Abstract
Objective
Although several risk factors have been identified for alcohol use disorder, many individuals with these factors do not go on to develop the disorder. Identifying early phenotypic differences between vulnerable individuals and healthy controls could help identify those at higher risk. Binge drinking, defined as reaching a blood alcohol level of 80 mg%, carries a risk of negative legal and health outcomes and may be an early marker of vulnerability. Using a carefully controlled experimental paradigm, we tested the hypothesis that risk factors for alcohol use disorder, including family history of alcoholism, male sex, impulsivity, and low level of response to alcohol, would predict rate of binging during an individual alcohol consumption session.
Method
This cross-sectional study included 159 young social drinkers who completed a laboratory session in which they self-administered alcohol intravenously. Cox proportional hazards models were used to determine whether risk factors for alcohol use disorder were associated with the rate of achieving a binge-level exposure.
Results
A greater percentage of relatives with alcoholism (hazard ratio 1.04, 95% CI 1.02 to 1.07), male sex (hazard ratio 1.74, 95% CI 1.03 to 2.93), and higher impulsivity (hazard ratio 1.17, 95% CI 1.00 to 1.37), were associated with a higher rate of binging throughout the session. Participants with all 3 risk factors had the highest rate of binging throughout the session compared to the lowest risk group (hazard ratio 5.27, 95% CI 1.81 to 15.30).
Conclusions
Binge drinking may be an early indicator of vulnerability to alcohol use disorder and should be carefully assessed as part of a thorough clinical evaluation.
Introduction
Alcohol use disorder has a lifetime prevalence of nearly one in three individuals in the United States (1). An important goal is to identify at-risk individuals prior to the development of this disorder so that they can be targeted for early intervention. One way to determine early phenotypic differences in those at risk is to examine behavior at the level of an individual drinking session. For example, rate of drinking and total alcohol exposure may differ between those at high and low risk. These parameters, however, are difficult to quantify in the field because of the lack of instruments that can continuously and accurately monitor blood alcohol concentration. Furthermore, asking individuals to report details about their rate of consumption does not account for variability in absorption and metabolism (2) and would likely be inaccurate because intoxication impairs recall (3). Despite these measurement difficulties, there is evidence that the rapid consumption of large quantities of alcohol leading to a blood alcohol concentration of 80 mg%, defined as binge drinking (4), affects psychological and physical well-being. Binge-drinking is associated with greater risk of negative health consequences (e.g. myocardial infarction) and legal trouble (5; 6). Binge drinking may signify an innate preference for higher brain alcohol exposure and may begin before an individual meets criteria for an alcohol use disorder, but this hypothesis has never been empirically tested.
One method to assess alcohol consumption that overcomes many of these measurement difficulties is intravenous alcohol self-administration (7). This method has shown good test-retest reliability and external validity (8; 9) and has been employed in pharmacological (10) and genetic studies (11). Intravenous alcohol self-administration has several advantages over oral self-administration. Whereas oral administration at fixed doses can result in up to threefold variability in alcohol exposure between subjects due to pharmacokinetic differences (12; 13), intravenous administration standardizes alcohol exposure by bypassing gastrointestinal absorption and first-pass metabolism. Inter-individual differences in alcohol distribution and elimination are accounted for by using an infusion algorithm that adjusts for age, sex, height, and weight (2). Accordingly, each infusion increases alcohol levels by a fixed quantity, allowing the infusion software to provide continuous estimates of blood alcohol levels that closely track brain alcohol exposure (14) and breathalyzer readouts (15). These estimates can then be used to measure an individual’s total alcohol exposure as well as how quickly they reach a binge level of exposure. This paradigm also eliminates specific cues associated with oral alcoholic beverages, including taste, smell, and appearance. As a result, intravenous self-administration should be driven primarily by alcohol’s pharmacodynamic effects, such as dopamine release in the nucleus accumbens (16). This method is therefore ideal to determine whether preference for higher alcohol exposure is evident prior to the development of alcohol use disorder among individuals with biological risk factors.
The DSM-5 lists the following genetic and physiological risk factors for alcohol use disorder (17): family history of alcoholism (18), male sex (1), impulsivity (19), absence of acute alcohol-related skin flush (20), preexisting schizophrenia or bipolar disorder (21), and a low level of response to alcohol (22). Although these factors markedly increase the risk of developing alcohol use disorder, it remains unclear how they affect the likelihood of risky drinking patterns prior to disorder onset. In the present study, we examined the largest community sample to date of young adult social drinkers using intravenous alcohol self-administration. We investigated whether the genetic and physiological risk factors listed in DSM-5 (except for skin flush and comorbid psychiatric disorders, which were exclusion criteria) were associated with the rate of binge-level exposure during an individual drinking session. We hypothesized that individuals at higher risk for developing an alcohol use disorder would exhibit a preference for higher brain alcohol exposure as demonstrated by higher rates of binging throughout the session and higher levels of total alcohol exposure.
Method
Participant characteristics
One hundred and sixty two social drinkers between the ages of 21 and 45 were recruited through newspaper advertisements and the National Institutes of Health (NIH) Normal Volunteer Office (for detailed demographic information, see Table 1 and ST1, ST2, ST3). To be included, participants must have consumed at least 5 drinks on one occasion at one point in their life. Participants completed a phone screen and subsequently completed an in-person assessment at the NIH Clinical Center in Bethesda, Maryland. The study protocol was approved by the NIH Addictions Institutional Review Board and participants were enrolled after providing written, informed consent.
Table 1.
