Abstract
Violence is increasingly viewed as a public health issue that may be ameliorated by health‐based interventions. The Healthy Brains and Behavior Study (HBBS) aims to identify environmental and biological risk factors for aggression in late childhood and to reduce aggression through psychological and nutritional treatments. Utilizing a cross‐disciplinary collaborative research approach, the HBBS has both human and animal components. The human component has two stages consisting of risk assessment followed by treatment. The risk assessment is based on 451 community‐residing children aged 11–12 years and their caregivers, during which genetic, brain imaging, neuroendocrine, psychophysiology, environment toxicology, neurocognitive, nutrition, psychological, social and demographic risk variables are collected. Children who met criteria (N = 219) for problematic aggressive behaviors were assigned to one of four treatment groups: cognitive‐behavior therapy (CBT) alone, nutritional supplements alone, both CBT and nutrition, or treatment‐as‐usual. Treatment duration was 12 weeks and all children whether in treatment or not were followed‐up at three, six, and 12 months. The animal component assessed the effects of dietary omega‐3 fatty acids on the development of aggression. This study contributes knowledge on how biological factors interact with social factors in shaping proactive and reactive aggression and assesses the efficacy of treatment approaches to reduce childhood aggression. Copyright © 2013 John Wiley & Sons, Ltd.
Keywords: healthy brain, behavior, violence, Philadelphia, study design, aggression
Introduction
Violence is increasingly viewed as a public health problem that is prefaced by genetic, neurobiological, psychological, and social risk factors which offer numerous and potentially novel opportunities for intervention. Furthermore, in this health context, a new generation of neurobiological research is beginning to cast a fresh perspective on aggression and violence (Hoptman and Antonius, 2011; Krug et al., 2002; Miczek et al., 2007; Siever, 2008; Soyka, 2011; van Goozen et al., 2007). Understanding the neurobiological basis of aggression and violence is critical to informing future attempts to tackle the major problem of aggression and violence in society. As violence has gained focus as a global public health problem (Krug et al., 2002), significant inroads have been made in our knowledge‐base on the psychosocial prediction and treatment of aggression.
Nevertheless, there are important knowledge gaps that preclude further advances. First, there has been a relative absence of an integrative biosocial approach that incorporates recent neurobiological knowledge on adult violence and applies this knowledge to the prediction and treatment of childhood aggression. Second, much less is known on brain imaging, genetic, neurotoxic, neuroendocrinological, and nutritional risk factors for childhood aggression relative to the large accumulation of knowledge acquired from decades of social research. Third, while violence is heterogeneous, biosocial prediction and treatment research has not adequately considered aggression subtypes, such as proactive versus reactive aggression (Raine et al., 2006).
One overarching goal of this study is to conduct one of the most systematic and wide‐ranging integrations of biosocial risk factors for childhood aggression conducted so far in order to delineate factors that increase risk and confer protection for child and adolescent aggression. A second overarching goal is to conduct one of the very few biosocial interventions on childhood aggression and develop relatively novel intervention programs based on recent scientific advances which reduce childhood aggression. A third goal is to examine two related but different manifestations of aggression – proactive and reactive aggression – which likely have different etiologies and will show a differential response to treatment.
The study responded to a request for applications (RFA) from the Pennsylvania Department of Health for collaborative research on violence prevention (Pennsylvania Department of Health, 2007). The RFA specified that the research must be biomedical, clinical, or health services in nature and must place an emphasis on health‐related issues that disproportionately affect vulnerable segments of the population. The research had to both improve the identification of individuals at risk for violence before serious violence occurred, and evaluate the efficacy of interventions. The RFA highlighted the importance of brain imaging, genetics, neuroendocrinology, and environmental toxins in addition to social processes as potentially important risk factors for violence, and a commitment to using a cross‐disciplinary collaborative research approach. Given the limited four‐year scope of the grant, the intervention needed to focus on short‐term or intermediate outcomes for future violence (e.g. aggressive and antisocial behavior). The RFA also specified that “It is expected that such studies should include heterogeneous populations at high risk, such as minorities, urban, low socio‐economic status, rural populations, as well as both males and females” (Pennsylvania Department of Health, 2007, p. v). These specifications played a major role in framing the nature of the study we report here with its significant emphasis on biological risk factors, and in developing a sampling frame to include populations vulnerable to violence, including minorities and other underserved segments of the population (Sampson et al., 2005).
Aims of the study
The specific aims are five‐fold. First, it aims to identify the environmental, social, psychological, and neurobiological factors that increase the risk that a child will become seriously aggressive later in life. Second, it seeks to test the effectiveness of two interventions (cognitive‐behavior therapy [CBT] and nutritional supplements) for the treatment of childhood aggression both alone and in conjunction. Third, it aims to identify factors that protect some children who are predisposed to aggression from developing this outcome. Fourth, it uses an animal model to assess the effectiveness of nutritional interventions in reducing aggression. Fifth, it examines the interaction of environmental and biological factors in giving rise to child aggression, and how these risk factors affect treatment outcome.
