Abstract
Several lines of evidence indirectly suggest that antigenic stimulation through the B‐cell receptor (BCR) supports chronic lymphocytic leukemia (CLL) development. In addition to self‐antigens, a number of microbial antigens have been proposed to contribute to the selection of the immunoglobulins expressed in CLL. How pathogen‐specific BCRs drive CLL development remains, however, largely unexplored. Here, we utilized mouse models of CLL pathogenesis to equip B cells with virus‐specific BCRs and study the effect of antigen recognition on leukemia growth. Our results show that BCR engagement is absolutely required for CLL development. Unexpectedly, however, neither acute nor chronic exposure to virus‐derived antigens influenced leukemia progression. Rather, CLL clones preferentially selected light chains that, when paired with virus‐specific heavy chains, conferred B cells the ability to recognize a broad range of autoantigens. Taken together, our results suggest that pathogens may drive CLL pathogenesis by selecting and expanding pathogen‐specific B cells that cross‐react with one or more self‐antigens.
Keywords: autoantigens, B‐cell receptor, chronic lymphocytic leukemia, infection, light chains
Subject Categories: Cancer, Haematology, Immunology
Introduction
Chronic lymphocytic leukemia (CLL), the most common adult leukemia in the Western World, is characterized by the clonal expansion of CD5+ B cells in blood and peripheral tissues (Zhang & Kipps, 2014). BCR signaling plays a critical role in CLL pathogenesis (Burger & Chiorazzi, 2013), and, accordingly, inhibitors targeting BCR‐associated kinases [Bruton's tyrosine kinase (BTK), phosphoinositide 3‐kinase (PI3K) δ] have shown great clinical efficacy in patients (Burger & Chiorazzi, 2013; Furman et al, 2014).
Patient‐derived CLL cells with either unmutated or mutated immunoglobulin genes often express similar, if not identical, BCRs with common stereotypic features and/or structural similarities (Burger & Chiorazzi, 2013; Stevenson et al, 2014; Zhang & Kipps, 2014). This marked restriction in the immunoglobulin gene repertoire of CLL cells suggests that binding to restricted sets of antigenic epitopes is key to the selection and the expansion of those normal B‐cell clones that eventually enter the CLL pathogenic process (Burger & Chiorazzi, 2013; Stevenson et al, 2014; Zhang & Kipps, 2014). The nature of such antigens and the mechanisms of BCR stimulation during CLL remain, however, incompletely understood. The majority of unmutated CLLs express low‐affinity BCRs that are polyreactive to several autoantigens (Burger & Chiorazzi, 2013; Stevenson et al, 2014; Zhang & Kipps, 2014). The BCR specificity of mutated CLLs is less characterized, although a number of self‐antigens, as well as microbial or virus‐associated antigens, have been identified (Zhang & Kipps, 2014). Indeed, epidemiological studies indicate that several infections are associated with CLL development and CLL‐associated immunoglobulins are known to react with various viruses and other pathogens (Landgren et al, 2007; Lanemo Myhrinder et al, 2008; Kostareli et al, 2009; Steininger et al, 2009, 2012; Hoogeboom et al, 2013; Hwang et al, 2014). If and how pathogen‐specific BCRs drive CLL development and progression is largely unexplored.
Results and Discussion
To begin addressing these issues, we took advantage of a well‐established CLL mouse model, the Eμ‐TCL1 transgenic mouse, where the oncogene Tcl1 is expressed in both immature and mature B cells (Bichi et al, 2002). As such, Eμ‐TCL1 transgenic mice develop a lymphoproliferative disorder that entails the clonal expansion of CD5+ IgM+ B cells (Bichi et al, 2002). Like in human CLL, the immunoglobulin rearrangements from different Eμ‐TCL1 leukemic mice can be structurally very similar and closely resemble antibodies reactive to self and to microbial antigens (Yan et al, 2006). We started out by generating Eμ‐TCL1 mice that either expressed defined virus‐specific BCRs or that lacked the BCR entirely. To this end, we bred Eμ‐TCL1 mice against the following mouse lineages: (i) KL25 mice (Hangartner et al, 2003), which carry a gene‐targeted immunoglobulin heavy chain expressing a neutralizing specificity for lymphocytic choriomeningitis virus (LCMV) strain WE; (ii) VI10YEN mice (Hangartner et al, 2003), which carry a gene‐targeted immunoglobulin heavy chain (VI10) and a transgenic non‐targeted immunoglobulin light chain (YEN) expressing a neutralizing specificity for vesicular stomatitis virus (VSV) serotype Indiana; and (iii) DHLMP2A mice (Casola et al, 2004), which carry a targeted replacement of Igh by the Epstein–Barr virus protein LMP2A and develop B cells lacking surface‐expressed and secreted immunoglobulins. Of note, the choice of these particular virus‐specific transgenic BCR lineages rests on the notion that they have been extremely useful at characterizing the role of humoral immunity in the pathogenesis of acute and chronic viral infections (Hangartner et al, 2003, 2006; Sammicheli et al, 2016) and that, being heavy‐chain knock‐in lineages, they allow for examining the eventual role of light chains in CLL development.
B cells isolated from the resulting progeny were first characterized with regard to Tcl1 expression, subset development, and BCR responsiveness. As shown in Fig EV1A, 8‐week‐old pre‐leukemic KL25 × Eμ‐TCL1, VI10YEN × Eμ‐TCL1, and DHLMP2A × Eμ‐TCL1 mice showed levels of splenic Tcl1 expression that were comparable to those of Eμ‐TCL1 mice expressing a polyclonal BCR repertoire. We next enumerated CD5+ B cells in blood, serosal cavities, secondary lymphoid organs and liver of the above‐mentioned mouse strains, again at 8 weeks of age. The number of CD5+ B cells in blood, spleen and lymph nodes of KL25 × Eμ‐TCL1, VI10YEN × Eμ‐TCL1, and DHLMP2A × Eμ‐TCL1 mice was similar to that detected in the same districts of Eμ‐TCL1 mice (Fig EV1B and C); performing a similar comparison in liver and peritoneum, however, indicated that CD5+ B cells were reduced in KL25 × Eμ‐TCL1, VI10YEN × Eμ‐TCL1, and DHLMP2A × Eμ‐TCL1 mice (Fig EV1B and C). While the molecular basis for this selective reduction of CD5+ B cells in liver and peritoneum of pre‐leukemic KL25 × Eμ‐TCL1, VI10YEN × Eμ‐TCL1, and DHLMP2A × Eμ‐TCL1 mice are unclear, it is worth noting that the extent of such reduction was similar in all the 3 above‐mentioned mouse lineages (Fig EV1B and C). We finally confirmed that both KL25 × Eμ‐TCL1 and VI10YEN × Eμ‐TCL1 mice express the respective virus‐specific BCR in all B‐cell subsets and appropriately respond to cognate antigen stimulation (Fig EV1D–G).
Figure EV1. Characterization of KL25 × Eμ‐TCL1, VI10YEN × Eμ‐TCL1, and DHLMP2A × Eμ‐TCL1 mice.
