Abstract
The present study investigated the inhibitory effect of curcumin on human breast cancer MCF-7 cells and investigated the potential underlying molecular mechanisms. MCF-7 cells were cultured with curcumin at different concentrations and time points. The effects of curcumin treatment on breast cancer cell proliferation were studied using a MTT assay. Reverse transcription-quantitative polymerase chain reaction and western blot analysis were used to assess the mRNA and protein expression levels of B-cell lymphoma 2 (Bcl-2) and Bcl-2-associated X (Bax), nuclear factor-κ-light-chain-enhancer of activated B cells (NF-κB) and inhibitor of NF-κB-α (IκBα). The proliferation of MCF-7 cells in the group treated with curcumin was markedly decreased compared with the control, with the greatest inhibitory effect at a concentration of 20 µM. The expression of Bax mRNA was increased and Bcl-2 mRNA expression was decreased compared with the control. Additionally, protein expression of NF-κB and IκB was increased. The data indicate that curcumin is able to inhibit breast cancer cell proliferation, possibly by regulating the NF-κB signaling pathway.
Keywords: curcumin, MCF-7, proliferation, apoptosis, nuclear factor-κ-light-chain-enhancer of activated B cells
Introduction
Breast cancer is the most frequent type of malignancy in females observed worldwide (1). The incidence of breast cancer is increasing. The prognosis of patients with late-stage breast cancer is closely associated with metastasis, as once the tumor metastasizes; there are few effective treatment options available (2). Tumor initiation and development is a complicated process and is associated with the loss of normal regulatory pathways in cell proliferation, differentiation and apoptosis (3,4).
Curcumin, a well-known chemopreventive agent extracted from turmeric, has a history of 5,000 years (5,6). In recent years, studies have indicated that curcumin is able to inhibit proliferation and survival, induce apoptotic and non-apoptotic (autophagocytosis and paraptosis) cell death, and reduce invasion and migration in various types of malignant cancer cells (7–9). Through regulation of the expression of genes associated with programmed cell death, curcumin causes a high degree of apoptosis in human breast cancer cells (10). However, few studies have been performed that investigate the underlying mechanisms of curcumin as a potential agent in breast cancer therapy. Notably, curcumin is a potent inhibitor of nuclear factor-κ-light-chain-enhancer of activated B cells (NF-κB), indicating its potential role in inhibiting tumor pathogenesis in a number of human malignancies and has a dose-dependent pharmacological effect (11,12). The present study aimed to investigate the anticancer effects of curcumin in MCF-7 cells and to investigate the underlying mechanisms.
Materials and methods
Cells and reagents
Dulbecco's modified Eagle's medium (DMEM) and fetal bovine serum (FBS) were obtained from HyClone™ (GE Healthcare, Chicago, IL, USA). Curcumin (purity >98%) was supplied by Sigma-Aldrich (Merck KGaA, Darmstadt, Germany).
Cell culture
Human breast cancer MCF-7 cell line was purchased from Shanghai Institute of Cell Biology, Chinese Academy of Sciences (Shanghai, China). The MCF-7 cells were cultured in DMEM supplemented with 10% FBS, 100 U/ml penicillin and 100 U/ml streptomycin (Sigma-Aldrich; Merck KGaA) in a humidified atmosphere of 95% air with 5% CO2 at 37°C.
Cell viability and proliferation assays
The viability and proliferation of MCF-7 cells were quantified using a standard MTT reduction assay. To measure the effects of curcumin, MCF-7 cells were seeded into 96-well plates at a density of 2×103 cells/well and allowed to adhere overnight. The density of viable cells was determined in a control plate. Curcumin was prepared immediately prior to use and added to test wells at a range of concentrations (2.5, 5, 10, 20 and 40 µM) for 24, 48 and 72 h. MTT (10 µl MTT/100 µl DMEM; Sigma-Aldrich; Merck KGaA) solution was added to the wells. Optical density of each culture was read by using a microplate reader at a wavelength of 570 nm.
