,198 | 28.3 | 1.2 |
| Metabolic Syndrome | ||||
| No | 1,250 | 164,408,975 | 80.1 | 1.5 |
| Yes | 370 | 40,858,592 | 19.9 | 1.5 |
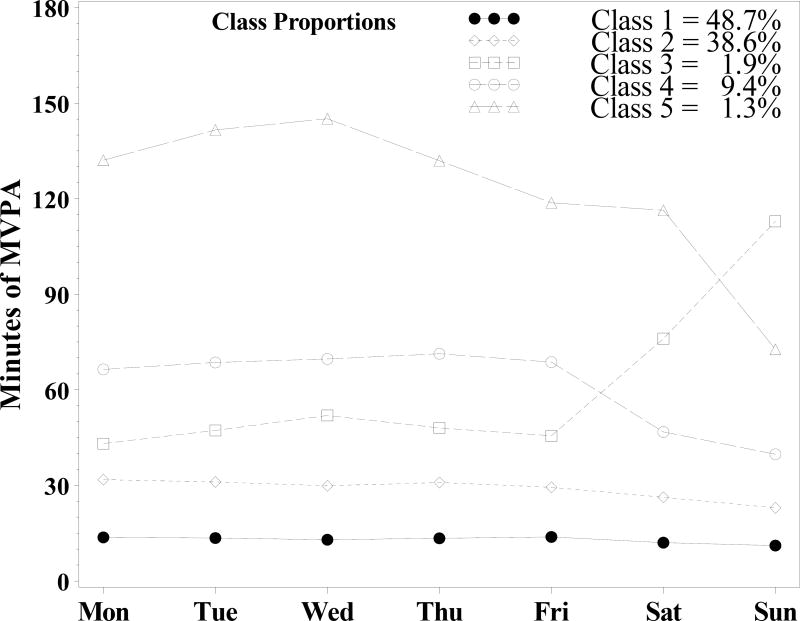
A five-class model was ultimately selected to best represent the statistical and substantive content of this analysis. Figure 2 summarizes the five-class LCA analysis for the larger population with non-missing BMI, HDL levels, and blood pressure. Most of the participants were classified into the two least active classes, representing 87.3% of the population. The most active class averaged 122.6 min/d of MVPA and represented only 1.3% of the population. Class three represents a class with a lower level of PA Monday through Friday but with a substantial increase in PA on the weekend, particularly on Sunday. This class, representing 1.9% of the population, will be referred to as the “weekend warrior”. With the exception of this class, the other four classes all demonstrated a reduction in PA on the weekends, particularly on Sunday.
Figure 2.
Five-Class Latent Class Analysis for Entire Study Population in Which Body Mass Index, High Density Lipoprotein Level, and Blood Pressure Were Available.
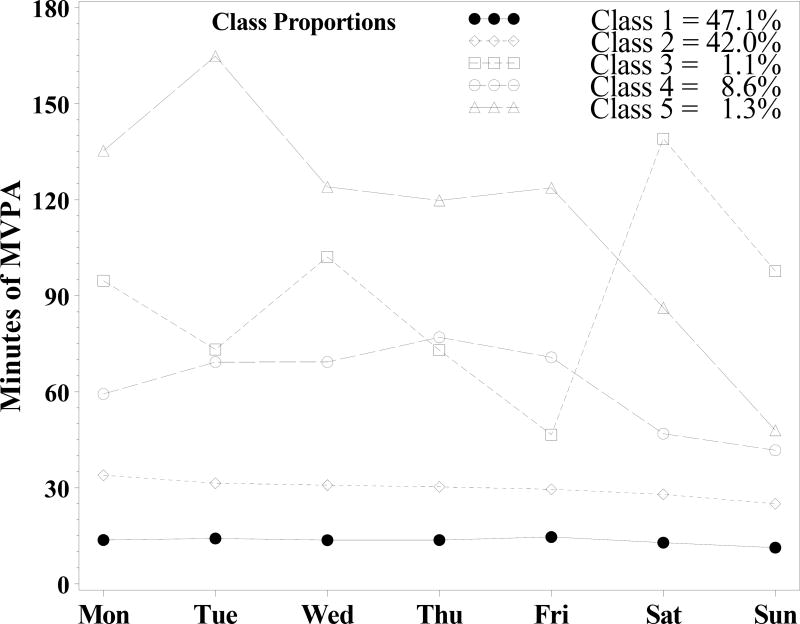
Figure 3 shows the LCA results for the subset of the population in which triglyceride and fasting blood glucose levels were recorded during the morning interview. The patterns for this reduced population were similar in appearance to those in Figure 2, with the exception of class three, which resembles that of the weekend warrior but with substantially more accumulated minutes of MVPA Monday through Thursday. For purposes of comparison, however, this class also will be referred to as the “weekend warrior”, representing 1.1% of the population. Most participants were classified into the two least active classes, representing 89.1% of the population. The most active class again represented 1.3% of the population, and all but the weekend warrior demonstrated a reduction in physical activity on the weekends.