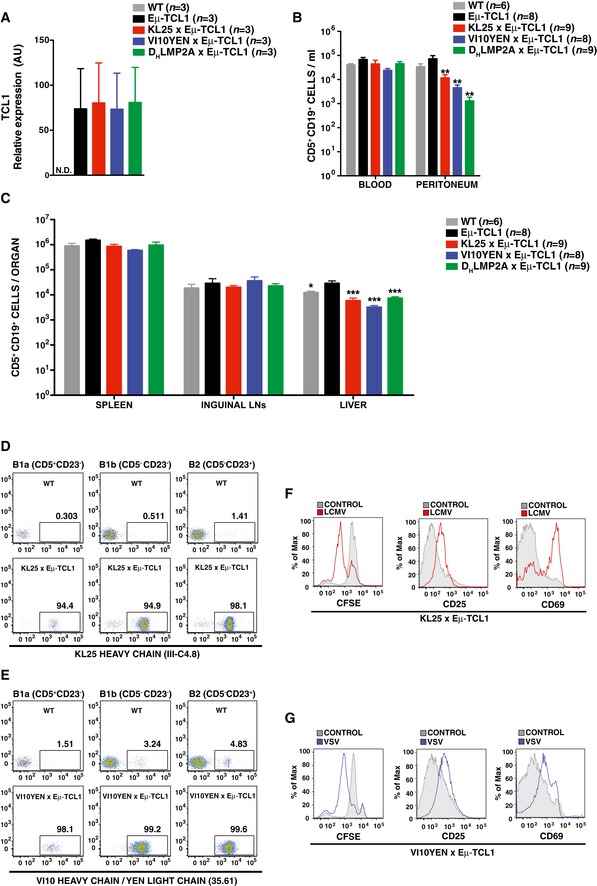
-
ATCL1 expression in the spleen of 8‐week‐old WT (gray), Eμ‐TCL1 (black), KL25 × Eμ‐TCL1 (red), VI10YEN × Eμ‐TCL1 (blue), and DHLMP2A × Eμ‐TCL1 (green) male mice analyzed by RT–qPCR. n = 3. Data are representative of more than three independent experiments.
-
BConcentration of CD5+ CD19+ cells per ml of blood and peritoneal wash of 8‐week‐old WT (gray), Eμ‐TCL1 (black), KL25 × Eμ‐TCL1 (red), VI10YEN × Eμ‐TCL1 (blue), and DHLMP2A × Eμ‐TCL1 (green) male mice. n = 6 (WT), 8 (Eμ‐TCL1), 9 (KL25 × Eμ‐TCL1), 8 (VI10YEN × Eμ‐TCL1), and 9 (DHLMP2A × Eμ‐TCL1).
-
CAbsolute numbers of CD5+ CD19+ cells in the indicated organs of the same mice described in (B).
-
DRepresentative flow cytometry plots showing transgenic BCR expression in B1a (CD19+ CD5+ CD23−), B1b (CD19+ CD5− CD23−), and B2 (CD19+ CD5− CD23+) cells from 8‐week‐old WT (top panel) and KL25 × Eμ‐TCL1 (bottom panel) male mice. Results are representative of more than 10 independent experiments.
-
ERepresentative flow cytometry plots showing transgenic BCR expression in B1a (CD19+ CD5+ CD23−), B1b (CD19+ CD5− CD23−), and B2 (CD19+ CD5− CD23+) cells from 8‐week‐old WT (top panel) and VI10YEN × Eμ‐TCL1 (bottom panel) male mice. Results are representative of more than 10 independent experiments.
-
F, GRepresentative flow cytometry plots showing proliferation (assessed by CFSE dilution, left panels) and activation (assessed by CD25 and CD69 upregulation, middle and right panels, respectively) of KL25 × Eμ‐TCL1 (F) or VI10YEN × Eμ‐TCL1 (G) B cells exposed or not to inactivated LCMV or VSV, respectively. Results are representative of three independent experiments.
We next compared KL25 × Eμ‐TCL1, VI10YEN × Eμ‐TCL1, and DHLMP2A × Eμ‐TCL1 mice to Eμ‐TCL1 mice expressing a polyclonal BCR repertoire with regard to leukemia development at steady state (in the absence of cognate antigen challenge). Disease progression was monitored by quantifying the frequency of CD5+ B cells in peripheral blood (Fig 1A), and we arbitrarily defined leukemic those mice that had ≥ 20% CD5+ cells among total CD19+ B cells (a frequency never reached by WT mice in the 36‐week‐long observation period) (Fig 1B). As previously reported (Bichi et al, 2002), Eμ‐TCL1 mice showed an expansion of circulating CD5+ B cells as early as 16 weeks of age, and by 36 weeks of age 100% of them were frankly leukemic, with accumulation of large numbers of CD5+ B cells in blood, serosal cavities and lymphoid as well as non‐lymphoid organs (Fig 1A–C). DHLMP2A × Eμ‐TCL1 mice showed a profound impairment in leukemia development (Fig 1A–C), indicating that BCR expression is required for leukemia growth and that the tonic signal provided by the LMP2A protein is not sufficient to support leukemic expansion. We then assessed whether pathogen‐specific BCRs sustained cancer development. Both KL25 × Eμ‐TCL1 and VI10YEN × Eμ‐TCL1 mice developed CLL, even though they differed in regard to disease incidence and leukemic cell accumulation. Whereas CLL development in KL25 × Eμ‐TCL1 mice occurred at a rate that was indistinguishable from that of Eμ‐TCL1 mice, VI10YEN × Eμ‐TCL1 mice had a more indolent course of disease (Fig 1A–C). These results indicate that the BCR shapes CLL incidence and behavior in vivo.
Figure 1. Leukemia development in KL25 × Eμ‐TCL1, VI10YEN × Eμ‐TCL1, and DHLMP2A × Eμ‐TCL1 mice.
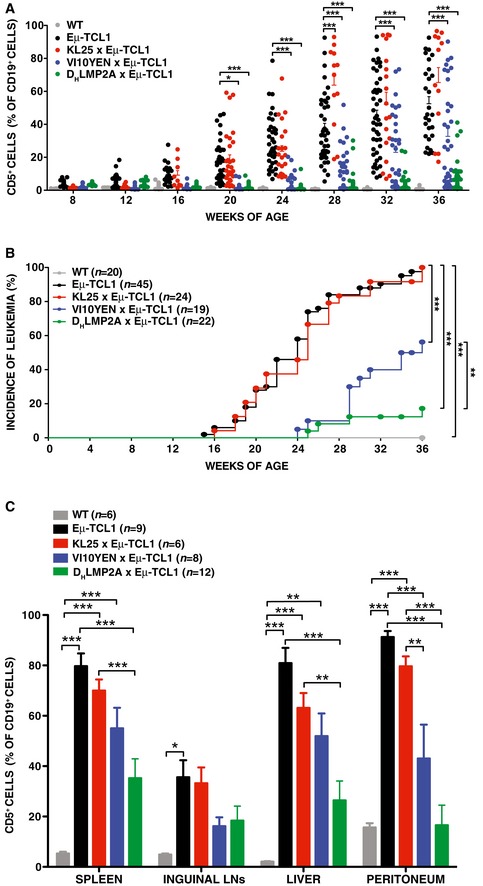
- Percentage of CD5+ cells (out of total CD19+ peripheral blood leukocytes) in WT (gray), Eμ‐TCL1 (black), KL25 × Eμ‐TCL1 (red), VI10YEN × Eμ‐TCL1 (blue), and DHLMP2A × Eμ‐TCL1 (green) male mice at the indicated time points. Two‐way ANOVA (Bonferroni's multiple comparison).
