Abstract
Background: Non-traumatic spinal cord dysfunction (SCDys) is caused by a large range of heterogeneous etiologies. Although most aspects of rehabilitation for traumatic spinal cord injury and SCDys are the same, people with SCDys have some unique rehabilitation issues. Purpose: This article presents an overview of important clinical rehabilitation principles unique to SCDys. Methods: Electronic literature search conducted (January 2017) using MEDLINE and Embase (1990–2016) databases for publications regarding SCDys. The focus of the literature search was on identifying publications that present suggestions regarding the clinical rehabilitation of SCDys. Results: The electronic search of MEDLINE and Embase identified no relevant publications, and the publications included were from the authors' libraries. A number of important clinical rehabilitation principles unique to people with SCDys were identified, including classification issues, general rehabilitation issues, etiology-specific issues, and a role for the rehabilitation physician as a diagnostic clinician. The classification issues were regarding the etiology of SCDys and the International Standards for Neurological Classification of Spinal Cord Injury. The general rehabilitation issues were predicting survival, improvement, and rehabilitation outcomes; admission to spinal rehabilitation units, including selection decision issues; participation in rehabilitation; and secondary health conditions. The etiology-specific issues were for SCDys due to spinal cord degeneration, tumors, and infections. Conclusions: Although there are special considerations regarding the rehabilitation of people with SCDys, such as the potential for progression of the underlying condition, functional improvement is typically significant with adequate planning of rehabilitation programs and special attention regarding the clinical condition of patients with SCDys.
Keywords: non-traumatic spinal cord injury, patient care management, rehabilitation, review, spinal cord damage, spinal cord diseases, spinal cord dysfunction, spinal cord injury
Non-traumatic spinal cord dysfunction (SCDys) refers to spinal cord damage that is not caused by trauma. The etiology of SCDys is extremely varied and heterogeneous,1 with the most common causes being degenerative conditions of the spinal column, benign and malignant tumors, vascular problems resulting in infarction or hemorrhage, infections, or inflammation.2,3
The incidence of SCDys is difficult to estimate due to its heterogeneous etiology and lack of reporting in most countries. However, the incidence of SCDys is estimated to be much higher than the incidence of traumatic spinal cord injury (SCI) in many developed countries.3,4 The incidence of SCDys in Canada is estimated to be 68 per million,5 and in the State of Victoria, Australia, the incidence rate is estimated as 26 per million.6 Furthermore, the incidence of SCDys varies by both age and gender. The incidence of SCDys in females is much higher than in traumatic SCI, but is still less than in males, with a female to male ratio of 1:1.6.6 The typical age of people with SCDys is higher than in SCI, with the typical median age reported in the range of 60 to 65 years.2–9
One study estimated that half of the causes of SCDys are age-related conditions.10 With population aging, it is projected that in most regions of the world the proportion of the population aged over 65 years will double between 2000 and 2050.11 As a result, it is anticipated that the incidence of SCDys will increase dramatically,6 and SCI rehabilitation centers will have to deal increasingly with the rehabilitation of persons with SCDys.
Most aspects of rehabilitation for traumatic SCI and SCDys are the same, but because of age, gender, and etiological differences, people with SCDys have some unique rehabilitation issues that are important to consider. Despite the forecast increase in SCDys, there is relatively little practical information in the literature regarding the rehabilitation management of these patients. Given this situation, we considered it inappropriate to prepare a typical formal systematic review. The aim of this article is to present a narrative review and give an overview of important clinical rehabilitation principles unique to people with SCDys, with a focus on both general differences and aspects that are unique to certain etiologies.
Methods
Literature search
We conducted an electronic search of the literature (January 2017) using the MEDLINE and Embase databases (1990–2016) for publications regarding SCDys, including the most common reported causes of these conditions (degenerative, benign or malignant tumor, vascular problems resulting in infarction or hemorrhage, infections, or inflammation). The terms used in the literature search were exactly the same as those used in a previously published gold standard comprehensive search strategy for SCDys.12 To identify publications on important clinical rehabilitation principles unique to people with SCDys, the publications identified by the above search were combined with the search terms “Recommendation*” OR “Patient Care Management”. The focus of the literature search was on identifying publications that present suggestions regarding the clinical management during rehabilitation of SCDys, especially concerning differences when compared to patients with SCI. Only publications in English were included. The search was restricted to the years 1990 and onwards, because we believed that prior to this date there would be very few publications of relevance. We screened publications identified by the above process by reviewing the title and abstract, and we reviewed the full text of those potentially of relevance. The processes involved are summarized in Figure 1. We also screened the reference sections of included publications for potentially relevant additional publications.
Figure 1.
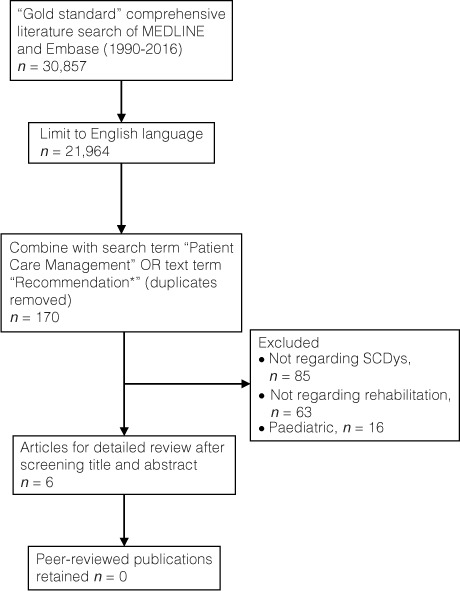
Flow chart of the search methodology and overview of results regarding rehabilitation management issues unique for people with spinal cord dysfunction.
In addition to the electronic search of the literature, we explored our personal libraries for additional potentially relevant articles. Our diverse backgrounds, as rehabilitation medicine physicians (physiatrists) from 4 different continents and developing and developed countries, meant that this strategy would increase the number of useful publications identified.
