Abstract
Staphylococcus warneri, a coagulase negative staphylococcus, has been isolated in prosthetic device-related infections and has been reported as a rare cause of endocarditis. We report a case of prosthetic aortic valve S. warneri endocarditis, in which the patient lacked typical infectious signs and symptoms, instead presenting with congestive heart failure due to perforation of the valve. Providers should consider endocarditis with a low virulence pathogen such as S. warneri when a patient with a prosthetic valve presents with heart failure, even in the absence of fever, leukocytosis and other infectious symptoms.
Keywords: Staphylococcus warneri, Prosthetic valve endocarditis
Introduction
Staphylococcus warneri is a member of the coagulase negative staphylococci (CoNS), occasionally isolated in cases of nosocomial bacteremia and typically associated with the presence of prosthetic devices such as dialysis catheters. It has been recognized as an uncommon cause of infective endocarditis with eight prior cases described in the English literature, six of which involved native valves and two of which involved prosthetic valves [1-7]. Herein, we present a case of prosthetic aortic valve endocarditis, in which the patient presented with symptoms of congestive heart failure (CHF) and the possibility of endocarditis was raised by new valvular dysfunction on echocardiography.
Case Report
A 67-year-old man presented to the emergency department (ED) complaining of stabbing chest pain, subjective fevers, chills, watery diarrhea, nausea and vomiting for 1 week. His past medical history was notable for three vessel coronary artery bypass grafts and a 23 mm bioprosthetic aortic valve replacement surgery 7 months prior, and an ischemic stroke 2 months prior that left him with residual left-sided hemiparesis. In the ED, he was found to have atrial fibrillation with rapid ventricular response and a heart rate in the 130s (Fig. 1). His exam was notable for a grade 3/6 early peaking systolic murmur, best heard at the left upper sternal border and no diastolic murmur, and decreased breath sounds at the bilateral lung bases without crackles. The remainder of his exam was unremarkable and he had no stigmata of endocarditis. The patient had no leukocytosis and laboratory values were largely unremarkable, except for a troponin in the indeterminate range (Table 1) [1-8]. Chest radiograph showed left basilar opacification, consolidation versus pleural effusion, and pulmonary venous congestion (Fig. 2). Shortly after admission, he developed hypoxic respiratory failure and required intubation and admission to the intensive care unit.
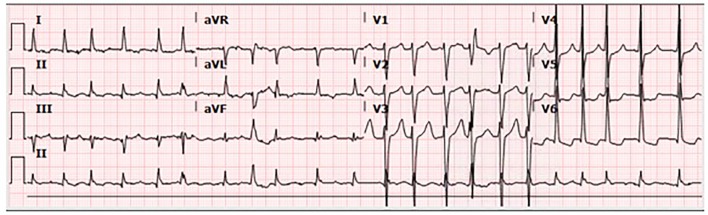
Figure 1.
The 12-lead electrocardiogram showing atrial fibrillation with rapid ventricular response and heart rate of 131 beats per minute.
Table 1. Laboratory Values on Hospital Admission.
| Complete blood count | |
|---|---|
| White blood cells | 5,500/mm3. Differential: neutrophils 51.9%, lymphocytes 26.7%, monocytes 13.3%, eosinophils 7.1%, basophils 1%. |
| Hemoglobin | 11.3 g/dL |
| Hematocrit | 34.5% |
| Platelets | 221,000/mm3 |
| Coagulation profile | |
| Prothrombin time (PT) | 14.2 s |
| Partial thromboplastin time (PTT) | 26.3 s |
| International normalized ratio (INR) | 1.11 |
| Comprehensive metabolic panel | |
| Sodium | 141 mmol/L |
| Potassium | 3.4 mmol/L |
| Chloride | 106 mmol/L |
| Bicarbonate | 26 mmol/L |
| Blood urea nitrogen | 16 mg/dL |
| Creatinine | 1.06 mg/dL |
| Glucose | 101 mg/dL |
| Albumin | 3.5 g/dL |
| Total protein | 6.1 g/dL |
| Alkaline phosphatase | 82 U/L |
| Alanine amino transferase (ALT) | 12 U/L |
| Aspartate amino transferase (AST) | 18 U/L |
| Total bilirubin | 0.7 mg/dL |
| Direct bilirubin | 0.1 mg/dL |
| Troponin | 0.058 mg/mL (reference ranges: normal ≤ 0.028; acute myocardial infarction ≥ 0.3) |
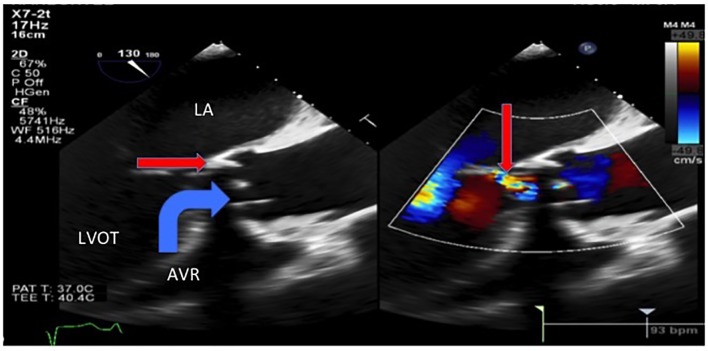
Figure 2.