Methods
Design
Animal component
The study has both animal and human components. The animal (mouse) component experimentally tests nutritional interventions (omega‐3 fatty acids) on the development of aggression in a stress‐sensitive mouse strain, the BALB/cJ strain. We chose omega‐3 fatty acids as a nutritional treatment because both initial animal and human studies are beginning to raise the possibility that this long‐chain omega‐3 fatty acid supplement could have beneficial effects in reducing levels of aggressive behavior. In animal studies, research has indicated that fatty acid deprivation increases aggression test scores in rats (DeMar et al., 2006). In human studies to date, initial evidence from both correlational (Hibbeln, 2001) and experimental studies in adults (Gesch et al., 2002) and children (Itomura et al., 2005; Stevens et al., 2003) suggest it may help antisocial and aggressive behavior. Therefore, omega‐3 fatty acids as a nutritional supplement was included in both the animal and human components of our study to test the hypothesis that such supplements can reduce aggression in mice and in children.
Human component/sample
Our focus in this paper is on the human component. The human component includes a risk assessment stage (step 1) and a treatment stage (step 2). A graphic presentation of the study design is presented in Figure 1.
Figure 1.
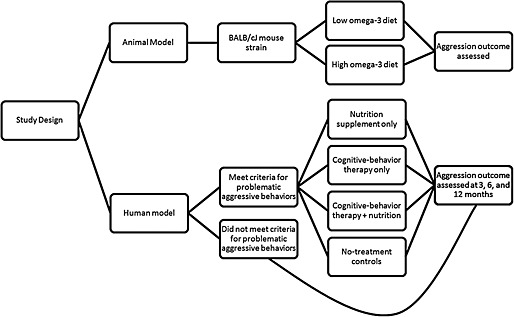
A graphic presentation of the study design.
The sample of male and female 11–12 year‐old children is drawn from all communities within Philadelphia County and in the suburban communities with zip codes that are contiguous to Philadelphia. Participants initially engage in a baseline assessment for risk and protective factors for aggression. Those who meet criteria for problematic aggressive behaviors are then randomly assigned to one of four three‐month treatment programs: nutrition supplementation only, CBT only, CBT + nutrition, and no‐treatment controls. Aggression outcome is assessed for all participants at three, six, and 12 months. For those assigned to treatment the first follow‐up is at the completion of the clinical trial which typically coincides with the three month follow‐up or slightly later if treatment was delayed or a session missed.
Interdisciplinary contributions
The investigators on the Philadelphia Healthy Brains and Behavior Study (HBBS) bring with them formal linkages from a variety of established research and community entities. The project's principal investigators (PIs), co‐PIs, and major external advisors have wide‐reaching interdisciplinary backgrounds and contributions which include six institutions, 13 disciplines (e.g. Criminology, Psychology, Psychiatry, Nursing, Medicine, Neuroscience, and animal research), and expertise including neurophysiology, neurobiology, genetics, injury prevention, environmental health, nutrition, prenatal events, and bone lead assessment.
The goals and activities of this study are integrated through an Executive Committee consisting of the PI and the three co‐PIs. The Executive Committee serves as the intellectual and administrative leadership of the project, ensuring sound scientific and fiscal management and accountability for each subcomponent of the research. Each lead investigator is responsible for monitoring Institutional Review Board (IRB) protocols for their subcomponent of the supported research and sharing documents and concerns with the PI. The Executive Committee is responsible for the overall coordination and integration of the interdisciplinary components of this project. Co‐PIs partner with co‐investigator teams to jointly lead specific components of the project. Communication and planning activities within these teams occur through electronic communication and bi‐weekly meetings.
Recruitment and training of staff
The study staff consists of three teams: the risk‐day assessment team, the intervention team, and the recruitment and retention team with additional staff working on animal and magnetic resonance imaging (MRI) assessment. The risk assessment team members are trained in the various parts of the risk‐day assessment, including diagnostic interviews, psychophysiology, neuroendocrinology, neurocognition, administration of social, psychological, and personality questionnaires, nutrition, organophosphates, and human subjects and HIPAA training. The intervention team consists of a lead interventionist who is a licensed therapist and who received additional training in CBT at the Beck Institute. The lead interventionist supervises four additional part‐time interventionists over the course of the study and is responsible for training all intervention staff to the manualized intervention. The recruitment and retention team is responsible for recruiting the appropriate population into the study (including connecting with community organizations and distributing study advertisements) and for completing follow‐up sessions with study participants.
Eligibility
The inclusion and exclusion criteria are presented in Table 1. There are no exclusions by sex or race/ethnicity. The intent is to enroll all eligible community‐dwelling youth. Children are excluded if they are pregnant or have metallic inserts (exclusions for the MRI), if they have pervasive developmental disorders or psychosis (an exclusion for the CBT arms of the randomized clinical trial [RCT]), or if they have metabolic disorders or seafood allergies (an exclusion for the nutritional arms of the RCT). The findings of the risk‐day assessment are used to determine if children meet criteria for the RCT. These criteria are specified in Table 1.
Table 1.