Data extraction: Presentation of findings
The lead author noted key clinical management themes identified in the literature. Subsequently, the co-authors added important additional points based on their clinical experiences and personal libraries that were not previously covered in publications. All authors had input into the wording of the comments and recommendations made that were based on opinion. Our consensus opinions are clearly identified as such throughout. It is important to note that we have considerable experience in managing people with SCDys, with a median of 20 years (range, 11–31 years) experience working with these patients. As such, we represent a panel of experts, and we made comments and recommendations that we believe are important and where there is an absence of published evidence. The findings are discussed in a narrative review below.
Results
Literature search
The electronic search of MEDLINE and Embase identified 6 potentially relevant publications.13–18 After reviewing these articles in detail, we found that none met the inclusion criteria (Figure 1). As a result, the publications included in this review were all identified from our libraries.
Classification issues unique to people with SCDys
Classification of etiology
The International Spinal Cord Injury Data Sets for Non-traumatic Spinal Cord Injury was published in 2014 and includes a basic and extended data set option.1 These include a classification system for the many heterogeneous causes of SCDys based on a 2-axis approach. The first axis uses a 2-tier (congenital-genetic and acquired), 5-level hierarchy that provides for increasing detail regarding the etiology. The conditions in the second level of the acquired tier are vertebral column degenerative disorders, metabolic disorders, vascular disorders, inflammatory and autoimmune diseases, radiation related, toxic, neoplastic, infection, and other miscellaneous causes (Table 1). Increasing specificity regarding the etiology of SCDys is given with each additional level, for example, neoplastic (level 2), benign (level 3), intramedullary (level 4), and ependymoma (level 5). The basic level of the data set consists of the etiology classified using axis one to the second level, as listed above. The levels in the classification can be collapsed down where the patient population is very small, for example, congenital and genetic, and expanded to more levels for more frequent causes. For example, infection (level 2) has the following in level 3: viral, bacterial, spirochaetal, fungal, and parasitic.
Table 1.
Brief outline of classification on spinal cord dysfunction

Axis 2 uses the International Statistical Classification of Diseases to code the initiating diseases or process that caused the SCDys. Additional items in the dataset include the timeframe of the onset of SCDys symptoms (acute [≤1 day], subacute [≤1 week], prolonged [>1 week to month], and lengthy [>1 month]) and the presence of any iatrogenic component in the etiology. The non-traumatic datasets facilitate an improvement in comparative research involving people with SCDys, especially epidemiological and prevention studies.
We recommend that the International Spinal Cord Injury Data Sets for Non-traumatic Spinal Cord Injury1 be used when classifying the etiology of SCDys in clinical practice and research.
Neurological classification
The International Standards for Neurological Classification of Spinal Cord Injury (ISNCSCI) were originally developed for traumatic SCI.19 Numerous authors have used them in people with SCDys,20–24 even though they have not been formally validated in these patients. It is believed, however, that for now, there is no reason why the ISNCSCI should not be used for describing the neurological impairment in people with SCDys.
General rehabilitation issues unique to people with SCDys
Predicting neurological improvement, rehabilitation outcomes, and survival
Predicting neurological improvement, rehabilitation outcomes, and survival following SCDys is extremely challenging, and the literature on these topics is scarce.3,4 People with SCDys tend to be older than those with traumatic SCI.2,3,5,6 As a result, even though there are no published studies to support our assertion, we believe that they have an increased occurrence of comorbid health conditions, such as obesity, diabetes, cardiovascular and respiratory diseases, or arthritis and other musculoskeletal conditions, and that the presence of these comorbid conditions can have an adverse influence on neurological improvement and rehabilitation outcomes. Level and grade of spinal cord damage influence neurological improvement and rehabilitation outcomes. SCDys typically results in an incomplete grade of spinal cord damage.9,22 It is very difficult, especially in the early period, to know which patients with SCDys will change in their level or completeness of lesion. Another important issue that limits interpretation of research to date is that many studies include SCDys patients with different etiologies and different prognoses.25 In particular, some conditions that cause SCDys are progressive, such as inoperable benign tumors, genetic conditions (eg, hereditary spastic paraplegia), inflammatory diseases (eg, multiple sclerosis and neuromyelitis optica), and infections (eg, human immunodeficiency virus).1 It is much more difficult to predict the neurological and rehabilitation outcomes in these patients with progressive or potentially progressive SCDys than in patients with non-progressive causes of SCDys. Issues unique to people with SCDys due to tumor are discussed in detail in a section below, and many of these also apply to other progressive causes of SCDys. As a result of the above factors, we believe that predicting the neurological and functional recovery in people with SCDys is more difficult than in SCI.
In addition to the limitations previously outlined that influence predicting the neurological and functional outcomes, the comparison of samples of rehabilitation patients with SCI and SCDys is made additionally challenging because of referral and selection bias and the fact that many studies come from single centers, typically with small sample sizes. The findings across studies have shown a high degree of variability.
