Abstract
In this prospective referring-physician–based survey, we investigated the definite clinical impact of 68Ga-DOTATATE PET/CT on managing patients with neuroendocrine tumors (NETs). Methods: We prospectively studied 130 patients with 68Ga-DOTATATE PET/CT referred for initial or subsequent management decisions (NCT02174679). Referring physicians completed one questionnaire before the scan (Q1) to indicate the treatment plan without PET/CT information, one immediately after review of the imaging report to denote intended management changes (Q2), and one 6 mo later (Q3) to verify whether intended changes were in fact implemented. To further validate the Q3 responses, a systematic electronic chart review was conducted. Results: All 3 questionnaires were completed by referring physicians for 96 of 130 patients (74%). 68Ga-DOTATATE PET/CT resulted in intended management changes (Q2) in 48 of 96 patients (50%). These changes were finally implemented (Q3) in 36 of 48 patients (75%). Q3 responses were confirmed in all patients with an available electronic chart (36/96; 38%). Conclusion: This prospective study confirmed a significant impact of 68Ga-DOTATATE PET/CT on the intended management of patients with NETs (50% of changes) and notably demonstrated a high implementation rate (75%) of these intended management changes.
Keywords: neuroendocrine tumors, somatostatin receptor, PET/CT, DOTATATE, impact on implemented management
Somatostatin receptor PET/CT imaging using 68Ga-DOTATATE is reproducible (1) and affects patient management (2). Recent retrospective analyses suggest that intended management changes are in fact implemented (2). We recently reported intended management changes in 60% of patients with NET after 68Ga-DOTATATE PET/CT imaging (3). In this subsequent prospective study, we investigated the definite clinical impact of 68Ga-DOTATATE PET/CT on NET patient management by comparing intended with actually implemented treatment strategies.
MATERIALS AND METHODS
Registration and Authorization
After submitting an initial investigational new drug application for 100 patients (NCT01873248) (3), we obtained an expanded-access investigational new drug number (122332; NCT02174679) from the Food and Drug Administration that allowed us to study an additional 300 patients. We enrolled 130 patients with suspected or histologically proven NETs who were referred to the University of California, Los Angeles, for a 68Ga-DOTATATE PET/CT scan. That institution’s review board approved the protocol, the informed consent forms, the participant information forms, and the prospective referring physician questionnaires (approval 12-001920). All patients provided written informed consent.
Patient Preparation and Image Acquisition
A standard 68Ga-DOTATATE PET/CT protocol was used (3). The median injected dose of 68Ga-DOTATATE was 185 MBq (5 mCi) (range, 85.1–210.9 MBq [2.3–5.7 mCi]). The median tracer uptake time was 61 min (range, 46–97 min). Images were acquired using a Biograph 64 or Biograph mCT (Siemens) after intravenous (110–120 mL of Omnipaque 350; GE Healthcare) and oral contrast application.
Survey
Referring physicians completed one questionnaire before the scan to indicate the treatment plan without 68Ga-DOTATATE PET/CT information (Q1), a second questionnaire immediately after receipt of the written clinical report and the images (on a DVD) to denote intended management changes (Q2), and a final questionnaire mailed 6 mo later to verify whether any intended changes were in fact implemented (Q3). To further verify and confirm the validity of the Q3 responses, the electronic chart was reviewed when available.
RESULTS
Referring Physicians and Questionnaires
Fifty-six different physicians referred 130 patients. Ninety-six complete sets of 3 questionnaires were returned (response rate, 74%) (Fig. 1). Q1 was completed within a median of 11 d before the scan (range, 0–59 d). Q2 and Q3 were completed within a median of 28 d (range, 1–281 d) and 207 d (range, 89–725 d) after the scan. In 14 patients, because of delayed responses by the referring physicians, Q2 and Q3 were completed at the same time. In the 82 remaining patients, the median interval between Q2 and Q3 completion was 183 d (range, 131–713 d).