Inclusion and exclusion criteria for the Philadelphia Healthy Brains and Behavior Study
| Inclusion criteria |
|---|
| 1. Community‐residing 11 and 12 year‐old boys and girls living in Philadelphia County or Pennsylvania suburbs located in contiguous zip codes to Philadelphia. |
| Exclusion criteria |
| 1. Psychotic disorder |
| 2. Mental retardation |
| 3. Claustrophobia |
| 4. Pervasive developmental disorders |
| 5. Conditions that precludes participation (or increase risk) in the clinical trial (Type 1 diabetes mellitus; metabolic diseases, gastrointestinal disorders affecting nutrient absorption, cancer) |
| 6. Currently on medication that may modify lipid metabolism |
| 7. Extensive use of nutritional supplements within the previous three months |
| 8. Seafood allergy |
| 9. Presence or history of orthopedic circumstances and metallic inserts interfering with magnetic resonance scanning |
| 10. Pregnancy |
| Entry criteria for the RCT component of the study |
| 1. Diagnosed with oppositional defiant disorder or having borderline diagnosis |
| 2. Diagnosed with conduct disorder or having borderline diagnosis |
| 3. Scored at least one standard deviation above a normed population mean on either the reactive or proactive components of the Reactive Proactive Aggression Questionnaire (Raine et al., 2006) |
Subject recruitment methods
After considerable discussion among the investigators about the most effective sampling strategy, we decided to seek access to community‐residing children through the Philadelphia School District, with referrals of aggressive children coming from schoolteachers. To this end our team engaged the support of the leaders of the Office of School Climate and Safety for the Philadelphia School System and through them met with the schools with a bullying program in place. Unfortunately, the Central Research Department for the school system did not approve recruitment of children through the school system for several reasons. We made a repeated approach to the school system in which we dropped both the targeting of at‐risk children and also any required time expenditure of school staff, and instead only requested to distribute flyers, but we still failed to obtain support.
In response to these challenges in recruitment, initial delays in institutional approvals, and based on the recommendations of the review panel, we reduced our recruitment goal to 350 parent–child pairs (from the originally planned 500), and made necessary adjustments to the study's analytic scope. We also instituted a number of enhancements to our initial recruitment approach, which has resulted in our recruitment exceeding the revised goal. These changes included: relaxing our age range to include 12‐year‐olds, widening geographic criteria to include suburbs more distant from the university, engaging in targeted, higher‐yield recruitment practices with new institutional partners, and developing a project newsletter which carries the recruitment advertisement to all current and past participants as well as all community partners.
Recruitment strategies include targeted mailings to parents of 11 to 12 year‐old children residing within the geographic sampling area. Parent names were obtained from the primary care research network of a local children's hospital and mailings included study information but with no indication of support from the network. These mailings are supplemented by lists purchased from USA Data (a direct mail company that gathers information from national compilers of consumer data and that could identify households with children in our age group). We collaborated with Nutritional Developmental Services to include recruitment advertisements on school lunch menus. Study flyers are posted in communities (e.g. recreation centers, libraries, local stores), and distributed to 11 and 12 year‐old patients in pediatric dental clinics and in charter schools. Additional sites for recruitment included city agencies such as city health clinics.
Families already in the study were asked to refer other families in exchange for a small financial incentive. Advertisements are placed on Craig's list, in local newspapers, and on public transportation.
Although we take great effort at recruiting broadly from the community, we cannot claim that the sample is representative of the general population.
Recruitment commenced following the approval of this study by the University of Pennsylvania's IRB on November 14, 2008 as well as by the city of Philadelphia's IRB. During this period, we identified, contacted, and began to recruit from geographically defined areas and potential organizations within the city of Philadelphia and the zip codes of the contiguous suburbs. Geographic areas (zip codes) where the 2000 census population of 11 to 12 year olds was 400 or greater were randomly assigned to a sampling list for the initial distribution of flyers and advertisements throughout these communities. Recruitment in the remaining communities followed this phase of saturated field outreach.
Data collection and results
First component: risk assessment
The risk assessment measures involve approximately eight hours of contact time, split between two days. The measure domains and instrument/data sources used and content of the tests administered are detailed in Table 2. As is evident in Table 2, the risk assessment entails the collection of biological, psychological, physical, demographic, and social data about the child from both child and parent. The organization of this day and the location of data collection is planned so as not to overwhelm the child and parent and not to cause undue fatigue that would interfere with the ability to collect reliable data. The parent is provided detailed information about what to expect during the risk‐assessment day and where to meet the study team in a location that is easily accessible by private or public transportation.
Table 2.
