Abstract
Case
We report a case of H1N1 influenza‐associated respiratory failure with severe obesity.
Outcome
A 54‐year‐old man was admitted to our intensive care unit (ICU) because of H1N1 influenza‐associated severe respiratory failure. He was severely obese, having a body mass index of 37.2. His respiratory condition remained severe under mechanical ventilation. We started veno‐venous extracorporeal membrane oxygenation immediately. Awake management was started on ICU Day 6, and the patient's respiratory physical therapy began the following day. His respiratory condition showed excellent improvement immediately following the initiation of respiratory physical therapy. The patient was successfully decannulated on ICU Day 9, and he was discharged from the ICU on Day 11. He was discharged from the hospital with no severe disability on disease Day 60.
Conclusion
Awake extracorporeal membrane oxygenation management with early respiratory physical therapy can be useful in the treatment of morbidly obese patients who present with severe respiratory failure.
Keywords: Extracorporeal membrane oxygenation, H1N1 influenza, obesity, respiration, respiratory physical therapy
Introduction
Veno‐venous extracorporeal membrane oxygenation (VV‐ECMO) is a clinically effective treatment for acute respiratory distress syndrome (ARDS).1 In patients with severe respiratory failure due to H1N1 influenza infection, VV‐ECMO is feasible and effective.2 However, the respiratory condition of obese patients is exacerbated by factors in addition to influenza. It is necessary to create a strategy for dealing with the respiratory effects from obesity. In this report, we discuss successful case management using awake VV‐ECMO and early respiratory physical therapy on an H1N1 influenza‐associated pneumonia patient with severe obesity.
Case
A 54‐year‐old man was admitted to our intensive care unit (ICU) because of H1N1 influenza‐associated severe respiratory failure. He had a history of hypertension, hyperuricemia and asthma. He consulted with a family doctor because of fever on disease Day 2. A diagnosis of influenza A was made by the rapid test, and zanamivir was prescribed. He consulted a Level II hospital because of dyspnea on that night and was admitted. Despite intense respiratory management and anti‐influenza drug treatment, his respiratory condition deteriorated.
On disease Day 3, he was transported to our ICU for further management.
The patient's height was 175 cm and his weight was 114 kg. His body mass index was 37.2. Bilateral consolidation and atelectasis were discovered in his chest imaging examination (Fig. 1). The mechanical ventilation mode included airway pressure release ventilation, with an inspiratory fraction of oxygen measure (FIO2) of 1.0, a pressure high of 20 cmH2O, a pressure low of 0 cmH2O, a time high of 3.0 s, and a time low of 0.5 s. His lung compliance was 16 mL/cmH2O. Blood gas analysis showed poor oxygenation and ventilation (pH 7.25, PaCO2 89 mmHg, PaO2 75 mmHg, HCO3 − 30 mmol/L). His PaO2/FIO2 ratio was 75, and his Murray score was 3.5. We started VV‐ECMO immediately, and the mechanical ventilation was changed to a lung‐rest setting. The patient was treated with a 25 Fr. cannula for drainage into his right atrium through the right internal jugular vein, and a 19 Fr. cannula for blood infusions into his right femoral vein. We used a magnetically driven centrifugal pump (Rotaflow Maquet, Rastatt, Germany) and a polymethylpentene oxygenator (BioCube NIPRO, Osaka, Japan).
Figure 1.
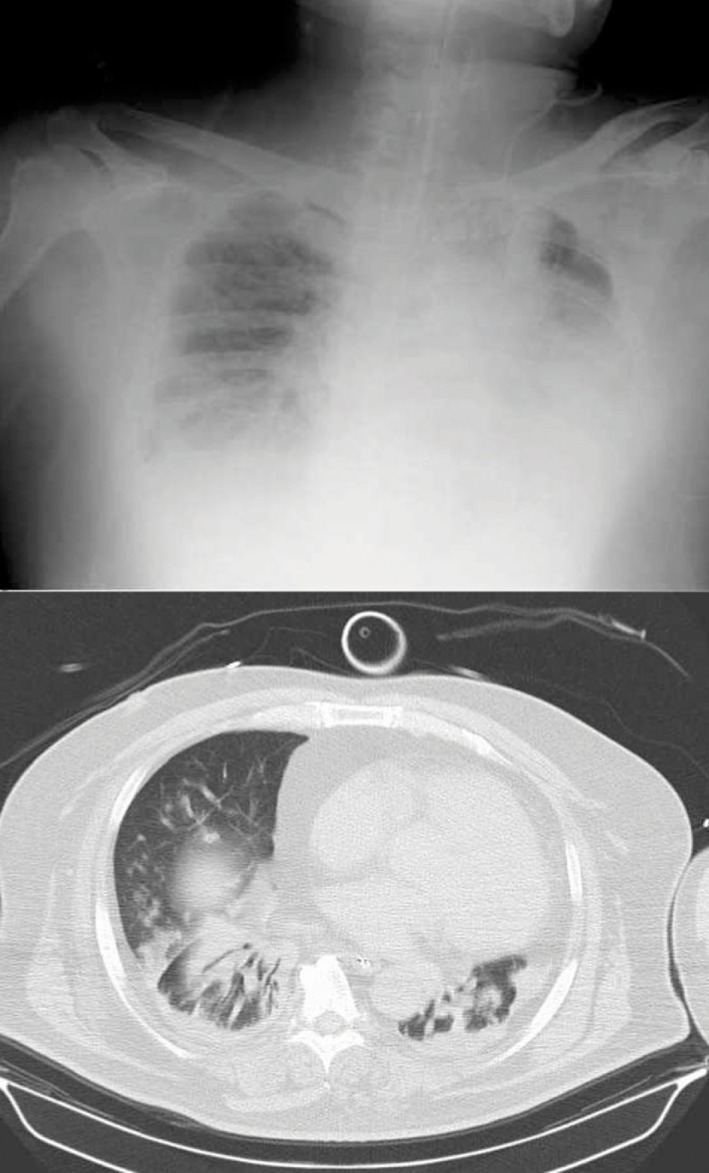
Chest X‐ray and computed tomography scans of a 54‐year‐old man with H1N1 influenza‐associated pneumonia on the first day of admission to the intensive care unit. These images show bilateral consolidation and atelectasis.