- Incidence of leukemia (defined as ≥ 20% CD5+ cells out of total CD19+ peripheral blood leukocytes) over time in the same mice described in (A). n = 4–20 (WT), 16–45 (Eμ‐TCL1), 8–29 (KL25 × Eμ‐TCL1), 14–34 (VI10YEN × Eμ‐TCL1), 19–35 (DHLMP2A × Eμ‐TCL1). Log‐rank (Mantel‐Cox).
- Percentage of CD5+ cells (out of total CD19+ cells) in the indicated organs of the same mice described in (A) at 36 weeks of age. n = 6 (WT), 9 (Eμ‐TCL1), 6 (KL25 × Eμ‐TCL1), 8 (VI10YEN × Eμ‐TCL1), 12 (DHLMP2A × Eμ‐TCL1). One‐way ANOVA (Bonferroni's multiple comparison).
Before attempting to pinpoint the mechanisms underlying the difference in CLL incidence between KL25 × Eμ‐TCL1 and VI10YEN × Eμ‐TCL1 mice, we sought to determine whether cognate antigen recognition, prior to disease onset, influenced CLL development and progression in Eμ‐TCL1 mice expressing virus‐specific BCRs. To this end, we infected 8‐week‐old VI10YEN × Eμ‐TCL1 mice (and Eμ‐TCL1 controls) with 106 p.f.u. of VSV Indiana. VSV infection induced B cells in VI10YEN × Eμ‐TCL1 mice to get activated, proliferate, and differentiate into Ab‐secreting cells (Fig EV2A), but it did not alter the kinetics of leukemia development or progression (Figs 2A and B, and EV2B). We then infected 8‐week‐old KL25 × Eμ‐TCL1 mice and Eμ‐TCL1 controls with 106 f.f.u. of LCMV WE. Unexpectedly, LCMV infection of both KL25 × Eμ‐TCL1 mice and Eμ‐TCL1 controls (that express a polyclonal BCR repertoire) abrogated CLL development (Fig EV3). The cellular and molecular underpinnings of this intriguing observation extend beyond the scope of this study and will be the subject of a future report. To avoid potentially confounding effects, we henceforth decided to test the role of antigenic stimulation in this setting by repetitively immunizing 8‐week‐old KL25 × Eμ‐TCL1 mice (and Eμ‐TCL1 controls) with the purified LCMV WE glycoprotein [which contains the antigenic determinant recognized by KL25 B cells (Sammicheli et al, 2016)]. Although LCMV immunization induced B cells in KL25 × Eμ‐TCL1 mice to get activated, proliferate and differentiate into Ab‐secreting cells (Fig EV4A), it did not alter the kinetics of leukemia development or progression (Figs 2C and D, and EV4B and C). Together, these results suggest that high‐affinity recognition of pathogen‐derived antigens does not affect CLL development or progression, and they prompted us to investigate whether virus‐specific BCRs may drive CLL pathogenesis by mechanisms that are unrelated to pathogen specificity.
Figure EV2. VSV infection does not affect CLL development or progression.
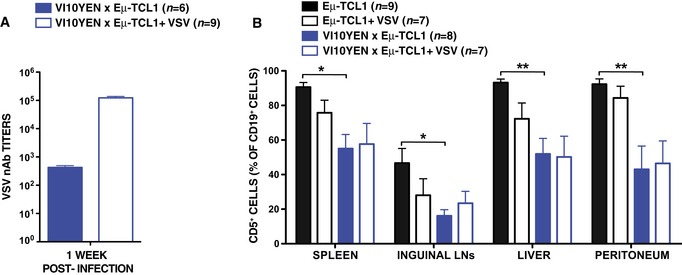
- VSV neutralizing antibody (nAb) titers in the serum of VI10YEN × Eμ‐TCL1 9‐week‐old male mice that were infected (open bars) or not (closed bars) with VSV 7 days earlier. n = 6 (VI10YEN × Eμ‐TCL1) and 9 (VI10YEN × Eμ‐TCL1 + VSV).
- Percentage of CD5+ cells (out of total CD19+ cells) in the indicated organs of Eμ‐TCL1 (black) and VI10YEN × Eμ‐TCL1 (blue) male mice that were infected (open bars) or not (closed bars) with 106 p.f.u. of VSV Indiana at 8 weeks of age and sacrificed 28 weeks later. n = 9 (Eμ‐TCL1), 7 (Eμ‐TCL1 + VSV), 8 (VI10YEN × Eμ‐TCL1), 7 (VI10YEN × Eμ‐TCL1 + VSV). One‐way ANOVA (Bonferroni’s multiple comparison).
Figure 2. High‐affinity antigen recognition does not affect CLL development or progression.
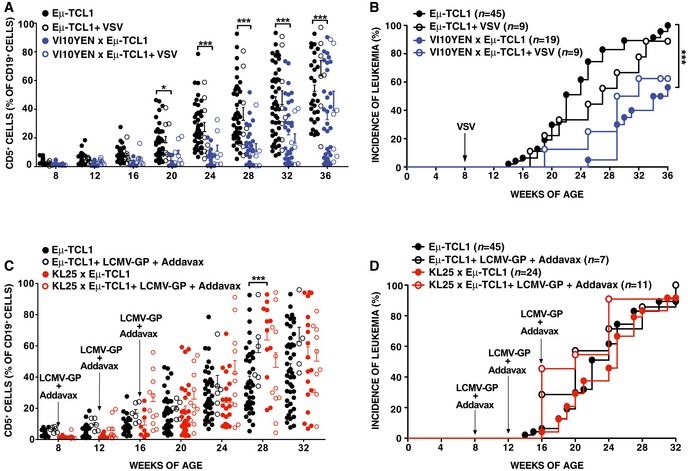
- Percentage of CD5+ cells (out of total CD19+ peripheral blood leukocytes) over time in Eμ‐TCL1 (black) and VI10YEN × Eμ‐TCL1 (blue) male mice that were infected (open symbols) or not (closed symbols) with 106 p.f.u. of VSV Indiana at 8 weeks of age.
- Incidence of leukemia (defined as ≥ 20% CD5+ cells out of total CD19+ peripheral blood leukocytes) over time in the same mice described in (A). n = 16–45 (Eμ‐TCL1), 9 (Eμ‐TCL1 + VSV), 14–34 (VI10YEN × Eμ‐TCL1), 7–9 (VI10YEN × Eμ‐TCL1 + VSV).
- Percentage of CD5+ cells (out of total CD19+ peripheral blood leukocytes) over time in Eμ‐TCL1 (black) and KL25 × Eμ‐TCL1 (red) mice that were immunized (open symbols) or not (closed symbols) with LCMV‐GP + Addavax at the indicated time points.
- Incidence of leukemia (defined as ≥ 20% CD5+ cells out of total CD19+ peripheral blood leukocytes) over time in the same mice described in (C). n = 16–45 (Eμ‐TCL1), 7 (Eμ‐TCL1 + LCMV‐GP + Addavax), 8–29 (KL25 × Eμ‐TCL1), 10–11 (KL25 × Eμ‐TCL1 + LCMV‐GP + Addavax).
Figure EV3. LCMV infection prevents CLL development in Eμ‐TCL1 mice.