Figure 3.
Five-Class Latent Class Analysis for the Subset of the Population in Which Triglycerides and Fasting Blood Glucose Levels Were Recorded During the Morning Interview.
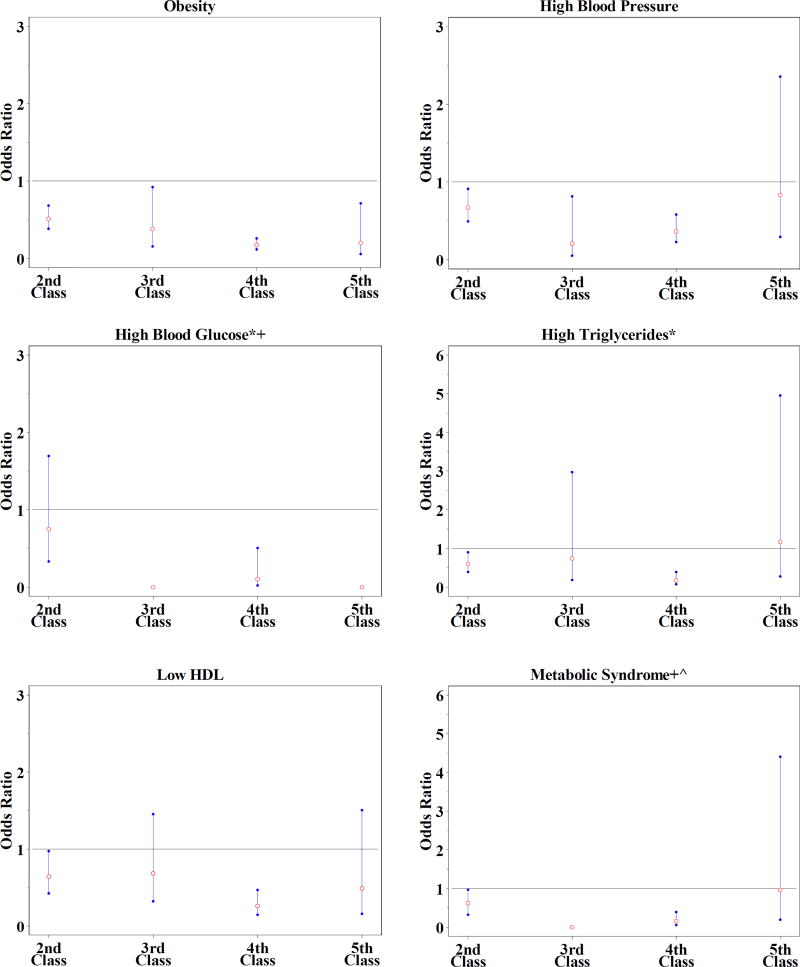
Figure 4 shows the results of the OR associations between the class assignments and the risk factors for the MS comparing the four more active classes with class one, the most sedentary class. The results for the ordinal variables with more than two levels (BMI, BP, and triglycerides) reflect the comparison of the highest level of the risk factor to the lower levels.
Figure 4.
Odds Ratios and 95% Confidence Intervals for Each of the Risk Factors, Comparing the Four More Active Classes With the Least Active Class (Class One).
* Blood glucose and triglycerides were only collected during the morning session of the physical exam, so these analyses represent a subset of the final study population.
+ For fasting blood glucose, no participants had elevated levels in classes three and five; therefore, the odds ratios were zero. No participants had the metabolic syndrome in class three.
^ Analysis represents a subset of the final study population among those with all nonmissing risk factors.
Membership in all of the more active classes led to statistically significantly lower odds of obesity compared to the least active class. This finding was based on a 95% confidence interval (CI) that did not include the null association.
Classes 2 through 4 had significantly lower odds of high blood pressure, with the weekend warrior having nearly one-fifth of the odds compared to the least active class. While the most active class had slightly lower odds of high BP than the least active class, this result was not significant.
