Abstract
Aim
In Japan, trauma surgery training remains insufficient, and on‐the‐job training has become increasingly difficult because of the decreasing number of severe trauma patients and the development of non‐operative management. Therefore, we assessed whether a 1‐day cadaver‐based seminar is effective for trauma surgery training.
Methods
Data were collected from 11 seminars carried out from January 2013 to March 2014, including a 10‐point self‐assessment of confidence levels (SACL) for 21 surgical skills and an evaluation of the contents before, just after, and a half‐year after the seminar. Statistical analysis was undertaken using the paired t‐test at P < 0.0167.
Results
A total of 135 participants were divided into three groups based on experience and clinical careers. The SACL improved in all skills between before and just after the seminar, however, they decreased between just after and a half‐year after the seminar. The SACL did not change significantly in all skills between just after and a half‐year after the seminar in highly experienced and experienced group members belonging to an emergency center.
Conclusions
A cadaver‐based seminar provided more self‐confidence just after the seminar for participants at all experience levels. This effect was not maintained after a half‐year, except in participants who can practice the skills at an emergency center. Practicing and participating in the seminar repeatedly is suggested to be effective for skills retention in trauma surgery.
Keywords: cadaver, educational seminar for trauma surgery, half‐year follow‐up, self‐assessment of confidence levels (SACL), skills retention
Introduction
In Japan, trauma surgery training remains insufficient, and on‐the‐job training has become increasingly difficult because of the decreasing number of severe trauma patients and the development of non‐operative management. Off‐the‐job training courses using animals or cadavers have been held in other countries. Advanced Trauma Operative Management (ATOM) and Definitive Surgical Trauma Care (DSTC) are off‐the‐job training courses using animals.1, 2 These two animal courses have Japanese branch offices, and have been held in Japan recently. However, it is not easy to attend the course, because of the expensive attendance fee (> ¥200,000). Definitive Surgical Trauma Skills (DSTS) and Advanced Surgical Skills for Exposure in Trauma (ASSET) are off‐the‐job training courses using cadavers.3, 4 These two cadaver courses do not have Japanese branch offices.
In Japan, surgical training using cadavers was initiated by Murakami et al. in 2003.5 However, there was some legal doubt, because there was no law that certified medical doctors could use cadavers for surgical training. “Guidelines for surgical training using cadavers” was announced by the Japan Surgical Society and the Japanese Association of Anatomists in 2012. The guidelines justify that medical doctors can use cadavers for surgical training under existing Japanese law.6
After publication of the guidelines, the Japanese Ministry of Health, Labour and Welfare publicly recruited for “The project of surgical training using cadavers” in 2012. Tokyo Medical University was chosen as one of the six members in the project. We publicly offered a 1‐day cadaver‐based educational seminar to discuss trauma surgery.
Methods
The present study was approved by the institutional review board of the faculty of Tokyo Medical University (IRB: 2139).
Setting
We held 11 1‐day seminars from January 2013 to March 2014. In each of the seminars we used three cadavers. All cadavers were embalmed with formalin solution. Participants were divided into three groups (A, highly experienced; B, experienced; C, little‐experienced) based on experience and clinical careers. The following criteria included surgery board certification (SBC: yes or no), post‐graduate year (PGY), and pre‐seminar self‐assessment of confidence levels (SACL) for 21 surgical skills: A, SBC‐yes and high confidence (average SACL, >7 points); B, SBC‐yes and middle confidence (average SACL, 3–7 points), SBC‐no and middle confidence and PGY ≥7; C, SBC‐yes and low confidence (average SACL, <3 points), SBC‐no and middle confidence and PGY <7, SBC‐no and low confidence. They carried out 21 surgical skills on the cadavers as shown in Figure 1. In addition, we conducted a mini‐lecture using a slide presentation before each section to confirm what participants were expected to do.
Figure 1.