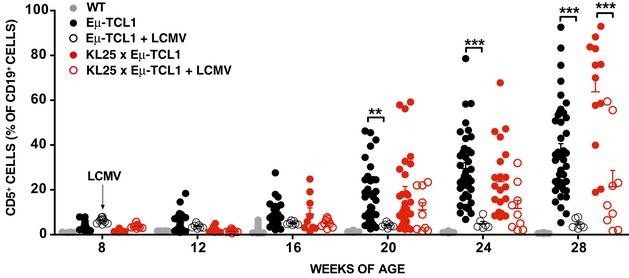
Percentage of CD5+ cells (out of total CD19+ peripheral blood leukocytes) over time in WT (gray) and in Eμ‐TCL1 (black) male mice that were infected (open symbols) or not (closed symbols) with LCMV. n = 4–20 (WT), 16–45 (Eμ‐TCL1), 6–10 (Eμ‐TCL1 + LCMV), 8–29 (KL25 × Eμ‐TCL1), 9–11 (KL25 × Eμ‐TCL1 + LCMV). Please note that the uninfected WT, Eμ‐TCL1, and KL25 × Eμ‐TCL1 controls are the same as the ones reported in Fig 1A. Results are expressed as mean + SEM. **P < 0.01, ***P < 0.001. Exact P‐values for each experiment are reported in Appendix Table S1. Two‐way ANOVA (Bonferroni’s multiple comparison) was used.Source data are available online for this figure.
Figure EV4. Immunization with LCMV‐GP does not affect CLL development or progression.
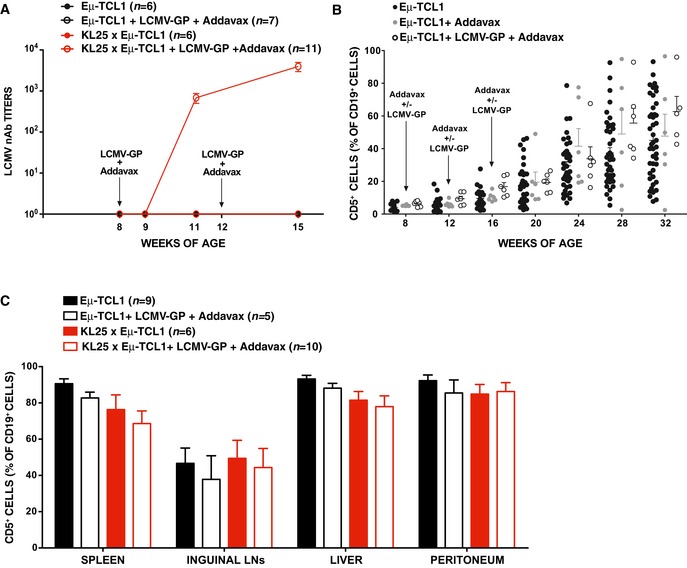
- LCMV neutralizing antibody (nAb) titers over time in the serum of Eμ‐TCL1 (black) and KL25 × Eμ‐TCL1 (red) male mice that were immunized (open symbols) or not (closed symbols) with LCMV‐GP + Addavax. n = 6 (Eμ‐TCL1), 7 (Eμ‐TCL1 + LCMV‐GP + Addavax), 6 (KL25 × Eμ‐TCL1), 11 (KL25 × Eμ‐TCL1 + LCMV‐GP + Addavax).
- Percentage of CD5+ cells (out of total CD19+ peripheral blood leukocytes) over time in control Eμ‐TCL1 mice (black symbols) or in mice that were injected intramuscularly with Addavax (gray) or with LCMV‐GP + Addavax (open symbols).
- Percentage of CD5+ cells (out of total CD19+ cells) in the indicated organs of Eμ‐TCL1 (black) and KL25 × Eμ‐TCL1 (red) mice that were immunized (open bars) or not (closed bars) with LCMV‐GP + Addavax and sacrificed 24 weeks after the first immunization. n = 9 (Eμ‐TCL1), 5 (Eμ‐TCL1 + LCMV‐GP + Addavax), 6 (KL25 × Eμ‐TCL1), 10 (KL25 × Eμ‐TCL1 + LCMV‐GP + Addavax).
To begin investigating such potential pathogenic mechanisms, we analyzed the BCR repertoire of leukemic KL25 × Eμ‐TCL1 and VI10YEN × Eμ‐TCL1 mice and compared it to that of age‐matched KL25 and VI10YEN mice. Since both KL25 and VI10YEN are knock‐in for the BCR heavy chain (Hangartner et al, 2003), there is no alternative heavy chain that these mice can express. Accordingly, all analyzed leukemic KL25 × Eμ‐TCL1 and VI10YEN × Eμ‐TCL1 mice expressed the expected transgenic heavy chain as an IgM (Tables EV1 and EV2, and Fig EV5). As per the light‐chain repertoire, we noticed that, when compared with age‐matched KL25 and VI10YEN mice, leukemic KL25 × Eμ‐TCL1 and VI10YEN × Eμ‐TCL1 mice had a biased light‐chain usage. Specifically, among the light chains preferentially expressed by leukemic KL25 × Eμ‐TCL1 mice, we found the IGKV12‐44*01 F/IGKJ2*01 F gene associated with the LCDR3 motif CQH‐HYGTPY‐TF and the IGKV6‐32*01 F/IGKJ2*01 F gene associated with the LCDR3 motif CQQ‐DYSS‐TF (Fig 3A and Table EV1). Similarly, leukemic VI10YEN × Eμ‐TCL1 mice preferentially expressed the IGKV6‐32*01 F/IGKJ2*01 F gene associated with the LCDR3 motif CQQ‐DYSS‐TF and the IGKV6‐32*01 F/IGKJ2*01 F gene associated with the LCDR3 motif CQQ‐DYSSPY‐TF (the YEN transgenic light chain, Fig 3A and Table EV2). This preferential light‐chain usage is reminiscent to what has been described for polyclonal Eμ‐TCL1 (Yan et al, 2006) and suggested that leukemic KL25 × Eμ‐TCL1 and VI10YEN × Eμ‐TCL1 mice selected BCRs capable of cross‐reacting with one or more autoantigens. One particular case in point is the capacity of CLL‐derived BCRs to recognize an internal epitope of the BCR itself, a feature referred to as cell autonomous signaling (Dühren‐von Minden et al, 2012). We therefore set out to test whether BCRs derived from leukemic KL25 × Eμ‐TCL1 and VI10YEN × Eμ‐TCL1 mice possessed cell autonomous signaling activity. To this end, we introduced the corresponding heavy and light chains in the BCR‐deficient murine B‐cell line TKO, which expresses an inactive B‐cell linker (BLNK) adaptor protein that becomes functional in the presence of 4‐hydroxytamoxifen (4‐OHT) (Dühren‐von Minden et al, 2012). Addition of 4‐OHT to TKO cells with an autonomously active BCR results in signal activation and propagation, ultimately resulting in an increase in intracellular Ca++ levels that is detectable by flow cytometry (Dühren‐von Minden et al, 2012; Fig 3B). The BCR composed of the KL25 transgenic heavy chain coupled with the light chain that was most frequently expressed in non‐leukemic 9‐month‐old KL25 mice (IGKV3‐10*01 F/IGKJ1*01 F gene associated with the LCDR3 motif CQQ‐NNEDPW‐TF) was not autonomously active (Fig 3C, left panel); similarly, the BCR composed of the VI10 transgenic heavy chain coupled to the transgenic YEN light chain (the most frequently expressed light chain