Risk assessment measures, instruments, and contents
| Domains | Instrument/data source | Content |
|---|---|---|
| Prenatal | Prenatal Psychosocial Scale a (Liu and Raine, unpublished manuscript) | Measures individual stress, support from partner, and support from others |
| Prenatal Life Events Scalea (Liu and Raine, unpublished manuscript) | • Prenatal psychosocial history | |
| • Measures the number of life events that have happened to the participant or someone close to her since she has been pregnant and her perception of how each event affected her | ||
| Revised Lewis Murray Scale a (Lewis et al., 1989; Liu and Raine, unpublished manuscript) | Rates 15 obstetric complications as absent or definitely present | |
| Family History‐Research Diagnostic Criteria a (Andreasen et al., 1977) | Collects information concerning family history and provides criteria for diagnoses | |
| Psychosocial | Conflict Tactics Scale a, b (Straus et al., 1996) | Assesses Child Abuse/Domestic Violence through measures of Verbal Aggression, and Violence within the family |
| Satisfaction with Life Scale a, b (Diener et al., 1985) | Measures global life satisfaction by making an overall judgment of life | |
| Alabama Parenting Questionnaire a (Frick, 1991) | Measures several dimensions of parenting proven to be important for understanding the causes of conduct problems and delinquency in youth | |
| Demographics Survey a (Frick, 1991) | Collects key demographic information including ethnicity, family income, parental education, parental occupation, living conditions, etc. | |
| Neighborhood Characteristics Questionnaire a (Raine, unpublished manuscript) | Used to study community influences on delinquency in adolescent males and includes measures of informal neighboring, neighborhood attachment, network size and breadth, neighborhood‐level organizational involvement, neighborhood anomie, local personal ties, social disorder, conflict subculture, and illegal economy | |
| Parental Stress Index a (Abidin, 1990) | Identifies potentially dysfunctional parent–child systems, predicts potential for parental behavior problems, and predicts children's future psychosocial adjustment | |
| Emotion Regulation Scale a (Gratz and Roemer, 2004) | Assesses clinically relevant difficulties in emotion regulation | |
| Personality | Antisocial Process Screening Device a (Frick and Hare, 2001) | • Screens for Antisocial Personality Disorder or psychopathy. |
| • Rates the characteristic psychopathic pattern of interpersonal, affective, and behavioral symptoms. | ||
| Child Behavior Checklist a, b (Achenbach, 1991) | • Evaluates maladaptive behavioral and emotional problems | |
| • Internalizing/externalizing behaviors | ||
| Reactive Proactive Questionnaire b (Raine et al., 2006) | Measures reactive/proactive aggression | |
| Cognitive, Affective and Somatic Empathy Scale (CASES) b (Raine, unpublished manuscript) | Measures empathy in three domains: cognitive, affective and motor | |
| Baumeister Self Control Scale b (Tangney et al., 2004) | Assesses people's ability to control their impulses, alter their emotions and thoughts, and to interrupt undesired behavioral tendencies and refrain from acting on them | |
| Aggression Questionnaire b (Buss and Perry, 1992) | Measures aggression on four scales: Physical Aggression, Verbal Aggression, Anger, and Hostility. | |
| Grit Scaleb (Duckworth et al., 2007) | Measures trait‐level perseverance and passion for long‐term goals | |
| Schizotypal Personality Questionnaire b (Raine, 1991) | Screens for scale for schizotypal personality disorder and contains subscales for all nine schizotypal traits. | |
| Zuckerman–Kuhlman Personality Questionnaire b (Zuckerman, 2002) | Assesses the five basic personality traits: Impulsive Sensation Seeking (ImpSS), Neuroticism‐Anxiety (N‐Anx), Aggression‐Hostility (Agg‐ Hos), Activity, and Sociability (Soc). | |
| Adolescent Development Scale b (Morris and Udry, 1980) | Measures adolescents' self‐reported development in male genitalia, testicular size, male pubic hair, female breasts, and female pubic hair. | |
| Conduct and Oppositional Defiant Disorder Questionnaire (CODD Questionnaire) b (Raine, unpublished manuscript) | Dimensional measures of: | |
| • Conduct Disorder | ||
| • Oppositional Defiant Disorder | ||
| Psychophysiology | Electrodermal | • Rest |
| Cardiovascular | • Orienting | |
| EEG | • Fear conditioning | |
| Event‐related potentialsb | • Social Stressor | |
| • P300 oddball | ||
| • Positive and Negative Affect stimuli | ||
| Neuroendocrinology | Saliva samples | • Testosterone |
| • Cortisol | ||
| • Alpha‐amylase | ||
| • DHEA‐S | ||
| Environmental Toxins | Substance Use Surveyb | Substance abuse/usage history |
| X‐ray florescence b | Tibial bone lead | |
| Urine Sample b | Biomarkers for exposure to organophosphates and pesticides | |
| Nutrition Food Recalls | Food/Dietary Recall Questionnaire a, b (Schakel et al., 1988; Schakel, 2001; Schakel et al., 1997) | Collects information about dietary habits and nutritional status |
| Basic Physiology | Physical exam b | Height and Weight |
| Head Injuries | Head Injury Survey a (Jacobs, 1988) | History of head injuries during childhood |
| Blood Analyses | Fasting blood samples b | • Omega‐3 fatty acids |
| • Calcium | ||
| • Cholesterol | ||
| • Glucose | ||
| • Serum ferritin | ||
| • Vitamin D | ||
| • Parathyroid hormone | ||
| Neurocognition | Wechsler Intelligence Scale for Children b (Wechsler, 2004) | Assesses a child's cognitive ability between the ages of six and 16 and can be completed without reading or writing |
| Penn Web‐Based Computerized | Domains Tested: | |
| Neurocognitive Battery (WebCNP) | • Abstraction and Mental Flexibility | |
| b (Gur et al., 2010) | • Sensory‐Motor Dexterity | |
| • Spatial Learning and Memory | ||
| • Verbal Memory | ||
| • Emotion Processing | ||
| • Attention | ||
| Neuroimaging | Anatomical MRI | • Gray, white, and CSF volumes |
| Functional MRI | • Activation to Face Emotion Perception Task and Modified Balloon Analog Risk Task | |
| Diffusion Tensor Imaging b | • White matter tractography | |
| Genetics | Blood b | • MAOA |
| • 5‐HTTLPR | ||
| • BDNF | ||
| • COMT | ||
| • DRD2 |
Completed by parents.
