Abstract
Case
An 89‐year‐old woman was admitted to our hospital because of dyspnea following abdominal pain and vomiting. According to chest computed tomography findings, a diagnosis of acute respiratory failure due to right‐sided Bochdalek hernia was made.
Outcome
Emergency laparotomy revealed that a bowel loop from the terminal ileum to the transverse colon had herniated into the right thoracic cavity through the foramen of Bochdalek. The herniated organs were reduced to the abdominal cavity and the foramen was repaired by direct suturing. The patient had good recovery and was discharged 78 days later.
Conclusion
Bochdalek hernias in elderly patients are rare, but may be complicated by strangulation of the herniated organ. This should be taken into account by acute care physicians. To prevent this fatal complication, regardless of symptoms, surgical treatment may be essential as soon as a diagnosis of adult Bochdalek hernia is made.
Keywords: Acute respiratory failure, adult, Bochdalek hernia, congenital diaphragmatic hernia, right side
Introduction
Congenital diaphragmatic hernia is a congenital anomaly caused by embryonic developmental failure of the diaphragm, and Bochdalek hernia (BH) accounts for approximately 95% of cases.1 Most cases of BH present with acute cardiorespiratory failure during the neonatal period; thus, BH in adults is unusual.2, 3, 4, 5 Regarding the side of occurrence, 80–90% of BH arise on the left side.1, 2, 3 Here, we report a rare case of right‐sided BH in an elderly patient. We also review relevant published case reports and discuss the clinical presentation and management of adult BH.
Case
An 89‐year‐old woman with hypertension was admitted to our hospital because of a sudden onset of dyspnea, following abdominal pain and vomiting that started 7 h prior to admission. She had no previous history of trauma or surgery. On admission, she appeared pale and had labored breathing. Her body temperature was 36.9°C; heart rate, 118 b.p.m.; respiratory rate, 40 breaths/min; and blood pressure, 180/95 mmHg. On physical examination, breath sounds were decreased in the right side of the chest and the abdomen was not distended. Laboratory results revealed leucocytosis (15,600/mm3), and blood gas analysis revealed hypoxia (PaO2, 54.5 mmHg under 2 L/min of nasal O2 cannula) and acidosis (pH 7.343; PaCO2, 41.5 mmHg; and base excess, −3.5 mmol/L). Plain chest radiography revealed bowel loops in the right thoracic cavity and mediastinal shift to the left side. Therefore, O2 was immediately administered using a facial mask at a rate of 8 L/min. Plain chest computed tomography (CT) revealed bowel loops in the right thoracic cavity, which herniated through the posterolateral portion of the right diaphragm and shifted the mediastinum to the left side (Fig. 1). Thus, the patient was diagnosed with acute respiratory failure due to right‐sided BH. Emergency endotracheal intubation followed by mechanical ventilation was initiated, and emergency surgery was carried out 12 h after the onset of symptoms. On laparotomy through a right subcostal incision, a bowel loop from the terminal ileum to the transverse colon was found to be herniated into the right thoracic cavity through a defect in the diaphragm at the posterolateral portion (Fig. 2A). The herniated organs were reduced to the abdominal cavity with traction, and incomplete attachment of the right colon and no ischemic changes were observed. The diaphragmatic defect, measuring 45 × 30 mm in diameter and without a hernia sac, corresponded to the foramen of Bochdalek (Fig. 2B). The foramen was repaired by tension‐free direct suturing without placing any chest drains. After the surgery, the patient underwent 8‐day‐long mechanical ventilation and received antibiotic treatment for associated pneumonia, and she had good recovery. Following rehabilitation for muscular atrophy of the lower legs, she was discharged 78 days later. At 2‐years follow‐up, she was in good condition, with no sign of recurrence.
Figure 1.