An anti‐influenza drug (peramivir) and antibiotics (meropenem, levofloxacin, and vancomycin) were given. The rapid nasopharyngeal swab specimen tested at our hospital was also positive for the influenza type A antigen. The polymerase chain reaction of the specimen was positive for influenza A H1N1pdm09. The sputum bacterial culture was negative.
The patient underwent tracheostomy on ICU Day 5. We started the awake ECMO management on ICU Day 6, and the patient started respiratory physical therapy on ICU Day 7 (Fig. 2). We discontinued sedative drug treatment in the daytime. The patient took a seated position on the edge of the bed while in respiratory physical therapy, which was undertaken for at least 15 min a day. No circuit trouble occurred during the respiratory physical therapy. His atelectasis and respiratory condition showed excellent improvement immediately following the initiation of respiratory physical therapy (Fig. 2). The patient was successfully decannulated on ICU Day 9. The imaging examination after decannulation showed the improvements in bilateral consolidation and atelectasis (Fig. 3). The patient was discharged from the ICU on disease Day 14. After that, he was transferred to a local hospital to continue his treatment and rehabilitation. On disease Day 60, he was discharged from the hospital with no evidence of severe disabilities.
Figure 2.
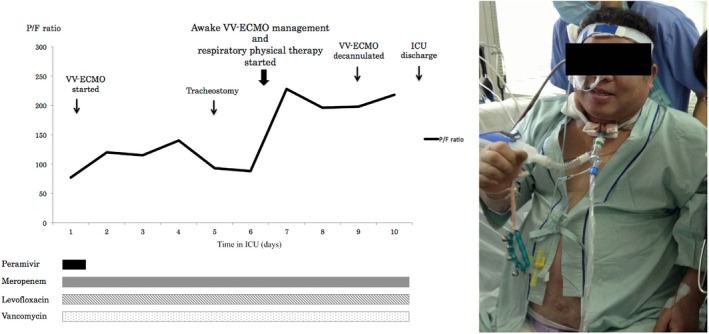
Clinical course of a 54‐year‐old man with H1N1 influenza‐associated pneumonia after admission to the intensive care unit (ICU) (left) and the respiratory physical therapy setup (right). The patient's PaO 2/FIO 2 (P/F) ratio showed excellent improvement immediately following respiratory physical therapy initiation. VV‐ECMO, veno‐venous extracorporeal membrane oxygenation.
Figure 3.