in non‐leukemic 9‐month‐old VI10YEN mice) did not possess autonomous signaling capability (Fig 3D, left panel). We next evaluated BCRs composed of the same KL25 and VI10 heavy chains coupled to the light chains that were most frequently expressed in 9‐month‐old leukemic KL25 × Eμ‐TCL1 and VI10YEN × Eμ‐TCL1 mice, respectively. When expressed together with the KL25 heavy chain, two of the light chains that were most frequently selected in leukemic KL25 × Eμ‐TCL1 mice endowed TKO cells with autonomous signaling activity (Fig 3C, right panels). By contrast, when expressed together with the VI10 heavy chain, the light chain most frequently selected in leukemic VI10YEN × Eμ‐TCL1 mice did not confer cell autonomous signaling activity to TKO cells (Fig 3D, right panel). The observation that KL25 × Eμ‐TCL1 mice—which progress rapidly to CLL (Fig 1A and B)—show cell autonomous signaling activity, whereas VI10YEN × Eμ‐TCL1 mice—which have a more indolent course of disease (Fig 1A and B)—do not is in agreement with the notion that autonomous signaling is an important pathogenic driver in CLL (Dühren‐von Minden et al, 2012; Iacovelli et al, 2015), but argues against autonomous signaling being an absolute prerequisite of leukemia development. Future studies should assess whether patient‐derived CLL cells that express a pathogen‐reactive BCR possess or lack cell autonomous signaling capability and whether this property relates to disease activity. The observation that leukemic VI10YEN × Eμ‐TCL1 mice showed a biased light‐chain usage that did not confer autonomous signaling activity (Fig 3D) prompted us to explore the possibility that these leukemic BCRs might be cross‐reacting with different autoantigens. To test this hypothesis and to characterize the nature of such potential autoantigens, we screened sera from young and old KL25, VI10YEN, Eμ‐TCL1, KL25 × Eμ‐TCL1, and VI10YEN × Eμ‐TCL1 mice against a panel of 124 nuclear, cytoplasmic, membrane, and phospholipid autoantigens known to be targeted by autoantibodies in various autoimmune diseases and in mouse and human CLL (Yan et al, 2006; Catera et al, 2008) (see the complete list of antigens in Table EV3). Sera from 8‐week‐old KL25, VI10YEN, Eμ‐TCL1, KL25 × Eμ‐TCL1, and VI10YEN × Eμ‐TCL1 mice as well as 9‐month‐old KL25 and VI10YEN mice did not react with most of the tested autoantigens; by contrast, sera from 9‐month‐old leukemic Eμ‐TCL1, KL25 × Eμ‐TCL1 and VI10YEN × Eμ‐TCL1 mice bound avidly to the vast majority of autoantigens that were examined (Fig 3E). To formally demonstrate that autoantibodies were indeed produced by the malignant cells, we generated monoclonal IgMs bearing the KL25 heavy chain coupled to the IGKV12‐44*01 F/IGKJ2*01 F light chain associated with the LCDR3 motif CQH‐HYGTPY‐TF (the most frequently selected light chain in leukemic KL25 × Eμ‐TCL1 mice) or the VI10 heavy chain coupled to the IGKV6‐32*01 F/IGKJ2*01 F light chain associated with the LCDR3 motif CQQ‐DYSS‐TF (the most frequently selected light chain in leukemic VI10YEN × Eμ‐TCL1 mice). Both monoclonal antibodies showed a significant degree of autoreactivity, with the antibody derived from KL25 × Eμ‐TCL1 mice recognizing a broader range of autoantigens (Fig 3E). These results indicate that leukemic KL25 × Eμ‐TCL1 and VI10YEN × Eμ‐TCL1 mice (and, possibly, polyclonal Eμ‐TCL1 mice) preferentially selected light chains that confer BCRs the capacity to cross‐react with a broad range of autoantigens. The data are consistent with the hypothesis, based on evidence obtained in CLL patients, that light chains, in association with defined heavy chains, are crucial in shaping the specificity of leukemic BCRs (Stamatopoulos et al, 2005; Hadzidimitriou et al, 2009; Kostareli et al, 2010).
Figure EV5. CLL clones in Eμ‐TCL1, KL25 × Eμ‐TCL1, and VI10YEN × Eμ‐TCL1 mice express IgM.
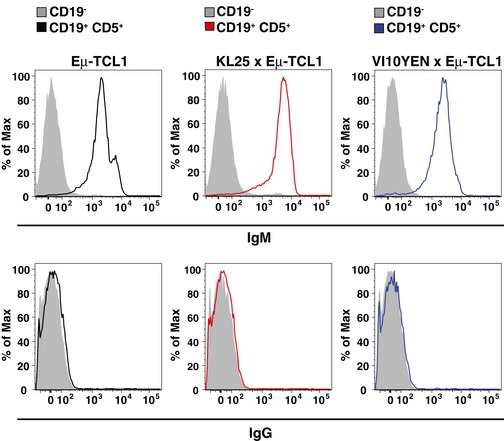
Representative flow cytometry plots of IgM (top panels) and IgG (bottom panels) expressions in CD19− cells (gray) and CD19+ CD5+ CLL cells (blue) in peripheral blood leukocytes isolated from 36‐week‐old Eμ‐TCL1 (left panels), KL25 × Eμ‐TCL1 (middle panels), and VI10YEN × Eμ‐TCL1 (right panels) male mice.
Figure 3. Pathogen‐specific B‐cell receptors drive chronic lymphocytic leukemia by light‐chain‐dependent cross‐reaction with autoantigens.
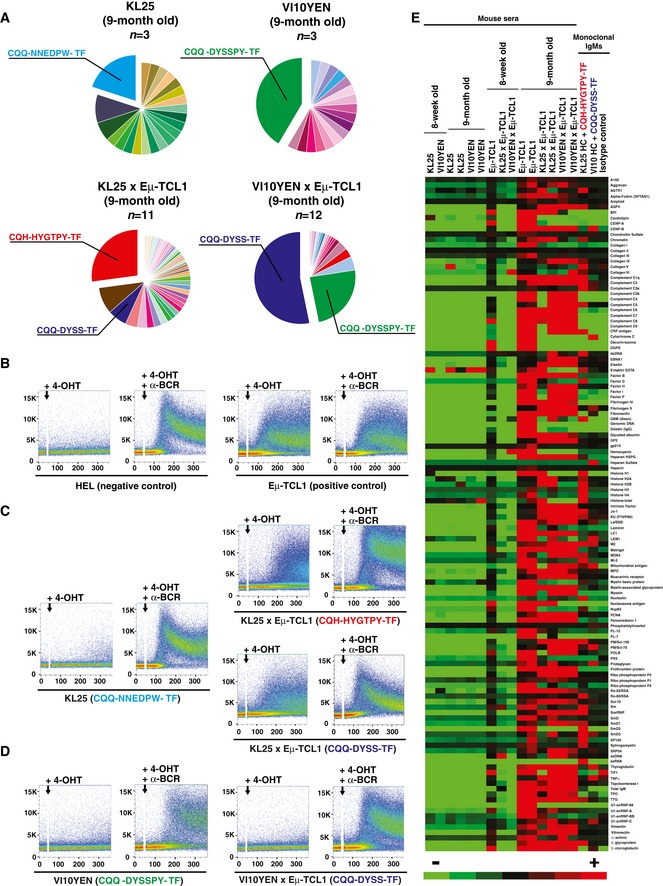
-
APie charts representing LCDR3 usage in 9‐month‐old KL25 (top left), VI10YEN (top right), KL25 × Eμ‐TCL1 (bottom left), and VI10YEN × Eμ‐TCL1 male mice (bottom right). n = 3 (KL25 and VI10YEN), 11 (KL25 × Eμ‐TCL1), 12 (VI10YEN × Eμ‐TCL1).