It has been reported that people with SCDys have major neurological improvement in the American Spinal Cord Injury Association Impairment Scale (AIS) grade.2,26 The authors, however, did not correct for the confounding effects of age, sex, impairment at admission, and the level of the lesion. In a study comparing SCI with SCDys, the same degree of neurological improvement was seen, with approximately 25% of AIS grade A, B, and C patients achieving an improvement of at least 1 AIS grade between admission and discharge.27 A study of people with SCDys due to spinal cord abscess compared to a sample with SCI reported a greater AIS improvement in the abscess group.28
A number of studies have compared rehabilitation outcomes in different SCDys etiologies9,27,29–36 with samples of SCI. In some studies, SCI patients achieved greater functional improvement than SCDys patients, with the exception of patients with vascular-related SCI.32,33 One study found similar degree of improvements in SCDys compared with SCI, but the SCDys cohort had higher admission and discharge functioning than SCI9; other studies report comparable outcomes at discharge for the traumatic and non-traumatic populations.27,31,34,35
In some studies, it seems that traumatic and non-traumatic patients have the same functional status at admission to rehabilitation.8,37 However, others authors report lower functional status for traumatic patients.9,27,36,38 It has been suggested that the low functional status of patients with traumatic SCI could be due to non-neurological trauma-related factors, such as major surgery sequelae, orthotics, and associated lesions that may affect the level of independence.27 In some studies, patients with SCDys achieve lower functional gains during a shorter length of stay compared to traumatic patients.8 However, other authors report that traumatic SCI and SCDys patients at discharge have comparable levels of daily life independence, walking ability, and bladder control.27
There are very limited data on survival after SCDys,9,39 and the generalizability is limited by the samples coming from a single center. A recent study found that SCDys from any etiology is independently associated with an increased mortality risk.9 The impact on life expectancy, however, varies according to the cause for SCDys. As would be expected, individuals with SCDys from metastatic cancer had the most limited survival after SCDys (1.6 ± 0.7 years), however other types of tumors did well. The survival of individuals with intramedullary tumors such as ependymomas did not differ from traumatic SCI. Following metastatic cancer, vascular SCDys due to ischemia had the second largest reduction in survival (mean survival, 5.5 ± 1.6 years). Age, male gender, SCDys etiology, and discharge functional status all influence survival after discharge from rehabilitation. Discharge FIM scores under 100 were associated with 10-year survival rates under 50%. Neither injury severity nor injury level is independently associated with survival after SCDys.9
Overall, persons with SCDys benefit from inpatient rehabilitation. As noted previously, discharge functional status is an important predictor of survival.9 Therefore, inpatient rehabilitation is as important for SCDys as it is for SCI. Similar to the wide range of outcomes following SCI, there is a wide range of outcomes following SCDys. Etiology, however, appears to be a critical factor in predicting outcomes following SCDys. Length of stay, outcomes, and survival all vary by SCDys etiology. Additional research is needed to identify optimal treatment pathways and to more thoroughly understand prognosis.
Admission to spinal rehabilitation units
There is evidence from numerous studies that people with SCDys have improved outcomes when admitted to a specialist spinal rehabilitation unit (SRU)40–42 compared with those admitted to a general rehabilitation unit because of the improved access to critical services and spinal cord medicine rehabilitation expertise.40,43 Despite this, many spinal SRUs preferentially admit people with SCI over those with SCDys.40,44,45 This bias appears to be directed against those people with underlying malignancy as the cause of SCDys.46–48
Therefore, if the needs of people with SCDys are the same as people with SCI, a personalized rehabilitation program is similarly essential. Two particularly important aspects of SCDys rehabilitation are (1) the uncertain, variable, and, at times, gradually deteriorating, neurological prognosis and (2) the uncertain, variable, and, at times, relatively short, life expectancy. These uncertainties pose particular challenges in relation to resource allocation decisions. For example, is an expensive power wheelchair indicated if life expectancy is 6 months? 12 months? A comprehensive examination of issues surrounding ethics and resource allocation is beyond the scope of this article, but these considerations are important in SCDys rehabilitation.
As with SCI, comorbid secondary health problems such as age- and frailty-related considerations; environmental factors, particularly the home access and internal layout; and personal factors, especially the availability of a caregiver and financial resources, all impact the rehabilitation plan. SCDys patients with limited life expectancy are managed with shorter rehabilitation hospital admissions that focus on basic rehabilitation goals and adaptation of temporary devices. Where possible, it is recommended that, before admission to a rehabilitation service, there is discussion between the patients, their families, and a senior rehabilitation physician (physiatrist) from the team regarding anticipated rehabilitation goals, estimated length of hospital stay, likely costs of equipment, possible home modifications, and an estimate of ongoing care. Further discussion on this issue for people with malignancy is provided below in the section, “Specific aspects relating to tumour as a cause of non-traumatic spinal cord dysfunction.”
We strongly believe that there is no justification for any selection bias of SRUs against people with SCDys. Although evidence shows that persons with SCDys have better outcomes from inpatient rehabilitation in a specialized SRU,42 not all patients with a potential for functional improvement receive adequate rehabilitation.45 This might be caused by a lack of information on rehabilitation potential by, for example, physicians and health insurance companies, as well a lack of available specialist rehabilitation programs for persons with SCDys. If there are challenges in meeting the demand for services to provide access to specialist SRU, then these should be addressed by a combination of lobbying of health bureaucrats and reconfiguring health systems models of care. For example, specialist in-reach teams provided in acute hospitals49 and a hub-and-spoke model of service provision, with support from specialist SRUs to non-specialist rehabilitation units, are 2 models of health service delivery that have potential for providing increased access to specialist spinal rehabilitation services.
Participation in rehabilitation
Some people with SCDys require ongoing treatments during rehabilitation for health conditions associated with the cause of their SCDys. For example, patients may require plasma exchange, intravenous immunoglobulin, or immunosuppressant medications (eg, rituximab for inflammatory conditions, such as neuromyelitis optica). With optimal planning for these treatments, it is possible to deliver them and rehabilitation services; these should not be a reason to defer transfer of a patient from acute wards to an SRU. Individuals with tumors may need radiation therapy or chemotherapy, and the scheduling of these treatments so as to minimize the impact on rehabilitation care is essential. For example, therapy might be better scheduled in the earlier part of the day and medical treatments delivered later in the day.
Because some rehabilitation units will not have experience with all specialist medical treatments, staff training may be necessary to ensure patient safety; not every treatment will be possible in every SRU. In our experience, however, the patient's rehabilitation needs and many types of medical management can be accommodated within the SRU.