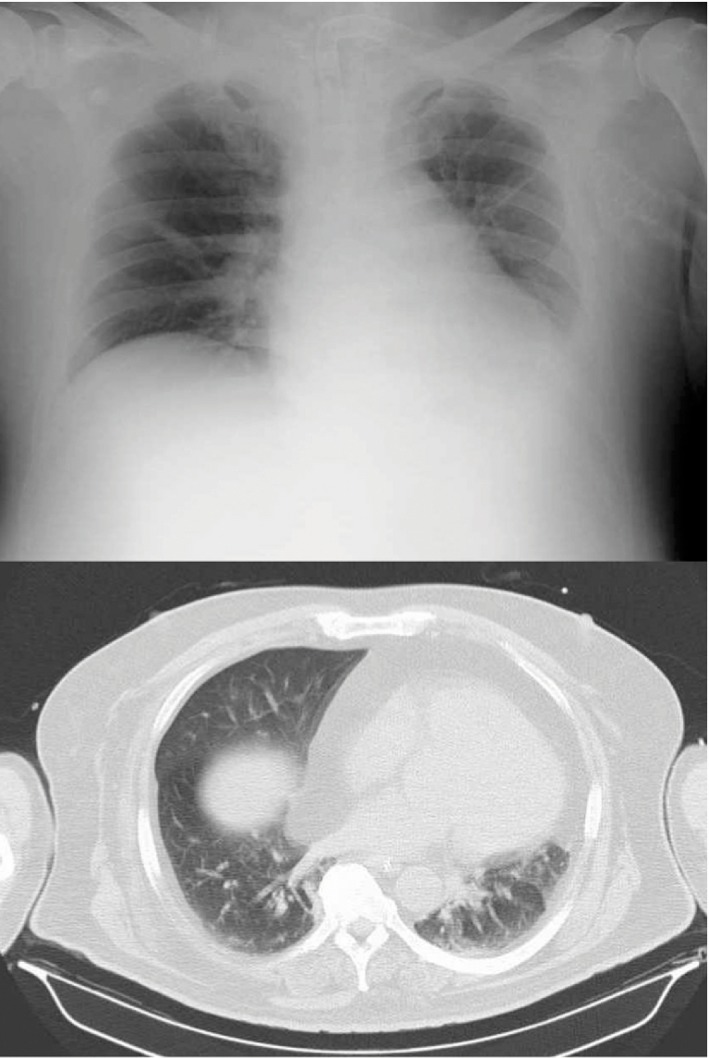
Chest X‐ray and computed tomography scans of a 54‐year‐old man with H1N1 influenza‐associated pneumonia after decannulation. These images show improvements in bilateral consolidation and atelectasis.
Discussion
Veno‐venous extracorporeal membrane oxygenation is useful for treating H1N1 influenza‐associated pneumonia.2 However, the respiratory condition of this patient was exacerbated by concomitant severe obesity. In obese patients, thoracic cage compliance is declined by excessive soft tissue. The position of the diaphragm is affected by the abdominal contents, and functional residual capacity is reduced.3 Atelectasis can develop and ventilation–perfusion ratio mismatch occurs.
Veno‐venous extracorporeal membrane oxygenation support alone was not enough; respiratory physical therapy was also required. Raising the body up is valuable for improving the respiratory conditions of obese patients.4 In order to allow the patient to undergo respiratory physical therapy with ease, we chose awake VV‐ECMO management. While we used the femoral vein for blood infusions, no circuit trouble occurred. The respiratory physical therapy could be carried out safely, even though the femoral vein was used for cannulation. Although prone positioning is an intervention technique that is used in the treatment of ARDS as well, Weig et al. reported the possibility of complications such as renal failure and hypoxic hepatitis when prone positioning is used in abdominally obese patients.5 For this reason, we did not choose prone positioning in this case study.
Linden et al. previously reported high survival rates in adult patients with severe ARDS using ECMO and pressure‐supported ventilation with minimal sedation.6 Awake management provides an increase of ventilation volume and pulmonary lymph flow, an improvement of hemodynamics, and better communication with the patient.7 Awake VV‐ECMO management and respiratory physical therapy facilitated the successful recovery of the patient's respiratory condition.
Conclusion
We reported a case of H1N1 influenza‐associated pneumonia in a severely obese patient. Awake VV‐ECMO management with early respiratory physical therapy facilitated the recovery of the patient's respiratory condition. Our findings have great implications for improving respiratory failure care for patients with severe obesity.
Conflict of Interest
None.
References
- 1. Peek GJ, Mugford M, Tiruvoipati R et al Efficacy and economic assessment of conventional ventilatory support versus extracorporeal membrane oxygenation for severe adult respiratory failure (CESAR): A multicenter randomized controlled trial. Lancet 2009; 374: 1351–1363. [DOI] [PubMed] [Google Scholar]
- 2. Zangrillo A, Biondi‐Zoccai G, Landoni G et al Extracorporeal membrane oxygenation (ECMO) in patients with H1N1 influenza infection: A systematic review and meta‐analysis including 8 studies and 266 patients receiving ECMO. Crit. Care 2013; 17: R30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Gibson GJ. Obesity, respiratory function and breathlessness. Thorax 2000; 55 (Suppl. 1): S41–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Vaughan RW, Bauer S, Wise L. Effect of position (semirecumbent versus supine) on postoperative oxygenation in markedly obese subjects. Anesth. Analg. 1976; 55: 37–41. [PubMed] [Google Scholar]
- 5. Weig T, Janitza S, Zoller M et al Influence of abdominal obesity on multiorgan dysfunction and mortality in acute respiratory distress syndrome patients treated with prone positioning. J. Crit. Care 2014; 29: 557–561. [DOI] [PubMed] [Google Scholar]
- 6. Linden V, Palmer K, Reinhard J et al High survival in adult patients with acute respiratory distress syndrome treated by extracorporeal membrane oxygenation, minimal sedation, and pressure supported ventilation. Intensive Care Med. 2000; 26: 1630–1637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Aokage T, Takeda S. Extracorporeal membrane oxygenation (ECMO) for severe respiratory failure due to influenza pneumonia. J. Jpn. Soc. Intensive Care Med. 2014; 21: 478–480. [Google Scholar]


