Abstract
Case
We report a case of acute calcific prevertebral tendinitis and discuss the clinical signs, symptoms, and radiologic findings of the disease.
Outcome
This 47‐year‐old man suffered from neck pain, odynophagia, and sore throat for 2 days. Acute calcific prevertebral tendinitis was noted. This disease, brought on by prolonged minor repetitive tendon injury, is an often overlooked cause of acute neck pain. The typical radiologic appearances of the disease include the calcification of the anterior surface of the C1–C2 spine and smooth soft tissue swelling over the retropharyngeal space.
Conclusion
Generally this disease is benign and may be misdiagnosed as deep neck infection. Drainage on this patient would be considered malpractice.
Keywords: Deep neck infection, neck pain, odynophagia, sore throat, tendinitis
Introduction
Acute calcific prevertebral tendinitis has similar clinical findings to deep neck infection. The latter usually has a higher rate of morbidity and mortality. The most common signs and symptoms noted on these patients include acute neck pain, severe sore throat, and odynophagia. Radiologic findings give us important clues when diagnosing this disease. Here we report a patient with acute neck pain, odynophagia, and severe sore throat, which we diagnosed as acute calcific prevertebral tendonitis by radiography findings.
Case Report
A 47‐year‐old man suffered from severe neck pain progressively with neck flexion limitation for 2 days, and was sent to the Emergency Department. He had progressive odynophagia, severe sore throat, and painful sensation at neck rotation. There was no fever, chill, or general soreness during the entire course of the illness. Physical examination showed clear discharge at the left tonsil area. There was tenderness over the hyoid bone area and swelling over the posterior pharyngeal wall. No lymph node enlargement stridor, or other airway obstruction signs were noted. The cervical spine X‐ray film (Fig. 1) showed thickening of the retropharyngeal space at the C2 level. A neck computed tomography (CT) scan revealed a smoothly unenhanced soft tissue swelling at the prevertebral space with calcific density over the anterior surface of the C1–C2 vertebral body. The contrast ring enhancement of the edge was not prominent and there was no fatty infiltration around the parapharyngeal space. (Figs. 2, 3). There was a slight increase of C‐reactive protein and leukocytosis noted on laboratory study. Under the suspicion of deep neck infection, we carried out needle puncture for this patient on the posterior wall of the pharynx and no fluid or pus was found.
Figure 1.

Lateral view of the cervical spine in a 47‐year‐old man suffering from neck pain, odynophagia, and sore throat showed thickening retropharyngeal space at the first and the second cervical spine level (arrow).
Figure 2.
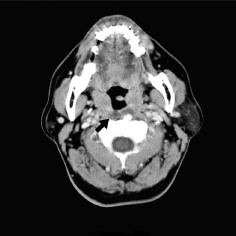
Axial view of an enhanced neck computed tomography scan in a 47‐year‐old man suffering from neck pain, odynophagia, and sore throat. There was swelling at the prevertebral space without airway compression (arrow), and there was no fatty infiltration around the parapharyngeal space.
Figure 3.

Sagittal view of an enhanced neck computed tomography scan in a 47‐year‐old man suffered from neck pain, odynophagia, and sore throat. There was one calcification over the anterior surface of the first and second cervical vertebral body (arrowhead). The contrast ring enhancement of the edge was not prominent.
Initially, antibiotic therapy was used because of suspicion of deep neck infection under the clinical signs and symptoms of neck pain with odynophagia and neck CT scan findings. However, the patient's neck pain persisted. Under the diagnosis of acute calcific tendinitis the patient was treated with non‐steroidal, anti‐inflammatory drugs. The neck pain subsided the following day.
Discussion
In 1964, Hartley first described acute calcific prevertebral tendinitis, or retropharyngeal calcific tendonitis, as a distinct clinical disease.1 This calcific tissue was confirmed by a scanning electron microscope and energy‐dispersive spectrometry revealed calcium and phosphorus components.2 Up to 2010, there were 71 published cases of acute calcific prevertebral tendinitis.3 Emergency physicians are still unacquainted with the disease and it could be confused with an infectious disease such as retropharyngeal abscess.