Characteristics of the Sample by Sex
| Characteristic | Male (N = 86) | Female (N = 73) | ||
|---|---|---|---|---|
|
| ||||
| Mean | SD | Mean | SD | |
| Age (years) | 26.4 | 5.2 | 25.8 | 5.0 |
| Family History Densitya,b | 3.6 | 8.5 | 2.6 | 6.9 |
| Delay Discountinga,c | −4.7 | 1.8 | −4.5 | 1.7 |
| Level of Alcohol Responsed,e | 4.8 | 2.1 | 3.7 | 1.7 |
| AUDIT Score | 5.8 | 2.5 | 5.1 | 2.8 |
|
| ||||
| N | % | N | % | |
|
| ||||
| Family History Positive | 17 | 19. | 11 | 15.1 |
| Current Alcohol Abusea | 2 | 2.4 | 2 | 2.7 |
Missing data for some participants: N = 158 for family history, N = 134 for delay discounting, N = 158 for current alcohol abuse
Family History Density is obtained by dividing the number of first and second degree relatives with an Alcohol Use Disorder by the total number of first and second degree relatives. This value is reported as a percentage. The value displayed here represents the mean and SD for the whole sample. For Family History Density in the Family History Positive group, see ST1.
Delay discounting is a behavioral measure of impulsivity in which participants choose between smaller immediate or larger delayed rewards. Values are reported as the natural logarithm of the discounting constant, k. Lower values of ln(k) indicate lower degrees of delay discounting and less impulsivity.
Level of Alcohol Response is derived from the Self-Rating of the Effects (SRE) of alcohol form, first five drinking occasions. The final score represents the mean of the number of drinks needed to achieve four possible intoxication-related outcomes, with a higher number indicating a lower level of response to alcohol.
Male and female participants have statistically different distributions for level of alcohol response using a Mann-Whitney test (Zu = 3.7, p<0.01)
Participants were excluded if they met any of the following criteria: (1) non-drinker, (2) lifetime history of mood, anxiety or psychotic disorders, (3) current or lifetime history of substance dependence (including alcohol and nicotine), (4) recent illicit use of psychoactive substances, (5) history of acute alcohol-related skin flush, (6) regular tobacco use (>20 uses/week), (7) history of clinically significant alcohol withdrawal, (8) lifetime history of suicide attempts, (9) current or chronic medical conditions, including cardiovascular conditions, requiring inpatient treatment or frequent medical visits, or (10) use of medications that may interact with alcohol within 2 weeks prior to the study. Females were excluded if they were breastfeeding, pregnant, or intended to become pregnant.
All subjects were assessed for psychiatric diagnoses, history of acute alcohol-related skin flush, drinking history, and other risk factors for alcohol use disorder. Diagnoses were assessed by the Structured Clinical Interview for DSM-IV Axis I disorders (SCID-IV) (23). History of acute alcohol-related skin flush was assessed using the Alcohol Flushing Questionnaire (24). Drinking history was assessed using the Alcohol Use Disorder Identification Test (AUDIT) (25). Two participants were excluded from this analysis because they were heavy drinkers based on the Timeline Followback Interview (>20 drinks/week for males, >15 drinks/week for females). One participant was excluded because software failure caused the session to be terminated prior to minute 20 of the alcohol self-administration session, resulting in a final sample size of 159 participants.
Alcohol Use Disorder Risk Factor Measures
Family History
Participants completed the Family Tree Questionnaire (26) to identify first- and second- degree relatives that may have had alcohol-related problems. They subsequently completed the Family History Assessment plus Individual Assessment Modules of the Semi-Structured Assessment for Genetics of Alcoholism for all identified relatives (27). This assessment is widely used in family history based studies, including large genetic studies such as the Collaboration on the Genetics of Alcoholism (COGA) (28). If no information was available about a relative, then that relative was scored as a zero. Relatives with a known history of alcohol-related problems were scored as a one. A family history density score was calculated by dividing the number of relatives with alcohol problems by the total number of first and second degree relatives. One participant did not complete this measure and his value was imputed with the sample median of 0 given that family history density was not normally distributed (Shapiro-Wilk test p < 0.001). We conducted all models with and without this participant and found that his exclusion did not alter our findings, so we report the results with this participant included.
Behavioral Impulsivity
Participants completed a delay discounting task (29), which is a well-validated measure of behavioral impulsivity that has a robust association with alcohol use disorder (30; 31). During this task, participants chose between smaller immediate rewards or $100 received after a delay (e.g. $90 now or $100 in seven days). Immediate rewards ranged in value from $0 to $100 and delay periods ranged from 7 to 30 days. The degree of discounting delayed rewards, k, can be calculated using the equation developed by Mazur and colleagues (32). Since k values were not normally distributed, they were normalized using a logarithmic transformation and reported as ln(k). Lower values of ln(k) suggest less impulsivity and lower degrees of discounting. A portion of the sample did not complete this task (N=25) and missing values of ln(k) were imputed with the sample mean.
Level of Response to Alcohol
Participants also completed the Self-Rating of the Effects of alcohol (SRE) form (33). This instrument assesses response to alcohol during the first five drinking occasions of a person’s life, their heaviest drinking period, and their most recent drinking period. For each period, it asks how many drinks it took for them to feel different, to feel dizzy, to begin stumbling, and to pass out. The final score represents the mean of the number of drinks needed to achieve each outcome, with a higher number of drinks indicating a lower level of response to alcohol. We focused on the first five drinking occasions in the present analyses to reduce the potentially confounding impact of tolerance.
