Abstract
Case
A pregnant (20 gestational weeks) 32‐year‐old woman was found in cardiac arrest. Spontaneous circulation returned after 15 min. She became brain dead on the 13th hospital day. The patient was in stable circulatory condition under nasal desmopressin and 20–30 mg/day of hydrocortisone. On the 92nd hospital day at gestational week 33 + 3 days, natural labor began and a healthy 2,130‐g girl (Apgar 6/8) was delivered vaginally with minimum assistance.
Outcome
The baby was discharged 40 days after birth and followed up regularly.
Conclusion
Brain death remains a hopeless condition for patients, but a brain‐dead woman may still be able to naturally deliver a healthy baby.
Keywords: Brain death, delivery, ethical issue, pregnancy, somatic support
Introduction
Brain death may occur in an individual of any age, and women of reproductive age are no exception. Adult brain‐dead bodies tend to have unstable circulation and to experience cardiac arrest within 1 week of the start of brain death. However, there are some cases of brain‐dead individuals with stable circulation under minimum medical support. If a pregnant woman becomes brain dead, physicians may be faced with the decision whether to withdraw the patient's medical support. It is also a difficult decision for the mother's spouse and/or family. Reports of only 12 babies delivered by cesarean operation from brain‐dead mothers have been published.1 Here we report a very rare case of a brain‐dead woman who naturally delivered a healthy baby girl weighing 2,130 g at 33 weeks of gestation on the 78th day of brain death. Practical and ethical issues are discussed.
Case
After a quarrel with her husband, a 32‐year‐old woman at 20 weeks' gestation attempted suicide by hanging herself. She was found in cardiac arrest by her family. Basic life support was soon provided by emergency personnel for several minutes, and her spontaneous circulation recovered on the way to a nearby hospital. The estimated cardiac arrest time was approximately 15 min. She was transferred to our hospital for intensive care. On admission she was in a deep coma with stable circulation, and the fetal heart beat was 140 b.p.m. Despite vigorous brain‐oriented treatment, the woman's neurologic status worsened, with fixed and dilated pupils. Diabetes insipidus occurred due to the lack of antidiuretic hormone.
We estimated that the patient became brain dead on the 13th hospital day (Fig. 1). Computed tomography showed severe diffuse brain swelling due to prolonged hypoxic damage. We confirmed her brain death by the standard brain death criteria of the Japanese Ministry of Health, Labor and Welfare.2 She was completely dependent on a ventilator. The standard apnea test was not carried out based on the possibility of a hypoxic effect on the fetus. She was treated with a continuous infusion of vasopressin at the rate of 0.01–0.02 U/h. She had been diagnosed with hypothyroidism before her suicide attempt, and she was treated with 150 μg levothyroxine daily. Levels of thyroid stimulating hormone and free T3 and T4 are shown in Figure 1.
Figure 1.
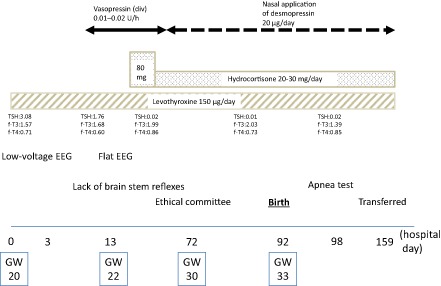
Clinical course of a pregnant 32‐year‐old brain‐dead woman. Normal level of thyroid stimulating hormone (TSH) is 0.5–5 μIU/mL, Band free (f‐)T3 is 2.3–4 pg/mL, and free T4 is 0.9–1.7 ng/dL. EEG, electroencephelogram; GW, gestational week.
The patient gradually achieved stable circulation, and the vasopressin was switched to 20 μg nasal desmopressin and 20–30 mg/day hydrocortisone with a standard enteral diet through a nasogastric tube. Hydrocortisone might be useful for stable circulation and fetal lung maturation. In our ethical committee, we engaged in lengthy deliberations regarding whether to withdraw the patient's somatic support, including the issue of intentional fetus death. A combined meeting of the referred intensivists, obstetricians, neonatal physicians, and ethical professionals was undertaken to discuss the options and ethical issues. We agreed that the family's consent was needed to withdraw her somatic support or to perform a cesarean operation for a safe delivery of the fetus. Extensive information regarding the prognosis of both the patient and the fetus was provided to the family, but they declined to terminate life support and declined a cesarean operation based on their emotional and social concerns.