Flow cytometry
To elucidate the mechanism underlying curcumin treatment on MCF-7 cells, cell cycle analysis by flow cytometry was performed. Approximately 1–5×106 MCF-7 cells were treated with 20 µM curcumin at 24, 48 and 72 h after the cells were collected, in accordance with the Annexin V-fluorescein isothiocyanate (FITC) kit manufacturer's protocol (ab14085; Abcam, Cambridge, MA, USA). Briefly, 195 µl cell suspension was added to 5 µl Annexin V-FITC solution, and the cells were incubated at room temperature for 10 min. The cells were then washed with PBS and suspended in 190 µl binding buffer from the kit. A total of 10 µl propidium iodide was added, and cells undergoing early apoptosis was detected by flow cytometry (BD FACSCalibur™; BD Biosciences, Franklin Lakes, NJ, USA). The BD FACSCalibur was equipped with a dual laser (488 and 635 nm) and CellQuest version 3.0 software (BD Biosciences).
Reverse transcription-quantitative polymerase chain reaction (RT-qPCR)
Total RNA was extracted from 1–5×106 MCF-7 cells co-cultured with curcumin for various durations using 1 ml TRIzol® reagent (Invitrogen; Thermo Fisher Scientific, Waltham, MA, USA), according to the manufacturer's protocol. The RNA sample was dissolved in RNase-free water and quantified spectrophotometrically. PrimeScript™ RT Master mix was used to transcribe cDNA, according to the manufacturer's protocol (Takara Biotechnology Co., Ltd., Dalian, China). The EzOmics SYBR qPCR kit was purchased from Biomics USA Inc., (Palo Alto, CA, USA), which included 5 µl cDNA template and 15 µl reaction mixture, containing 10 µl 2X SYBR Green mix, 0.5 µM forward primer, 0.5 µM reverse primer and RNase-free H2O. RT-qPCR analysis was performed to detect the relative expression levels of B-cell lymphoma 2 (Bcl-2), Bcl-2-associated X (Bax) and β-actin. β-actin was used as an internal control for input RNA. The amplification procedure was as follows: 40 cycles of 95°C for 30 sec, 95°C for 5 sec, 95°C for 30 sec and 72°C for 30 sec, followed by 95°C for 1 min, 95°C for 30 sec and 75°C for 30 sec. Primers were designed using the Primer Express version 3.0 software package (Applied Biosystems; Thermo Fisher Scientific, Inc.) for the expression experiments. The primers (Sangon Biotech Co., Ltd., Shanghai, China) used are as follows: Bcl-2 forward, 5′-GTTTGATTTCTCCTGGCTGTCTC-3′ and reverse, 5′-GAACCTTTTGCATATTTGTTTGG-3′; Bax forward, 5′-AAGCTGAGCGAGTGTCTCAAG-3′ and reverse, 5′-CAAAGTAGAAAAGGGCGACAAC-3′; β-actin forward, 5′-TGGCACCCAGCACAATGAA-3′ and reverse, 5′-CTAAGTCATAGTCCGCCTAGAAGCA-3′. The mRNA expression of each gene was normalized to that of β-actin. Data were analyzed using ABI Prism 7900 Sequence Detection system version 2.3 software (Applied Biosystems; Thermo Fisher Scientific, Inc.). The relative mRNA expression was calculated using the comparative Cq method (2−ΔΔCq) (13).
Western blot analysis
The BCA Protein Assay kit (Santa Cruz Biotechnology, Inc., Santa Cruz, CA, USA) was used to semi-quantitatively assess protein concentration. A total of 50 µg protein from each well was loaded onto a 10% SDS-PAGE and, following this, electroblotted onto a nitrocellulose membrane. The membranes were blocked in TBST (pH 7.4; 20 mM Tris HCl, 150 mM NaCl and 0.1% Tween-20) containing 5% skimmed milk for 2 h at 4°C, and then incubated for 16 h at 4°C with anti-NF-κB p65 (1:2,000; cat. no. SC-8008; Santa Cruz Biotechnology, Inc.) and IκB (1:1,000; cat. no. SC-371; Santa Cruz Biotechnology, Inc.) antibodies. The membrane was washed twice using TBS and 0.05% Tween-20 (Biosharp Life Sciences, Hefei, China), and subsequently incubated at room temperature for 2 h with horseradish peroxidase-conjugated rabbit anti-mouse immunoglobulin G (1:1,000; cat. no. SC-358922; Santa Cruz Biotechnology, Inc.). An electrochemiluminescence kit (Beyotime Institute of Biotechnology, Haimen, China) was used to visualize the immunoreactions according to the manufacturer's instructions.