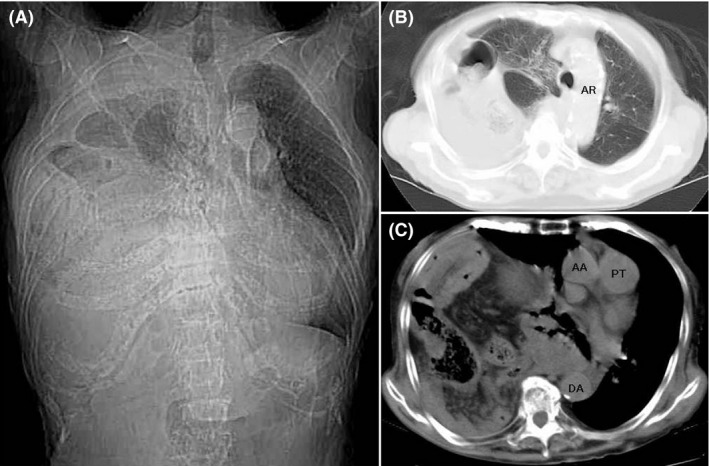
Plain chest computed tomography findings on admission of an 89‐year‐old woman with right‐sided Bochdalek hernia. A, Scout view revealed bowel loops in the right thoracic cavity, which compressed the right lung to the apex of the thoracic cavity and shifted the mediastinum to the left side. B, C, Axial views at the level of Th4 (B) and Th7 (C) revealed that the bowel loops in the right thoracic cavity seemed to be the colon, which had herniated through the posterolateral portion of the right diaphragm. AA, ascending aorta; AR, arch of aorta; DA, descending aorta; PT, pulmonary trunk.
Figure 2.
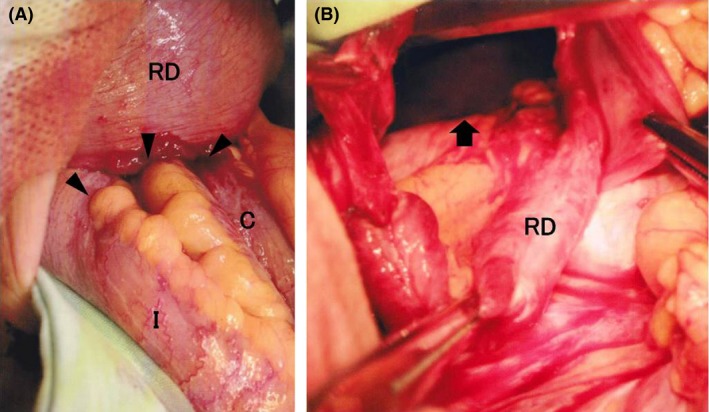
Intraoperative findings in an 89‐year‐old woman with right‐sided Bochdalek hernia. A, A bowel loop was found to be herniated into the right thoracic cavity through a diaphragmatic defect (arrow heads). B, The diaphragmatic defect (arrow) corresponded to the foramen of Bochdalek. C, transverse colon; I, terminal ileum; RD, right diaphragm.