Secondary health conditions in non-traumatic SCDys
Secondary health conditions after SCDys, such as pressure injuries, neuropathic pain, and spasticity, are prevalent, but they appear to be less common than in SCI during inpatient rehabilitation.10,50,51 In a community sample of people with SCI and SCDys, it was reported that there was no major difference in the occurrence or severity of most secondary health conditions in the 2 groups.52 However, another study from Canada reported that there was a lower prevalence of secondary health conditions in the SCDys cohort,53 but this may be partially accounted for by those with SCDys having more incomplete spinal cord damage. Based on our clinical experience and expertise, we believe that the treatment of these conditions in principle does not differ between those with SCDys or SCI, after adjusting for age.
Sexuality issues
Although it has been proposed that people with SCDys have inferior sexual adjustment compared to those with traumatic SCI because they may have more medical complications that can potentially interfere with sexual rehabilitation programs,54 this assertion is not supported by evidence from a recent study. This study, using the self-report version of the International SCI Data Sets for sexual function for males and females, found that, compared to those with traumatic SCI, those with SCDys were more likely to have sexual issues prior to their SCDys, retain the ability to have orgasms, and be less likely to be able to ejaculate or menstruate.55 Otherwise, there was no difference between those with traumatic SCI and non-traumatic SCDys regarding sexual problems or issues, the ability to have psychogenic erections or genital arousal, and the ability to have reflex erections or genital arousal. These differences could possibly be explained by the older age and higher frequency of incomplete spinal cord damage in people with SCDys. Another difference regarding sexuality in people with SCDys is that they have reported to be less likely to receive education regarding the consequences of SCDys for sexuality during SRU admission compared to those with traumatic SCI.56 Overall, respondents with either etiology reported a low rate of having received sexuality education and a very poor satisfaction with the education provided. There was a belief among those with SCDys that there was a bias of staff against offering sexuality education to females, those who did not have a partner, and those who were older.
Specific aspects relating to degenerative causes of non-traumatic SCDys
Degenerative conditions of the spine are recognized as the most common cause of SCDys globally.3,22 When patients have a spinal fusion as part of the surgical management of their degenerative spinal condition, it is important for clinicians to remember that there can be late complications, including symptomatic adjacent spinal segment degeneration. This occurs in 5% to 18% of patients during a follow-up of 4 to 14 years.57 As with all patients with SCDys or SCI, lifelong follow-up in a specialist spinal rehabilitation review clinic is recommended as best practice.58 In these reviews, it is important to question patients with previous spinal fusion about any symptoms regarding loss of function or pain that could indicate the hallmark of adjacent spinal segment degeneration.
Specific aspects relating to tumor as a cause of non-traumatic SCDys
Benign and malignant tumors are among the most common causes of SCDys, responsible for between 15% and 30% of patients in SRUs that admit patients with any etiology of spinal cord damage.1,9,22 Having the dual diagnosis of a tumor causing SCDys presents enormous challenges for the patient, their family, and the rehabilitation team. Practical recommendations for rehabilitation teams concerning the management of people who have SCDys due to tumor have been reported previously.48,59–61 We highlight key aspects of these recommendations.
A framework has been previously proposed for guiding the rehabilitation of people with SCDys due to tumors, which forms an acronym, NOM-PRS48,59; this was based on earlier work in this area.61 The acronym stands for neurological, oncologic, medical, pain, rehabilitation, and support status of the patient. A detailed expansion of the NOMPRS framework and practical considerations for rehabilitation teams managing people with SCDys due to tumor are given in Table 2, which is adapted from previously published versions.48,59 The cornerstones of NOMPRS are as follows:
N: Neurological status. The more complete spinal cord damage, the worse the probability of improvement.22 Because SCDys lesions can be progressive, it is important to anticipate functional status changes.
O: Oncologic status determines the survival prognosis, which varies for different tumor types. Within the same tumor groups, there is also a wide variation in prognosis.
M:Medical comorbidities may have an additional influence on the ability of patients to participate in rehabilitation and require optimal management.
P: Pain is common and multifactorial. Comprehensive assessment is necessary to diagnose the cause(s) and formulate management strategies.
R: Rehabilitation-specific team and organization issues include a target length of stay for inpatient rehabilitation, based on previous studies and opinion of experts, of 4 to 6 weeks for those with a poor prognosis (eg, <6 months).46,48,62–64
S: Social supports have a critical influence on discharge planning, particularly the person's ability to return to the community and remain at home as long as possible, if that is what he or she desires. Supports can be either provided by the family or paid for by the patient or family.
Table 2.
NOMPRS framework and practical considerations for managing people with spinal cord dysfunction due to tumorsa(CONT.) a

Table 2.
NOMPRS framework and practical considerations for managing people with spinal cord dysfunction due to tumorsa a

Specific aspects relating to infections as cause of non-traumatic SCDys
Patients with infections resulting in SCDys are reported to account for between 2.5% and 13% of patients admitted into SRUs in developed countries2,36 and 25% to 44% in developing countries.51,65,66 The most common pathogens that cause infections resulting in SCDys are bacteria (especially Staphylococci and Streptococcus species in developed countries). Mycobacterium tuberculosis (especially in developing countries) and viruses are also well documented, while fungal and parasitic aetiologies are rare.36,67–70
There are challenges to the early recognition of symptoms relating to the onset of SCDys in patients with an infectious cause, especially those due to bacteria and M. tuberculosis.71,72 Pain and weakness are the most common presenting symptoms, even more common than fever.36 The insidious onset of clinical symptoms and the non-specificity of examination findings early in the onset of infections resulting in SCDys means that there is often a delay in diagnosis and management of these infections that increases their severity.71,72
It is possible that cases of infections causing SCDys, including bacteria such as M. tuberculosis,73 could be prevented by appropriate education programs targeting health care providers and focusing on strategies to raise awareness of key clinical features that suggest the possibility of an infectious cause for a SCDys.74 National and global programs are needed to provide the education and resources necessary to reduce the incidence of infections causing SCDys. M. tuberculosis control programs in developing countries do not specifically address SCDys, resulting in increased morbidity and long-term disability.