Statistical analysis
Statistical analyses were performed with one-way analysis of variance followed by Bonferroni test or t-test when appropriate using SPSS version 10.0 statistical software (SPSS, Inc., Chicago, IL, USA). P<0.05 was used to indicate a statistically significant difference. Data of continuous variables are presented as the mean ± standard deviation.
Results
Inhibition of cell growth by curcumin treatment
Following treatment of the MCF-7 cells for 24, 48 and 72 h with curcumin, the growth inhibitory activity of curcumin was determined, and then the viability of the cells was measured by MTT assay. Briefly, MCF-7 cells exposed to curcumin exhibited a significant decrease in cell proliferation in a time- and dose-dependent manner compared with those treated with control (P<0.05; Fig. 1).
Figure 1.
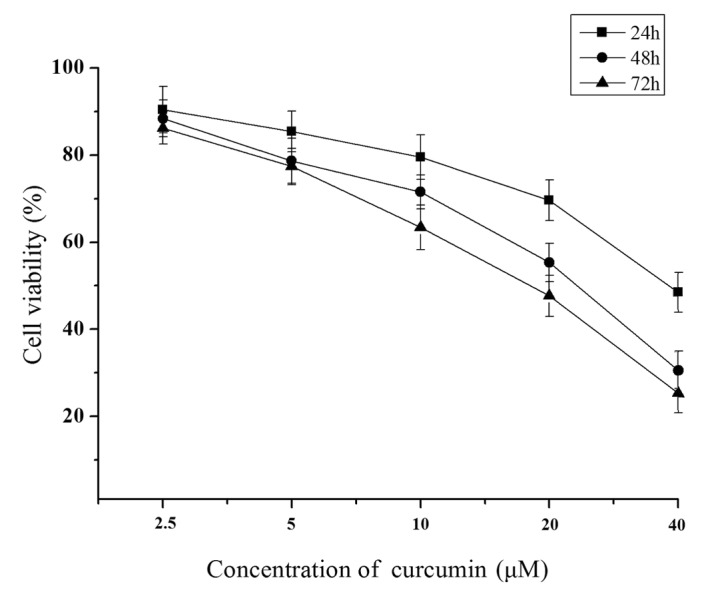
Viability of human breast cancer MCF-7 cells assessed using MTT assay following incubation of cells with 2.5, 5, 10, 20 and 40 µM curcumin for 24, 48 and 72 h. *P<0.05 vs. control.
Effect of curcumin treatment on cell cycle and apoptosis
Following treatment of MCF 7-cells with 20 µM curcumin for 24, 48 and 72 h, the apoptotic rate was 20.52, 28.65 and 36.25%, respectively. Compared with the control group, this was a significant difference at each time point (P<0.05; Table I). Cell cycle measurements revealed that MCF-7 cells treated with curcumin significantly increased the proportion of cells in the G0/G1 phase (P<0.01) and significantly decreased the proportion of cells in the S phase (P<0.01; Table I).
Table I.
Effect of curcumin treatment on cell cycle and apoptosis as determined by flow cytometry.
| Cell cycle, % | |||
|---|---|---|---|
| Time, h | G1/S | G2/M | Apoptosis, % |
| 0 (control) | 35.68 | 65.29 | 4.52 |
| 24 | 36.27a | 56.71a | 20.52a |
| 48 | 52.46a | 36.19a | 28.65a |
| 72 | 65.84a | 15.63a | 36.25a |
Data are presented as the mean ± standard error (n=5).