-
B–DRepresentative flow cytometry analyses of Ca2+ flux after activation of the ERT2‐BLNK fusion protein by 4‐OHT with or without an anti‐mouse light‐chain antibody (α‐BCR) in TKO cells expressing the indicated BCR (the CDR3 corresponding to the expressed light chain is indicated in parentheses). Addition of 4‐OHT with or without α‐BCR is marked by an arrow. Results are representative of three independent experiments.
-
ESera from 8‐week‐ and 9‐month‐old KL25, VI10YEN, Eμ‐TCL1, KL25 × Eμ‐TCL1, and VI10YEN × Eμ‐TCL1 male mice or monoclonal IgMs from leukemic KL25 × Eμ‐TCL1 and VI10YEN × Eμ‐TCL1 mice were screened for the presence of autoantibodies against a panel of 124 nuclear, cytoplasmic, membrane, and phospholipid autoantigens. The heat maps are based on the normalized fluorescent intensity of autoantibodies and are represented on a color scale range between +200 (red) and −200 (green) standard deviations.
In conclusion, we here demonstrate that BCR expression is required for leukemia growth in the Eμ‐TCL1 transgenic mouse model and that CLL clones preferentially select light chains that, when paired with virus‐specific heavy chains, confer B cells the ability to recognize a broad range of autoantigens. Taken together, our results suggest that pathogens may drive CLL pathogenesis by selecting and expanding pathogen‐specific B cells that cross‐react with one or more self‐antigens. The interaction between malignant B cells and self‐antigens may then be crucial for disease progression.
Materials and Methods
Mice
C57BL/6 and CD45.1 (inbred C57BL/6) mice were purchased from Charles River. Eμ‐TCL1 mice (Bichi et al, 2002) were provided by C. Croce (Ohio State University). DHLMP2A mice (Casola et al, 2004) (inbred Balb/c) were originally provided by K. Rajewsky (Harvard Medical School) and bred more than 10 generations against C57BL/6 mice. Heavy‐chain knock‐in and light‐chain BCR‐transgenic mice specific for VSV Indiana (VI10YEN (Hangartner et al, 2003)) and heavy‐chain knock‐in BCR‐transgenic mice specific for LCMV WE (KL25, Hangartner et al, 2003) were obtained through the European Virus Archive. Of note, the Eμ‐TCL1 transgene was brought to homozygosity in all lineages. Mice were housed under specific pathogen‐free conditions, and, in all experiments, they were matched for age and sex before experimental manipulation. All experimental animal procedures were approved by the Institutional Animal Committee of the San Raffaele Scientific Institute.
Infections and immunizations
Eight‐week‐old male mice were infected intravenously with 1 × 106 plaque‐forming units (p.f.u.) of VSV serotype Indiana, or with 1 × 106 focus‐forming units (f.f.u.) of LCMV WE. Alternatively, mice were immunized intramuscularly with 10 μg of recombinant LCMV WE glycoprotein (GP)‐1‐human IgG fusion protein (Sommerstein et al, 2015) mixed at 1:1 ratio with a squalene‐based oil‐in‐water nano‐emulsion (AddaVax, InvivoGen), as described (Sammicheli et al, 2016). Viruses were propagated and quantified as described (Iannacone et al, 2008; Tonti et al, 2013), and dissolved in 200 μl of PBS prior to intravenous injection.
Mice were retro‐orbitally bled at the indicated time points for VSV‐ or LCMV‐specific Abs measured by VSV neutralization assay or LCMV focus reduction assay, as described (Sammicheli et al, 2016). All infectious work was performed in designated BSL‐2 and BSL‐3 workspaces in accordance with institutional guidelines.
Flow cytometry‐based analyses
Mice were bled retro‐orbitally every 2 weeks, and leukemia development and progression were assessed by flow cytometry‐based quantification of CD19+ CD5+ cells. White blood cell counts were performed on an automated cell counter (HeCoVet; Seac–Radim). Mice were sacrificed at 36 weeks of age or earlier if they showed signs of advanced leukemia (i.e. lethargy, impaired mobility, hunched posture, labored breathing, splenomegaly, and/or hepatomegaly). Single‐cell suspensions of livers, spleens, and lymph nodes were generated as described (Tonti et al, 2013; Guidotti et al, 2015). Peritoneal cells were removed by injection of 10 ml of HBSS into the peritoneal cavity followed by withdrawal of the peritoneal exudates. All flow cytometry stainings of surface‐expressed molecules were performed as described (Sammicheli et al, 2016). Antibodies used included PB‐conjugated anti‐CD19 (eBio1D3, BD Pharmingen), APC‐ and PerCP‐conjugated anti‐CD5 (53–7.3, BD Pharmingen), FITC‐conjugated anti‐CD23 (B3B4, BD Pharmingen), PE‐Cy7‐conjugated anti‐CD3 (145‐2C11, BD Pharmingen), APC‐conjugated anti‐IgM (11/41, BD Pharmingen), Alexa‐Fluor 546 anti‐mouse IgG (polyclonal, Invitrogen), FITC‐conjugated anti‐CD69 (H1.2F3, BD Pharmingen), PE‐conjugated anti‐CD25 (PC61, BioLegend), eFluor 450‐conjugated anti‐B220 (RA3‐682, eBioscience), PerCP‐conjugated anti‐B220 (RA3‐B2, BioLegend), and PE‐conjugated Streptavidin (BD Pharmingen). The anti‐idiotypic antibodies 35.61 (Hangartner et al, 2003) (which recognizes a combinatorial determinant provided by VH and Vk of VI10) and III‐C4.8 (Hangartner et al, 2003) (which recognizes the VH of KL25) were produced from hybridoma supernatants and biotinylated according to standard methods. All flow cytometry analyses were performed in FACS buffer containing PBS with 2 mM EDTA and 2% FBS on a FACS CANTO (BD Pharmingen) and analyzed with FlowJo software (Treestar Inc.).
Quantification of TCL1 expression
Total RNA was extracted from splenocytes using the ReliaPreptm kit (Promega) according to the manufacturer's instructions. mRNA was reverse‐transcribed with Promega RT reagents (Promega). Real‐time quantitative PCRs were performed on a ABI 7900 HT Fast Real‐Time PCR System (Applied Biosystems) with FastStart Universal SYBR Green Master Mix (Roche) using the following primers: TCL‐1 (forward) 5′‐GCCTGGCTGCCCTTAACC‐3′, TCL‐1 (reverse) 5′‐GACGCAAGAGCACCCGTAAC‐3′, β‐actin (forward) 5′‐AAGAGAAGGGTTACCCGGGATA‐3′, β‐actin (reverse) 5′‐CCTAAGGCCAACCGTGAAAA‐3′. Every reaction was run in triplicates, and β‐actin levels were used as an endogenous control for normalization.
B‐cell activation in vitro
Naïve B cells from the spleens of KL25 × Eμ‐TCL1 and VI10YEN × Eμ‐TCL1 were negatively selected by magnetic isolation and tested for their capacity to get activated and proliferate in response to PFA‐inactivated VSV or LCMV as described (Sammicheli et al, 2016).