Intravenous Alcohol Self-Administration
Participants were instructed not to drink alcohol in the 48 hours prior to study procedures. Upon arrival, they provided a breathalyzer reading to confirm abstinence. Participants also provided a urine sample that was tested for illicit drugs and, for females, pregnancy; both had to be negative to proceed with the study session. After eating a standardized (350 kcal) meal, an intravenous catheter was inserted into a vein in the forearm. Self-administration was conducted using the Computer-assisted Alcohol Infusion System software, which controls the rate of infusion of 6.0% v/v alcohol in saline for each individual using a physiologically-based, pharmacokinetic model for alcohol distribution and metabolism that accounts for sex, age, height and weight (2).
The alcohol self-administration session consisted of a 25-minute priming phase and a 125-minute free access phase. During the first 10 minutes of the priming phase, participants were required to push a button four times at 2.5 minute intervals. Each button press resulted in an alcohol infusion that raised blood alcohol concentration by 7.5 mg% in 2.5 minutes, such that participants achieved a peak concentration of approximately 30 mg% at minute 10. During the next 15 minutes, the button remained inactive while participants experienced the effects of the alcohol. At minute 25, the free access phase began and participants were instructed to “try to recreate a typical drinking session out with friends.” Participants could self-administer ad libitum, but they had to wait until one infusion was completed before initiating another. Blood alcohol concentration was estimated continuously by the software based on infusion rate and model-estimated metabolism and a readout was provided at 30-second intervals. Breath alcohol concentration was also obtained via breathalyzer at 15-minute intervals to confirm the software-calculated estimates; these readings were entered into the software to provide the model feedback and the infusion rate was automatically adjusted accordingly (2). Software estimates of blood alcohol concentration were used to determine if a participant reached binge-level exposure, defined as achieving an estimated blood alcohol concentration greater than 80 mg% (4). A limit was imposed such that estimated blood alcohol concentration could not exceed 100 mg% to prevent adverse events due to intoxication.
Statistical Analysis
To examine whether risk factors for alcohol use disorder were predictors of rate of binging throughout the free access phase of the IV alcohol self-administration session, we plotted Kaplan-Meier survival curves and conducted Cox proportional hazards models. We generated four Kaplan-Meier survival curves using binary variables (Figure 1): (1) male versus female, (2) family history positive versus negative, (3) high versus low impulsivity (median split), and (4) high versus low level of response to alcohol (median split). For the Cox proportional hazards analyses, the outcome variable was time to binge (estimated blood alcohol concentration of 80 mg%) and participants were censored when they reached a binge or ended the session early (one participant). For the initial Cox proportional hazards model, five independent variables were included: sex was coded as a binary variable (0 for females, 1 for males) and delay discounting, family history density, level of response to alcohol, and age were entered as continuous variables.
Figure 1. Cumulative Probability of Achieving Binge Level Exposure by Each Alcohol Use Disorder Risk Factora.
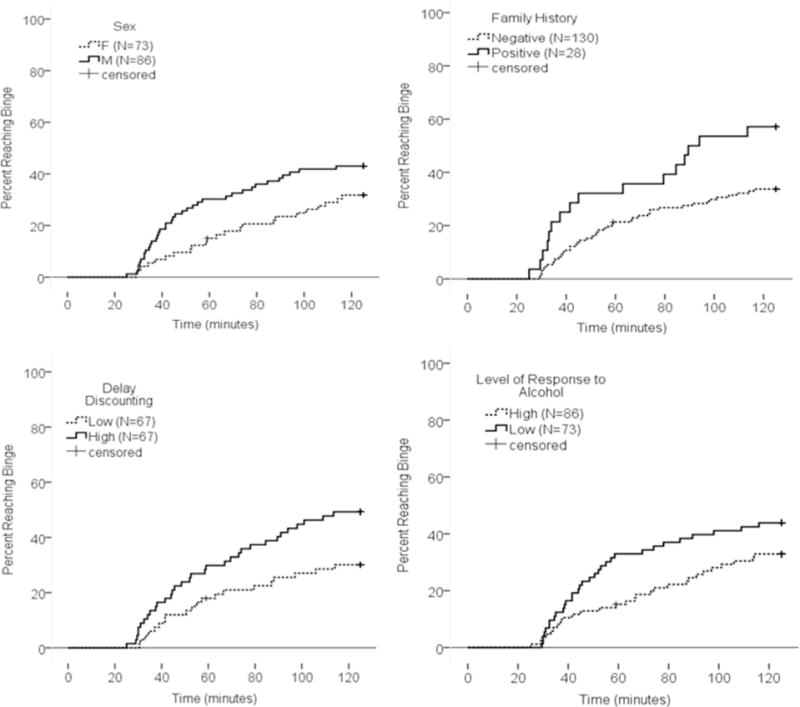
aCumulative probability of achieving a binge level exposure (estimated breath alcohol concentration of 80 mg%) was higher in males than females, family history positive than negative individuals, high than low delay discounters, and low than high responders to alcohol.
To determine whether faster rate of consumption translated into greater overall exposure to alcohol, we calculated area under the curve (AUC, mg%*min) for the alcohol concentration versus time curve across the free-access phase of the session. Three individuals ended the session early due to software malfunction or adverse events (at minutes 59, 88.5, and 99.5), so to generate the AUC for these participants we imputed values for the remainder of the session by carrying their last observed alcohol concentration forward. To confirm the validity of this approach, we applied the same imputation procedure for 20 random participants starting at minute 59 and found that the imputed values correlated highly with the actual values (Spearman’s rho > 0.9). We conducted Mann-Whitney tests to compare AUC distributions for each risk factor as AUC values were not normally distributed (Shapiro Wilk test p < 0.05). For these analyses, we used the binary categorical risk factors described above.