Completed by child.
Although the study coordinator provides a review of the informed consent via telephone with the parent, obtaining a full written informed consent from the caregiver (and assent from the child) is the first activity completed on the risk‐assessment day. Following consent/assent, the child gives a fasting blood sample. The study staff then collects a urine specimen during the day. A nutritional breakfast is provided after the blood sample is obtained after which the child and parent are accompanied by study staff to the risk‐assessment laboratory located about 10 minutes across campus. Most of the remaining data collection takes place in this laboratory. The study team is well‐versed in checking the child for signs of fatigue, provides rest periods for the child, and supplies a mid‐day lunch break. To complete the risk assessment, each child is scheduled to undergo an MRI scan on a different day. Initially, we tried to incorporate the MRI during the risk assessment day, but the scheduling system was independent of our study, creating a challenge in coordinating the test that was located on another part of campus. For this reason, we separated the MRI scan from the rest of the risk assessments, and added additional incentives and travel support with IRB approval. Baseline demographic data are presented in Table 3 and descriptive data on key behavioral measures are presented in Table 4.
Table 3.
Baseline demographic data in Philadelphia Healthy Brains and Behavior Study
| Demographic information (n) | Mean (standard deviation) | [Range] | Frequency (Percent of total) |
|---|---|---|---|
| Age (years) (413) | 11.46 (0.52) | 11, 13 | |
| Gender (413) | |||
| Boys | 216 (52.0%) | ||
| Girls | 197 (47.5%) | ||
| Race (413) | |||
| White/Caucasian | 45 (10.8%) | ||
| African Americans/Blacks | 338 (81.4%) | ||
| Hispanics/Latino | 4 (1.0%) | ||
| Asian/Pacific Islanders | 1 (0.2%) | ||
| Native American | 2 (0.5%) | ||
| Multiracial | 18 (4.3%) | ||
| Other | 5 (1.2%) | ||
| Parental marital status (410) | |||
| Never married | 237 (57.1%) | ||
| Married | 101 (24.3%) | ||
| Divorced | 34 (8.2%) | ||
| Separated | 30 (7.2%) | ||
| Widowed | 8 (1.9%) | ||
| Father lives with the child and mother (410) | |||
| No | 254 (61.2%) | ||
| Yes | 156 (37.6%) | ||
| Family monthly income (392) | 2949.90 (3007.44) | 0, 22000 | |
| Siblings (408) | |||
| 0 | 25 (6.0%) | ||
| 1 | 82 (19.8%) | ||
| 2 | 89 (21.4%) | ||
| 3 | 86 (20.7%) | ||
| > 3 | 126 (30.4%) | ||
| Father's education (years) (338) | 12.76 (2.13) | 4, 22 | |
| Father's occupation (352) | |||
| Unemployed | 129 (31.1%) | ||
| Mother's education (years) (407) | 13.35 (2.226) | 8, 23 | |
| Mother's occupation (441) | |||
| Unemployed | 228 (51.7%) |
Because the data collection/entries are still ongoing, the N values reported here may not be consistent across tables.
Table 4.
Descriptive data on key behavioral measures
| Measure/instrument | N | Mean (standard deviation) |
|---|---|---|
| Child Behavior Checklist | ||
| Total problems | 380 | 32.12 (24.81) |
| Internalizing | 380 | 7.53 (7.36) |
| Externalizing | 380 | 10.34 (9.28) |
| Aggression | 380 | 7.26 (6.53) |
| Rule‐breaking | 380 | 3.31 (3.33) |
| Attention | 380 | 5.11 (4.45) |
| Reactive–Proactive Aggression Questionnaire | ||
| Reactive aggression | 412 | 9.41 (4.41) |
| Proactive aggression | 412 | 2.38 (3.08) |
| Total aggression | 412 | 11.79 (6.68) |
| Diagnostic Interview Schedule for Children | ||
| Conduct Disorder lifetime diagnosis | 443 | 14.2% |
| Oppositional Defiant Disorder lifetime diagnosis | 443 | 19.1% |
| Child Self‐report | ||
| Oppositional Defiant Disorder | 411 | 5.87 (3.72) |
| Conduct Disorder | 411 | 2.19 (3.18) |
| Oppositional Defiant Disorder and Conduct Disorder | 411 | 8.06 (6.29) |
Second component: randomized clinical trial (RCT)
The intervention consists of four groups: CBT only, nutritional supplements only, CBT combined with nutritional supplements, and usual care. The CBT manualized intervention was developed from an existing program from the Penn Resiliency program (Cutuli et al., 2006) that was originally developed as a group‐based CBT to enhance self‐esteem and resiliency in school‐aged children. We selected this program because of its proven efficacy in children of mixed racial and ethnic backgrounds. Working with one of the original authors of the intervention, we converted this CBT to an individualized conjoint parent–child program with an enhanced focus on aggressive behaviors. We piloted this revised intervention on youth prior to study inception to refine the language and the exercises that had been transformed from group to individual exercises and homework. Once this process was completed, an accompanying parent manual was developed to complement the youth lessons and to enhance parenting techniques that would reward good behavior and reduce reinforcements of aggressive behaviors.