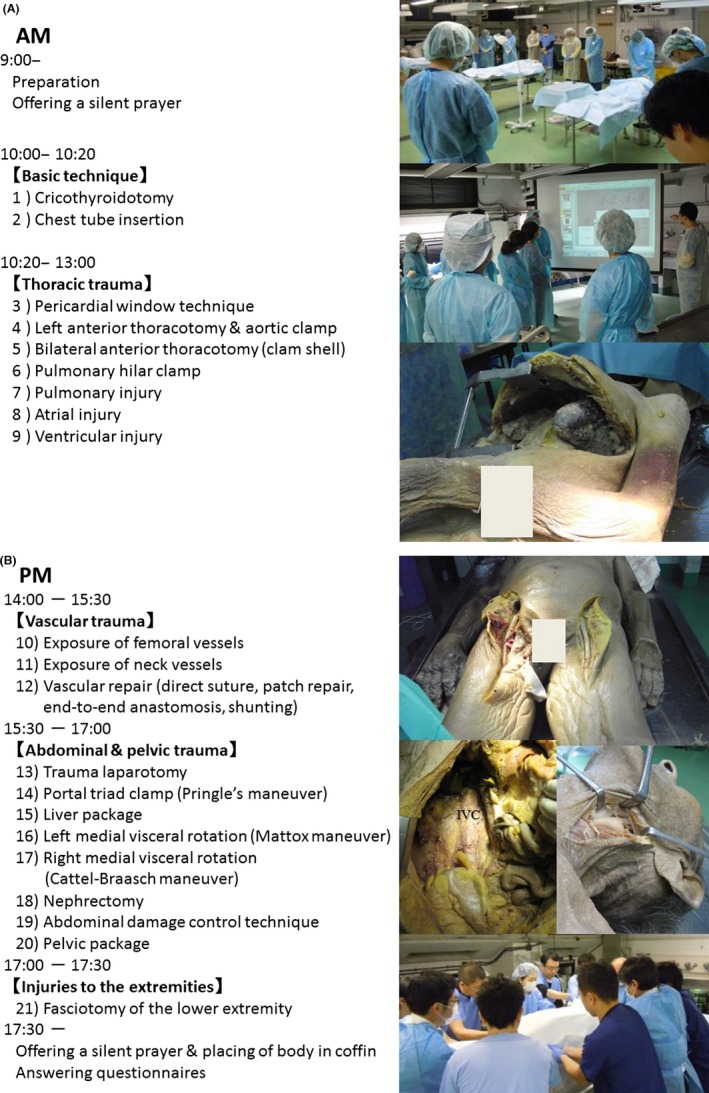
One‐day cadaver‐based educational seminar for trauma surgery and 21 surgical skills practiced by participants, showing morning (A) and afternoon (B) schedules.
The participants answered the questionnaires including the SACL for the 21 skills (10‐point visual analog scale scores, as follows: 0 points, cannot do at all; 5 points, can do with help of an adviser; 10 points, can do independently) and an evaluation of the contents before, just after, and a half‐year after the seminar. We asked participants to answer these questionnaires before and a half‐year after via e‐mail (Fig. 2).
Figure 2.

Example of a self‐assessment of confidence levels for 21 surgical skills covered during a one‐day cadaver‐based educational seminar for trauma surgery.
Statistical analysis
Evaluation and analysis of all data was carried out using Microsoft Excel 2013 for Windows (Microsoft, Redmond, WA, USA) with paired t‐tests. P‐values < 0.0167 (=0.05/3 with a Bonferroni correction for multiple comparisons) were considered to be statistically significant.
Results
A total of 135 participants were divided into three groups, as follows: A, n = 50; B, n = 44; C, n = 41, then completed the seminar. The answers of all 135 participants were returned in “pre”, “post”, and “after a half‐year” questionnaires (response rate 100%) (Table 1).
Table 1.
Comparisons of participants in a one‐day cadaver‐based educational seminar for trauma surgery, divided into three groups according to experience
| A, n = 50 | B, n = 44 | C, n = 41 | |
|---|---|---|---|
| PGY, years | 17.1 ± 5.09 | 11.2 ± 5.22 | 8.24 ± 6.18 |
| Gender, n (%) | |||
| Male | 46 (92) | 43 (98) | 36 (88) |
| Female | 4 (8) | 1 (2) | 5 (12) |
| Workplace, n (%) | |||
| Emergency center | 25 (50) | 27 (61) | 33 (80) |
| Non‐emergency center | 25 (50) | 17 (39) | 8 (20) |
| Board certification member, n | |||
| Emergency medicine | 27 | 18 | 14 |
| Trauma surgery | 6 | 1 | 0 |
| General surgery | 44 | 22 | 2 |
| Gastroenterological surgery | 15 | 4 | 0 |
| Hepato‐biliary‐pancreatic surgery | 1 | 2 | 0 |
| Cardiovascular surgery | 2 | 0 | 0 |
| Neurosurgery | 1 | 1 | 0 |
| Orthopedics | 0 | 1 | 1 |
| Transplantation | 1 | 0 | 0 |
| Urology | 0 | 0 | 2 |
| Burns | 1 | 0 | 0 |
| Anesthesiology | 0 | 1 | 2 |
| Intensive care | 4 | 2 | 1 |
| Radiology | 0 | 0 | 1 |
| Internal medicine | 0 | 0 | 1 |
| Cardiology | 1 | 0 | 1 |
| Pediatrics | 0 | 1 | 0 |
| Psychiatry | 0 | 1 | 0 |
| Gastroenterological endoscopy | 2 | 2 | 0 |
| Senior fellow, n | |||
| Emergency medicine | 4 | 1 | 0 |
| General surgery | 14 | 0 | 0 |
| Gastroenterological surgery | 5 | 0 | 0 |
| Hepato‐biliary‐pancreatic surgery | 1 | 0 | 0 |
| Neurosurgery | 1 | 1 | 0 |
| Anesthesiology | 0 | 1 | 2 |
| Gastroenterological endoscopy | 1 | 0 | 0 |
| Cumulative total number | 131 | 59 | 27 |
A, highly experienced; B, experienced; C, little‐experienced; PGY, post‐graduate year.