To assess the additive effects of significant variables from the above analyses, we coded individuals according to their number of risk factors for alcohol use disorder. For this analysis, we only used the binary risk factors described above, excluding level of response to alcohol, which did not contribute to the above models. We thus created four groups: a 0, 1, 2, and 3 risk factor group. The 0 risk factor group served as the reference group. We plotted Kaplan-Meier survival curves to examine differences between groups and also fit a Cox proportional hazards model additionally adjusted for age. We also tested if there was evidence of additive effects of risk factors on overall alcohol exposure during the session by comparing the AUC values for different risk groups using a Jonckheere-Terpstra test (34; 35).
Results
Effect of Risk Factors on Rate of Binging
Overall, 60 participants achieved a binge-level exposure and 99 participants had estimated blood alcohol concentrations beneath 80 mg% across the entire session. A higher percentage of bingers were found in family history positive relative to negative individuals (57.1% and 33.1% respectively), males relative to females (43.0% and 31.5% respectively), high relative to low delay discounting individuals (49.3% and 29.9% respectively), and those with a low relative to high level of response to alcohol (43.8% and 32.6% respectively; Figure 1).
We tested if risk factors for alcohol use disorder predicted rate of binging throughout the session using a Cox proportional hazards model with all four risk factors and age as independent variables (Model 1). Family history density was a significant predictor (hazard ratio 1.04, 95% CI 1.02 to 1.07, p = 0.001), whereas male sex (hazard ratio 1.71, 95% CI 1.00 to 2.94, p = 0.052) and delay discounting (hazard ratio 1.17, 95% CI 1.00 to 1.37, p = 0.056) were marginally significant. Level of response to alcohol was not a significant predictor of rate of binging throughout the session (hazard ratio 1.01, 95% CI 0.89 to 1.15, p = 0.840, Table 2). Since level of response was not contributing to the model and was significantly correlated with sex (Spearman’s rho = 0.29, ST4), we dropped it from the model. In this second analysis (Model 2), male sex (hazard ratio 1.74, 95% CI 1.03 to 2.93, p=0.038), delay discounting (hazard ratio 1.17, 95% CI 1.00 to 1.37, p = 0.048), and family history density (hazard ratio 1.04, 95% 1.02 to 1.07, p = 0.002) all significantly predicted binge rate throughout the session. The effects of these risk factors remained consistent when controlling for AUDIT score (Model 3). As would be expected, participants with a higher AUDIT score were more likely to binge (hazard ratio 1.14, 95% CI 1.04 to 1.24, p = 0.004).
Table 2.
Hazard Ratios from Cox Proportional Hazards Models Examining the Effect of Alcohol Use Disorder Risk Factors on Rate of Binginga
| Model 1
|
Model 2
|
Model 3
|
||||
|---|---|---|---|---|---|---|
| Hazard Ratio | 95% CI | Hazard Ratio | 95% CI | Hazard Ratio | 95% CI | |
| Family History | 1.04 | 1.02, 1.07 | 1.04 | 1.02, 1.07 | 1.04 | 1.02, 1.07 |
| Density (%) | ||||||
| Male Sex | 1.71 | 1.00, 2.94 | 1.74 | 1.03, 2.93 | 1.67 | 0.99, 2.82 |
| Delay | 1.17 | 1.00, 1.37 | 1.17 | 1.00, 1.37 | 1.17 | 1.00, 1.37 |
| Discounting | ||||||
| Level of Alcohol | 1.01 | 0.89, 1.15 | — | — | — | — |
| Response | ||||||
| Age | 0.90 | 0.83, 0.97 | 0.90 | 0.83, 0.96 | 0.91 | 0.85, 0.98 |
| AUDIT Score | — | — | — | — | 1.14 | 1.04, 1.24 |
Model 1 examines alcohol use disorder risk factors and age. Model 2 excludes level of alcohol response as it was significantly correlated with sex and did not contribute to Model 1. Model 3 also accounts for AUDIT score to control for the effect of alcohol consumption. For all three models, female sex is the reference group.
Effects of Individual Risk Factors on Total Alcohol Exposure
We tested if each individual risk factor was associated with total alcohol exposure as measured by the area under the estimated blood alcohol concentration versus time curve during the free access phase. Median alcohol exposure was higher in family history positive individuals, males, and participants with delay discounting scores above the median (SF1), with significantly different distributions across sex and delay discounting groups and marginal significance across family history groups (family history U(28, 130) = 2247, p = 0.052; sex U(86, 73) = 3763, p = 0.031; delay discounting U(67, 67) = 2839, p = 0.008). There was no significant difference between those with high and low levels of alcohol response (U(73, 86) = 2619, p = 0.072).
Additive Effects of Risk Factors on Rate of Binging
To investigate whether the significant risk factors from the prior analysis had additive effects, we divided participants based on their number of risk factors into four groups: 0 risk factors (n = 26), 1 risk factor (n = 65), 2 risk factors (n = 36) and 3 risk factors (n = 8), where 0 risk factors indicates a family history negative female with a delay discounting score below the median (see ST5 for characteristics of sample by risk factor group). Cox proportional hazards regression controlling for age demonstrated that, relative to the 0 risk factor group, the 2 risk factor group (hazard ratio 2.54, 95% CI 1.05 to 6.12, p = 0.038) and 3 risk factor group (hazard ratio 5.27, CI 1.81 to 15.30, p = 0.002) binged at higher rates throughout the session. The 0 and 1 risk factor groups did not differ (hazard ratio 1.29, 95% CI 0.55 to 3.04, p = 0.562). These effects remained significant when controlling for level of alcohol response as a continuous variable and AUDIT score (see ST6).