Discussion
The embryological etiology of BH is considered as follows:2 until the 4th week of gestation, the thoracic and abdominal cavities are in communication and comprise a pleuroperitoneal canal. This canal is gradually separated into the thoracic and abdominal cavities and is finally closed by the development of the diaphragm, which results from the fusion of two muscle groups, that is, the septum transversum and the pleuroperitoneal folds. This fusion is completed during the 8th week of gestation at the posterolateral portion (the lumbocostal trigone) on each side of the diaphragm. The failure of this fusion creates a muscular defect in the diaphragm at the posterolateral portion, the so‐called “foramen of Bochdalek”, and allows the abdominal organs to herniate into the thoracic cavity through this foramen. If the foramen is large, herniation may occur during the prenatal period, and the lung may be compressed and its development hindered, leading to pulmonary hypoplasia.1 In such cases, BH presents with acute cardiorespiratory failure immediately after birth, with the overall mortality rate remaining at approximately 30% despite recent advances in neonatology and pediatric surgery.1 However, if the foramen is small, herniation may not easily occur, and BH may remain asymptomatic until herniation occurs later in life. This mechanism may account for the presentation of adult BH.4
We accessed, through the Japan Medical Abstracts Society, 109 case reports of adult BH from Japan from 1982 to 2015 (Table 1), and analyzed them for the current study. In terms of age distribution, 65% of patients were between the ages of 16 and 64 years, and the number of the patients decreased with increasing age. This may suggest that adult BH occurs more frequently in younger persons, and, to the best of our knowledge, our case is the oldest to be reported. The left/right side ratio of BH in these cases was 5.1:1, which is similar to that in previous studies.2, 3 Embryologically, the pleuroperitoneal canal closes earlier on the right side than on the left.2 In addition, even if the foramen of Bochdalek remains patent on the right side, the liver may buttress the foramen and prevent the herniation of abdominal organs.3 These factors may account for the lower incidence of right‐sided BH. Unlike neonatal BH, the common initial presentation of disease in adults was non‐specific digestive symptoms such as abdominal pain, nausea, and vomiting rather than respiratory symptoms. However, 17% of cases presented with respiratory symptoms following digestive symptoms. Furthermore, precipitating factors that had induced abdominal symptoms were identified in 25 (25%) cases, and a common feature of these factors was an increase in intra‐abdominal pressure including physical effort, defecation, asthma attack, or pregnancy. Diagnosing adult BH is considered difficult because of the wide variation of symptoms;2 however, the sequence of symptoms, that is, respiratory symptoms following digestive symptoms induced by increased intra‐abdominal pressure, may be characteristic of adult BH, and this pattern of onset may help to detect this disease. Interestingly, 16 (16%) cases were asymptomatic and were diagnosed incidentally by radiological examinations, and 6 (38%) were of right‐sided BH. This high proportion of right‐sided BH in asymptomatic cases may be explained by the buttressing effect of the liver; Brown et al.2 suggested that right‐sided cases of BH are less likely to manifest symptoms. For the diagnosis of BH, chest X‐ray is useful; however, adult BH may be difficult to appreciate on chest X‐ray alone in some cases.2 Computed tomography is considered the preferred diagnostic imaging method,2, 5 and in the 104 reviewed reports, CT was used in 87 (84%) cases. Other imaging methods used for the diagnosis of adult BH included upper gastrointestinal contrast studies (42 cases), barium enema studies (18 cases), magnetic resonance imaging (18 cases), and gastrointestinal endoscopy (14 cases).
Table 1.
One hundred and nine Japanese cases of Bochdalek hernia in adults, 1982–2015
| Characteristics | No. of patients (%) |
|---|---|
| Age, years | |
| 16–64 | 71 (65) |
| 65–74 | 24 (22) |
| 75–84 | 12 (11) |
| 85+ | 2 (2) |
| Sex | |
| Male | 46 (42) |
| Female | 63 (58) |
| Laterality of hernia (n = 105) | |
| Left | 86 (82) |
| Right | 17 (16) |
| Bilateral | 2 (2) |
| Initial presentation of disease (n = 103) | |
| Digestive symptoms | 42 (40) |
| Respiratory symptoms | 28 (27) |
| Respiratory symptoms following digestive symptoms | 17 (17) |
| Asymptomatic | 16 (16) |
| Surgical approach (n = 102) | |
| Transabdominal | 62a (61) |
| Transthoracic | 19b (18) |
| Thoracoabdominal | 16c (16) |
| Not done | 5 (5) |
| Hernia repair (n = 96) | |
| Direct suturing | 73 (76) |
| Interposition mesh graft | 23 (24) |
| Coexisting congenital anomaly | |
| Incomplete attachment of intestine | 10 (48) |
| Intestinal malrotation | 5 (24) |
| Mesenterium commune | 5 (24) |
| Hepatic hypoplasia | 1 (4) |
| Strangulation of herniated organ | |
| Stomach | 7 (39) |
| Colon | 6 (33) |
| Small bowel | 5 (28) |
| Prognosis (n = 97) | |
| Alive | 92 (95) |
| Dead | 5 (5) |
Combined with laparoscopy, 12 (19%).