The SACL improved in all skills between before and just after the seminar (4.8 ± 3.5 vs. 7.1 ± 2.6, P < 0.0001, n = 135); however, they decreased between just after and a half‐year after the seminar (7.1 ± 2.6 vs. 6.8 ± 2.9, P < 0.0001). Examining these results according to each skill, the SACL decreased in the following skills between just after and a half‐year after the seminar, respectively (P < 0.0167): left anterior thoracotomy and aortic clamp (7.7 ± 2.3 vs. 7.4 ± 2.8), bilateral anterior thoracotomy (7.2 ± 2.5 vs. 6.8 ± 2.9), atrial injury (5.4 ± 2.4 vs. 5.0 ± 2.6), trauma laparotomy (8.0 ± 2.5 vs. 7.6 ± 3.0), portal triad clamp (7.7 ± 2.7 vs. 7.3 ± 3.2), liver package (7.5 ± 2.6 vs. 7.1 ± 3.0), left medial visceral rotation (6.8 ± 2.8 vs. 6.2 ± 3.1), and right medial visceral rotation (6.7 ± 2.9 vs. 6.2 ± 3.2) (Table 2).
Table 2.
Self‐assessment of confidence levels for 21 surgical skills in 135 participants before (BS), after (AS), and a half‐year after (HS) a cadaver‐based educational seminar for trauma surgery
| Evaluation, average ± standard deviation | Significant differences | |||||
|---|---|---|---|---|---|---|
| BS | AS | HS | BS vs. AS | BS vs. HS | AS vs. HS | |
| Basic technique | ||||||
| 1) Cricothyroidotomy | 8.0 ± 2.5 | 9.2 ± 1.4 | 9.3 ± 1.3 | *** | *** | ns |
| 2) Chest tube insertion | 9.4 ± 1.5 | 9.7 ± 0.9 | 9.8 ± 0.8 | * | * | ns |
| Thoracic trauma | ||||||
| 3) Pericardial window technique | 4.8 ± 3.4 | 7.3 ± 2.2 | 7.2 ± 2.5 | *** | *** | ns |
| 4) Left anterior thoracotomy & aortic clamp | 5.1 ± 3.8 | 7.7 ± 2.3 | 7.4 ± 2.8 | *** | *** | * |
| 5) Bilateral anterior thoracotomy (clam shell) | 4.1 ± 3.6 | 7.2 ± 2.5 | 6.8 ± 2.9 | *** | *** | * |
| 6) Pulmonary hilar clamp | 3.9 ± 3.5 | 6.5 ± 2.4 | 6.4 ± 2.8 | *** | *** | ns |
| 7) Pulmonary injury | 3.9 ± 3.1 | 6.2 ± 2.7 | 6.1 ± 2.8 | *** | *** | ns |
| 8) Atrial injury | 2.6 ± 2.6 | 5.4 ± 2.4 | 5.0 ± 2.6 | *** | *** | * |
| 9) Ventricular injury | 2.5 ± 2.6 | 5.2 ± 2.4 | 5.0 ± 2.7 | *** | *** | ns |
| Vascular trauma | ||||||
| 10) Exposure of femoral vessels | 5.8 ± 3.1 | 8.0 ± 2.1 | 7.8 ± 2.3 | *** | *** | ns |
| 11) Exposure of neck vessels | 4.6 ± 2.8 | 7.1 ± 2.2 | 6.8 ± 2.4 | *** | *** | ns |
| 12) Vascular repair (direct suture, patch repair, end‐to‐end anastomosis, shunting) | 3.4 ± 2.5 | 5.8 ± 2.4 | 5.5 ± 2.5 | *** | *** | ns |
| Abdominal and pelvic trauma | ||||||
| 13) Trauma laparotomy | 6.1 ± 3.6 | 8.0 ± 2.5 | 7.6 ± 3.0 | *** | *** | * |
| 14) Portal triad clamp (Pringle's maneuver) | 5.7 ± 3.8 | 7.7 ± 2.7 | 7.3 ± 3.2 | *** | *** | ** |
| 15) Liver package | 5.3 ± 3.5 | 7.5 ± 2.6 | 7.1 ± 3.0 | *** | *** | * |
| 16) Left medial visceral rotation (Mattox maneuver) | 3.8 ± 3.3 | 6.8 ± 2.8 | 6.2 ± 3.1 | *** | *** | ** |
| 17) Right medial visceral rotation (Cattell–Braasch maneuver) | 3.8 ± 3.3 | 6.7 ± 2.9 | 6.2 ± 3.2 | *** | *** | ** |
| 18) Nephrectomy | 3.7 ± 3.2 | 6.1 ± 2.7 | 5.8 ± 3.1 | *** | *** | ns |
| 19) Abdominal damage control technique | 4.6 ± 3.2 | 6.7 ± 2.7 | 6.4 ± 2.9 | *** | *** | ns |
| 20) Pelvic package | 4.5 ± 3.3 | 7.4 ± 2.4 | 7.1 ± 2.7 | *** | *** | ns |
| Injuries to the extremities | ||||||
| 21) Fasciotomy of the lower extremity | 4.3 ± 3.0 | 6.2 ± 2.1 | 6.0 ± 2.4 | *** | *** | ns |
| Total | 4.8 ± 3.5 | 7.1 ± 2.6 | 6.8 ± 2.9 | *** | *** | *** |
Participants answered questionnaires including a self‐assessment of confidence levels for 21 surgical skills (0 points, cannot do at all; 5 points, can do with help of an adviser; 10 points, can do independently). P‐values < 0.0167 (=0.05/3 with a Bonferroni correction for multiple comparisons) were considered to be statistically significant.