Fidelity monitoring
As recommended by external site visitor reviewers, we added three part‐time interventionists in addition to our full‐time lead interventionist for the CBT arm. We routinely conduct fidelity monitoring of randomly‐selected sessions with the lead interventionists. To date, results demonstrate that there are very rare examples of deviations from technique and intent on the part of the interventionist (two deviations in 20 randomly selected sessions). Fidelity monitoring has expanded to the three additional interventionists.
In addition, we recognize that retention in this study is important in order to reduce bias and improve generalizability (Needham et al., 2005). We are experienced at using multiple strategies to enhance retention. Consistent with recommendations from Rajotte et al. (2003), the following well‐established strategies are in place: (1) establish a working research relationship with the child and parent; (2) schedule intervention sessions at times convenient to the child/parent; (3) incorporate a schedule for make‐up sessions; (4) compensate for intervention attendance; (5) compensate on a pro‐rated basis for follow‐up assessments; (6) arrange follow‐up appointments at a time and location convenient for child/parent.
Furthermore, to ensure continuation in all CBT sessions, parents have the option to bring the child either to the offices of the study team or to have the interventionist conduct the session in their home. Although we recognize that varying locations (office versus home) may introduce some confounding, we track and include these data in our analysis. In addition, our analytic approach is an intent‐to‐treat analysis for maximal scientific rigor, but we also monitor completion of the intervention and ascertain the effects of varying “doses” of the intervention on outcomes.
Third component: animal model
The animal project focuses on the effects of dietary omega‐3 fatty acids on social interactions, the development of aggression, and hormonal stress‐responses (corticosterone levels). We have maintained BALB/cJ mice, a strain known to be highly stress responsive and relatively aggressive (Augustsson and Meyerson, 2004; Dow et al., 2011), on diets with either low omega‐3 (omega‐6:omega‐3 ratio of 20) or high omega‐3 fatty acid content (omega‐6:omega‐3 ratio of 1) from the juvenile period to adulthood. Once assigned to a particular type of diet, each mouse is maintained continuously on that type of diet throughout this developmental period. Mice on the two different diets are assessed for aggressive and social affiliative behaviors between littermates in their home cages at two time points during adolescent development, and then in response to intrusion of an unfamiliar intruder mouse during adulthood, in three resident‐intruder tests on three consecutive days. Corticosterone levels are measured following the exposure to the unfamiliar intruder mouse following the third resident‐intruder test. The controlled nature of this mouse model study may provide additional insights into the effects of omega‐3 fatty acid content of diets on modulation of social behavior, aggression, and stress responses.
Planned analyses
Analyses will center around two main components of the study. The first set will focus on the risk assessment data and will include all participants. The focus of these analyses lies with identifying the environmental, social, psychological, and neurobiological factors that act as risk factors or confer protection for childhood aggression. Analyses will assess interactions between putative protective factors and risk factors, to identify risk factors that are specific to either reactive or proactive forms of aggression, and to examine the interaction of environmental and biological factors in contributing to child aggression.
The second set of analyses will focus on treatment outcome. Will the nutritional supplement group show reductions in aggression which are just as strong as the CBT group? Will any post‐treatment effects be maintained at follow‐up? Will the combination of both nutritional supplements and CBT be more effective in reducing aggression than either treatment alone?
Our plan for statistical analyses is to emphasize bioinformatics for the prediction component and more traditional statistical techniques for a priori hypotheses on risk/protective factors and treatment components. Regarding traditional techniques, data reduction and main analyses will be similar to those conducted in our prior research which have used combinations of analysis of variance (ANOVA), multivariate analysis of variance (MANOVA), covariance analysis, chi‐square, multiple regression, multinomial logistic regression, confirmatory factor analysis, and structural equation modeling. Regarding bioinformatics (machine learning and data mining), we will use bioinformatics analytic techniques, largely taken from the machine learning (ML) and data mining (DM) domains, as adjuncts to the planned statistical analyses for each of the aims of this project. The rationale for incorporating these techniques in this project is not to supplant traditional statistical analyses. Rather, we will use these techniques to inform the statistical analyses by discovering patterns in the data, such as genetic, imaging, psychosocial, behavioral, and environmental interactions with participant characteristics and ultimately with aggression as the clinical outcome. Analytic approaches continue to evolve as the study develops and may be revised.
Comments
This research project tackles the enormously important issue of youth violence. If we can predict future aggression and violence at a relatively early age before it starts, we will be in a much better position to apply intervention programs to take aggression‐prone children off a life path to violent crime.
This interdisciplinary study involving more than nine departments across four Schools at the University of Pennsylvania and five additional institutions within Pennsylvania will be one of the most comprehensive biosocial attempts to explain aggression in children. The inclusion of an animal model provides additional avenues for translational research, and for further investigating the biological mechanisms of nutritional interventions. Additionally, we are working to identify how participation in this project by outside organizations can lead to sustainable replication, should the interventions be found to be effective. This inclusion of outside organizations has led to strong interest in the areas of recreation, nutritional services, primary health care, and school counseling.