Reported outcomes following SCDys due to infections are variable. Some authors have reported favorable neurological and function recovery to a better degree than with other causes of SCDys.22,74 It has been reported that people with an infectious cause of SCDys have significant improvement in theirAIS grade,22,28,74 bladder and bowel continence, and mobility.74,75 One study found that continence and especially mobility can continue to improve up to a year after rehabilitation discharge.74 In contrast, a different study reported that infection-related SCDys patients had complete injuries more commonly, had lower functional status, and longer length of stay than patients with other causes of SCDys and with overall rehabilitation outcomes very similar to SCI patients.36
Rehabilitation physician as a diagnostic clinician
Sometimes there are patients with SCDys who come under the care of a rehabilitation physician (physiatrist), either admitted into an SRU or seen in a clinic, with an unresolved diagnosis of their SCDys or with an incorrect diagnosis. A rehabilitation physician can sometimes identify a differential diagnoses not previously considered and commence investigations while starting functional rehabilitation. In some instances, the rehabilitation physician can make the correct diagnosis and start the appropriate condition-specific management plan or identify a medical reason for lack of improvement or deterioration in neurology or functioning. A number of examples of these situations have been discussed previously,76 and others include spinal cord damage being mistakenly diagnosed as due to inflammation instead of spondylosis77; and multilevel bacterial infections of the spine that are not recognized, especially tuberculosis, with only one level being identified in acute hospital work-up78 until lack of improvement/deterioration in rehabilitation or medical instability triggers a search for the reason.
Based on these situations, and our clinical experiences, we feel that it is important to note that rehabilitation physicians working with people who have SCDys have a vital role as diagnostic clinicians to identify the correct diagnosis where there is a possibility of a missed or incorrect diagnosis.
Discussion
A number of important clinical rehabilitation issues unique to people with SCDys have been highlighted in this article. Classification issues were identified regarding the use of the International Spinal Cord Injury Data Sets for Non-traumatic Spinal Cord Injury to classify the etiology of SCDys and the lack of formal validity testing of the ISNCSCI in people with SCDys. General rehabilitation issues involve the prediction of survival, improvement, and rehabilitation outcomes; decisions about admission into spinal rehabilitation units; participation in rehabilitation; and secondary health conditions. There were numerous important rehabilitation principles unique to persons with SCDys due to degenerative conditions, tumors, and infections that were identified. Finally, we identified a role for the rehabilitation physician as a diagnostic clinician.
As far as we are aware, this is the first article to synthesize the literature regarding issues unique to the rehabilitation management of people with SCDys and combine these with recommendations from experts. We have provided a framework for guiding clinicians who have less experience working with people who have SCDys that we hope will be useful for optimizing the rehabilitation outcomes. We decided against preparing this article as a formal systematic review, because we did not believe that there would be a sufficient number of publications of adequate scientific rigor to make such an approach of practical value to clinicians.
There are a number of limitations that need to be acknowledged. The inability of the electronic literature search to find any relevant articles is possibly a reflection of the likelihood that the recommendations made in journal articles only appear in the discussion section and are not likely to be included in the abstract or considered in the listing of key terms for indexing in electronic databases. It may also be indicative of the different terms used to describe SCDys in the literature.12 As a result, the literature search may have missed some important publications. To address this, we also searched our personal libraries for relevant publications. The inclusion of publications from our libraries does restrict the ability of researchers to replicate our method. However, given the results of the formal literature search, we believe that this approach was necessary and appropriate.
In conclusion, there are numerous special considerations regarding the rehabilitation of people with SCDy that are different from the rehabilitation of people with traumatic SCI. However, with adequate planning of the rehabilitation program and special attention to the clinical conditions of patients with SCDys, functional improvement is typically significant. People with SCDys should have the same access to specialist spinal rehabilitation as that available to people with traumatic SCI.
REFERENCES
- 1. New PW, Marshall R.. International Spinal Cord Injury Data Sets for Non-Traumatic Spinal Cord Injury. Spinal Cord. 2014; 52: 123– 132. [DOI] [PubMed] [Google Scholar]