Additive Effects of Risk Factors on Total Alcohol Exposure
Individuals with a greater number of risk factors achieved higher levels of alcohol exposure, with median AUC values of 2132.5 mg%*min, 3814.8 mg%*min, 4565.7 mg%*min, and 7208.5 mg%*min for individuals with the lowest to highest number of risk factors respectively. The results of a Jonckheere-Terpstra test for ordered alternatives indicated that there was a significant effect of number of risk factors on the distribution of AUC values with a small to medium effect size (TJT=3746.0, p=0.001, Kendall’s τ=0.22, Figure 3). Bonferroni corrected pairwise comparisons indicated that the distribution of the AUCs for the 2 and 3 risk factor groups were significantly different than that of the 0 risk factor group, and the 3 risk factor group’s distribution of AUC values also differed from that of the 1 risk factor group (p < 0.05 for all tests).
Figure 3. Total Alcohol Exposure by Alcohol Use Disorder Risk Factor Groupa.
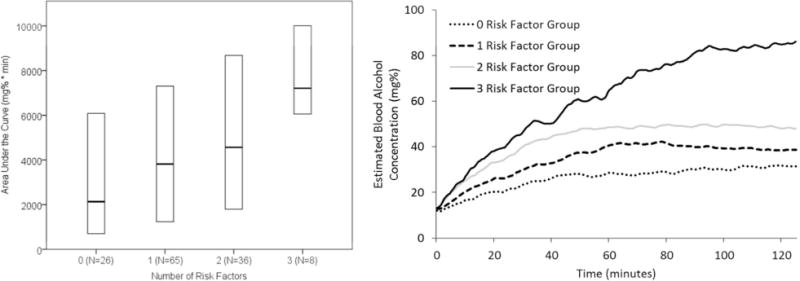
a(A) The area under the curve for the estimated breath alcohol concentration by time plot (total alcohol exposure) was examined in each Alcohol Use Disorder risk factor group. Having a higher number of risk factors was significantly associated with total alcohol exposure during the session. The horizontal line in the middle of each box indicates the median, while the bottom and top borders of the box represent the 25th and 75th percentile values, respectively. (B) Lines represent mean blood alcohol concentration for each group.
Discussion
Young social drinkers at risk for an alcohol use disorder had consumption patterns that were markedly different from low risk drinkers during a free-access intravenous alcohol self-administration session. Vulnerable drinkers had higher rates of binging throughout the session and greater overall exposure to alcohol. The effects of these risk factors were additive. This finding is especially remarkable given the similarity of AUDIT scores between the higher and lower risk groups and given that these effects remained largely unchanged when controlling for AUDIT scores. We believe that this is the first large pharmacokinetically-controlled study to show that the presence of risk factors for alcohol use disorder leads to different patterns of drinking at the level of an individual drinking session in young social drinkers who have not yet developed the disorder. These findings suggest an innate neurobiological preference for higher alcohol exposure that may contribute to alcohol use disorder risk.
Of the factors we examined, family history of alcoholism was most strongly associated with rate of binging during the session, with a small to medium effect size. This finding accords with epidemiologic studies showing that up to half of the risk of alcoholism is genetic and corroborates the results of a small intravenous alcohol self-administration study that showed that family history positive individuals achieved higher alcohol exposures (36). Our study extends these intravenous alcohol self-administration results by showing that participants with a greater percentage of biological relatives with alcohol problems were at greater risk. Our study also found higher rates of alcohol consumption in males compared to females, which is consistent with a recent study of intravenous alcohol self-administration in adolescents (9). Delay discounting has previously been observed as a predictor of laboratory alcohol consumption (8), and we confirmed that here. Level of response to alcohol was not related to rate of binging or total alcohol exposure in our study. This may be partially due to the surprising fact that participants with a low level of response to alcohol in our study actually had lower family history densities for alcoholism than participants with a high level of response (ST3), which is the opposite of what has been found in most studies (37), although controlling for family history density did not change our results. Level of response to alcohol may have been influenced by recall bias and may have shown more predictive power if it had been assessed experimentally as in Schuckit and colleagues’ original studies (22). Despite some evidence that level of response may vary as a function of rate of change in blood alcohol concentration and drinking history (37; 38), we chose to use a simpler static measure of level of response here. More complex assessments of level of response may yield different results.
There were several limitations to this study, most notably the cross-sectional design. Longitudinal studies will be needed to confirm that differing patterns of consumption early on are predictive of the development of an alcohol use disorder. Intravenous alcohol self-administration also differs in many ways from real-world alcohol consumption. However, recent results suggest that intravenous self-administration is reflective of external consumption patterns when comparing across drinkers of varying severity (9; 39). A few individuals in our sample were in their forties and an even younger sample would have been ideal to assess the effects of these risk factors, although the vast majority of our sample (86.1%) was at or below the age of 30. When we controlled for age in our analyses, the effects we observed remained significant. The additive risk factor analysis requires replication, especially given the low number of individuals in the 3 risk factor group. Finally, we could not assess how acute alcohol-related skin flush, smoking, and preexisting psychiatric disorders contribute to rate of binging in this sample because these were exclusion factors for our study. This limits the generalizability of our findings, especially as smoking and psychopathology are highly comorbid with alcoholism. Future studies should determine whether these factors affect rates of alcohol consumption in young adults.