By examining a wide range of neighborhood, environmental, social, psychological, psychiatric, and neurobiological risk and productive factors for aggression, we hope to be better able to predict later violence. Our experimental interventions to reduce aggression in children may provide novel ways of tackling this critically‐important problem in growing children and adolescents. We anticipate that by more effectively addressing aggression and violence at a critical period in childhood, we may contribute to improving the health status of all children and adults and also limit the enormous financial, physical, emotional, and psychological damage that violence perpetration creates in society in general. Because violence is a major public health problem, more effective early prediction and treatment of aggression and violence is thought to be of major benefit to society.
Declaration of interest statement
The authors have no competing interests.
Acknowledgments
This project was funded, in part, under a grant from the Pennsylvania Department of Health (SAP# 4100043366). The Department specifically disclaims responsibility for any analyses, interpretations or conclusions. It was also supported by the Clinical & Translational Research Center, Perelman School of Medicine, University of Pennsylvania (grant number UL1‐RR‐024134). We also thank the CHOP Pediatric Research Consortium for their help during the recruitment stage.
References
- Abidin R.R. (1990) Parenting Stress Index (PSI), Charlottesville, VA: Pediatric Psychology Press. [Google Scholar]
- Achenbach T.M. (1991) Manual for the Child Behavior Checklist/4–18 and 1991 Profile, Burlington, VT: Department of Psychiatry, University of Vermont. [Google Scholar]
- Andreasen N.J., Endicott J., Spitzer R.L., Winokur G. (1977) The family history method using diagnostic criteria. Archives of General Psychiatry, 34(10), 1229–1235. [DOI] [PubMed] [Google Scholar]
- Augustsson H., Meyerson B.J. (2004) Exploration and risk assessment: a comparative study of male house mice (Mus musculus musculus) and two laboratory strains. Physiology Behavior, 81(4), 685–698. [DOI] [PubMed] [Google Scholar]
- Buss A.H., Perry M. (1992) The aggression questionnaire. Journal of Personal and Sociol Psychology, 63(3), 452–459. [DOI] [PubMed] [Google Scholar]
- Cutuli J., Chaplin T.M., Gillham J.E., Reivich K.J., Seligman M.E.P. (2006) Preventing co‐occurring depression symptoms in adolescents with conduct problems. Annals of the New York Academy of Sciences, 1094(1), 282–286. [DOI] [PubMed] [Google Scholar]
- DeMar J.C. Jr, Ma K., Bell J.M., et al (2006) One generation of n‐3 polyunsaturated fatty acid deprivation increases depression and aggression test scores in rats. Journal of Lipid Research, 47(1), 172–180. [DOI] [PubMed] [Google Scholar]
- Diener E., Emmons R.A., Larsen R.J., Griffin S. (1985) The satisfaction with life scale. Journal of Personal Assessment, 49(1), 71–75. [DOI] [PubMed] [Google Scholar]
- Dow H.C., Kreibich A.S., Kaercher K.A., Sankoorikal G.M., Pauley E.D., Lohoff F.W., Brodkin E.S. (2011) Genetic dissection of intermale aggressive behavior in BALB/cJ and A/J mice. Genes and Brain Behavior, 10(1), 57–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duckworth A.L., Peterson C., Matthews M.D., Kelly D.R. (2007) Grit: perseverance and passion for long‐term goals. Journal of Personal and Social Psychology, 92(6), 1087–1101. [DOI] [PubMed] [Google Scholar]
- Frick P. (1991) The Alabama Parenting Questionnaire. Unpublished instrument, University of Alabama.
- Frick P., Hare R. (2001) The Antisocial Process Screening Device, Toronto: Multi‐Health Systems. [Google Scholar]
- Gesch C.B., Hammond S.M., Hampson S.E., Eves A., Crowder J.M. (2002) Influence of supplementary vitamins, minerals and essential fatty acids on the antisocial behavior of young adult prisoners: randomized, placebo‐controlled trial. British Journal of Psychiatry, 181, 22–28. [DOI] [PubMed] [Google Scholar]
- Gratz K.L., Roemer L. (2004) Multidimensional assessment of emotion regulation and dysregulation: development, factor structure, and initial validation of the difficulties in emotion regulation scale. Journal of Psychopathology and Behavioral Assessment, 26(1), 41–54. [Google Scholar]
- Gur R.C., Richard J., Hughett P., Calkins M.E., Macy L., Bilker W.B., Brensinger C., Gur R.E. (2010) A cognitive neuroscience‐based computerized battery for efficient measurement of individual differences: Standardization and initial construct validation. Journal of Neuroscience Methods, 187(2), 254–262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pennsylvannia Department of Health . (2007) Request for Applications: Collaborative Research on Violence Prevention or Regenerative Medicine and Post‐natal Stem Cell Biology, RFA Number 06‐07‐15, Harrisburg, PA: Department of Health. [Google Scholar]