P<0.05 vs. the control. h, hours.
Effect of curcumin treatment on the levels of Bcl-2 and Bax RNA expression
Compared with the control group, the expression level of bcl-2 mRNA in MCF-7 cells treated with 20 µM curcumin was significantly decreased at treatment at 24, 48 and 72 h, but the level of bax mRNA was significantly increased at 24, 48, and 72 h (P<0.05; Fig. 2).
Figure 2.
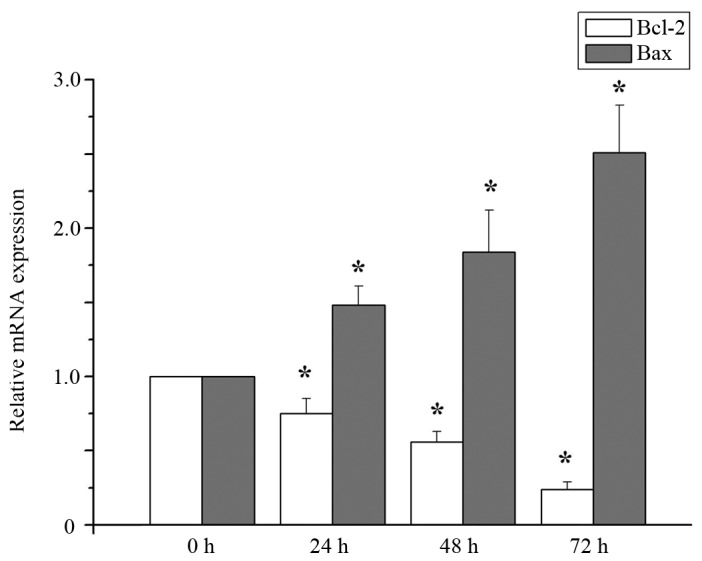
Levels of Bcl-2 and Bax RNA expression. *P<0.05 vs. control. Bcl-2, B-cell lymphoma 2; Bax, Bcl-2-associated X.
Effect of curcumin treatment on NF-κB and IκBα protein expression
Level of NF-κB p65 protein expression was lower, and expression of IκBα was higher in cells treated with 20 µM curcumin at 24, 48 and 72 h, compared with 0 h (P<0.05; Fig. 3).
Figure 3.
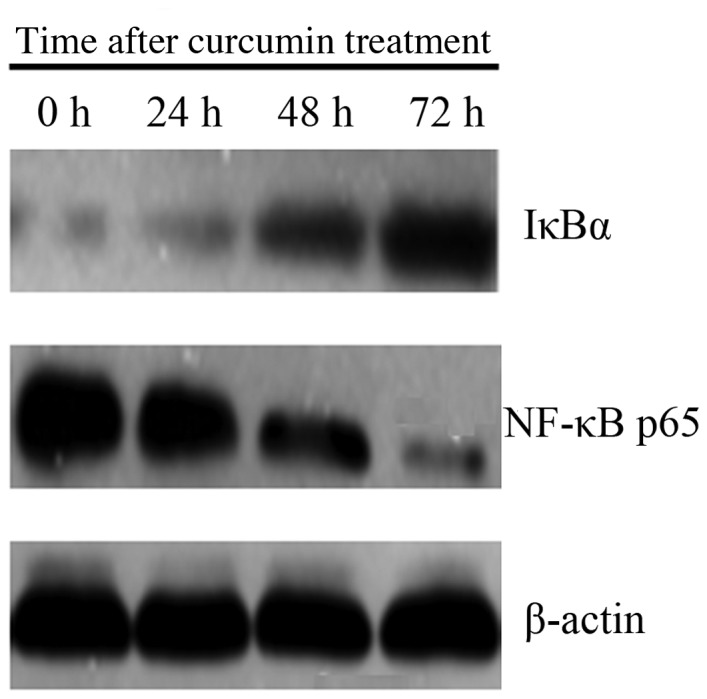
Levels of NF-κB p65 and IκBα protein expression by western blotting. NF-κB, nuclear factor-κ-light-chain-enhancer of activated B cells; IκBα, inhibitor of NF-κB-α.