Prior to the development of an alcohol use disorder, those at higher risk demonstrated differing patterns of alcohol consumption including higher rates of binging and greater total alcohol exposure. Although most screening tools for alcoholism focus on quantity of consumption across many sessions, focusing on binging and total alcohol exposure during individual drinking sessions may be clinically relevant and may allow for earlier detection of high risk individuals. Assessing binging and total alcohol exposure in the laboratory, and eventually in the field when appropriate technology is available, may be a helpful way of selecting individuals who require early intervention. Clinical questions regarding the time course of typical drinking sessions, in addition to standard questions about quantity of alcohol consumed, may help better characterize total alcohol exposure and stratify risk. There are likely neurobiological factors that contribute to the way each person drinks, and this may dispose some individuals to achieve blood alcohol concentrations that endanger them.
Supplementary Material
Figure 2. Cumulative Probability of Achieving Binge Level Exposure by Alcohol Use Disorder Risk Factor Groupa.
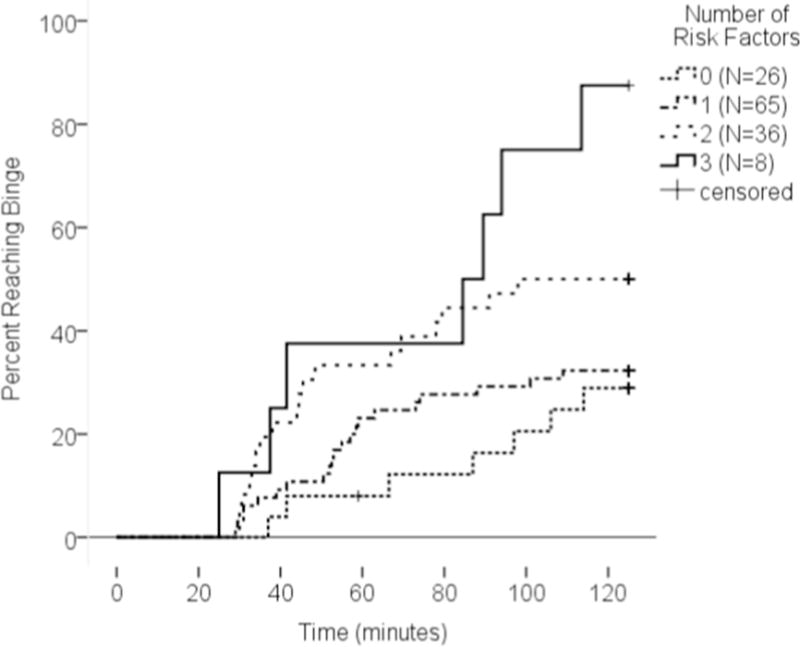
aEach participant was categorized as having either 0, 1, 2, or 3 risk factors (0 = female, family history negative, low impulsivity; 3 = male, family history positive, high impulsivity). The cumulative probability of binging increased in participants with a greater numbers of risk factors.
Acknowledgments
This study was supported by the NIAAA Division of Intramural Clinical and Biological Research (Z1A AA000466). Development of the software used for the intravenous alcohol self-administration session was supported by Sean O’Connor, M.D. at the Indiana Alcohol Research Center (NIH P60 AA007611). We would like to acknowledge the late Dr. Daniel Hommer for his mentorship and clinical oversight, Dr. Mary Lee, Dr. David T. George and Nurse Practitioner LaToya Sewell for medical support and monitoring safety of the participants, and Markus Heilig, Reza Momenan and Melanie Schwandt for their programmatic and operational support. We thank Tasha Cornish and Monique Ernst for comments on earlier drafts of this manuscript. We thank Joel Stoddard and Ruth Pfeiffer for analytic suggestions. We could not have completed this study without the help of the staff of the 5-SW day hospital and 1-HALC alcohol clinic at the NIH Clinical Center. Lastly, for their help collecting this data, we are grateful to our post-baccalaureate trainees: Julnar Issa, Megan Cooke, Marion Coe, Molly Zametkin, Kristin Corey, Jonathan Westman, Lauren Blau, and Courtney Vaughan.
ClinicalTrials.gov identifier: NCT00713492
Footnotes
Disclosures: All authors report no conflict of interests.
References
- 1.Grant BF, Goldstein RB, Saha TD, Patricia Chou S, Jeesun J, Haitao Z, Pickering RP, June Ruan W, Smith SM, Boji H, Hasin DS. Epidemiology of DSM-5 Alcohol Use Disorder. JAMA Psychiatry. 2015;72:757. doi: 10.1001/jamapsychiatry.2015.0584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ramchandani VA, Bolane J, Li TK, O’Connor S. A physiologically-based pharmacokinetic (PBPK) model for alcohol facilitates rapid BrAC clamping. Alcohol Clin Exp Res. 1999;23:617–623. [PubMed] [Google Scholar]
- 3.Goodwin DW, Powell B, Bremer D, Hoine H, Stern J. Alcohol and recall: state-dependent effects in man. Science. 1969;163:1358–1360. doi: 10.1126/science.163.3873.1358. [DOI] [PubMed] [Google Scholar]
- 4.US Department of Health & Human Services; NIH; National Institute on Alcohol Abuse & Alcoholism. NIAAA Council Approves Definition of Binge Drinking [Internet] PsycEXTRA Dataset. Available from: http://dx.doi.org/10.1037/e306662005-004.