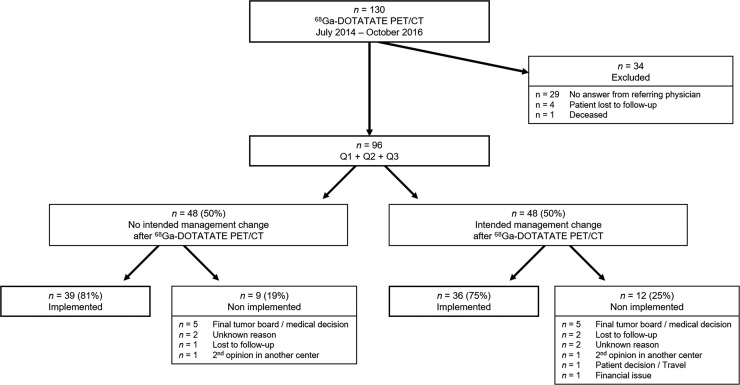
FIGURE 1.
Patient flowchart for inclusion and management change.
Patient Population
The demographics of the 96 patients are presented in Table 1.
TABLE 1.
Patient Characteristics
| Parameter | Primary staging, n = 23 (24%) | Restaging, n = 73 (76%) |
| Primary tumor location | ||
| Chest | 1 | 9 |
| Pancreas | 5 | 16 |
| Small bowel | 6 | 31 |
| Colon | 0 | 2 |
| Other | 2 | 5 |
| Unknown | 9 | 10 |
| Tumor grade | ||
| Low | 7 | 35 |
| Intermediate | 4 | 17 |
| High | 0 | 6 |
| Unknown | 12 | 15 |
| Tumor stage | ||
| I | 0 | 7 |
| II | 0 | 2 |
| III | 1 | 10 |
| IV | 2 | 40 |
| Unknown | 20 | 14 |
| Prior treatment | ||
| Surgery | 4 | 50 |
| Chemotherapy | 0 | 15 |
| Octreotide | 1 | 42 |
| PRRT | 0 | 6 |
| Other | 0 | 20 |
| Prior SSTR imaging | ||
| SPECT | 5 | 15 |
| PET | 2 | 8 |
| Both | 1 | 1 |
PRRT = peptide receptor radionuclide therapy; SSTR = somatostatin receptor.
Impact on Intended Patient Management
The intended treatment strategies before (Q1) and after (Q2) 68Ga-DOTATATE PET/CT, and the final implemented management (Q3), are summarized in Table 2. 68Ga-DOTATATE PET/CT resulted in intended management changes in 48 of 96 patients (50%) (Fig. 1).
TABLE 2.
Summary of Different Treatment Options as Indicated on Q1, Q2, and Q3
| Option | Considered before DOTATATE (Q1) | Intended after DOTATATE (Q2) | Finally implemented (Q3) |
| Surgery | 21 (22%) | 18 (19%) | 17 (18%) |
| Chemotherapy | 17 (18%) | 12 (13%) | 13 (14%) |
| XRT | 7 (7%) | 4 (4%) | 3 (3%) |
| Octreotide | 43 (45%) | 32 (33%) | 34 (35%) |
| PRRT | 10 (10%) | 12 (13%) | 9 (9%) |
| w/w | 27 (28%) | 33 (34%) | 31 (32%) |
| Other | 12 (13%) | 6 (6%) | 3 (3%) |
DOTATATE = 68Ga-DOTATATE PET/CT; XRT = external-beam radiotherapy; PRRT = peptide receptor radionuclide therapy; w/w = watch and wait.
Total number of items is higher than 100% because multiple treatment options were possible for Q1, Q2, and Q3.
Implementation of Intended Management
Intended management changes after 68Ga-DOTATATE PET/CT (as indicated in Q2) were in fact implemented in 36 of 48 patients (75%) as specified in Q3 (Fig. 1).