IGHV and IGLV sequencing analysis
Total cellular RNA was isolated from the spleens of leukemic mice using ReliaPrep™ RNA Tissue Miniprep System (Promega). RNA was reverse‐transcribed using oligo‐dT, and cDNA was amplified by PCR using Phusion® Flash High‐Fidelity PCR Master Mix (Thermo Fisher Scientific) with FR1 and constant region primers (Iacovelli et al, 2015). PCR products were purified using Wizard® SV Gel and PCR Clean‐Up System (Promega) and directly sequenced using Sanger ABI 3730xl (GATC Biotech). Samples with more than one IGHV or IGLV rearrangement were cloned into Zero Blunt® TOPO® plasmid and analyzed by sequencing. Alignments of IGHV or IGLV genes against murine germline sequences were performed with IMGT/V‐QUEST software (http://www.imgt.org/).
Analysis of cell autonomous BCR signaling activity
IGHV and IGLV genes were amplified by anchor‐PCR using poly‐G‐tailed complementary DNA and a poly‐C‐containing primer and inserted into respective retroviral vectors, as described (Dühren‐von Minden et al, 2012). 1 × 106 freshly transduced TKO cells expressing ERT2–SLP65 was loaded with Indo‐1 (Invitrogen) using Pluronic (Invitrogen). Induction of ERT2–SLP65 was performed by the addition of 2 μM 4‐OHT (Sigma‐Aldrich). Calcium flux was measured with LSR Fortessa (Becton Dickinson). Cross‐linking of the BCR with goat anti‐mouse kappa (10 μg/ml; Southern Biotech) was used as a positive control.
Monoclonal IgM production
Recombinant monoclonal IgMs expressing the KL25 heavy chain coupled to the IGKV12‐44*01 F/IGKJ2*01 F light chain associated with the LCDR3 motif CQH‐HYGTPY‐TF (the most frequently selected light chain in leukemic KL25 × Eμ‐TCL1 mice) or the VI10 heavy chain coupled to the IGKV6‐32*01 F/IGKJ2*01 F light chain associated with the LCDR3 motif CQQ‐DYSS‐TF (the most frequently selected light chain in leukemic VI10YEN × Eμ‐TCL1 mice) were produced in HEK293 cells by Absolute Antibody (Oxford, UK).
Protein microarray analysis
Sera from young and old KL25, VI10YEN, Eμ‐TCL1, KL25 × Eμ‐TCL1, and VI10YEN × Eμ‐TCL1 mice and monoclonal IgMs derived from leukemic KL25 × Eμ‐TCL1 and VI10YEN × Eμ‐TCL1 mice were screened for autoreactivity by using an autoantigen proteomic microarray comprising 124 different antigens. Monoclonal IgMs were tested at a concentration of 1 mg/ml. An isotype control (ThermoFisher, catalog number: 026800) was used as a negative control. Autoantigens microarrays were manufactured, hybridized and scanned by the Genomics & Microarray Core Facility at UT Southwestern Medical Center. Normalized fluorescent intensity values were analyzed with Cluster 3.0 and Java‐TreeView software to generate the heat map. Color scale ranges between +200 and −200 standard deviations.
Statistical analyses
Results are expressed as mean + SEM. All statistical analyses were performed in Prism (GraphPad Software). Means among three or more groups were compared with one‐way or two‐way analysis of variance with Bonferroni's post‐test. Kaplan–Meier survival curves were compared with the log‐rank (Mantel‐Cox) test. Exact P‐values for each experiment are reported in Appendix Table S1.
Author contributions
NJO and MDG designed and performed experiments, analyzed data, prepared the figures, and wrote the paper; JF, PDL, and AF performed experiments and analyzed data; RÜ performed the cell autonomous signaling experiments on TKO cells; SI performed the initial light‐chain sequencing experiments; DGE, FC‐C, HJ, PG, and LGG provided conceptual advice and revised the paper; MI designed and coordinated the study, provided funding, analyzed the data, and wrote the paper.
Conflict of interest
The authors declare that they have no conflict of interest.
For more information
The paper explained.
Problem
Chronic lymphocytic leukemia (CLL), the most common adult leukemia in the Western World, is characterized by the clonal expansion of a subset of B lymphocytes. Epidemiological studies have associated several infections to CLL, but if and how pathogens drive leukemia development and progression is largely unexplored.
Results
We show here, in animal models of disease, that a specific protein (the B‐cell receptor) is required for leukemia development. Moreover, acute or chronic infections do not lead to faster leukemia development or progression. Rather, recognition of autoantigens is a major pathogenic driver in CLL.
Impact
Our results help clarify the role of B‐cell receptor signaling in CLL and should instruct the further development and use of drugs targeting this pathway.
Supporting information
Appendix
Expanded View Figures PDF
Table EV1
Table EV2
Table EV3
Source Data for Expanded View
Review Process File
Source Data for Figure 1A
Source Data for Figure 1B
Source Data for Figure 1C
Source Data for Figure 2A
Source Data for Figure 2B
Source Data for Figure 2C
Source Data for Figure 2D
Acknowledgements
We thank M. Silva for secretarial assistance; M. Mainetti, L. Giustini, and M. Raso for technical assistance; C. Croce for Eμ‐TCL1 mice; A. Mondino for critical reading of the manuscript; and all the members of the Iannacone laboratory for helpful discussions. Flow cytometry was carried out at FRACTAL, a flow cytometry resource and advanced cytometry technical applications laboratory established by the San Raffaele Scientific Institute. This work was supported by ERC grants 281648 and 725038 (to M.I.), Italian Association for Cancer Research (AIRC) grants 15350 (to M.I.), 15189 (to P.G.) and 9965 (to M.I., P.G. and F.C.C), Italian Ministry of Health grant GR‐2011‐02347925 (to M.I.), Fondazione Regionale per la Ricerca Biomedica grant 2015‐0010 (to M.I.), European Molecular Biology Organization (EMBO) Young Investigator Program (to M.I.), and a Career Development Award from the Giovanni Armenise‐Harvard Foundation (to M.I.).