- 5.Ruidavets J-B, Ducimetière P, Evans A, Montaye M, Haas B, Bingham A, Yarnell J, Amouyel P, Arveiler D, Kee F, Bongard V, Ferrières J. Patterns of alcohol consumption and ischaemic heart disease in culturally divergent countries: the Prospective Epidemiological Study of Myocardial Infarction (PRIME) BMJ. 2010;341:c6077. doi: 10.1136/bmj.c6077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wechsler H. Health and behavioral consequences of binge drinking in college. A national survey of students at 140 campuses. JAMA. 1994;272:1672–167. [PubMed] [Google Scholar]
- 7.Zimmermann US, O’Connor S, Ramchandani VA. Modeling alcohol self-administration in the human laboratory. Curr Top Behav Neurosci. 2013;13:315–35. doi: 10.1007/7854_2011_149. [DOI] [PubMed] [Google Scholar]
- 8.Stangl BL, Vatsalya V, Zametkin MR, Cooke ME, Plawecki MH, O’Connor S, Ramchandani VA. Exposure-Response Relationships during Free-Access Intravenous Alcohol Self-Administration in Nondependent Drinkers: Influence of Alcohol Expectancies and Impulsivity [Internet] Int J Neuropsychopharmacol. 2016 doi: 10.1093/ijnp/pyw090. Available from: http://dx.doi.org/10.1093/ijnp/pyw90. [DOI] [PMC free article] [PubMed]
- 9.Jünger E, Gan G, Mick I, Seipt C, Markovic A, Sommer C, Plawecki MH, O’Connor S, Smolka MN, Zimmermann US. Adolescent Women Induce Lower Blood Alcohol Levels Than Men in a Laboratory Alcohol Self-Administration Experiment. Alcohol Clin Exp Res. 2016;40:1769–177. doi: 10.1111/acer.13122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vatsalya V, Gowin JL, Schwandt ML, Momenan R, Coe MA, Cooke ME, Hommer DW, Bartlett S, Heilig M, Ramchandani VA. Effects of Varenicline on Neural Correlates of Alcohol Salience in Heavy Drinkers [Internet] Int J Neuropsychopharmacol. 2015;18 doi: 10.1093/ijnp/pyv068. Available from: http://dx.doi.org/10.1093/ijnp/pyv068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Suchankova P, Yan J, Schwandt ML, Stangl BL, Caparelli EC, Momenan R, Jerlhag E, Engel JA, Hodgkinson CA, Egli M, Lopez MF, Becker HC, Goldman D, Heilig M, Ramchandani VA, Leggio L. The glucagon-like peptide-1 receptor as a potential treatment target in alcohol use disorder: evidence from human genetic association studies and a mouse model of alcohol dependence. Transl Psychiatry. 2015;5:e583. doi: 10.1038/tp.2015.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ramchandani VA, Plawecki M, Li T-K, O’Connor S. Intravenous ethanol infusions can mimic the time course of breath alcohol concentrations following oral alcohol administration in healthy volunteers. Alcohol Clin Exp Res. 2009;33:938–944. doi: 10.1111/j.1530-0277.2009.00906.x. [DOI] [PubMed] [Google Scholar]
- 13.Friel PN, Baer JS, Logan BK. Variability of ethanol absorption and breath concentrations during a large-scale alcohol administration study. Alcohol Clin Exp Res. 1995;19:1055–1060. doi: 10.1111/j.1530-0277.1995.tb00988.x. [DOI] [PubMed] [Google Scholar]
- 14.Gomez R, Behar KL, Watzl J, Weinzimer SA, Gulanski B, Sanacora G, Koretski J, Guidone E, Jiang L, Petrakis IL, Pittman B, Krystal JH, Mason GF. Intravenous ethanol infusion decreases human cortical γ-aminobutyric acid and N-acetylaspartate as measured with proton magnetic resonance spectroscopy at 4 tesla. Biol Psychiatry. 2012;71:239–246. doi: 10.1016/j.biopsych.2011.06.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Plawecki MH, Zimmermann US, Vitvitskiy V, Doerschuk PC, Crabb D, O’Connor S. Alcohol Exposure Rate Control Through Physiologically Based Pharmacokinetic Modeling. Alcohol Clin Exp Res. 2012;36:530–542. doi: 10.1111/j.1530-0277.2011.01706.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ramchandani VA, Umhau J, Pavon FJ, Ruiz-Velasco V, Margas W, Sun H, Damadzic R, Eskay R, Schoor M, Thorsell A, Schwandt ML, Sommer WH, George DT, Parsons LH, Herscovitch P, Hommer D, Heilig M. A genetic determinant of the striatal dopamine response to alcohol in men. Mol Psychiatry. 2011;16:809–817. doi: 10.1038/mp.2010.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5®) American Psychiatric Pub; 2013. [Google Scholar]
- 18.Dawson DA, Grant BF. Family history of alcoholism and gender: their combined effects on DSM-IV alcohol dependence and major depression. J Stud Alcohol. 1998;59:97–106. doi: 10.15288/jsa.1998.59.97. [DOI] [PubMed] [Google Scholar]
- 19.Caspi A, Moffitt TE, Newman DL, Silva PA. Behavioral observations at age 3 years predict adult psychiatric disorders. Longitudinal evidence from a birth cohort. Arch Gen Psychiatry. 1996;53:1033–1039. doi: 10.1001/archpsyc.1996.01830110071009. [DOI] [PubMed] [Google Scholar]