Twelve of the 21 patients (57%) initially considered for surgery were eventually switched to conservative treatment. Conversely, 8 of 75 patients (11%) in whom surgery was not initially considered had surgery (Fig. 2). Nine of 17 patients (53%) who were initially scheduled for chemotherapy were eventually switched to alternative strategies. Nine of 69 patients (13%) in whom some treatment was considered were finally switched to watch and wait.
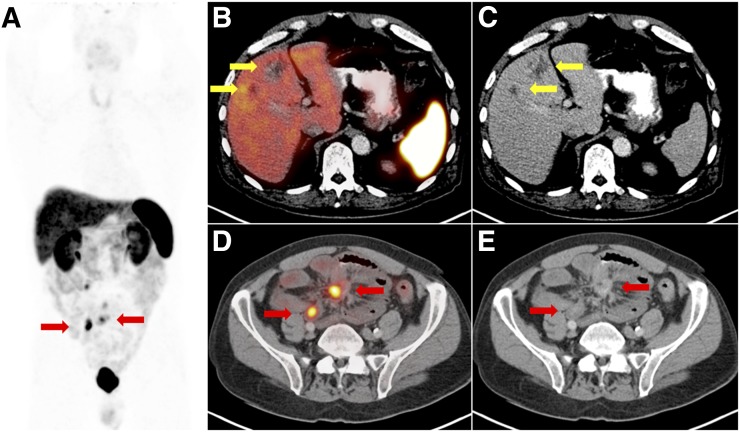
FIGURE 2.
Example 62-y-old man referred for initial staging of metastatic small-bowel low-grade NET. CT and MRI showed mesenteric mass, enlarged abdominal lymph nodes, and equivocal liver lesions (hemangiomas vs. metastases). He had prior slightly increased level of 24-h urine 5-hydroxyindoleacetic acid, supporting suspicion of hepatic metastases. Referring physician indicated in Q1 that patient was being considered for octreotide treatment. 68Ga-DOTATATE PET/CT ruled out hepatic metastasis (yellow arrows) and confirmed mesenteric primary site and lymph node involvement (red arrows), as seen on 68Ga-DOTATATE PET maximum-intensity projection (A), fused 68Ga-DOTATATE PET/CT axial views (B and D), and corresponding CT axial views (C and E). In Q2, referring physician indicated intended management change toward surgery, which was confirmed later in Q3. Patient finally underwent resection of small-bowel NET with wide margins. Follow-up MRI and urinary carcinoid biomarker showed no disease recurrence.
Implementation rates were similar in the small group of patients in whom Q2 and Q3 were completed at the same time (10/14; 71%) and in the 82 patients with a Q2-to-Q3 completion interval of 131–713 d (65/82; 79%).
The intended management (as indicated in Q2) was not implemented in 21 of the 96 patients (22%; Table 3). Reasons for failure to implement were final tumor board or medical decision (10/21; 48%), second opinion in another institution (2/21; 10%), patient decision (1/21; 5%), financial issue (1/21; 5%), loss to follow-up (3/21; 14%), or unknown (4/21; 19%).
TABLE 3.