EMBO Mol Med (2017) 9: 1482–1490
References
- Bichi R, Shinton SA, Martin ES, Koval A, Calin GA, Cesari R, Russo G, Hardy RR, Croce CM (2002) Human chronic lymphocytic leukemia modeled in mouse by targeted TCL1 expression. Proc Natl Acad Sci USA 99: 6955–6960 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burger JA, Chiorazzi N (2013) B cell receptor signaling in chronic lymphocytic leukemia. Trends Immunol 34: 592–601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casola S, Otipoby KL, Alimzhanov M, Humme S, Uyttersprot N, Kutok JL, Carroll MC, Rajewsky K (2004) B cell receptor signal strength determines B cell fate. Nat Immunol 5: 317–327 [DOI] [PubMed] [Google Scholar]
- Catera R, Silverman GJ, Hatzi K, Seiler T, Didier S, Zhang L, Hervé M, Meffre E, Oscier DG, Vlassara H et al (2008) Chronic lymphocytic leukemia cells recognize conserved epitopes associated with apoptosis and oxidation. Mol Med 14: 665–674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dühren‐von Minden M, Übelhart R, Schneider D, Wossning T, Bach MP, Buchner M, Hofmann D, Surova E, Follo M, Köhler F et al (2012) Chronic lymphocytic leukaemia is driven by antigen‐independent cell‐autonomous signalling. Nature 489: 309–312 [DOI] [PubMed] [Google Scholar]
- Furman RR, Sharman JP, Coutre SE, Cheson BD, Pagel JM, Hillmen P, Barrientos JC, Zelenetz AD, Kipps TJ, Flinn I et al (2014) Idelalisib and rituximab in relapsed chronic lymphocytic leukemia. N Engl J Med 370: 997–1007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guidotti LG, Inverso D, Sironi L, Di Lucia P, Fioravanti J, Ganzer L, Fiocchi A, Vacca M, Aiolfi R, Sammicheli S et al (2015) Immunosurveillance of the liver by intravascular effector CD8(+) T cells. Cell 161: 486–500 [DOI] [PubMed] [Google Scholar]
- Hadzidimitriou A, Darzentas N, Murray F, Smilevska T, Arvaniti E, Tresoldi C, Tsaftaris A, Laoutaris N, Anagnostopoulos A, Davi F et al (2009) Evidence for the significant role of immunoglobulin light chains in antigen recognition and selection in chronic lymphocytic leukemia. Blood 113: 403–411 [DOI] [PubMed] [Google Scholar]
- Hangartner L, Senn BM, Ledermann B, Kalinke U, Seiler P, Bucher E, Zellweger RM, Fink K, Odermatt B, Bürki K et al (2003) Antiviral immune responses in gene‐targeted mice expressing the immunoglobulin heavy chain of virus‐neutralizing antibodies. Proc Natl Acad Sci USA 100: 12883–12888 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hangartner L, Zinkernagel RM, Hengartner H (2006) Antiviral antibody responses: the two extremes of a wide spectrum. Nat Rev Immunol 6: 231–243 [DOI] [PubMed] [Google Scholar]
- Hoogeboom R, van Kessel KPM, Hochstenbach F, Wormhoudt TA, Reinten RJA, Wagner K, Kater AP, Guikema JEJ, Bende RJ, van Noesel CJM (2013) A mutated B cell chronic lymphocytic leukemia subset that recognizes and responds to fungi. J Exp Med 210: 59–70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hwang K‐K, Trama AM, Kozink DM, Chen X, Wiehe K, Cooper AJ, Xia S‐M, Wang M, Marshall DJ, Whitesides J et al (2014) IGHV1‐69 B cell chronic lymphocytic leukemia antibodies cross‐react with HIV‐1 and hepatitis C virus antigens as well as intestinal commensal bacteria. PLoS One 9: e90725 24614505 [Google Scholar]
- Iacovelli S, Hug E, Bennardo S, Duehren‐von Minden M, Gobessi S, Rinaldi A, Suljagic M, Bilbao D, Bolasco G, Eckl‐Dorna J et al (2015) Two types of BCR interactions are positively selected during leukemia development in the Eμ‐TCL1 transgenic mouse model of CLL. Blood 125: 1578–1588 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iannacone M, Sitia G, Isogawa M, Whitmire JK, Marchese P, Chisari FV, Ruggeri ZM, Guidotti LG (2008) Platelets prevent IFN‐alpha/beta‐induced lethal hemorrhage promoting CTL‐dependent clearance of lymphocytic choriomeningitis virus. Proc Natl Acad Sci USA 105: 629–634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kostareli E, Hadzidimitriou A, Stavroyianni N, Darzentas N, Athanasiadou A, Gounari M, Bikos V, Agathagelidis A, Touloumenidou T, Zorbas I et al (2009) Molecular evidence for EBV and CMV persistence in a subset of patients with chronic lymphocytic leukemia expressing stereotyped IGHV4‐34 B‐cell receptors. Leukemia 23: 919–924 [DOI] [PubMed] [Google Scholar]
- Kostareli E, Sutton L‐A, Hadzidimitriou A, Darzentas N, Kouvatsi A, Tsaftaris A, Anagnostopoulos A, Rosenquist R, Stamatopoulos K (2010) Intraclonal diversification of immunoglobulin light chains in a subset of chronic lymphocytic leukemia alludes to antigen‐driven clonal evolution. Leukemia 24: 1317–1324 [DOI] [PubMed] [Google Scholar]
- Landgren O, Rapkin JS, Caporaso NE, Mellemkjaer L, Gridley G, Goldin LR, Engels EA (2007) Respiratory tract infections and subsequent risk of chronic lymphocytic leukemia. Blood 109: 2198–2201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lanemo Myhrinder A, Hellqvist E, Sidorova E, Söderberg A, Baxendale H, Dahle C, Willander K, Tobin G, Bäckman E, Söderberg O et al (2008) A new perspective: molecular motifs on oxidized LDL, apoptotic cells, and bacteria are targets for chronic lymphocytic leukemia antibodies. Blood 111: 3838–3848 [DOI] [PubMed] [Google Scholar]
- Sammicheli S, Kuka M, Di Lucia P, de Oya NJ, De Giovanni M, Fioravanti J, Cristofani C, Maganuco CG, Fallet B, Ganzer L et al (2016) Inflammatory monocytes hinder antiviral B cell responses. Sci Immunol 1: eaah6789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sommerstein R, Flatz L, Remy MM, Malinge P, Magistrelli G, Fischer N, Sahin M, Bergthaler A, Igonet S, ter Meulen J et al (2015) Arenavirus glycan shield promotes neutralizing antibody evasion and protracted infection. PLoS Pathog 11: e1005276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stamatopoulos K, Belessi C, Hadzidimitriou A, Smilevska T, Kalagiakou E, Hatzi K, Stavroyianni N, Athanasiadou A, Tsompanakou A, Papadaki T et al (2005) Immunoglobulin light chain repertoire in chronic lymphocytic leukemia. Blood 106: 3575–3583 [DOI] [PubMed] [Google Scholar]
- Steininger C, Rassenti LZ, Vanura K, Eigenberger K, Jäger U, Kipps TJ, Mannhalter C, Stilgenbauer S, Popow‐Kraupp T (2009) Relative seroprevalence of human herpes viruses in patients with chronic lymphocytic leukaemia. Eur J Clin Invest 39: 497–506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steininger C, Widhopf GF, Ghia EM, Morello CS, Vanura K, Sanders R, Spector D, Guiney D, Jäger U, Kipps TJ (2012) Recombinant antibodies encoded by IGHV1‐69 react with pUL32, a phosphoprotein of cytomegalovirus and B‐cell superantigen. Blood 119: 2293–2301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevenson FK, Forconi F, Packham G (2014) The meaning and relevance of B‐cell receptor structure and function in chronic lymphocytic leukemia. Semin Hematol 51: 158–167 [DOI] [PubMed] [Google Scholar]
- Tonti E, Jiménez de Oya N, Galliverti G, Moseman EA, Di Lucia P, Amabile A, Sammicheli S, De Giovanni M, Sironi L, Chevrier N et al (2013) Bisphosphonates target B cells to enhance humoral immune responses. Cell Rep 5: 323–330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yan X‐J, Albesiano E, Zanesi N, Yancopoulos S, Sawyer A, Romano E, Petlickovski A, Efremov DG, Croce CM, Chiorazzi N (2006) B cell receptors in TCL1 transgenic mice resemble those of aggressive, treatment‐resistant human chronic lymphocytic leukemia. Proc Natl Acad Sci USA 103: 11713–11718 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang S, Kipps TJ (2014) The pathogenesis of chronic lymphocytic leukemia. Annu Rev Pathol 9: 103–118 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix
Expanded View Figures PDF
Table EV1
Table EV2
Table EV3
Source Data for Expanded View
Review Process File
Source Data for Figure 1A
Source Data for Figure 1B
Source Data for Figure 1C
Source Data for Figure 2A
Source Data for Figure 2B
Source Data for Figure 2C
Source Data for Figure 2D