- 2. New P, Reeves R, Smith É, . et al. International retrospective comparison of inpatient rehabilitation for patients with spinal cord dysfunction epidemiology and clinical outcomes. Arch Phys Med Rehabil. 2015; 96: 1080– 1087. [DOI] [PubMed] [Google Scholar]
- 3. New PW, Cripps RA, Lee BB.. A global map for non-traumatic spinal cord injury epidemiology: Towards a living data repository. Spinal Cord. 2014; 52: 97– 109. [DOI] [PubMed] [Google Scholar]
- 4. Bickenbach J, Boldt I, Brinkhof M, . et al. A global picture of spinal cord injury. : Bickenbach J, Officer A, Shakespeare T, von Groote P, . International Perspectives on Spinal Cord Injury. Geneva: World Health Organization; 2013: 11– 42. [Google Scholar]
- 5. Noonan VK, Fingas M, Farry A, . et al. The incidence and prevalence of SCI in Canada: A national perspective. Neuroepidemiology. 2012; 38: 219– 226. [DOI] [PubMed] [Google Scholar]
- 6. New PW, Sundararajan V.. Incidence of non-traumatic spinal cord injury in Victoria, Australia: A population-based study and literature review. Spinal Cord. 2008; 46: 406– 411. [DOI] [PubMed] [Google Scholar]
- 7. McKinley WO, Seel RT, Hardman JT.. Nontraumatic spinal cord injury: Incidence, epidemiology, and functional outcome. Arch Phys Med Rehabil. 1999; 80: 619– 623. [DOI] [PubMed] [Google Scholar]
- 8. McKinley WO, Seel RT, Gadi RK, Tewksbury MA.. Nontraumatic vs. traumatic spinal cord injury. A rehabilitation outcome comparison. Am J Phys Med Rehabil. 2001; 80: 693– 699. [DOI] [PubMed] [Google Scholar]
- 9. Hatch BB, Wood-Wentz CM, Therneau TM, Walker MG, Payne JM, Reeves RK.. Factors predictive of survival and estimated years of life lost in the decade following nontraumatic and traumatic spinal cord injury. Spinal Cord. 2017; 55: 540– 544. [DOI] [PubMed] [Google Scholar]
- 10. New PW, Rawicki HB, Bailey MJ.. Nontraumatic spinal cord injury: Demographic characteristics and complications. Arch Phys Med Rehabil. 2002; 83: 996– 1001. [DOI] [PubMed] [Google Scholar]
- 11. United Nations. . Report of the Second World Assembly on Ageing; April 8–12, 2002; Madrid. [Google Scholar]
- 12. New PW, Delafosse V.. What to call spinal cord damage not due to trauma? Implications for literature searching. J Spinal Cord Med. 2012; 35: 89– 95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. McLinton A, Hutchison C.. Malignant spinal cord compression: A retrospective audit of clinical practice at a UK regional cancer centre. Br J Cancer. 2006; 94: 486– 491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kiekens C, Van Rie KMC, Peers KHE, Lysens RJ.. Cost of rehabilitation care in traumatic and nontraumatic spinal cord injury in a European context. Top Spinal Cord Inj Rehabil. 2011; 16: 43– 52. [Google Scholar]
- 15. Rouleau P, Guertin PA.. Traumatic and nontraumatic spinal-cord-injured patients in Quebec, Canada. Part 3: Pharmacological characteristics. Spinal Cord. 2011; 49: 186– 195. [DOI] [PubMed] [Google Scholar]
- 16. Hagen EM, Rekand T.. Management of bladder dysfunction and satisfaction of life after spinal cord injury in Norway. J Spinal Cord Med. 2014; 37: 310– 316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. New PW, Dillon L.. Neurogenic bladder and urodynamic outcomes in patients with spinal cord myelopathy. Top Spinal Cord Inj Rehabil. 2015; 21: 250– 256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Hinrichs T, Prodinger B, Brinkhof MW, Gemperli A; SwiSCI study group. . Subgroups in epidemiological studies on spinal cord injury: Evaluation of international recommendations in the Swiss Spinal Cord Injury Cohort Study. J Rehabil Med. 2016; 48: 141– 148. [DOI] [PubMed] [Google Scholar]
- 19. Kirshblum SC, Burns SB, Biering-Sorensen F, . et al. International standards for neurological classification of spinal cord injury (revised 2011). J Spinal Cord Med. 2011; 34: 535– 546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Shin JC, Kim DH, Yu SJ, Yang HE, Yoon SY.. Epidemiologic change of patients with spinal cord injury. Ann Rehabil Med. 2013; 37 1: 50– 56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Jensen EK, Biering-Sørensen F.. Medication before and after a spinal cord lesion. Spinal Cord. 2014; 52 5: 358– 363. [DOI] [PubMed] [Google Scholar]
- 22. New PW, Reeves RK, Smith É, . et al. International retrospective comparison of inpatient rehabilitation for patients with spinal cord dysfunction: Differences according to etiology. Arch Phys Med Rehabil. 2016; 97: 380– 385. [DOI] [PubMed] [Google Scholar]
- 23. Andresen SR, Bing J, Hansen RM, . et al. Ultramicronized palmitoylethanolamide in spinal cord injury neuropathic pain: A randomized, double-blind, placebo-controlled trial. Pain. 2016; 157 9: 2097– 2103. [DOI] [PubMed] [Google Scholar]
- 24. Baunsgaard CB, Nissen UV, Christensen KB, Biering-Sørensen F.. Modified Ashworth scale and spasm frequency score in spinal cord injury: Reliability and correlation. Spinal Cord. 2016; 54 9: 702– 708. [DOI] [PubMed] [Google Scholar]
- 25. Ditunno JF. Point of view. Spine. 2004; 29: 2283. [Google Scholar]
- 26. Catz A, Goldin D, Fishel B, Ronen J, Bluvshtein V, Gelernter I.. Recovery of neurologic function following nontraumatic spinal cord lesions in Israel. Spine. 2004; 29 20: 2278– 2282. [DOI] [PubMed] [Google Scholar]
- 27. Scivoletto G, Farchi S, Laurenza L, Molinari M.. Traumatic and non-traumatic spinal cord lesions: An Italian comparison of neurological and functional outcomes. Spinal Cord. 2011; 49: 391– 396. [DOI] [PubMed] [Google Scholar]