Portable chest X-ray on admission, with opacification of the left lung base (pleural effusion vs. consolidation), scattered density in the right lung base, and pulmonary venous congestion.
Transthoracic echocardiogram showed new prosthetic valvular dysfunction with at least moderate aortic regurgitation and severely elevated transaortic gradients aortic when compared with his last echocardiogram 2 months prior (that showed a normally functioning and a well-seated bioprosthetic valve). He remained afebrile throughout admission, but because of the new valvular dysfunction, there was a suspicion for infective endocarditis and blood cultures were obtained. The patient was started on broad-spectrum antibiotics for suspected aspiration pneumonia. Transesophageal echocardiogram showed an avulsed and perforated bioprosthetic valve cusp resulting in severe aortic regurgitation and severely elevated transaortic gradients (Figs. 3 and 4).
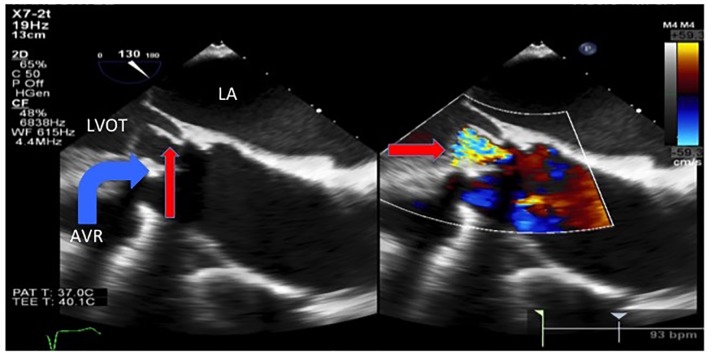
Figure 3.
Transesophageal echocardiogram showed severe intravalvular aortic regurgitation (thin arrow) due to an avulsed and prolapsed non-coronary aortic cusp seen here prolapsing into the aortic annulus during systole with the regurgitant jet of intravalvular aortic regurgitation. LA: left atrium. LVOT: left ventricular outflow tract. AVR: aortic valve replacement.
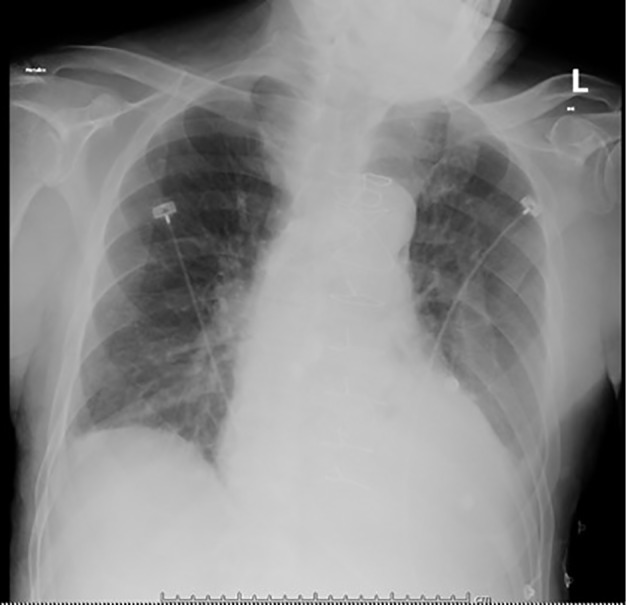
Figure 4.
Transesophageal echocardiogram showed an avulsed and prolapsed non-coronary aortic cusp (thin arrow) seen here prolapsing into the LVOT during diastole with the severe intravalvular aortic regurgitation jet. LA: left atrium. LVOT: left ventricular outflow tract. AVR: aortic valve replacement.
The patient received ceftazidime and metronidazole for suspected aspiration pneumonia. Oxacillin and vancomycin were started when blood cultures began growing gram positive cocci in clusters in four of four bottles. These bacteria were subsequently speciated as S. warneri (minimum inhibitory concentration (MIC) to oxacillin > 4 µg/mL; MIC to vancomycin = 1 µg/mL). The patient refused valve replacement surgery and transarterial valve replacement. He had acute kidney injury, thus gentamicin was not given and rifampin 300 mg orally three times daily was added to the vancomycin for the 6-week treatment course. The patient was discharged to a Skilled Nursing Facility to complete his antibiotic course, after which he was lost to follow-up.
Discussion
There are eight case reports in the English language literature of S. warneri causing endocarditis (Table 2). Cases of native valve endocarditis have involved the aortic, mitral, and pulmonic valves and prosthetic valve endocarditis has involved the aortic valve. S. warneri is capable of causing aortic ring abscesses and valvular destruction so severe that the patients often require valve replacement surgery [4]. Current recommendations for methicillin-resistant coagulase negative staphylococcal prosthetic valve endocarditis are a combination of vancomycin and rifampin for 6 weeks, and gentamicin for the first 2 weeks [9].