Discussion
The breast cancer MCF-7 cell line was selected to assess the potential effects of curcumin. The results of the present study demonstrated that curcumin was able to inhibit MCF-7 cell proliferation and promote apoptosis, possibly by regulating the NF-κB signaling pathway.
It is well known that breast cancer is one of the most common malignancies in females and the main cause of cancer-associated mortality of females worldwide (14,15). In breast cancer the complicated process is able to cause the loss of normal regulatory pathways between cell proliferation, differentiation and apoptosis (3). The cytotoxic activity of curcumin in certain types of cancer cells is well known, with many reports highlighting the anti-proliferative effect of curcumin on cells. Curcumin inhibits cell survival and proliferation and leads to apoptosis of lung cancer cells by reducing the expression level of Axl receptor tyrosine kinase and affecting Axl activation of non-small cell lung cancer (16). Curcumin significantly suppressed cell growth, decreased clonogenic potential, inhibited migration and invasion and induced apoptosis and cell cycle arrest in pancreatic cancer cells, liver cancer HepG2 cells and prostate cancer DU-145 cells (17,18). It has been reported that a high concentration of curcumin is able to induce apoptosis in human leukemia cells (19). However it has also been demonstrated that curcumin is able to inhibit apoptosis in T lymphocytes (20).
Uncontrolled cell proliferation and inhibition of cell death is central to cancer development. Tumor cells exhibit resistance to apoptosis in order to survive and metastasize. The common features of cancer development, including genetic modification and changes in apoptotic pathways in the pathogenesis, can provide an insight into therapeutic targets. Treatment strategies that are designed to destroy the cancer cells by activating apoptosis signaling pathways are required, ideally therapies that are able to induce tumor cell-selective apoptosis, and no harmful effects on normal cells (21). NF-κB is a critical regulator of fundamental cell functions, including cell proliferation and survival (22). The mammalian NF-κB family consists of five transcription factors: p65 (RelA), RelB, c-Rel, p105/p50 (NF-κB1) and p100/p52 (NF-κB2) (23). RelA, RelB and c-Rel are synthesized as final proteins, and all of the members can form homo- and heterodimers and shuttle from the cytoplasm to the nucleus in response to cell stimulation (23). NF-κB transcription factors are characterized by the presence of a highly-conserved Rel homology domain (RHD), which is responsible for dimerization, DNA binding and interaction with the inhibitor of κB (IκB) proteins (24). The IκB proteins, including IκBα, IκBβ, IκBε, IκBγ, Bcl-3 and the precursor Rel proteins p100 and p105, are characterized by the presence of multiple ankyrin repeats, which are protein-protein interaction domains that interact with NF-κB via the RHD (24). Therefore, the present study investigated the expression of NF-κB p65 and IκBa in NF-κB pathway. The present study aimed to investigate the anticancer effects of curcumin in breast cancer MCF-7 cells and to further investigate the molecular mechanisms in human breast cancer cells. The results of the present study revealed that proliferation of MCF-7 cells treated with curcumin was markedly decreased in a concentration- and time-dependent manner. The inhibitory effect of curcumin was the greatest at a concentration of 20 µM. mRNA expression of Bax in cells treated with curcumin was increased and Bcl-2 expression was decreased compared with the non-treated cells. Protein expression of NF-κB p65 was decreased and IκB was increased.
In conclusion, curcumin was able to inhibit proliferation, and the potential mechanism may be associated with the regulation of the NF-κB signaling pathway by curcumin.
Acknowledgements
The authors thank the Central Research Laboratory, The Second Hospital of Shandong University (Shandong, China) for technical assistance and support. The present study was supported by grants from the National Natural Science Foundation of China (grant no. 81400072), the Natural Science Foundation of Shandong Province (grant nos. ZR2016HM67, 2013HQ047 and ZR2013HM103), Science and Technology Development Project of Shandong (grant nos. 2016GSF201044 and 2016GSF201203) and the Medical and Health Science Technology Development Plan Project of Shandong Province (grant no. 2015WS0307).