Combined with thoracoscopy, 6 (32%).
Combined with laparoscopy and/or thoracoscopy, 3 (19%).
The optimal strategy for BH surgical treatment is controversial.3 Authors who are in favor of the transabdominal approach emphasize its facility to not only reduce the hernia contents to the abdominal cavity but also to deal with complications such as obstruction, strangulation, perforation, or coexisting congenital anomaly.3, 4 In contrast, the transthoracic approach is advocated by other authors because of the convenience of dissecting adhesions between the pleura and hernia contents.5 Although the most frequently applied approach in the reviewed reports was transabdominal, no significant difference in outcome was found between the approaches, as evidenced in previous studies.2, 5 Therefore, surgeons may choose the more familiar approach. Due to recent advances in equipment and techniques, reports of laparoscopic and thoracoscopic surgery for adult BH being used with positive outcomes are increasingly common,2 and in the reports reviewed here, these techniques were used in 21 (22%) cases. In our case, we were concerned that increased intra‐abdominal pressure induced by the pneumoperitoneum technique used during laparoscopy might lead to the progression of herniation and result in the development of cardiorespiratory failure. Therefore, we chose laparotomy instead of laparoscopy. For BH repair, direct suturing was more frequently applied than interposition mesh graft; however, recurrence occurred in 2 (3%) of directly sutured cases. Schumacher et al.5 suggested that direct suturing may be preferable when the foramen may be closed without undue tension, and the use of mesh graft may be recommended when the size of the foramen exceeds 20–30 cm2. Strangulation of the herniated organ is one of the fatal complications of BH, and 18 (18%) cases experienced this complication. To confirm strangulation of the herniated organ preoperatively, contrast‐enhanced CT is the most accurate imaging method and should be used in cases with suspected strangulation.6 It has been recognized that the prognosis of adult BH is better than that of neonatal BH;2 nevertheless, in the present study, the mortality rate was 5% and 3 (60%) cases experienced strangulation of the herniated organ.
Conclusion
Bochdalek hernia in elderly patients is rare, but may be complicated by strangulation of the herniated organ. This should be taken into account by acute care physicians. To prevent this fatal complication, regardless of symptoms, surgical treatment may be essential as soon as a diagnosis of adult BH is made.
Conflict of Interest
None declared.
Funding Information
No funding information provided.
References
- 1. Robinson PD, Fitzgerald DA. Congenital diaphragmatic hernia. Paediatr. Respir. Rev. 2007; 8: 323–35. [DOI] [PubMed] [Google Scholar]
- 2. Brown SR, Horton JD, Trivette E, Hofmann LJ, Johnson JM. Bochdalek hernia in the adult: demographics, presentation, and surgical management. Hernia 2011; 15: 23–30. [DOI] [PubMed] [Google Scholar]
- 3. Rout S, Foo FJ, Hayden JD, Guthrie A, Smith AM. Right‐sided Bochdalek hernia obstructing in an adult: case report and review of the literature. Hernia 2007; 11: 359–62. [DOI] [PubMed] [Google Scholar]
- 4. Salustio R, Nabais C, Paredes B, Sousa FV, Porto E, Fradique C. Association of intestinal malrotation and Bochdalek hernia in an adult: a case report. BMC Res. Notes 2014; 7: 296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Schumacher L, Gilbert S. Congenital diaphragmatic hernia in the adult. Thorac. Surg. Clin. 2009; 19: 469–72. [DOI] [PubMed] [Google Scholar]
- 6. Ohira G, Shuto K, Kono T et al Utility of arterial phase of dynamic CT for detection of intestinal ischemia associated with strangulation ileus. World J. Radiol. 2012; 4: 450–4. [DOI] [PMC free article] [PubMed] [Google Scholar]