An informed decision was made to continue medical support. We had to prepare to save the fetus in case of an accidental delivery. Obstetricians regularly checked the condition of the fetus, and the fetal growth was in the normal range (Fig. 2). On the 92nd hospital day (at 33 weeks and 3 days of gestation) natural labor started without the use of any labor accelerator, and a healthy 2,130‐g girl was delivered vaginally with minimum assistance by obstetricians. The baby's Apgar score was 6/8, and she was discharged 40 days after birth. Her growth was followed by a pediatrician regularly. We confirmed that the mother was apneic by the standard apnea test on the 98th hospital day. The serum level of pituitary hormones was very low (1.0 pg/mL adrenocorticotropic hormone, <0.1 ng/mL human growth hormone, 0.1 mIU/mL luteinizing hormone, 0.1 mIU/mL follicle stimulating hormone, 0.02 μIU/mL thyroid stimulating hormone); only prolactin was 25.4 ng/mL. The mother was transferred to a local hospital and died approximately 1 year after brain death.
Figure 2.
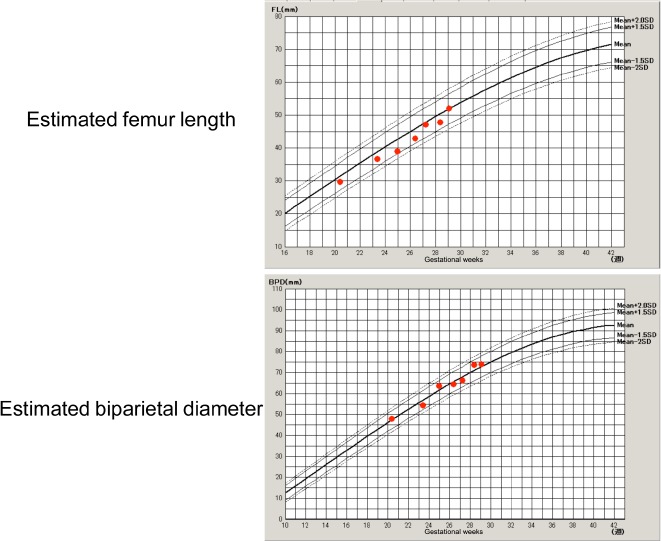
Estimated femur length (FL) and biparietal diameter (BPD) of the fetus of a 32‐year‐old brain‐dead woman on the standard growth curve, shown by ultrasound echography.
Discussion
Severe intrinsic or traumatic brain damage may cause brain death in a pregnant woman. Feldman et al. reported seven such cases in 20003 and Esmaeilzadeh et al. reviewed an additional 23 cases in 2010.1 As noted earlier, 12 babies have been delivered by cesarean operation from brain‐dead mothers, at an average of 30 gestational weeks, but there has been no report of a natural delivery from a brain‐dead mother, to our knowledge. The present case appears to be the first case of a natural delivery from a brain‐dead mother under prolonged somatic support. It is surprising that labor can occur in a patient with a condition of pituitary hormonal disarrangement such as that in prolonged brain death.
Conclusion
Brain death remains a hopeless condition for a patient, but a pregnant woman who is brain dead may still have the ability to give birth naturally to a healthy baby.
Conflict of Interest
None.
Acknowledgment
We thank the staff of Intensive Care Medicine and the Department of Obstetrics, Kumamoto University Hospital who participated in the treatment of the patient and infant. Written informed consent was obtained from the patient's family for publication.
References
- 1. Esmaeilzadeh M, Dictus C, Kayvanpour E et al One life ends, another begins: Management of a brain‐dead pregnant mother—A systematic review. BMC Med. 2010; 8: 74–85. Available from: http://www.biomedcentral.com/1741‐7015/8/74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Takeuchi K, Takeshita H, Takakura K et al Evolution of criteria for determination of brain death in Japan. Acta Neurochir. 1987; 87: 93–98. [DOI] [PubMed] [Google Scholar]
- 3. Feldman DM, Borgida AF, Rodis JF, Campbell WA. Irreversible maternal brain injury during pregnancy: A case report and review of literature. Obstet. Gynecol. Surv. 2000; 55: 708–714. [DOI] [PubMed] [Google Scholar]