*P < 0.0167 (=0.05/3); **P < 0.001; ***P < 0.0001. ns, > 0.0167.
We analyzed these results for each of the three groups. The SACL improved in all skills between before and just after the seminar in all groups (A, 6.8 ± 2.8 vs. 8.4 ± 1.9; B, 4.8 ± 3.3 vs. 7.2 ± 2.5; C, 2.3 ± 2.9 vs. 5.4 ± 2.6; P < 0.0001). The SACL did not change significantly in all skills between just after and a half‐year after the seminar in group B (7.2 ± 2.5 vs. 7.1 ± 2.6; P > 0.0167). Examining these results according to each skill, the SACL decreased in the following skills between just after and a half‐year after the seminar, respectively, in group C (P < 0.0167): left anterior thoracotomy and aortic clamp (6.3 ± 2.4 vs. 5.3 ± 2.9), bilateral anterior thoracotomy (5.6 ± 2.4 vs. 4.6 ± 2.7), atrial injury (3.6 ± 1.8 vs. 2.9 ± 2.1), ventricular injury (3.6 ± 1.9 vs. 2.8 ± 2.1), vascular repair (4.4 ± 2.1 vs. 3.7 ± 2.0), portal triad clamp (5.1 ± 2.3 vs. 4.2 ± 2.8), liver package (5.4 ± 2.4 vs. 4.5 ± 2.7), and left medial visceral rotation (4.3 ± 2.3 vs. 3.5 ± 2.7) (Table 3).
Table 3.
Self‐assessment of confidence levels for 21 surgical skills before (BS), after (AS), and a half‐year after (HS) a cadaver‐based educational seminar for trauma surgery in 135 participants grouped according to surgical experience
| Evaluation, average ± standard deviation | Significant difference | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| BS | AS | HS | AS vs. HS | ||||||||||
| A | B | C | A | B | C | A | B | C | A | B | C | ||
| Basic technique | |||||||||||||
| 1) Cricothyroidotomy | 9.3 ± 1.4 | 8.4 ± 2.1 | 6.1 ± 2.9 | 9.6 ± 1.1 | 9.3 ± 1.2 | 8.7 ± 1.8 | 9.7 ± 0.6 | 9.5 ± 0.9 | 8.3 ± 1.9 | ns | ns | ns | |
| 2) Chest tube insertion | 10.0 ± 0.1 | 9.6 ± 1.1 | 8.6 ± 2.3 | 10.0 ± 0.0 | 9.7 ± 0.8 | 9.4 ± 1.4 | 10.0 ± 0.3 | 9.8 ± 0.5 | 9.5 ± 1.2 | ns | ns | ns | |
| Thoracic trauma | |||||||||||||
| 3) Pericardial window technique | 7.0 ± 2.5 | 4.8 ± 3.0 | 2.0 ± 2.6 | 8.6 ± 1.6 | 7.6 ± 1.8 | 5.3 ± 1.8 | 8.5 ± 1.9 | 7.6 ± 2.4 | 5.1 ± 2.0 | ns | ns | ns | |
| 4) Left anterior thoracotomy & aortic clamp | 7.2 ± 2.9 | 5.2 ± 3.8 | 2.5 ± 3.1 | 9.0 ± 1.4 | 7.7 ± 2.4 | 6.3 ± 2.4 | 8.9 ± 1.7 | 7.6 ± 2.7 | 5.3 ± 2.9 | ns | ns | ** | |
| 5) Bilateral anterior thoracotomy (clam shell) | 6.2 ± 3.3 | 4.1 ± 3.3 | 1.6 ± 2.6 | 8.6 ± 1.8 | 7.3 ± 2.5 | 5.6 ± 2.4 | 8.3 ± 2.2 | 7.0 ± 2.6 | 4.6 ± 2.7 | ns | ns | * | |
| 6) Pulmonary hilar clamp | 6.2 ± 2.9 | 3.6 ± 3.3 | 1.5 ± 2.4 | 8.1 ± 1.8 | 6.5 ± 2.3 | 4.7 ± 1.8 | 8.0 ± 2.0 | 6.6 ± 2.6 | 4.3 ± 2.6 | ns | ns | ns | |
| 7) Pulmonary injury | 6.4 ± 2.0 | 3.4 ± 2.8 | 1.1 ± 2.0 | 8.0 ± 1.7 | 6.4 ± 2.4 | 3.8 ± 1.9 | 8.2 ± 1.7 | 6.3 ± 2.3 | 3.3 ± 2.0 | ns | ns | ns | |