Classes two and four had significantly lower odds of having low levels of HDLs, with class four experiencing 26% of the odds of low HDL levels compared with the least active class. The weekend warrior and the most active class both demonstrated lower HDL levels, but neither result was significant based on CIs that included the null.
The blood glucose, triglyceride and MS analyses represented roughly half of the overall study population, causing less stability in the results. No participants in classes three and five experienced high blood glucose, leading to an OR of zero with no variance estimates. Class four experienced significantly lower odds of high glucose levels, odds that were nearly 10% of the odds of the least active class.
Both classes two and four indicated statistically significant lower odds of high triglyceride levels compared to the least active class. The associations between classes three and five and high triglyceride levels were close to the null but had CIs that were very wide, indicating unstable results or imprecise estimates.
Similarly, classes two and four indicated statistically significant reductions in the odds of being classified as having the metabolic syndrome, while class 3 presented no participants with the MS. The OR for class five was very close to the null association with wide CIs.
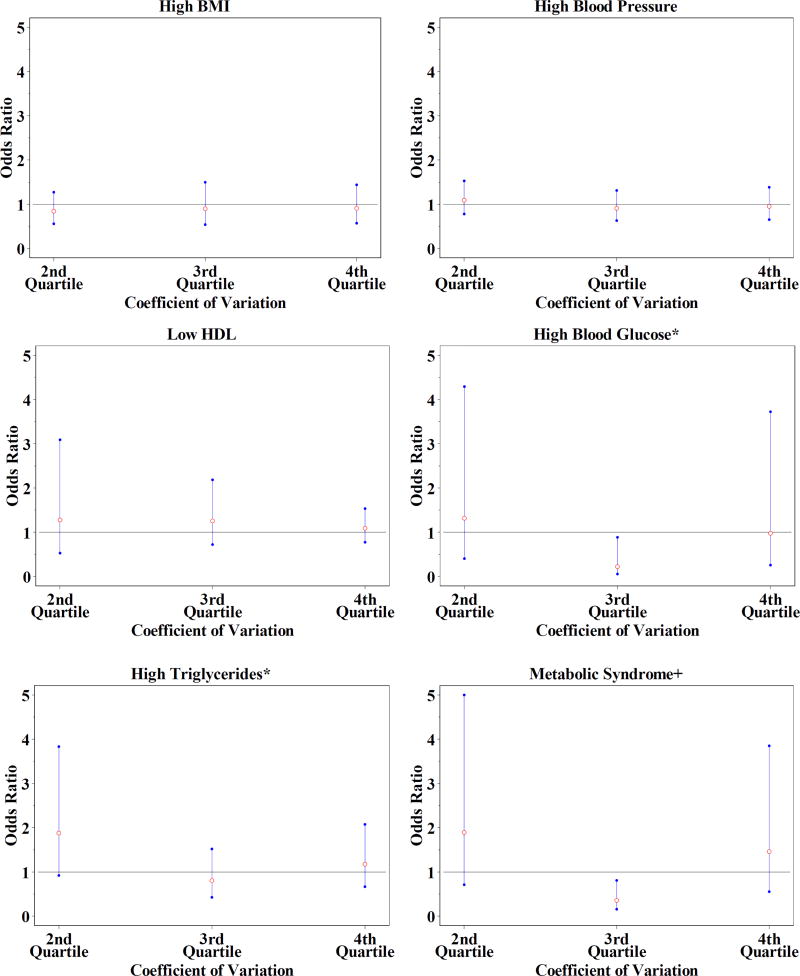
Figure 5 shows the ORs and 95% CIs from the secondary analysis of the risk factors comparing the three higher quartiles of CVs with the lowest quartile of CV, among study participants who achieved at least 150 minutes of MVPA over the 7 days. Body mass index, high BP, and low HDL all demonstrated associations that, for all three quartiles of CVs, were very near the null association compared to the lowest quartile of CV. For high blood glucose, only the third quartile of CV demonstrated lower odds compared to the first quartile, while the second and fourth quartiles of CV had ORs very near the null, with wide CIs, compared to the lowest quartile of CV. The ORs for high triglyceride levels were farther from the null, but all three quartiles included the null association compared to the lowest quartile of CV. Finally, the ORs for the MS demonstrated the third quartile of CV with lower odds compared to the first quartile, while the second and fourth quartiles had ORs somewhat above the null but with wide CIs.