References
- 1.Pu Z, Yuan X, Zhang X, Chen Q, Xie H. Meta-analysis on the association between CYP2D6*10 gene polymorphism and disease free survival of breast cancer patients receiving tamoxifen treatment in Asia. Bangladesh J Pharmacol. 2014;9:652–662. doi: 10.3329/bjp.v9i4.20849. [DOI] [Google Scholar]
- 2.Li Z, Kang Y. Emerging therapeutic targets in metastatic progression: A focus on breast cancer. Pharmacol Ther. 2016;161:79–96. doi: 10.1016/S1525-0016(16)33011-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chung SS, Vadgama JV. Curcumin and epigallocatechin gallate inhibit the cancer stem cell phenotype via down-regulation of STAT3-NFκB signaling. Anticancer Res. 2015;35:39–46. [PMC free article] [PubMed] [Google Scholar]
- 4.Ramachandran C, You W. Differential sensitivity of human mammary epithelial and breast carcinoma cell lines to curcumin. Breast Cancer Res Treat. 1999;54:269–278. doi: 10.1023/A:1006170224414. [DOI] [PubMed] [Google Scholar]
- 5.Li YB, Gao JL, Zhong ZF, Hoi PM, Lee SM, Wang YT. Bisdemethoxycurcumin suppresses MCF-7 cells proliferation by inducing ROS accumulation and modulating senescence-related pathways. Pharmacol Rep. 2013;65:700–709. doi: 10.1016/S1734-1140(13)71048-X. [DOI] [PubMed] [Google Scholar]
- 6.Ramachandran C, Rodriguez S, Ramachandran R, Nair Raveendran PK, Fonseca H, Khatib Z, Escalon E, Melnick SJ. Expression profiles of apoptotic genes induced by curcumin in human breast cancer and mammary epithelial cell lines. Anticancer Res. 2005;25:3293–3302. [PubMed] [Google Scholar]
- 7.Basnet P, Skalko-Basnet N. Curcumin: An anti-inflammatory molecule from a curry spice on the path to cancer treatment. Molecules. 2011;16:4567–4598. doi: 10.3390/molecules16064567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chen Y, Shu W, Chen W, Wu Q, Liu H, Cui G. Curcumin, both histone deacetylase and p300/CBP-specific inhibitor, represses the activity of nuclear factor kappa B and Notch 1 in Raji cells. Basic Clin Pharmacol Toxicol. 2007;101:427–433. doi: 10.1111/j.1742-7843.2007.00142.x. [DOI] [PubMed] [Google Scholar]
- 9.Goel A, Kunnumakkara AB, Aggarwal BB. Curcumin as ‘Curecumin’: from kitchen to clinic. Biochem Pharmacol. 2008;75:787–809. doi: 10.1016/j.bcp.2007.08.016. [DOI] [PubMed] [Google Scholar]
- 10.Wang Y, Yu J, Cui R, Lin J, Ding X. Curcumin in treating breast cancer: A review. J Lab Autom. 2016;21:723–731. doi: 10.1177/2211068216655524. [DOI] [PubMed] [Google Scholar]
- 11.Hatcher H, Planalp R, Cho J, Torti FM, Torti SV. Curcumin: From ancient medicine to current clinical trials. Cell Mol Life Sci. 2008;65:1631–1652. doi: 10.1007/s00018-008-7452-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lin YG, Kunnumakkara AB, Nair A, Merritt WM, Han LY, Armaiz-Pena GN, Kamat AA, Spannuth WA, Gershenson DM, Lutgendorf SK, et al. Curcumin inhibits tumor growth and angiogenesis in ovarian carcinoma by targeting the nuclear factor-kappaB pathway. Clin Cancer Res. 2007;13:3423–3430. doi: 10.1158/1078-0432.CCR-06-3072. [DOI] [PubMed] [Google Scholar]