| 8) Atrial injury | 4.5 ± 2.5 | 2.4 ± 2.2 | 0.6 ± 1.2 | 6.9 ± 2.0 | 5.4 ± 2.2 | 3.6 ± 1.8 | 6.5 ± 2.0 | 5.4 ± 2.4 | 2.9 ± 2.1 | ns | ns | ** | |
| 9) Ventricular injury | 4.2 ± 2.6 | 2.3 ± 2.2 | 0.6 ± 1.1 | 6.7 ± 1.9 | 5.1 ± 2.2 | 3.6 ± 1.9 | 6.6 ± 2.3 | 5.2 ± 2.4 | 2.8 ± 2.1 | ns | ns | ** | |
| Vascular trauma | |||||||||||||
| 10) Exposure of femoral vessels | 7.7 ± 2.1 | 5.8 ± 2.8 | 3.4 ± 2.7 | 8.9 ± 1.6 | 7.9 ± 2.2 | 7.0 ± 1.9 | 8.6 ± 1.8 | 8.0 ± 2.4 | 6.6 ± 2.3 | ns | ns | ns | |
| 11) Exposure of neck vessels | 6.1 ± 2.3 | 4.9 ± 2.4 | 2.4 ± 2.5 | 8.0 ± 1.9 | 7.1 ± 2.3 | 5.9 ± 2.0 | 7.9 ± 1.9 | 7.0 ± 2.3 | 5.3 ± 2.3 | ns | ns | ns | |
| 12) Vascular repair (direct suture, patch repair, end‐to‐end anastomosis, shunting) | 5.0 ± 2.3 | 3.2 ± 2.1 | 1.8 ± 2.0 | 7.3 ± 1.8 | 5.4 ± 2.3 | 4.4 ± 2.1 | 7.0 ± 2.1 | 5.5 ± 2.1 | 3.7 ± 2.0 | ns | ns | * | |
| Abdominal and pelvic trauma | |||||||||||||
| 13) Trauma laparotomy | 8.6 ± 2.2 | 6.5 ± 3.1 | 2.6 ± 2.7 | 9.2 ± 1.6 | 8.7 ± 2.1 | 5.8 ± 2.4 | 9.2 ± 1.9 | 8.2 ± 2.5 | 5.1 ± 2.9 | ns | ns | ns | |
| 14) Portal triad clamp (Pringle's maneuver) | 8.4 ± 2.5 | 6.1 ± 3.1 | 1.9 ± 2.6 | 9.3 ± 1.3 | 8.2 ± 2.5 | 5.1 ± 2.3 | 9.1 ± 1.8 | 8.1 ± 2.7 | 4.2 ± 2.8 | ns | ns | * | |
| 15) Liver package | 7.9 ± 2.3 | 5.4 ± 2.9 | 2.1 ± 2.7 | 9.0 ± 1.4 | 7.8 ± 2.4 | 5.4 ± 2.4 | 8.9 ± 1.8 | 7.4 ± 2.6 | 4.5 ± 2.7 | ns | ns | * | |
| 16) Left medial visceral rotation (Mattox maneuver) | 6.0 ± 2.9 | 4.0 ± 3.0 | 1.1 ± 1.9 | 8.6 ± 1.8 | 7.1 ± 2.5 | 4.3 ± 2.3 | 8.2 ± 2.0 | 6.4 ± 2.7 | 3.5 ± 2.7 | ns | ns | * | |
| 17) Right medial visceral rotation (Cattell–Braasch maneuver) | 6.2 ± 2.9 | 3.8 ± 2.9 | 1.0 ± 1.7 | 8.5 ± 1.9 | 7.0 ± 2.6 | 4.2 ± 2.2 | 8.2 ± 2.0 | 6.5 ± 2.8 | 3.4 ± 2.8 | ns | ns | ns | |
| 18) Nephrectomy | 5.9 ± 2.7 | 3.8 ± 2.6 | 0.8 ± 1.9 | 7.8 ± 1.9 | 6.4 ± 2.4 | 3.8 ± 2.1 | 7.8 ± 2.2 | 6.2 ± 2.6 | 3.1 ± 2.6 | ns | ns | ns | |
| 19) Abdominal damage control technique | 7.1 ± 2.0 | 4.6 ± 2.7 | 1.6 ± 2.1 | 8.5 ± 1.6 | 6.7 ± 2.4 | 4.4 ± 2.3 | 8.1 ± 2.1 | 6.8 ± 2.4 | 4.0 ± 2.8 | ns | ns | ns | |
| 20) Pelvic package | 6.7 ± 2.7 | 4.2 ± 3.2 | 2.2 ± 2.5 | 8.4 ± 1.7 | 7.6 ± 2.3 | 5.9 ± 2.4 | 8.3 ± 2.1 | 7.3 ± 2.6 | 5.3 ± 2.7 | ns | ns | ns | |
| Injuries to the extremities | |||||||||||||
| 21) Fasciotomy of the lower extremity | 5.5 ± 2.6 | 4.5 ± 3.0 | 2.6 ± 2.8 | 6.9 ± 2.1 | 6.1 ± 2.2 | 5.5 ± 1.9 | 6.9 ± 2.2 | 6.1 ± 2.1 | 5.0 ± 2.7 | ns | ns | ns | |
| A | B | C | |||||||||||
| Total | 6.8 ± 2.8 | 4.8 ± 3.3 | 2.3 ± 2.9 | 8.4 ± 1.9 | 7.2 ± 2.5 | 5.4 ± 2.6 | 8.2 ± 2.1 | 7.1 ± 2.6 | 4.8 ± 2.9 | *** | *** | *** | BS vs. AS |
| *** | *** | *** | BS vs. HS | ||||||||||
| * | ns | *** | AS vs. HS | ||||||||||
A, Highly experienced group (n = 50); B, experienced group (n = 44); C, little‐experienced group (n = 41).
