Abstract
Case
A 49‐year‐old man had idiopathic epilepsy with recurrent convulsions and history of cleft palate, mental retardation, schizophrenia, and cataract. He had convulsions the day before and on the day of admission. Fosphenytoin was given i.v.; his convulsion stopped, but he lost consciousness 2 h later and was admitted. Glasgow Coma Scale score on arrival was 3. Cerebral computed tomography showed bilateral calcification in the basal ganglia. Laboratory tests showed decreased serum calcium and albumin and increased creatine kinase. He regained consciousness after i.v. calcium gluconate administration. Additionally, he showed decreased parathyroid hormone and 1,25(OH)2 vitamin D. Suspecting hypoparathyroidism, i.v. calcium gluconate was changed to oral vitamin D. His medical history and physical appearance suggested 22q11.2 deletion syndrome, confirmed by chromosomal analysis.
Outcome
The patient was discharged after 29 days and remains convulsion‐free.
Conclusion
Hypocalcemia due to hypoparathyroidism should be considered in the differential diagnosis of adult recurrent convulsions.
Keywords: Convulsion, hypocalcemia, hypoparathyroidism, 22q11.2 deletion syndrome
Introduction
Convulsions account for approximately 1% of all emergency outpatients.1 Hypocalcemia due to hypoparathyroidism can cause secondary convulsions,2, 3, 4 but this condition is usually diagnosed in newborns or during early adulthood.2, 3, 4, 5, 6 Delayed diagnosis until middle age has been considered extremely rare; however, 22q11.2 deletion syndrome, a relatively frequent cause of hypoparathyroidism, is the most common microdeletion syndrome in humans (1:4,000 live births), with autosomal dominant inheritance pattern.7 We describe an alarming case of hypoparathyroidism related to 22q11.2 deletion syndrome diagnosed in a middle‐aged patient with recurrent convulsions, and we highlight the need for recognition of this disease among emergency physicians.
Case
A 49‐year‐old man with a history of idiopathic epilepsy was admitted to our hospital because of recurrent convulsions. The patient had been treated with valproic acid but he discontinued treatment; at 36 years of age, he experienced a flare‐up of epileptic manifestations. Valproic acid was reinitiated and he received psychiatric follow‐up treatment. Additionally, he had a medical history of cleft palate, mental retardation, schizophrenia, and cataract and took haloperidol. He lived in a vocational training facility.
One day before admission, he had a brief generalized convulsion. The next day, he had another convulsion and was taken by ambulance to his psychiatrist. Fosphenytoin was administered i.v. and his convulsion stopped. Two hours later, he lost consciousness and was admitted to our medical emergency center. On arrival, his Glasgow Coma Scale score was 3 on a scale of 3–15. His temperature was 37.8°C, blood pressure was 120/70 mmHg, pulse was 56/min, respiratory rate was 20/min, and oxygen saturation was 100% in ambient air. Cerebral computed tomography showed bilateral calcification in the basal ganglia (Fig. 1A). Laboratory tests showed serum calcium, 4.4 mg/dL (normal range, 8.2–10.2); serum phosphate, 5.5 mg/dL (normal range, 2.5–5.5); serum albumin, 3.0 mg/dL (normal range, 3.5–5.5); and creatine kinase, 7,026 U/L (normal range, 40–200). Cerebrospinal fluid examination showed no abnormalities. Calcium gluconate was given i.v. and he gradually regained consciousness. Considering his past medical history, he was diagnosed with chronic hypocalcemia. Additional laboratory tests revealed intact parathyroid hormone, 7 pg/mL (normal range, 10–65) and 1,25(OH)2 vitamin D, 14 pg/mL (normal range, 20–60). Hypoparathyroidism was strongly suspected. Intravenous calcium gluconate was changed to an oral vitamin D preparation, and he was transferred to the general ward.
Figure 1.
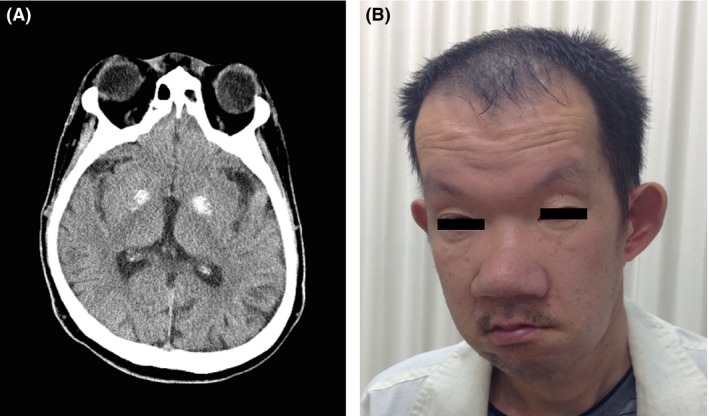
A, Computed tomography of a 49‐year‐old man with idiopathic epilepsy and recurrent convulsions. The scan of the patient's head at admission showed bilateral calcification in the basal ganglia. B, The patient had narrowing of the palpebral fissure, eyelid swelling, and a flat nasal root.
At first, unusual computed tomography findings of calcifications on bilateral basal ganglia led us to suspect 22q11.2 deletion syndrome. Moreover, the patient's medical history with persistent hypocalcemia and recurrent convulsions also led to this diagnosis. Narrowing of the palpebral fissure, eyelid swelling, and a flat nasal root (Fig. 1B), which was reminiscent of 22q11.2 deletion syndrome, confirmed our diagnosis. After obtaining informed consent, a chromosomal study provided a definitive diagnosis of 22q11.2 deletion syndrome (Fig. 2). The patient was discharged 29 days after admission. He has remained convulsion‐free for 1 year since his discharge, without additional anticonvulsants.