- 13.Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) method. Methods. 2001;25:402–408. doi: 10.1006/meth.2001.1262. [DOI] [PubMed] [Google Scholar]
- 14.Siegel R, Naishadham D, Jemal A. Cancer statistics, 2012. CA Cancer J Clin. 2012;62:10–29. doi: 10.3322/caac.20138. [DOI] [PubMed] [Google Scholar]
- 15.Rengarajan T, Nandakumar N, Rajendran P, Haribabu L, Nishigaki I, Balasubramanian MP. D-pinitol promotes apoptosis in MCF-7 cells via induction of p53 and Bax and inhibition of Bcl-2 and NF-κB. Asian Pac J Cancer Prev. 2014;15:1757–1762. doi: 10.7314/APJCP.2014.15.4.1757. [DOI] [PubMed] [Google Scholar]
- 16.Kim KC, Baek SH, Lee C. Curcumin-induced downregulation of Axl receptor tyrosine kinase inhibits cell proliferation and circumvents chemoresistance in non-small lung cancer cells. Int J Oncol. 2015;47:2296–2303. doi: 10.3892/ijo.2015.3004. [DOI] [PubMed] [Google Scholar]
- 17.Zhou X, Su J, Feng S, Wang L, Yin X, Yan J, Wang Z. Antitumor activity of curcumin is involved in down-regulation of YAP/TAZ expression in pancreatic cancer cells. Oncotarget. 2016;7:79076–79088. doi: 10.18632/oncotarget.12596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sha J, Li J, Wang W, Pan L, Cheng J, Li L, Zhao H, Lin W. Curcumin induces G0/G1 arrest and apoptosis in hormone independent prostate cancer DU-145 cells by down regulating Notch signaling. Biomed Pharmacother. 2016;84:177–184. doi: 10.1016/j.biopha.2016.09.037. [DOI] [PubMed] [Google Scholar]
- 19.Iqbal B, Ghildiyal A, Sahabjada, Singh S, Arshad M, Mahdi AA, Tiwari S. Antiproliferative and apoptotic effect of curcumin and TRAIL (TNF Related Apoptosis inducing Ligand) in chronic myeloid leukaemic cells. J Clin Diagn Res. 2016;10:XC01–XC05. doi: 10.7860/JCDR/2016/18507.7579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Somasundaram S, Edmund NA, Moore DT, Small GW, Shi YY, Orlowski RZ. Dietary curcumin inhibits chemotherapy-induced apoptosis in models of human breast cancer. Cancer Res. 2002;62:3868–3875. [PubMed] [Google Scholar]
- 21.Tor YS, Yazan LS, Foo JB, Armania N, Cheah YK, Abdullah R, Imam MU, Ismail N, Ismail M. Induction of apoptosis through oxidative stress-related pathways in MCF-7, human breast cancer cells, by ethyl acetate extract of Dillenia suffruticosa. BMC Complement Altern Med. 2014;14:55. doi: 10.1186/1472-6882-14-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Oida K, Matsuda A, Jung K, Xia Y, Jang H, Amagai Y, Ahn G, Nishikawa S, Ishizaka S, Jensen-Jarolim E, et al. Nuclear factor-ĸB plays a critical role in both intrinsic and acquired resistance against endocrine therapy in human breast cancer cells. Sci Rep. 2014;4:4057. doi: 10.1038/srep04057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Colomer C, Marruecos L, Vert A, Bigas A, Espinosa L. NF-κB members left home: NF-κB-independent roles in cancer. biomedicines. 2017;5 doi: 10.3390/biomedicines5020026. pii: E26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ghosh S, May MJ, Kopp EB. NF-kappa B and Rel proteins: Evolutionarily conserved mediators of immune responses. Annu Rev Immunol. 1998;16:225–260. doi: 10.1146/annurev.immunol.16.1.225. [DOI] [PubMed] [Google Scholar]