The participants answered the questionnaires including a self‐assessment of confidence levels for 21 surgical skills (0 points, cannot do at all; 5 points, can do with help of an adviser; 10 points, can do independently). P‐values < 0.0167 (=0.05/3 with a Bonferroni correction for multiple comparisons) were considered to be statistically significant.
*P < 0.0167 (=0.05/3); **P < 0.001; ***P < 0.0001. ns, >0.0167.
Additionally, we analyzed these results according to workplace, that is, emergency center or non‐emergency center. The SACL did not change significantly in all skills between just after and a half‐year after the seminar among members of groups A and B belonging to an emergency center (A, 8.6 ± 1.7 vs. 8.7 ± 1.7; B, 7.4 ± 2.4 vs. 7.6 ± 2.4; P > 0.0167) and C group members belonging to a non‐emergency center (4.3 ± 2.2 vs. 4.1 ± 2.9; P > 0.0167) (Table 4).
Table 4.
Self‐assessment of confidence levels for 21 surgical skills before (BS), after (AS), and a half‐year after (HS) a cadaver‐based educational seminar for trauma surgery in 135 participants grouped according workplace (emergency center or non‐emergency center)
| Evaluation, average ± standard deviation | Significant difference | ||||||
|---|---|---|---|---|---|---|---|
| Workplace | BS | AS | HS | BS vs. AS | BS vs. HS | AS vs. HS | |
| Emergency center | |||||||
| A | 25 | 7.6 ± 2.3 | 8.6 ± 1.7 | 8.7 ± 1.7 | *** | *** | ns |
| B | 27 | 5.7 ± 3.0 | 7.4 ± 2.4 | 7.6 ± 2.4 | *** | *** | ns |
| C | 33 | 2.5 ± 3.1 | 5.6 ± 2.6 | 4.9 ± 2.9 | *** | *** | *** |
| Total | 85 | 5.0 ± 3.5 | 7.1 ± 2.6 | 6.9 ± 2.9 | *** | *** | *** |
| Non‐emergency center | |||||||
| A | 25 | 5.9 ± 3.1 | 8.1 ± 2.0 | 7.8 ± 2.4 | *** | *** | *** |
| B | 17 | 3.3 ± 3.1 | 6.8 ± 2.6 | 6.3 ± 2.8 | *** | *** | *** |
| C | 8 | 1.3 ± 2.2 | 4.3 ± 2.2 | 4.1 ± 2.9 | *** | *** | ns |
| Total | 50 | 4.3 ± 3.5 | 7.1 ± 2.6 | 6.7 ± 2.9 | *** | *** | *** |
A, Highly experienced group; B, experienced group; C, little‐experienced group.
The participants answered questionnaires including a self‐assessment of confidence levels for 21 surgical skills (0 points, cannot do at all; 5 points, can do with help of an adviser; 10 points, can do independently). P‐values < 0.0167 (= 0.05/3 with a Bonferroni correction for multiple comparisons) were considered to be statistically significant.
*P < 0.0167 (=0.05/3); **P < 0.001; ***P < 0.0001. ns, >0.0167.
Discussion
We developed an original cadaver‐based educational seminar for trauma surgery cooperating with the Department of Anatomy (Tokyo Medical University, Tokyo, Japan). We started the seminar in 2007 for the faculty, residents, and medical students of our department, and surgeons of affiliated hospitals. This seminar was continued eight times until 2011, and the cumulative total of participants was 93. We asked the participants to answer simple questionnaires before and after the seminar. The number of skills that participants thought to be able to do by themselves increased in 72.5% of the participants, and all participants answering this seminar questionnaire believed it to be useful for trauma surgery education.7 We confirmed whether our seminar conformed with the “Guidelines for surgical training using cadavers” after the guidelines were announced in 2012. At first, our seminar corresponded with “It established skill, however difficult for training on the job or on the animal model because of its high level technique” which is one of the regulated conditions of the guidelines. We confirmed the legal conditions next. We received approval from the Tokyo Medical University body donation society “Toju‐kai” and we obtained consent from the donors and their families while the donors were alive. Furthermore, we consulted with the Tokyo Medical University Medical Ethics Committee and obtained approval. Finally, we confirmed that our seminar was fully compliant with the guidelines. Afterwards, we re‐started our seminar for not only our university and affiliated hospitals, but also other universities or hospitals by public announcement.