- 28. Koo DW, Townson AF, Dvorak MF, Fisher CG.. Spinal epidural abscess: A 5-year case-controlled review of neurologic outcomes after rehabilitation. Arch Phys Med Rehabil. 2009; 90: 512– 516. [DOI] [PubMed] [Google Scholar]
- 29. McKinley WO, Huang ME, Tewksbury MA.. Neoplastic vs. traumatic spinal cord injury: An inpatient rehabilitation comparison. Am J Phys Med Rehabil. 2000; 79: 138– 144. [DOI] [PubMed] [Google Scholar]
- 30. Mckinley WO, Tewksbury MA, Mujteba NM.. Spinal stenosis vs traumatic spinal cord injury: A rehabilitation outcome comparison. J Spinal Cord Med. 2002; 25: 28– 32. [DOI] [PubMed] [Google Scholar]
- 31. Scivoletto G, Cosentino E, Mammone A, Molinari M.. Inflammatory myelopathies and traumatic spinal cord lesions: Comparison of functional and neurological outcome. Phys Ther. 2008; 88: 471– 484. [DOI] [PubMed] [Google Scholar]
- 32. McKinley W, Sinha A, Ketchum J, Deng X.. Comparison of rehabilitation outcomes following vascular-related and traumatic spinal cord injury. J Spinal Cord Med. 2011; 34 4: 410– 415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Pouw MH, Hosman AJ, van Kampen A, Hirschfeld S, Thietje R, van de Meent H.. Is the outcome in acute spinal cord ischaemia different from that in traumatic spinal cord injury? A cross-sectional analysis of the neurological and functional outcome in a cohort of 93 paraplegics. Spinal Cord. 2011; 49: 307– 312. [DOI] [PubMed] [Google Scholar]
- 34. Scivoletto G, Lapenna L, Di Donna V, . et al. Neoplastic myelopathies and traumatic spinal cord lesions: An Italian comparison of functional and neurological outcomes. Spinal Cord. 2011; 49: 799– 805. [DOI] [PubMed] [Google Scholar]
- 35. Scivoletto G, Laurenza L, Mammone A, Foti C, Molinari M.. Recovery following ischemic myelopathhies and traumatic spinal cord lesions. Spinal Cord. 2011; 49: 897– 902. [DOI] [PubMed] [Google Scholar]
- 36. Brubaker ML, Luetmer MT, Reeves RK.. Clinical features and inpatient rehabilitation outcomes of infection-related myelopathy. Spinal Cord. 2017; 55: 264– 268. [DOI] [PubMed] [Google Scholar]
- 37. Gupta A, Taly AB, Srivastava A, Vishal S, Murali T.. Traumatic vs non-traumatic spinal cord lesions: Comparison of neurological and functional outcomes after in-patient rehabilitation. Spinal Cord. 2008; 46: 482– 487. [DOI] [PubMed] [Google Scholar]
- 38. Ones K, Yilmaz E, Beydogan A, Gultekin O, Caglar N.. Comparison of functional results in non-traumatic and traumatic spinal cord injury. Disabil Rehabil. 2007; 29: 1185– 1191. [DOI] [PubMed] [Google Scholar]
- 39. Ronen J, Goldin D, Bluvshtein V, Fishel B, Gelernter I, Catz A.. Survival after nontraumatic spinal cord lesions in Israel. Arch Phys Med Rehabil. 2004; 85 9: 1499– 502. [DOI] [PubMed] [Google Scholar]
- 40. Smith M. Efficacy of specialist versus non-specialist management of spinal cord injury within the UK. Spinal Cord. 2002; 40: 11– 16. [DOI] [PubMed] [Google Scholar]
- 41. Eriks I, Angenot E, Lankhorst G.. Epidural metastatic spinal cord compression: Functional outcome and survival after inpatient rehabilitation. Spinal Cord. 2004; 42: 235– 239. [DOI] [PubMed] [Google Scholar]
- 42. New PW, Simmonds F, Stevermuer T.. Comparison of patients managed in specialised spinal rehabilitation units with those managed in non-specialised rehabilitation units. Spinal Cord. 2011; 49: 909– 916. [DOI] [PubMed] [Google Scholar]
- 43. New PW. Non-traumatic spinal cord injury: What is the ideal setting for rehabilitation? Aust Health Rev. 2006; 30: 353– 361. [DOI] [PubMed] [Google Scholar]
- 44. Celani MG, Spizzichino L, Ricci S, Zampolini M, Franceschini M; for the Retrospective Study Group on SCI. . Spinal cord injury in Italy: A multicentre retrospective study. Arch Phys Med Rehabil. 2001; 82: 589– 596. [DOI] [PubMed] [Google Scholar]
- 45. New PW, Simmonds F, Stevermuer T.. A population-based study comparing traumatic spinal cord injury and non-traumatic spinal cord injury using a national rehabilitation database. Spinal Cord. 2011; 49. [DOI] [PubMed] [Google Scholar]
- 46. Parsch D, Mikut R, Abel R.. Postacute management of patients with spinal cord injury due to metastatic tumour disease: Survival and efficacy of rehabilitation. Spinal Cord. 2003; 41: 205– 210. [DOI] [PubMed] [Google Scholar]
- 47. Ruff RL, Ruff SS, Wang X.. Persistent benefits of rehabilitation on pain and life quality for nonambulatory patients with spinal epidural metastasis. J Rehablil Res Dev. 2007; 44: 271– 278. [DOI] [PubMed] [Google Scholar]
- 48. New PW, Marshall R, Stubblefield MD, Scivoletto G.. Rehabilitation of people with spinal cord damage due to tumor: Literature review, international survey and practical recommendations for optimizing their rehabilitation. J Spinal Cord Med. 2017; 40: 213– 221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. New PW. A multidisciplinary consultation team to address the unmet needs of hospitalized spinal cord injury patients. Arch Neurol. 2010; 67: 1074– 1076. [DOI] [PubMed] [Google Scholar]
- 50. McKinley WO, Teskbury M, Godbout CJ.. Comparison of medical complications following nontraumatic and traumatic spinal cord injury. J Spinal Cord Med. 2002; 25: 88– 93. [DOI] [PubMed] [Google Scholar]
