Contemporary cardiac intensive care units (CICU) have evolved into intensive care units for patients with a primary cardiovascular diagnosis.1,2 In response to this changing clinical environment, the American Heart Association (AHA) published a scientific statement advocating for organizational, staffing, and educational evolution in CICUs.3 The AHA statement also provided a roadmap for the future of acute cardiovascular care delivery, which included (1) CICU care delivery in advanced units with unit-based physician staffing (historically referred to as closed units), (2) dedicated cardiac-intensivist training, and (3) a descriptive 3-tiered CICU categorization.3 Herein, we describe the current organizational structures, professional staffing, and medical and technological resources available in CICUs in the United States.
Methods and Results
A 16-question cross-sectional web-based survey (Supplemental Methods; Qualtrics™ platform; Provo, UT, USA) was first emailed to 542 Mission: Lifeline hospital coordinators with a request for the survey to be completed with help from the hospital’s CICU medical director or unit manager between October 2015 and April 2016. The survey was subsequently emailed to 1,389 Acute Coronary Treatment and Intervention Outcomes Network (ACTION) Registry-Get with the Guidelines (GWTG) CICU directors between May and November 2016. To preclude duplicate responses from hospitals present on both contact lists, all responding Mission: Lifeline hospitals were removed from the ACTION Registry-GWTG contact list prior to circulation. The study was approved by the Duke Institutional Review Board. A description of study programs, registries, and statistical methods is provided in the Supplemental Methods.
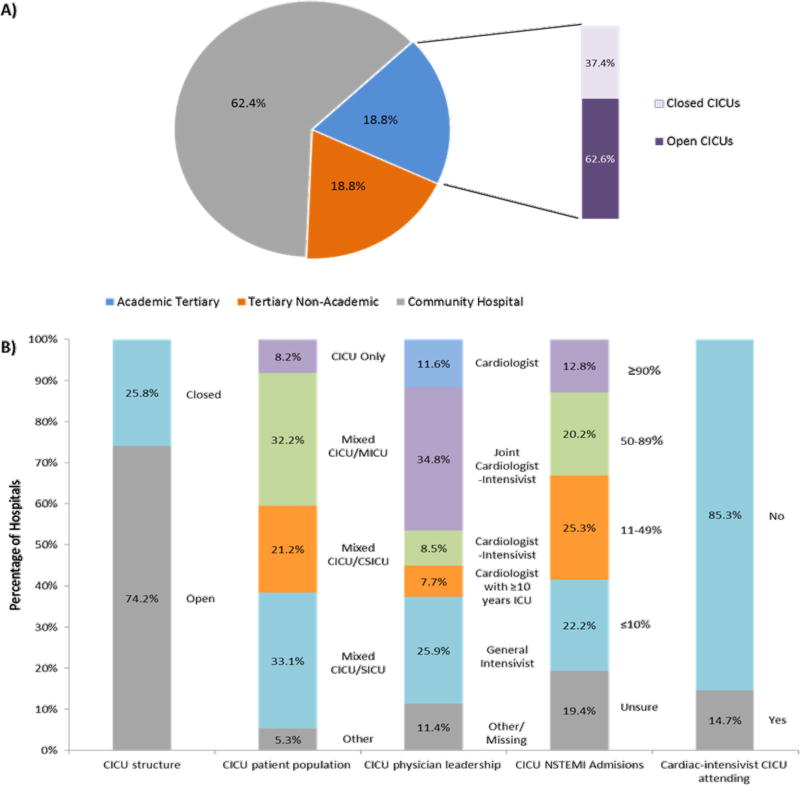
A total of 612 sites (31.7% response rate) completed the survey, including 138 Mission: Lifeline and 474 ACTION-GWTG sites. CICU organization, staffing and resource characteristics stratified by hospital type are presented in Supplemental Table 1. The distribution of academic, tertiary non-academic, and community hospitals was 18.8%, 18.8%, and 62.4%, respectively (Figure 1a). CICUs most frequently (74.2%) had an open staffing model (Figure 1b) and only 8.2% of all centers had dedicated CICUs. There was joint physician leadership by a cardiologist and an intensivist in 34.8% of units, followed by general intensivists (25.9%), and cardiologists (19.3%). Dual-boarded cardiologist-intensivists were physician leaders in 8.5% of CICUs and practicing in 14.7% of units. A dedicated cardiac critical care training program was available in 33 (6.5%) centers. There were no differences between Mission: Lifeline and ACTION Registry-GWTG respondents (Supplemental Table 2).
Figure 1.