The ASSET course adopts a five‐point SACL (ranging from 1 [little confidence] to 5 [extreme confidence]) for the participants, and reported that SACL improved after the course.4 Our seminar adopted a 10‐point SACL. We subdivided the point score to understand participants' confidence in detail. The SACL improved in all skills between before and just after the seminar among all participants. The results were the same when we re‐analyzed this in the three experienced groups. We also added a free‐response column in the questionnaire just after the seminar. The impressions were different depending on the background of the participants. The emergency specialists and surgeons answered that this seminar was very effective for trauma surgical education. The residents answered that this seminar was effective; however, they felt anxiety in practicing skills by themselves. Furthermore, the skills that participants desired to develop were also different, depending on the background.
There are few reports about cadaver surgical training courses for trauma that analyze the retention of participants' skills. Gunst et al.8 undertook an original 1‐day trauma exposure course with cadavers. They also adopted a 5‐point SACL for the total of 18 participants as assessment before, immediately after, and several months (median, 6 months) after the course. They reported that SACL improved after the course, and did not decline several months after. However, this was a limited result because the number of participants was small. We e‐mailed questions to participants, including a SACL, regarding 21 surgical skills a half‐year after the seminar. The SACL decreased in all skills between just after and a half‐year after the seminar among all participants. Examining this result according to each skill, the SACL decreased in several skills between just after and a half‐year after the seminar. The all‐participants' results were almost the same as group C participants' results. This means that group C participants' results affected the all‐participants' results.
The SACL decreased in all skills between just after and a half‐year after the seminar among group A, although the SACL did not decrease in each skill. We supposed that group A contained many general surgeons who engaged in little trauma surgery, and their confidence affected group A's result. To examine this supposition, we re‐analyzed these results according to workplace, namely, emergency center or non‐emergency center. The SACL did not decrease in all skills between just after and a half‐year after the seminar among participants in group A and B who worked in an emergency center. The SACL also did not decrease in all skills between just after and a half‐year after the seminar among participants in group C who worked at a non‐emergency center. However, the number of participants in this subgroup was small (n = 8), and four of them were orthopedists or general surgeons who were applying for board certification. Our results suggest that participants who belong to an emergency center in which trauma surgery was practiced usually can maintain the skills. Therefore, practicing skills covered by the seminar is effective for skills retention.
We also added a free‐response question by e‐mail, asking whether participants practiced skills in their clinical work a half‐year after the seminar. The cumulative number of practiced skills are shown in Table 5. Some participants answered that they were able to practice skills for cases in which they had never attempted operations before. The answer of a veteran neurosurgeon (PGY33) was impressive. He encountered an acute airway obstructive case in which he could not perform oral intubation, so he successfully performed a cricothyroidotomy, which he had never attempted before. Many participants answered that they wanted to practice skills when they encountered cases. Some gastroenterological surgeons answered that the vascular repair skill was helpful in treating unexpected bleeding at scheduled operations. Some senior participants answered that the seminar was useful in teaching operative skills for residents.
Table 5.
Skills practiced by 135 participants a half‐year after completing a one‐day cadaver‐based educational seminar for trauma surgery
| Cumulative number, n | Total | |||
|---|---|---|---|---|
| A | B | C | ||
| Pericardial window technique | 3 | 1 | 1 | 5 |
| Left anterior thoracotomy | 2 | 3 | 3 | 8 |
| Thoracic aortic clamp | 2 | 1 | 2 | 5 |
| Bilateral anterior thoracotomy | 4 | 1 | 2 | 7 |
| Pulmonary hilar clamp | 2 | 2 | 0 | 4 |
| Pelvic package | 2 | 1 | 1 | 4 |
| Other skills | 5 | 6 | 3 | 14 |
| Total | 20 | 15 | 12 | 47 |
A, Highly experienced group; B, experienced group; C, little‐experienced group.
A free‐response question was e‐mailed to participants a half‐year after the seminar, asking whether participants had practiced skills covered by the seminar in their clinical work.
Regarding the evaluation method for the seminar participants, we adopted only a 10‐point SACL. Some recent ASSET courses have adopted other evaluation methods. Shackelford et al. reported measuring the time to complete vascular control, and the mean time decreased significantly after ASSET training.9 Mackenzie et al. reported using the individual procedure score for evaluation, and the score increased after ASSET training.10 We think that measuring the time to complete skills or adopting complex evaluation methods are doubtful for cadaver surgical training because these evaluations disturb the principal of our seminar, namely, “Teach clinical anatomy gently and by taking time”, although those are better objective evaluations. Actually, participants often trained for the skills while they discussed their surgical experiences in their groups. Participants sometimes explained and taught about their specialties to group members, including instructors. There were many opinions voiced after the seminar that this mini‐discussion was good.
We consider target participants to be senior residents, physicians, and surgeons who are working in an emergency (trauma) center, or surgeons who do not routinely engage in emergency care, but need to engage when trauma patients are brought to the hospital. In this study, the SACL did not decrease in all skills between just after and a half‐year after the seminar among group B participants. Most in this group belonged to an emergency center, and had surgical skills. This was the reason why the retention of group B was high. Suitable participants for seminars might be similar to those in group B. The surgeons who do not routinely engage in emergency care, for example, gastroenterological surgeons, do not fully experience thoracic, vascular, retroperitoneal, pelvic, and extremities injury. The seminar provided a good training opportunity for them. Once the seminar provides the skill, they can practice it easily, because they already have basic surgical techniques. However, they lose confidence when time passes without practice. There are several reports about retention of laparoscopic surgical training and educational effect. These reports suggest that participating in the seminar repeatedly is effective for skills retention.11, 12 Therefore, if the surgeons cannot practice the skills in their workplace, their repeated participation in the seminar seems to be effective to prevent losing confidence.