Signs and symptoms of acute calcific prevertebral tendinitis are non‐specific and may resemble other neck diseases. Usual signs and symptoms include neck pain, flexion limitation, and odynophagia. Prevertebral soft tissue swelling will be found on cervical spine X‐ray film. Calcification due to inflammation of the longus colli muscle and tendon may be present at the prevertebral space.2, 4
Although cases of acute calcific prevertebral tendinitis are found predominantly among patients between 30 and 60 years of age, it can also present in patients younger than 21 and older than 81.5, 6
The pathogenesis of acute calcific prevertebral tendinitis is inflammation.2, 4 The typical radiological finding is asymmetric soft tissue swelling with calcification deposits along the superior medial portion of the longus colli muscle, at the anterior surface at the level of C1 and C2, which is the insertion point of this muscle.7, 8 Contrast CT scans play an important part in the diagnosis of acute calcific prevertebral tendonitis. The findings of smooth soft tissue edema with lack of contrast enhancement on CT scan help us in differentiating from an abscess. The contrast ring enhancement is more prominent around the edge of abscesses and fatty infiltration will also be increased around an abscess. The CT scan can also help us to identify calcifications, which may not be visible on plain film, as in this case. The role of magnetic resonance imaging (MRI) is not clear in the diagnosis of prevertebral calcific tendinitis. Diffuse longus colli muscle swelling with high signal in the prevertebral space will be present in T2‐weighted MRI.5 An MRI study may be helpful to differentiate fluid and effusion more accurately.9
Acute prevertebral calcific tendinitis is a self‐limited condition. If calcific tendonitis is not treated, it usually resolves spontaneously within several weeks.10 Conservative treatment with non‐steroidal anti‐inflammatory drugs is the mainstay of treatment, yet one brief course of steroids can be considered for more rapid pain relief.3 Cervical immobilization can help alleviating the symptoms.
Although acute calcific prevertebral tendinitis is a benign and rare disease, it is an important differential diagnosis as it mimics abscess in the retropharyngeal space. The clinical significance of this report is that awareness of this rare disease can help to prevent us from carrying out unnecessary drainage in affected patients. Neck MRI may have a role in the differential diagnosis between acute prevertebral calcific tendinitis and deep neck infection. An otolaryngologist consultation is necessary to check the airway condition when there are signs of airway compromise. If there is leukocytosis or increased C‐reactive protein levels, other infective conditions, such as retropharyngeal abscess, must be ruled out before making a diagnosis of this benign condition. Drainage in this case would be malpractice. The needle puncture should be the final step if the results of clinical examinations are ambiguous.
Conflict of Interest
None.
References
- 1. Hartley J. Acute cervical pain associated with retropharyngeal calcium deposit: A case report. J. Bone Joint Surg. Am. 1964; 46: 1753–1754. [PubMed] [Google Scholar]
- 2. Ring D, Vaccaro AR, Scuderi G, Pathria MN, Garfin SR. Acute calcific retropharyngeal tendinitis. Clinical presentation and pathological characterization. J. Bone Joint Surg. Am. 1994; 76: 1636–1642. [DOI] [PubMed] [Google Scholar]
- 3. Park R, Halpert DE, Baer A, Kunar D, Holt PA. Retropharyngeal calcific tendinitis: case report and review of the literature. Semin. Arthritis Rheum. 2010; 39: 504–509. [DOI] [PubMed] [Google Scholar]
- 4. Kupferman TA, Rice CH, Gage‐White L. Acute prevertebral calcific tendinitis: A nonsurgical cause of prevertebral fluid collection. Ear Nose Throat J. 2007; 86: 164–166. [PubMed] [Google Scholar]
- 5. Mihmanli I, Karaarslan E, Kanberoglu K. Inflammation of vertebral bone associated with acute calcific tendinitis of the longus colli muscle. Neuroradiology 2001; 43: 1098–1101. [DOI] [PubMed] [Google Scholar]
- 6. Kaplan MJ, Eavey RD. Calcific tendinitis of the longus colli muscle. Ann. Otol. Rhinol. Laryngol. 1984; 93: 215–219. [DOI] [PubMed] [Google Scholar]
- 7. Razon RV, Nasir A, Wu GS, Soliman M, Trilling J. Retropharyngeal calcific tendonitis: Report of two cases. J. Am. Board Fam. Med. 2009; 22: 84–88. [DOI] [PubMed] [Google Scholar]
- 8. Artenian DJ, Lipman JK, Scidmore GK, Brant‐Zawadzki M. Acute neck pain due to tendonitis of the longus colli: CT and MRI findings. Neuroradiology 1989; 31: 166–169. [DOI] [PubMed] [Google Scholar]
- 9. Eastwood JD, Hudgins PA, Malone D. Retropharyngeal effusion in acute calcific prevertebral tendinitis: Diagnosis with CT and MR imaging. AJNR Am. J. Neuroradiol. 1998; 19: 1789–1792. [PMC free article] [PubMed] [Google Scholar]
- 10. Shin DE, Ahn CS, Choi JP. The acute calcific prevertebral tendinitis: Report of two cases. Asian Spine J. 2010; 4: 123–127. [DOI] [PMC free article] [PubMed] [Google Scholar]