Detailed Treatment Management of 21 Patients with No Implemented Intended Management
| Considered before DOTATATE (Q1) | Intended after DOTATATE (Q2) | Final implemented management (Q3) | Reason for nonimplementation |
| Surgery | → CTx/other | → CTx | Tumor board/final medical decision |
| Surgery | → w/w | → Surgery | Tumor board/final medical decision |
| w/w | → Surgery | → Octreotide/other | Tumor board/final medical decision |
| CTx/PRRT | → CTx | → XRT/other | Tumor board/final medical decision |
| CTx/PRRT | → PRRT | → CTx/PRRT | Tumor board/final medical decision |
| CTx/PRRT/octreotide/other | → CTx/PRRT/octreotide/other | → Surgery/CTx/octreotide | Tumor board/final medical decision |
| XRT | → XRT | → Surgery/CTx | Tumor board/final medical decision |
| PRRT | → PRRT | → Octreotide | Tumor board/final medical decision |
| PRRT/octreotide | → PRRT/octreotide | → CTX/octreotide | Tumor board/final medical decision |
| Surgery | → Surgery | → Surgery/other | Tumor board/final medical decision |
| Surgery/octreotide | → Surgery | → Octreotide/w/w | Second opinion in another institution |
| Octreotide | → Octreotide | → PRRT | Second opinion in another institution |
| Surgery/XRT/w/w | → XRT | → w/w | Patient decision/travel |
| CTx | → PRRT | → CTX/octreotide | Financial issue |
| Surgery | → w/w | Unknown | Lost to follow-up |
| CTx/XRT/octreotide | → CTx/other | Unknown | Lost to follow-up |
| Other | → Other | Unknown | Lost to follow-up |
| Other | → Octreotide/other | Unknown | Unknown |
| Octreotide/w/w | → Surgery/octreotide/w/w | Unknown | Unknown |
| Surgery | → Surgery | Unknown | Unknown |
| w/w | → w/w | Unknown | Unknown |
DOTATATE = 68Ga-DOTATATE PET/CT; CTx = chemotherapy; XRT = external-beam radiotherapy; PRRT= peptide receptor radionuclide therapy; w/w = watch and wait.
In 36 of 96 patients (38%) an electronic chart review of patients managed at our institution was possible (all other patients were referred from outside institutions). All implemented management changes as stated in Q3 were confirmed (median interval of 14 mo; range, 2–29 mo) after PET.
DISCUSSION
This prospective survey enabled a systematic assessment of how referring physicians act on 68Ga-DOTATATE PET/CT study information. Management changes were intended in 50% of the patients, and these changes were implemented in 75% of these cases.
An impact on management of any diagnostic test suggests value for patients and is a prerequisite for widespread acceptance. The broad coverage of 18F‐FDG PET/CT by the Centers for Medicare and Medicaid Services was the result of the National Oncology PET Registry, which showed a significant impact of 18F-FDG PET/CT on the management of tens of thousands of cancer patients (40% of management changes) (4). However, one concern about the National Oncology PET Registry is that intended management changes may not have been implemented (5,6). In the current study, 68Ga-DOTATATE PET/CT resulted in intended management changes in 48 of 96 patients (50%), which is comparable to results from prior retrospective studies (2,3,7–11). However, no prospective study has elucidated prospectively the rate of implemented management changes. We demonstrated a high implementation rate of these intended management changes (36/48; 75%).
Potential reasons for lack of implementation may be conflicting results and conclusions made by tumor boards versus treating physicians, resulting in different recommendations. Q2 timing did not uniformly allow clinicians to take all other factors into account that can affect final decision making. Moreover, a few patients elected not to follow the intended treatment plan for personal or financial reasons or decided to obtain a second opinion at another institution (Table 3).
A major limitation of this study is a possible responder bias (12–14). However, a high number of different referring physicians (>50) returned the questionnaires at a high response rate of 74%, indicating limited bias. If all nonresponding physicians had indicated that intended management was not implemented, the overall implementation rate would still have been 58%. In addition, we confirmed questionnaire responses via systematic electronic chart review in 36 of 96 patients (38%).
CONCLUSION
This prospective referring physician–based survey confirmed the significant impact of 68Ga-DOTATATE PET/CT on intended management of patients with NET (50% of changes) and notably demonstrated a high implementation rate (75%) of these intended management changes.
DISCLOSURE
Dr. Jeremie Calais is the recipient of a grant from the Fondation ARC pour la recherche sur le cancer (SAE20160604150). Dr. Johannes Czernin is the recipient of a grant from the U.S. Department of Energy (DE SC 0012363) and is a founder of Trethera Therapeutics and Sofie Biosciences. Dr. Wolfgang Fendler received a scholarship from the German Research Foundation (Deutsche Forschungsgemeinschaft, DFG, grant 807122). Dr. Joseph R. Pisegna is the recipient of a grant from the National Institutes of Health, NIDDK (U01 DK-14-028). No other potential conflict of interest relevant to this article was reported.