Our seminars use cadavers fixed principally in formalin and thus participants could not experience the actual feeling of organs, observe bleeding, nor experience elasticity. Recently, we reported that the use of cadavers embalmed by the “saturated salt solution (SSS)” method, which was first developed by Coleman and Kogan,13 contributed to solving such problems considerably.14, 15 Actually, we held a 1‐day cadaver‐based advanced educational seminar to discuss trauma surgery with SSS‐embalmed cadavers in September, 2015.
Conclusions
Acadaver‐based seminar provides more self‐confidence just after the seminar for participants at all experience levels. This effect is not maintained after a half‐year, except in participants who can practice the skills in an emergency center. Practicing and participating in the seminar repeatedly is suggested to be effective for skills retention in trauma surgery.
This may be the first report about cadaver surgical training that investigates skills retention after a half‐year follow‐up in detail.
Conflict of interest
None.
Acknowledgments
The authors wish to thank Ms. Manami Mishima, Ms. Shihoko Komoda, Ms. Chieko Kusumoto, Ms. Itsuko Kumagai, Ms. Yuki Ogawa, and Mr. Koichi Koyama for excellent secretarial and technical assistance. The authors respect and appreciate cadaver donors and their families.
[The copyright line for this article was changed on 31 October 2016 after original online publication]
References
- 1. Advanced Trauma Operative Management [homepage on the internet]. American college of surgeons committee on trauma [cited 7 March 2012]. Available from: https://www.facs.org/quality%20programs/trauma/education/atom.
- 2. Definitive Surgical Trauma Care Courses [homepage on the internet]. International Association for Trauma Surgery and Intensive Care [cited 18 October 2009]. Available from: http://www.iatsic.org/DSTC.html.
- 3. Ryan JM, Roberts P. Definitive surgical trauma skills: a new skills course for specialist registrars and consultants in general surgery in the United Kingdom. Trauma 2002; 4: 184–8. [Google Scholar]
- 4. Bowyer MW, Kuhls DA, Haskin D, et al Advanced surgical skills for exposure in trauma (ASSET): the first 25 courses. J. Surg. Res. 2013; 183: 553–8. [DOI] [PubMed] [Google Scholar]
- 5. Murakami G. Fresh cadaver dissection for surgical education and consent of donor. Japan Med. J. 2005; 4261: 53–8. [Google Scholar]
- 6.“Guideline of the surgical training using cadaver ” [homepage on the internet] Japan Surgical society [cited 20 June 2012]. Available from: https://www.jssoc.or.jp/journal/guideline/info20120620.html.
- 7. Homma H, Kaneko N, Oda J, et al The trauma operation skill study seminar with human cadavers: Approach for Japanese version DSTS. Jpn. J. Acute Care Surg. 2012; 2: 55–61. [Google Scholar]
- 8. Gunst M, O'Keeffe T, Hollett L, et al Trauma Operative Skills in the Era of Nonoperative Management: the Trauma Exposure Course (TEC). J. Trauma Acute Care Surg. 2009; 67: 1091–6. [DOI] [PubMed] [Google Scholar]
- 9. Shackelford S, Garofalo E, Shalin V, et al Development and validation of trauma surgical skills metrics: preliminary assessment of performance after training. J. Trauma Acute Care Surg. 2015; 79: 105–10. [DOI] [PubMed] [Google Scholar]
- 10. Mackenzie CF, Garofalo E, Shackelford S, et al Using an Individual Procedure Score Before and After the Advanced Surgical Skills Exposure for Trauma Course Training to Benchmark a Hemorrhage‐Control Performance Metric. J. Surg. Educ. 2015; 72: 1278–89. [DOI] [PubMed] [Google Scholar]
- 11. Varley M, Choi R, Kuan K, et al Prospective randomized assessment of acquisition and retention of SILS skills after simulation training. Surg. Endosc. 2015;29:113–8. [DOI] [PubMed] [Google Scholar]
- 12. Bruwaene SV, Schijven MP, Miserez M, et al Maintenance training for laparoscopic suturing: the quest for the perfect timing and training model: a randomized trial. Surg. Endosc. 2013; 27: 3823–9. [DOI] [PubMed] [Google Scholar]
- 13. Coleman R, Kogan I. An improved low‐formaldehyde embalming fluid to preserve cadavers for anatomy teaching. J. Anat. 1998; 192: 443–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hayashi S, Homma H, Naito M, et al Saturated salt solution method: a useful cadaver embalming for surgical skills training. Medicine 2014; 93: e196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Hayashi S, Naito M, Kawata S, et al History and future of human cadaver preservation for surgical training: from formalin to saturated salt solution method. Anat. Sci. Int. 2016; 91: 1–7. [DOI] [PubMed] [Google Scholar]