- 51. Gupta A, Taly AB, Srivastava A, Murali T.. Non-traumatic spinal cord lesions: Epidemiology, complications, neurological and functional outcome of rehabilitation. Spinal Cord. 2009; 47: 307– 311. [DOI] [PubMed] [Google Scholar]
- 52. New PW. Secondary conditions in a community sample of people with spinal cord damage. J Spinal Cord Med. 2016; 39: 665– 670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Rouleau P, Ayoub E, Guertin PA.. Traumatic and non-traumatic spinal cord-injured patients in Quebec, Canada: 1. Epidemiological, clinical and functional characteristics. Open Epidemiol J. 2011: 133– 139. [Google Scholar]
- 54. Lombardi G, Del Popolo G, Macchiarella A, Mencarini M, Celso M.. Sexual rehabilitation in women with spinal cord injury: A critical review of the literature. Spinal Cord. 2010; 48: 842– 829. [DOI] [PubMed] [Google Scholar]
- 55. New PW, Currie KE.. Development of a comprehensive survey of sexuality issues including a self-report version of the International Spinal Cord Injury sexual function basic datasets. Spinal Cord. 2016; 54: 584– 591. [DOI] [PubMed] [Google Scholar]
- 56. New PW, Seddon M, Redpath C, Currie KE, Warren N.. Recommendations for spinal rehabilitation professionals regarding sexual education needs and preferences of people with spinal cord dysfunction: A mixed methods study. Spinal Cord. 2016; 54: 1203– 1209. [DOI] [PubMed] [Google Scholar]
- 57. Park P, Garton HJ, Gala VC, Hoff JT, McGillicuddy JE.. Adjacent segment disease after lumbar or lumbosacral fusion: Review of the literature. Spine. 2004; 29: 1938– 1944. [DOI] [PubMed] [Google Scholar]
- 58. Hasnan N, Engkasan JP, Ramakrishnan K, . et al. Follow-up after spinal cord injury. : Chhabra HS, . ISCoS Textbook on Comprehensive Management of Spinal Cord Injuries. New Delhi, India: Wolters Kluwer; 2015: 888– 905. [Google Scholar]
- 59. New PW. Understanding the role of rehabilitation medicine in the care of patients with tumor causing spinal cord dysfunction. Curr Phys Med Rehabil Rep. 2017; 5: 40– 45. [Google Scholar]
- 60. Stubblefield MD, O'Dell MW.. Cancer Rehabilitation. Principles and Practice. New York: Demos Medical Publishing; 2009. [Google Scholar]
- 61. Stubblefield MD, Bilsky MH.. Barriers to rehabilitaiton of the neurosurgical spine cancer patient. J Surg Oncol. 2007; 95: 419– 426. [DOI] [PubMed] [Google Scholar]
- 62. McKinley WO, Conti-Wyneken AR, Vokac CW, Cifu DX.. Rehabilitative functional outcome of patients with neoplastic spinal cord compressions. Arch Phys Med Rehabil. 1996; 77: 892– 895. [DOI] [PubMed] [Google Scholar]
- 63. Fattal C, Gault D, Leblond C, . et al. Metastatic paraplegia: Care management characteristics within a rehabilitation center. Spinal Cord. 2009; 47: 115– 121. [DOI] [PubMed] [Google Scholar]
- 64. Tan M, New PW.. Retrospective study of rehabilitation outcomes following spinal cord injury due to tumour. Spinal Cord. 2012; 50: 127– 131. [DOI] [PubMed] [Google Scholar]
- 65. Owolabi LF, Ibrahim A, Samaila AA.. Profile and outcome of non-traumatic paraplegia in Kano, northwestern Nigeria. Ann Afr Med. 2011; 10: 86– 90. [DOI] [PubMed] [Google Scholar]
- 66. Vaishnav B, Suthar N, Modi D.. Acute non-traumatic paraparesis: A comprehensive analysis of aetiology and clinical profile in an Indian subpopulation. Natl J Integr Res Med. 2014; 5: 17– 21. [Google Scholar]
- 67. Darouiche RO. Spinal epidural abscess. N Engl J Med. 2006; 355: 2012– 2020. [DOI] [PubMed] [Google Scholar]
- 68. Govender G. Spinal infections. J Bone Joint Surg [Br]. 2005; 87-B: 1454– 1458. [DOI] [PubMed] [Google Scholar]
- 69. Grewal S, Hocking G, Wildsmith GAW.. Epidural abscesses. Br J Anaesth. 2006; 96: 292– 302. [DOI] [PubMed] [Google Scholar]
- 70. Sendi P, Bregenzer T, Zimmerli W.. Spinal epidural abscess in clinical practice. Q J Med. 2008; 101: 1– 12. [DOI] [PubMed] [Google Scholar]
- 71. Khanna RK, Malik GM, Rock JP, Rosenblum ML.. Spinal epidural abscess: Evaluation of factors influencing outcome. Neurosurg. 1996; 39: 958– 964. [DOI] [PubMed] [Google Scholar]
- 72. Maslen DR, Jones SR, Crislip MA, Bracis R, Dworkin RJ, Flemming JE.. Spinal epidural abscess: Optimizing patient care. Arch Intern Med. 1993; 153: 1713– 1721. [PubMed] [Google Scholar]
- 73. Moon MS. Tuberculosis of the spine: Controversies and a new challenge. Spine. 1997; 22: 1791– 1797. [DOI] [PubMed] [Google Scholar]
- 74. New PW, Astrakhantseva I.. Rehabilitation outcomes following infections causing spinal cord myelopathy. Spinal Cord. 2014; 52: 444– 448. [DOI] [PubMed] [Google Scholar]
- 75. McKinley W, Merrell C, Meade M, Brooke K, DiNicola A.. Rehabilitation outcomes after infection-related spinal cord disease: A retrospective analysis. Am J Phys Med Rehabil. 2008; 87: 275– 280. [DOI] [PubMed] [Google Scholar]
- 76. Ohry A, Brooks ME, Rozin R.. Misdiagnosis of spinal cord injuries--the physiatrist's point of view. Paraplegia. 1980; 18: 15– 20. [DOI] [PubMed] [Google Scholar]
- 77. Flanagan EP, Krecke KN, Marsh RW, Giannini C, Keegan BM, Weinshenker BG.. Specific pattern of gadolinium enhancement in spondylotic myelopathy. Ann Neurol. 2014; 76: 54– 65. [DOI] [PubMed] [Google Scholar]
- 78. Garg RK, Somvanshi DS.. Spinal tuberculosis: A review. J Spinal Cord Med. 2011; 34: 440– 454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Eva G, Paley J, Miller M, Wee B.. Patients' constructions of disability in metastatic spinal cord compression. Palliat Med. 2009; 23: 132– 140. [DOI] [PubMed] [Google Scholar]