REFERENCES
- 1.Fendler WP, Barrio M, Spick C, et al. 68Ga-DOTATATE PET/CT interobserver agreement for neuroendocrine tumor assessment: results of a prospective study on 50 patients. J Nucl Med. 2017;58:307–311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Barrio M, Czernin J, Fanti S, et al. The impact of somatostatin receptor–directed PET/CT on the management of patients with neuroendocrine tumor: a systematic review and meta-analysis. J Nucl Med. 2017:58:756–761. [DOI] [PubMed] [Google Scholar]
- 3.Herrmann K, Czernin J, Wolin EM, et al. Impact of 68Ga-DOTATATE PET/CT on the management of neuroendocrine tumors: the referring physician’s perspective. J Nucl Med. 2015;56:70–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hillner BE, Siegel BA, Liu D, et al. Impact of positron emission tomography/computed tomography and positron emission tomography (PET) alone on expected management of patients with cancer: initial results from the National Oncologic PET Registry. J Clin Oncol. 2008;26:2155–2161. [DOI] [PubMed] [Google Scholar]
- 5.Levine MN, Julian JA. Registries that show efficacy: good, but not good enough. J Clin Oncol. 2008;26:5316–5319. [DOI] [PubMed] [Google Scholar]
- 6.Larson SM. Practice-based evidence of the beneficial impact of positron emission tomography in clinical oncology. J Clin Oncol. 2008;26:2083–2084. [DOI] [PubMed] [Google Scholar]
- 7.Panagiotidis E, Alshammari A, Michopoulou S, et al. Comparison of the impact of 68Ga-DOTATATE and 18F-FDG PET/CT on clinical management in patients with neuroendocrine tumors. J Nucl Med. 2017;58:91–96. [DOI] [PubMed] [Google Scholar]
- 8.Skoura E, Michopoulou S, Mohmaduvesh M, et al. The impact of 68Ga-DOTATATE PET/CT imaging on management of patients with neuroendocrine tumors: experience from a national referral center in the United Kingdom. J Nucl Med. 2016;57:34–40. [DOI] [PubMed] [Google Scholar]
- 9.Ambrosini V, Campana D, Bodei L, et al. 68Ga-DOTANOC PET/CT clinical impact in patients with neuroendocrine tumors. J Nucl Med. 2010;51:669–673. [DOI] [PubMed] [Google Scholar]
- 10.Srirajaskanthan R, Kayani I, Quigley AM, Soh J, Caplin ME, Bomanji J. The role of 68Ga-DOTATATE PET in patients with neuroendocrine tumors and negative or equivocal findings on 111In-DTPA-octreotide scintigraphy. J Nucl Med. 2010;51:875–882. [DOI] [PubMed] [Google Scholar]
- 11.Has Simsek D, Kuyumcu S, Turkmen C, et al. Can complementary 68Ga-DOTATATE and 18F-FDG PET/CT establish the missing link between histopathology and therapeutic approach in gastroenteropancreatic neuroendocrine tumors? J Nucl Med. 2014;55:1811–1817. [DOI] [PubMed] [Google Scholar]
- 12.Seltzer MA, Yap CS, Silverman DH, et al. The impact of PET on the management of lung cancer: the referring physician’s perspective. J Nucl Med. 2002;43:752–756. [PubMed] [Google Scholar]
- 13.Cartwright A. Professionals as responders: variations in and effects of response rates to questionnaires, 1961-77. Br Med J. 1978;2:1419–1421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Donaldson GW, Moinpour CM, Bush NE, et al. Physician participation in research surveys: a randomized study of inducements to return mailed research questionnaires. Eval Health Prof. 1999;22:427–441. [DOI] [PubMed] [Google Scholar]