Figure 5.
Odds Ratios And 95% Confidence Intervals for the Secondary Analysis of the Risk Factors, Comparing the Three Higher Quartiles of The Coefficients of Variation With the Lowest Quartile of the Coefficient of Variation Among Study Participants Who Achieved at Least 150 Minutes of Moderate-to-Vigorous Physical Activity During the 7 Days.
* Blood Glucose and Triglycerides were only collected during the morning session of the physical exam, so these analyses represent a subset of the final study population.
+ Analysis represents a subset of the final study population among those with all non-missing risk factors.
Discussion
For the first time to our knowledge, objectively measured PA data sampled from throughout the United States has been analyzed to determine the patterns of PA across a 7-day week, while simultaneously examining the associations between these patterns and several biological markers of health. The primary observation from the analysis of the five PA classes is that, in nearly all cases, the four more active classes were associated with lower odds of the five risk factors and the metabolic syndrome itself compared to the most sedentary class. The one exception was the association between class five and triglyceride levels, although even this result was close to the null and had a very wide CI. The consistency of these results across the various risk factors provides encouraging evidence of the potential benefits of PA.
Classes two and four comprised roughly 40% and 9% of the population, respectively, and produced point estimates which were much more stable than those produced for classes three and five which composed 1.9% and 1.3% of the larger population, respectively. Comparing only these two larger classes, class four had notably lower odds of all of the risk factors compared to class two, and class two had significantly lower odds of all of the risk factors compared to the least active class, indicating a consistent dose response relationship. This is important because class two represents a class of which most participants would meet the PA recommendations of 30 minutes of PA on most days of the week. Nevertheless, these results indicate that participating in PA at roughly twice this recommended amount may be associated with lower odds of being classified with any of the risk factors used in this study.
A recent article has attempted to assess the effect of the weekend warrior activity pattern on the risk of mortality.28 In this study, the mortality outcomes of the weekend warrior, defined as those who accumulate a large quantity of PA (≥ 1000 kcal/wk) over a short period of time (1–2 d/wk), were compared to those who accumulate a similar amount of activity over a longer period of time (≥3 d/wk), along with those who are insufficiently active (500–999 kcal/wk) or sedentary (<500 kcal/wk). Among low-risk men, weekend warriors demonstrated the lowest relative risk of mortality, while among high risk men only the regularly active showed improved mortality risks as compared to the most sedentary group.
In the present study, comparing classes three and four represents a similar assessment. Class three, the weekend warrior, accumulated a large portion of their minutes during the weekend, while class four accumulated a consistently larger amount of activity Monday through Friday, with a reduction on the weekend. For obesity, low HDL, and high triglycerides, the weekend warrior had higher odds compared to class four, while the weekend warrior had lower odds of high BP and blood glucose levels and the MS. However, the small sample size for the weekend warrior makes these comparisons tenuous. Thus, it is unclear from this analysis whether an individual benefits to a greater degree from a consistently active daily lifestyle or from a highly active weekend lifestyle.
The secondary analysis resolved some of the problems related to small class sizes. In this analysis, no association was observed between the amount of variation in the accumulation of PA over a 7-day week and the respective risk factors, with the exception of the third quartile’s association with significantly lower blood glucose levels and the MS. These results in combination with the previous results present a relatively consistent picture that meeting the recommendations for physical activity is indeed associated with lower odds of all of the biological markers related to the MS (i.e. BP, triglyceride and blood glucose levels, HDL, BMI as well as the syndrome itself). It may also be that more PA may be better. However, among those participants who met the minimum requirement for total PA in a week, acquiring PA consistently over the week had associations with all of the risk factors that were similar to acquiring PA erratically. For example, two days in which 75 minutes of MVPA are accumulated may lead to similar benefits as 30 minutes of MVPA spread over 5 days.
The lack of association between the quartiles of CVs and any of the risk factors for the MS was interesting given our initial hypothesis. Among individuals who were regularly active, the cross-sectional assessment should have had a higher probability of sampling during a post-activity period compared to those who were irregularly active. As such, the postexercise reductions in certain measures, including BP, and blood glucose and triglyceride levels, might have been apparent in the OR analyses, but in this case were not. One possible explanation is that, while PA is known to affect all of the relevant risk factors, it may not affect classification according to the clinical cut points used in this study. Another possibility is that there was some non-random selection for when participants were assessed (i.e. those who were irregularly active chose to be assessed on the day that they also set aside for PA). Another possibility is that the sample size was insufficient to adequately assess associations that were small in magnitude.