Distribution of CICU survey responses by (a) hospital type and (b) organizational structure, leadership, and admission practices
Differences by hospital type and CICU population
Academic medical centers more frequently had a closed unit staffing model (37.4%), dedicated CICUs (23.6%) (Supplemental Table 1), medical leadership by a cardiologist (32.3%) or dual-boarded cardiologist-intensivist (14.1%), an attending cardiologist-intensivist (25.3%), and plans to hire a cardiologist intensivist (18.3%) compared with tertiary non-academic and community hospitals. Trainee education (95.8%) and critical care cardiology subspecialty training programs (24.2%) were also more prevalent in academic centers.
Differences between dedicated CICUs and mixed population ICUs are provided in Supplemental Figure 1 and Supplemental Table 4. Compared with mixed units, dedicated CICUs more frequently were at academic centers; had closed staffing models, cardiology medical leadership, and plans to hire a cardiologist-intensivist; and had established critical care cardiology subspecialty training programs.
CICU Categorization
Only 11.3% of respondents were aware of the AHA position paper on transformation of CICU medical staffing and training models; among whom 52.7% felt their unit currently met Level 1 standards. The prevalence of recommended Level 1 CICU therapeutic technologies, staffing and education initiatives is presented in Supplemental Table 3. Overall only 10.8% of units met Level 1 criteria, including 26.1% of academic, 18.3% of tertiary non-academic, and 3.9% of community sites. In a sensitivity analysis that included cardiologists with ≥10 years of ICU focus as part of the medical leadership the percentage of overall and academic units that met Level 1 criteria rose to 13.2% and 34.8%, respectively.
Comment
In medical and surgical intensive care, a meta-analysis of non-randomized trials reported that high intensity staffing, defined as either mandatory intensivist consultation or closed units with all care primarily directed by an intensivist, was associated with reduced ICU mortality.4 It is important to recognize the limitations of the studies within this meta-analysis, which included small sample sizes, non-contemporary cohorts, and non-randomized design. However, based on the consistency of published evidence, the AHA and other national CICU practice statements recommend unit-based staffing models of CICU care delivery, wherein a single dedicated physician maintains primary responsibility for all patients in the unit, as the preferred approach for advanced CICUs.3,5,6 A recent single center Korean study reported that a transition from an open to a closed model was associated with a reduction in mortality; however, the organizational change also included a staffing shift from general cardiologists to cardiologist-intensivists.7 In this survey, we observed that 74% of hospitals had open staffing models. This proportion is substantially lower than the 55% closed CICU unit structure reported by O’Malley and colleagues in a survey of 123 CICUs. We believe this difference is likely largely due to differences in hospital mix; 78% of responders were from an academic center in the O’Malley study.8 In this study, the relatively low prevalence of best-practice unit-based physician staffing in CICUs suggests a potential opportunity to improve care delivery and patient outcomes. However, as recognized in the AHA scientific statement, such efforts to improve care at hospital and systems levels must take into account the diversity of needs and resources across varied settings and should recognize that the organization and staffing of the CICU likely should be individualized to the care system.3
The European Society of Cardiology was the first organization to advocate advanced training in general intensive care among CICU practitioners followed by the AHA’s scientific statement on the evolution of critical care cardiology, and the ACC’s Core Training Statement (COCATS)-4, which outlined critical care cardiology training levels, but the proportion of hospitals with dual-trained practitioners has remained unclear.3,5,9 A 2012 American and a 2014 Canadian survey reported that 4% and 6.8% of centers, respectively, had an attending cardiologist-intensivist.3,6 Although the number of centers (14.7%) in our report exceeds these historical reports, the overall results may belie the impact the above-mentioned scientific and training statements have had on academic medical centers where 25% of CICUs had a dual-trained attending and 18% were planning to hire or recruit a dual-boarded physician. In addition, nearly one quarter of academic centers self-reported a critical care cardiology training program, and an additional 9.5% were contemplating or in the process of establishing a program. Taken together, our results suggest a potential early national shift in CICU staffing and hiring practices along with an increase in dedicated critical care training pathways in development. Follow-up studies are necessary to accurately evaluate temporal trends, determine the optimal balance between training capacity and workforce needs, and to evaluate whether training cardiology graduates to manage the growing complexity of non-cardiovascular disease in contemporary CICUs can improve patient outcomes. The Supplemental Discussion section provides a commentary on the percentage of centers that met Level 1 criteria and study limitations.
Conclusions
In a cross-sectional survey of CICUs in the United States, we observed that less than 10% of units had dedicated CICU populations and the majority of units had an open staffing model. Only 10.8% of centers currently have the on-site resources, leadership and staffing that meet Level 1 CICU criteria. These results highlight that CICU administrators should assess the patient care needs within their communities and regions with the goal of potentially redesigning and improving care delivery. In academic centers, cardiologist-intensivists attending in the CICU and critical care training programs were high compared with historical studies and may signal a transition in national CICU staffing and training in academic centers.