- 20.Li D, Zhao H, Gelernter J. Strong protective effect of the aldehyde dehydrogenase gene (ALDH2) 504lys (*2) allele against alcoholism and alcohol-induced medical diseases in Asians. Hum Genet. 2012;131:725–737. doi: 10.1007/s00439-011-1116-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Regier DA, Farmer ME, Rae DS, Locke BZ, Keith SJ, Judd LL, Goodwin FK. Comorbidity of mental disorders with alcohol and other drug abuse. Results from the Epidemiologic Catchment Area (ECA) Study. JAMA. 1990;264:2511–2518. [PubMed] [Google Scholar]
- 22.Schuckit MA. Low level of response to alcohol as a predictor of future alcoholism. Am J Psychiatry. 1994;151:184–189. doi: 10.1176/ajp.151.2.184. [DOI] [PubMed] [Google Scholar]
- 23.First MB. Structured Clinical Interview for DSM-IV-TR Axis I Disorders: Patient Edition. 2005 [Google Scholar]
- 24.Johnson RC, Nagoshi CT, Schwitters SY, Bowman KS, Ahern FM, Wilson JR. Further investigation of racial/ethnic differences and of familial resemblances in flushing in response to alcohol. Behav Genet. 1984;14:171–178. doi: 10.1007/BF01065539. [DOI] [PubMed] [Google Scholar]
- 25.Saunders JB, Aasland OG, Babor TF, de la Fuente JR, Grant M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative Project on Early Detection of Persons with Harmful Alcohol Consumption–II. Addiction. 1993;88:791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- 26.Vogel-Sprott M, Chipperfield B, Hart DM. Family history of problem drinking among young male social drinkers: Reliability of the Family Tree Questionnaire. Drug Alcohol Depend. 1985;16:251–256. doi: 10.1016/0376-8716(85)90049-3. [DOI] [PubMed] [Google Scholar]
- 27.Bucholz KK, Cadoret R, Cloninger CR, Dinwiddie SH, Hesselbrock VM, Nurnberger JI, Jr, Reich T, Schmidt I, Schuckit MA. A new, semi-structured psychiatric interview for use in genetic linkage studies: a report on the reliability of the SSAGA. J Stud Alcohol. 1994;55:149–158. doi: 10.15288/jsa.1994.55.149. [DOI] [PubMed] [Google Scholar]
- 28.Rice JP, Reich T, Bucholz KK, Neuman RJ, Fishman R, Rochberg N, Hesselbrock VM, Nurnberger JI, Jr, Schuckit MA, Begleiter H. Comparison of direct interview and family history diagnoses of alcohol dependence. Alcohol Clin Exp Res. 1995;19:1018–1023. doi: 10.1111/j.1530-0277.1995.tb00983.x. [DOI] [PubMed] [Google Scholar]
- 29.Bickel WK, Odum AL, Madden GJ. Impulsivity and cigarette smoking: delay discounting in current, never, and ex-smokers. Psychopharmacology. 1999;146:447–454. doi: 10.1007/pl00005490. [DOI] [PubMed] [Google Scholar]
- 30.MacKillop J, Amlung MT, Few LR, Ray LA, Sweet LH, Munafò MR. Delayed reward discounting and addictive behavior: a meta-analysis. Psychopharmacology. 2011;216:305–321. doi: 10.1007/s00213-011-2229-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Amlung M, Vedelago L, Acker J, Balodis I, MacKillop J. Steep delay discounting and addictive behavior: a meta-analysis of continuous associations. Addiction. 2017;112:51–62. doi: 10.1111/add.13535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mazur JE. In: An Adjusting Procedure for Studying Delayed Reinforcement. Quantitative Analyses of Behavior, v5. The effect of Delay and of Intervening Events on Reinforcement Value. Commons ML, Mazur JE, Nevin JA, Rachlin H, editors. 1987. pp. 55–73. [Google Scholar]
- 33.Schuckit MA, Smith TL, Tipp JE. The Self-Rating of the Effects of alcohol (SRE) form as a retrospective measure of the risk for alcoholism. Addiction. 1997;92:979–988. [PubMed] [Google Scholar]
- 34.Terpstra TJ. The asymptotic normality and consistency of kendall’s test against trend, when ties are present in one ranking. Indagationes Mathematicae (Proceedings) 1952;55:327–333. [Google Scholar]
- 35.Jonckheere AR. A Distribution-Free k-Sample Test Against Ordered Alternatives. Biometrika. 1954;41:133. [Google Scholar]
- 36.Zimmermann US, Mick I, Laucht M, Vitvitskiy V, Plawecki MH, Mann KF, O’Connor S. Offspring of parents with an alcohol use disorder prefer higher levels of brain alcohol exposure in experiments involving computer-assisted self-infusion of ethanol (CASE) Psychopharmacology. 2009;202:689–697. doi: 10.1007/s00213-008-1349-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Quinn PD, Fromme K. Subjective response to alcohol challenge: a quantitative review. Alcohol Clin Exp Res. 2011;35:1759–1770. doi: 10.1111/j.1530-0277.2011.01521.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wetherill L, Morzorati SL, Foroud T, Windisch K, Darlington T, Zimmerman US, Plawecki MH, O’Connor SJ. Subjective perceptions associated with the ascending and descending slopes of breath alcohol exposure vary with recent drinking history. Alcohol Clin Exp Res. 2012;36:1050–1057. doi: 10.1111/j.1530-0277.2011.01642.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hendershot CS, Wardell JD, McPhee MD, Ramchandani VA. A prospective study of genetic factors, human laboratory phenotypes, and heavy drinking in late adolescence [Internet] Addict Biol. 2016 doi: 10.1111/adb.12397. Available from: http://dx.doi.org/10.1111/adb.12397. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