This study has many strengths worth noting. The present work represents the first LCA analysis (to our knowledge) that uses objectively measured, nationally representative PA data sampled from across the United States to assess the associations between patterns of PA and several biological markers of health. Structuring the analysis around those factors believed to be associated with the MS helped present a clearer view of how PA may influence the risk factors for cardiovascular disease. The five classes provided a potent indicator of overall activity level by capturing many important aspects of physical activity including frequency, intensity and time at or above the moderate-to-vigorous intensity level. For analysis purposes, therefore, this data reduction very concisely captures many of the important aspects needed to adequately assess the associations between PA and health status. A large study population led to many statistically significant and clinically meaningful results. The secondary analysis provided an important contribution to the understanding of whether the overall health benefits received from physical activity are altered by “how” it is accumulated.
The primary weakness of this study is that the data were collected cross-sectionally. As such, the results (while compelling) may only be viewed as associations between PA and the various risk factors. While effort was made to control for potential sociodemographic confounders, residual confounding may still be the source of the observed associations.
Accelerometers do not capture all types of PA, particular static activities such as raking leaves or riding a bike.24 Therefore, while the present analyses do not rely on self-report, they may still not reflect a complete picture of the activity levels of the U.S. population. Similarly, the cut-points for what constitutes MVPA are also sensitive to the types of activities being performed. Changing these cut points would affect the amount of physical activity that participants were credited for, which in turn could have affected the outcome of the LCA.
SO WHAT? Implications for Health Promotion Practitioners and Researchers
These results indicate that accumulating the total amount of PA recommended for a week is consistently associated with positive profiles of the biological risk factors related to the MS, and that accumulating substantially more PA than what the recommendations suggest may be even better. However, the manner in which PA is accumulated, either spread over many days of the week or compressed into just a couple, may have similar associations with the risk factors for the MS as well as the syndrome itself.
Acknowledgments
This research was supported by the National Institutes of Health Grant NIDDK 56350 award to the Department of Nutrition's Clinical Nutrition Research Center.
References
- 1.Physical activity and cardiovascular health. NIH Consens Statement. 1995;13(3):1–33. [PubMed] [Google Scholar]
- 2.Grundy SM, Blackburn G, Higgins M, Lauer R, Perri MG, Ryan D. Physical activity in the prevention and treatment of obesity and its comorbidities: evidence report of independent panel to assess the role of physical activity in the treatment of obesity and its comorbidities. Med Sci Sports Exerc. 1999;31(11):1493–1500. doi: 10.1097/00005768-199911000-00001. [DOI] [PubMed] [Google Scholar]
- 3.DiPietro L. Physical activity in the prevention of obesity: current evidence and research issues. Med Sci Sports Exerc. 1999;31(11 suppl):S542–546. doi: 10.1097/00005768-199911001-00009. [DOI] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention (CDC) Trends in leisure-time physical inactivity by age, sex, and race/ethnicity: United States, 1994–2004. MMWR Morb Mortal Wkly Rep. 2005;54(39):991–994. [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention (CDC) Adult participation in recommended levels of physical activity: United States, 2001 and 2003. MMWR Morb Mortal Wkly Rep. 2005;54(47):1208–1212. [PubMed] [Google Scholar]
- 6.Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999–2004. JAMA. 2006;295(13):1549–1555. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- 7.Freedman DS, Khan LK, Serdula MK, Galuska DA, Dietz WH. Trends and correlates of class 3 obesity in the United States from 1990 through 2000. JAMA. 2002;288(14):1758–1761. doi: 10.1001/jama.288.14.1758. [DOI] [PubMed] [Google Scholar]