Supplementary Material
Acknowledgments
We would like to gratefully acknowledge the survey support provided by Ms. Allison Groom from the AHA and Ms. Sarah Sears from the ACC. We would also like to acknowledge the organizational contributions of the AHA’s science and medicine advisor, Ms. Anne Leonard. We would like to thank Ms L. Soulard for copy-editing this manuscript. All persons named in this section have provided the corresponding author with permission to be named in the manuscript.
Funding: This survey was funded by the AHA. This research was supported in part by the Intramural Research Program of the NIH, Critical Care Medicine Department.
Footnotes
Disclosures: Sean van Diepen, Zachary K. Wegerman, Christopher B. Granger, Amanda Stebbins, David A. Morrow, Michael A. Solomon, Jeffrey Soble, Timothy D. Henry, Ian C. Gilchrist, Jason N. Katz, Mauricio G. Cohen, L. Kristin Newby: none. Christopher B. Fordyce; Advisory Board for Bayer Pharmaceuticals.
References
- 1.Katz JN, Minder M, Olenchock B, Price S, Goldfarb M, Washam JB, Barnett CF, Newby LK, van Diepen S. The Genesis, Maturation, and Future of Critical Care Cardiology. J Am Coll Cardiol. 2016;68:67–79. doi: 10.1016/j.jacc.2016.04.036. [DOI] [PubMed] [Google Scholar]
- 2.van Diepen S, Cook DJ, Jacka M, Granger CB. Critical Care Cardiology Research: A Call to Action. Circ Cardiovasc Qual Outcomes. 2013;6:237–242. doi: 10.1161/CIRCOUTCOMES.111.969501. [DOI] [PubMed] [Google Scholar]
- 3.Morrow DA, Fang JC, Fintel DJ, Granger CB, Katz JN, Kushner FG, Kuvin JT, Lopez-Sendon J, McAreavey D, Nallamothu B, Page RL, Parrillo JE, Peterson PN, Winkelman C. Evolution of Critical Care Cardiology: Transformation of the Cardiovascular Intensive Care Unit and the Emerging Need for New Medical Staffing and Training Models. Circulation. 2012;126:1408–1428. doi: 10.1161/CIR.0b013e31826890b0. [DOI] [PubMed] [Google Scholar]
- 4.Pronovost PJ, Angus DC, Dorman T, Robinson KA, Dremsizov TT, Young TL. Physician staffing patterns and clinical outcomes in critically ill patients: a systematic review. JAMA. 2002;288:2151–2162. doi: 10.1001/jama.288.17.2151. [DOI] [PubMed] [Google Scholar]
- 5.Hasin Y, Danchin N, Filippatos GS, Heras M, Janssens U, Leor J, Nahir M, Parkhomenko A, Thygesen K, Tubaro M, Wallentin LC, Zakke I. Recommendations for the structure, organization, and operation of intensive cardiac care units. Eur Heart J. 2005;26:1676–1682. doi: 10.1093/eurheartj/ehi202. [DOI] [PubMed] [Google Scholar]
- 6.Le May M, van Diepen S, Liszkowski M, Schnell G, Tanguay J-F, Granger CB, Ainsworth C, Diodati JG, Fam N, Haichin R, Jassal D, Overgaard C, Tymchak W, Tyrrell B, Osborne C, Wong G. From Coronary Care Units to Cardiac Intensive Care Units: Recommendations for Organizational, Staffing, and Educational Transformation. Can J Cardiol. 2016;32:1204–1213. doi: 10.1016/j.cjca.2015.11.021. [DOI] [PubMed] [Google Scholar]
- 7.Na SJ, Chung CR, Jeon K, Park C-M, Suh GY, Ahn JH, Carriere KC, Song YB, Choi JO, Hahn JY, Choi JH, Choi SH, On YK, Gwon H-C, Jeon E-S, Kim D-K, Yang JH. Association Between Presence of a Cardiac Intensivist and Mortality in an Adult Cardiac Care Unit. J Am Coll Cardiol. 2016;68:2637–2648. doi: 10.1016/j.jacc.2016.09.947. [DOI] [PubMed] [Google Scholar]
- 8.O’Malley RG, Olenchock B, Bohula-May E, Barnett C, Fintel DJ, Granger CB, Katz JN, Kontos MC, Kuvin JT, Murphy SA, Parrillo JE, Morrow DA. Organization and staffing practices in US cardiac intensive care units. Eur Heart J Acute Cardiovasc Care. 2013;2:3–8. doi: 10.1177/2048872612472063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.O’Gara PT, Adams JE, Iii, Drazner MH, Indik JH, Kirtane AJ, Klarich KW, Newby LK, Scirica BM, Sundt M. COCATS 4 Task Force 13: Training in Critical Care Cardiology. J Am Coll Cardiol. 2015;65:1877–1886. doi: 10.1016/j.jacc.2015.03.027. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.