- Hibbeln J.R. (2001) Seafood consumption and homicide mortality. A cross‐national ecological analysis. World Review of Nutrition and Dietetics, 88, 41–46. [DOI] [PubMed] [Google Scholar]
- Hoptman M.J., Antonius D. (2011) Neuroimaging correlates of aggression in schizophrenia: an update. Current Opinion in Psychiatry, 24(2), 100–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Itomura M., Hamazaki K., Sawazaki S., Kobayashi M., Terasawa K., Watanabe S., Hamazaki T. (2005) The effect of fish oil on physical aggression in schoolchildren – a randomized, double‐blind, placebo‐controlled trial. Journal of Nutritional Biochemistry, 16(3), 163–171. [DOI] [PubMed] [Google Scholar]
- Jacobs H. (1988) The Los Angeles head injury survey: procedures and initial findings. Archives of Physical Medicine and Rehabilitation, 69(6), 425–431. [PubMed] [Google Scholar]
- Krug E.G., Mercy J.A., Dahlberg L.L., Zwi A.B. (2002) The world report on violence and health. Lancet, 360(9339), 1083–1088. [DOI] [PubMed] [Google Scholar]
- Lewis S., Owen M., Murray R. (1989) Obstetric complications and schizophrenia: methodology and mechanisms In Schizophrenia: Scientific Progress, Schultz S., Tamminga C. (eds), pp. 56–68, New York: Oxford University Press. [Google Scholar]
- Miczek K.A., de Almeida R.M.M., Kravitz E.A., Rissman E.F., de Boer S.F., Raine A. (2007) Neurobiology of escalated aggression and violence. Journal of Neuroscience, 27(44), 11803–11806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris N.M., Udry J.R. (1980) Validation of a self‐administered instrument to assess stage of adolescent development. Journal of Youth and Adolescence, 9(3), 271–280. [DOI] [PubMed] [Google Scholar]
- Needham I., Abderhalden C., Halfens R.J.G., Dassen T., Haug H.‐J., Fischer J.E. (2005) The Impact of Patient Aggression on Carers Scale: instrument derivation and psychometric testing. Scandinavian Journal of Caring Sciences, 19(3), 296–300. [DOI] [PubMed] [Google Scholar]
- Raine A. (1991) The SPQ: a scale for the assessment of schizotypal personality based on DSM‐III‐R criteria. Schizophrenia Bulletin, 17(4), 555–564. [DOI] [PubMed] [Google Scholar]
- Raine A., Dodge K., Loeber R., Gatzke‐Kopp L., Lynam D., Reynolds C., et al (2006) The Reactive–Proactive Aggression Questionnaire: differential correlates of reactive and proactive aggression in adolescent boys. Aggressive Behavior, 32(2), 159–171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rajotte E., Fuchs C., Zatzick D. (2003) Engaging and following trauma survivors in real world clinical investigations. The Journal of Nervous and Mental Disease, 191(4), 265–268. [DOI] [PubMed] [Google Scholar]
- Sampson R.J., Morenoff J.D., Raudenbush S. (2005) Social anatomy of racial and ethnic disparities in violence. American Journal of Public Health, 95(2), 224–232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schakel S., Sievert Y., Buzzard I. (1988) Sources of data for developing and maintaining a nutrient database. Journal of the American Dietetic Association, 88(10), 1268. [PubMed] [Google Scholar]
- Schakel S.F. (2001) Maintaining a nutrient database in a changing marketplace: keeping pace with changing food products – a research perspective. Journal of Food Composition and Analysis, 14(3), 315–322. [Google Scholar]
- Schakel S.F., Buzzard I.M., Gebhardt S.E. (1997) Procedures for estimating nutrient values for food composition databases. Journal of Food Composition and Analysis, 10(2), 102–114. [Google Scholar]
- Siever L.J. (2008) Neurobiology of aggression and violence. American Journal of Psychiatry, 165(4), 429–442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soyka M. (2011) Neurobiology of aggression and violence in schizophrenia. Schizophrenia Bulletin, 37(5), 913–920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevens L., Zhang W., Peck L., Kuczek T., Grevstad N., Mahon A., Zentall S.S., Arnold I.E., Burgess J.R. (2003) EFA supplementation in children with inattention, hyperactivity, and other disruptive behaviors. Lipids, 38(10), 1007–1021. [DOI] [PubMed] [Google Scholar]
- Straus M.A., Hamby S.L., Boney‐McCoy S., Sugarman D.B. (1996) The revised conflict tactics scales (CTS2). Journal of Family Issues, 17(3), 283–316. [Google Scholar]
- Tangney J.P., Baumeister R.F., Boone A.L. (2004) High self‐control predicts good adjustment, less pathology, better grades, and interpersonal success. Journal of Personality, 72(2), 271–324. [DOI] [PubMed] [Google Scholar]
- van Goozen S.M., Fairchild G., Snoek H., Harold G.T. (2007) The evidence for a neurobiological model of childhood antisocial behavior. Psychological Bulletin, 133(1), 149–182. [DOI] [PubMed] [Google Scholar]
- Wechsler D. (2004) The Wechsler Intelligence Scale for Children — Fourth Edition, London: Pearson Assessment. [Google Scholar]
- Zuckerman M. (2002) Zuckerman–Kuhlman Personality Questionnaire (ZKPQ): an alternative five‐factorial model. In De Raad B., Perugini M. (eds), Big Five Assessment, Hogrefe & Huber Publishers. pp. 377–396. [Google Scholar]