- 8.National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002;106(25):3143–3421. [PubMed] [Google Scholar]
- 9.American College of Sports Medicine and American Diabetes Association joint position statement: Diabetes mellitus and exercise. Med Sci Sports Exerc. 1997;29(12):i–vi. [PubMed] [Google Scholar]
- 10.Bassuk SS, Manson JE. Physical activity and the prevention of cardiovascular disease. Curr Atheroscler Rep. 2003;5(4):299–307. doi: 10.1007/s11883-003-0053-7. [DOI] [PubMed] [Google Scholar]
- 11.Mikines KJ, Sonne B, Farrell PA, Tronier B, Galbo H. Effect of physical exercise on sensitivity and responsiveness to insulin in humans. Am J Physiol. 1988;254(3 Pt 1):E248–259. doi: 10.1152/ajpendo.1988.254.3.E248. [DOI] [PubMed] [Google Scholar]
- 12.Dishman RK, Washburn RA, Heath G, Kaplan RL, Kaplan BH. Physical activity epidemiology. Champaign, IL: Human Kinetics; 2004. [Google Scholar]
- 13.Halliwill JR. Mechanisms and clinical implications of post-exercise hypotension in humans. Exerc Sport Sci Rev. 2001;29(2):65–70. doi: 10.1097/00003677-200104000-00005. [DOI] [PubMed] [Google Scholar]
- 14.Kenney MJ, Seals DR. Postexercise hypotension. Key features, mechanisms, and clinical significance. Hypertension. 1993;22(5):653–664. doi: 10.1161/01.hyp.22.5.653. [DOI] [PubMed] [Google Scholar]
- 15.Centers for Disease Control and Prevention. National Helath and Nutrition Examination Survey, 2007–2008 Overview. Atlanta, Ga: Centers for Disease Control and Prevention; 2008. [Google Scholar]
- 16.Pate RR, Pratt M, Blair SN, et al. Physical activity and public health: a recommendation from the Centers for Disease Control and Prevention and the American College of Sports Medicine. JAMA. 1995;273(5):402–407. doi: 10.1001/jama.273.5.402. [DOI] [PubMed] [Google Scholar]
- 17.United States. Physical activity and health: a report of the Surgeon General. Atlanta, Ga: Centers for Disease Control and Prevention, US Dept of Health and Human Services; 1996. Public Health Service, Office of the Surgeon General, National Center for Chronic Disease Prevention and Health Promotion (U.S.), President's Council on Physical Fitness and Sports (U.S.) [Google Scholar]
- 18.Chobanian AV, Bakris GL, Black HR, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289(19):2560–2572. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 19.American Diabetes Association/American College of Cardiology. Redefining diabetes control. Diabetes Cardiovasc Dis Rev. 2001;1:1–8. [Google Scholar]
- 20.Expert Panel on the Identification, Evaluation, and Treatment of Overweight in Adults. Am J Clin Nutr. 1998;68(4):899–917. doi: 10.1093/ajcn/68.4.899. [DOI] [PubMed] [Google Scholar]
- 21.Metcalf BS, Curnow JS, Evans C, Voss LD, Wilkin TJ. Technical reliability of the CSA activity monitor: The EarlyBird Study. Med Sci Sports Exerc. 2002;34(9):1533–1537. doi: 10.1097/00005768-200209000-00022. [DOI] [PubMed] [Google Scholar]
- 22.Berrigan D, Troiano R, Schmitz K. Physical Activity Measured by Accelerometry in that National Health and Nutrition Examination Survey 2003–2004. Paper presented at: Fourth Active Living Research Annual Conference; February 22, 2007; Coronado, Calif. [Google Scholar]
- 23.Catellier DJ, Hannan PJ, Murray DM, et al. Imputation of missing data when measuring physical activity by accelerometry. Med Sci Sports Exerc. 2005;37(11 Suppl):S555–562. doi: 10.1249/01.mss.0000185651.59486.4e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Matthew CE. Calibration of accelerometer output for adults. Med Sci Sports Exerc. 2005;37(11 Suppl):S512–522. doi: 10.1249/01.mss.0000185659.11982.3d. [DOI] [PubMed] [Google Scholar]
- 25.Metzger JS, Catellier DJ, Evenson KR, Treuth MS, Rosamond WD, Siega-Riz AM. Patterns of Objectively Measured Physical Activity in the United States. Med Sci Sports Exerc. 2008;40(4):630–638. doi: 10.1249/MSS.0b013e3181620ebc. [DOI] [PubMed] [Google Scholar]
- 26.Muthen BO. MPlus Technical Appendices. Los Angeles, CA: Muthen & Muthen; 1998–2004. [Google Scholar]
- 27.Agresti A. Categorical data analysis. New York: Wiley; 1990. [Google Scholar]
- 28.Lee IM, Sesso HD, Oguma Y, Paffenbarger RS., Jr The "weekend warrior" and risk of mortality. Am J Epidemiol. 2004 Oct 1;160(7):636–641. doi: 10.1093/aje/kwh274. [DOI] [PubMed] [Google Scholar]