Figure 2.
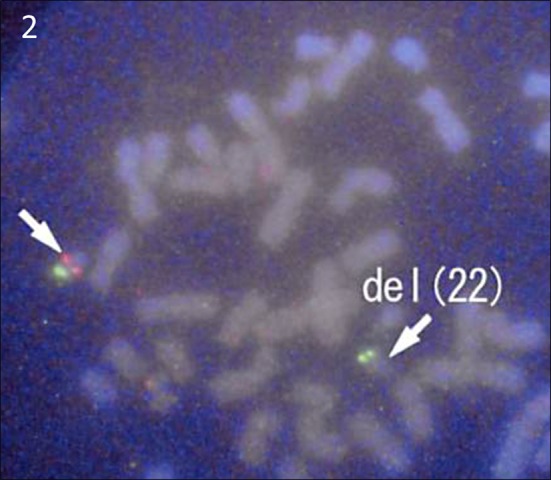
Chromosomal study provided a definitive diagnosis of 22q11.2 deletion syndrome. Arrows show heterozygous deletion in chromosome 22q11.2.
Discussion
In the current case, the patient experienced recurrent convulsions and hypocalcemia caused by hypoparathyroidism related to 22q11.2 deletion syndrome, which was finally diagnosed at 49 years of age. There were two possible reasons why this patient with hypoparathyroidism had a delayed diagnosed. First, the patient had been followed‐up by psychiatrists due to a diagnosis of schizophrenia. The treating psychiatrist had apparently not determined his calcium levels and he was followed‐up with an outpatient service. Second, valproic acid had been administered, which has the potential to induce hypocalcemia as a side‐effect related to bone turnover.8 Therefore, physicians may have recognized his hypocalcemia as effects of valproic acid administration.
With early diagnosis of hypoparathyroidism related to 22q11.2 deletion syndrome, three beneficial points are considered. First, adequate calcium supplementation may allow withdrawal from antiepileptic drug treatment in patients with recurrent convulsions.9 Second, appropriate convulsion control can decrease the recurrence of convulsions, preventing further brain damage. Third, vitamin D replacement therapy remains the standard care for hypoparathyroidism and parathyroid hormone 1‐84 is not yet designated as an initial therapy due to its high cost, the necessity for s.c. administration, and uncertainty about the long‐term safety of dosing to treat primary hypoparathyroidism. However, a systematic review carried out by Ramakrishnan et al. suggested that recombinant parathyroid hormone is useful for normalizing serum calcium levels, which may be a promising treatment for hypoparathyroidism.10
Emergency physicians should consider hypocalcemia due to hypoparathyroidism in their differential diagnosis when managing an adult patient without a clear cause for recurrent convulsions. Hypoparathyroidism associated with psychiatric illness should also be considered suggestive of 22q11.2 deletion syndrome, which is a relatively frequent cause of parathyroid insufficiency.7
Conflict of Interest
None.
References
- 1. Krumholz A, Grufferman S, Orr ST, Stern BJ. Seizures and seizure care in an emergency department. Epilepsia 1989; 30: 175–81. [DOI] [PubMed] [Google Scholar]
- 2. Eom TH, Kim YH, Kim JM. Recurrent seizures, mental retardation and extensive brain calcinosis related to delayed diagnosis of hypoparathyroidism in an adolescent boy. J. Clin. Neurosci. 2015; 22: 894–6. [DOI] [PubMed] [Google Scholar]
- 3. Maeda K, Sekine O. Reading epilepsy as the initial symptom of idiopathic hypoparathyroidism. Intern. Med. 2011; 50: 1235–7. [DOI] [PubMed] [Google Scholar]
- 4. Belluzzo M, Monti F, Pizzolato G. A case of hypocalcemia‐related epilepsia partialis continua. Seizure 2011; 20: 720–2. [DOI] [PubMed] [Google Scholar]
- 5. Christopher RH, David KV, Pricilla RA. Primary hypoparathyroidism presenting with new adult onset seizures in family practice. J. Family Med. Prim. Care 2014; 3: 266–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Cao Z, Yu R, Dun K, Burke J, Caplin N, Greenaway T. 22q11.2 deletion presenting with severe hypocalcaemia, seizure and basal ganglia calcification in an adult man. Intern. Med. J. 2011; 41: 63–6. [DOI] [PubMed] [Google Scholar]
- 7. Passeri E, Frigerio M, Valaperta R, Costa E, Ambrosi B, Corbetta S. Adult onset hypoparathyroidism in a patient with psychiatric illness: a 71 years delayed diagnosis of DiGeorge syndrome. J. Endocrinol. Invest. 2010; 33: 852–3. [DOI] [PubMed] [Google Scholar]
- 8. Pratico AD, Pavone P, Scuderi MG, Li Volti G, Bernardini R, Cantarella G, et al Symptomatic hypocalcemia in an epileptic child treated with valproic acid plus lamotrigine: a case report. Cases J. 2009; 2: 7394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Modi S, Tripathi M, Saha S, Goswami R. Seizures in patients with idiopathic hypoparathyroidism: effect of antiepileptic drug withdrawal on recurrence of seizures and serum calcium control. Eur. J. Endocrinol. 2014; 170: 777–83. [DOI] [PubMed] [Google Scholar]
- 10. Ramakrishnan Y, Cocks HC. Impact of recombinant PTH on management of hypoparathyroidism: a systematic review. Eur. Arch. Otorhinolaryngol. 2016; 273(4): 827–35. [DOI] [PubMed] [Google Scholar]