Table 2. Review of Previously Published Cases of Staphylococcus warneri Endocarditis.
| Reference | Presenting signs and symptoms | Valve(s) involved (native vs. prosthetic valve) | Presence of vegetation and/or intracardiac abscess on echo or surgical examination |
|---|---|---|---|
| Dan et al (1984) [1] | 32-year-old male with fatigue, anorexia, CP, fever, tachycardia, new diastolic murmur and systolic crescendo-decrescendo murmur | Aortic (native valve) | Vegetation present |
| Wood et al (1989) [2] | 66-year-old male with worsening low back pain, became febrile, XR with vertebral disc prosthesis, disk space narrowing, and end plate destruction of L2-3 | Aortic and Mitral (native valves) |
Vegetations on both valves and aortic valve ring abscess |
| Kamath et al (1992) [3] | 64-year-old male with fevers, subconjunctival hemorrhage, slinter hemorrhages, systolic murmur, and diastolic murmur | Mitral, aortic, and pulmonary valves | Vegetations on all 3 valves |
| Abgrall et al (2001) [8] | 71-year-old male s/p aortic valve replacement 5 days prior, afebrile, no leukocytosis. Blood cultures negative; culture of vegetation tags with S. warneri | Aortic (prosthetic valve) | Vegetation present with suspected aortic valve ring abscess |
| Stollberger et al (2006) [4] | 48-year-old male s/p L4-5 disk prosthesis implantation, with recurrent fevers, night sweats every 3 - 4 months | Aortic (native) | Vegetation present |
| Kini et al (2010) [5] | 78-year-old female with cough, pleural effusions, and bilateral lower extremity edema with clear serous discharge | Mitral (native valve) | Vegetation present |
| Arslan et al (2011) [6] | 43-year-old female with aortic valve replacement 3 years prior with recent prosthetic valve endocarditis due to S. warneri 3 months prior, presented with 20 days of fevers, night sweats | Aortic valve (prosthetic valve) | Vegetation present |
| Bhardwaj et al (2016) [7] | 59-year-old male with history of scalp laceration 2 weeks prior presenting with 3 days of lethargy, abdominal pain, acute kidney injury, and hypotensive, pansystolic murmur | Mitral (native valve) | Vegetations present (two in total) |
| Current case (2017) | 67-year-old male with valve replacement 7 months prior, presenting with chest pain, constitutional symptoms, no documented fever | Aortic (prosthetic valve) | No vegetations or Aortic valve ring abscess |
This case is unique because it highlights that endocarditis caused by relatively low virulence pathogens can present with symptoms that are predominantly non-infectious. CoNS tend to be less virulent bacteria and often require the presence prosthetic material to cause disease [2]. They are adept at forming biofilms and they have fewer numbers and “less aggressive” virulence factors compared to Staphylococcus aureus [10].
While the lack of fever and other signs and symptoms of infection may be due to the low virulence pathogen, host factors may have also been involved in this patient’s atypical presentation. Elderly patients may have “blunted or absent” febrile responses to severe infections in approximately 20-30% of cases [11]. Perhaps a combination of a relatively lower organism virulence, older age, and the absence of vegetations (suggesting a milder case of endocarditis) explains why this patient lacked fever and leukocytosis.
In summary, clinicians should consider endocarditis caused by relatively low virulence organisms such as S. warneri in patients with a prosthetic valve presenting with new CHF or valvular dysfunction even if the patient lacks typical signs of infections such as fever and leukocytosis, especially if the patient is of advanced age.
References
- 1.Dan M, Marien GJ, Goldsand G. Endocarditis caused by Staphylococcus warneri on a normal aortic valve following vasectomy. Can Med Assoc J. 1984;131(3):211–213. [PMC free article] [PubMed] [Google Scholar]
- 2.Wood CA, Sewell DL, Strausbaugh LJ. Vertebral osteomyelitis and native valve endocarditis caused by Staphylococcus warneri. Diagn Microbiol Infect Dis. 1989;12(3):261–263. doi: 10.1016/0732-8893(89)90024-2. [DOI] [PubMed] [Google Scholar]
- 3.Kamath U, Singer C, Isenberg HD. Clinical significance of Staphylococcus warneri bacteremia. J Clin Microbiol. 1992;30(2):261–264. doi: 10.1128/jcm.30.2.261-264.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stollberger C, Wechsler-Fordos A, Geppert F, Gulz W, Brownstone E, Nicolakis M, Finsterer J. Staphylococcus warneri endocarditis after implantation of a lumbar disc prosthesis in an immunocompetent patient. J Infect. 2006;52(1):e15–18. doi: 10.1016/j.jinf.2005.04.016. [DOI] [PubMed] [Google Scholar]
- 5.Kini GD, Patel K, Parris AR, Tang JS. An unusual presentation of endocarditis caused by Staphylococcus warneri. Open Microbiol J. 2010;4:103–105. doi: 10.2174/1874285801004010103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Arslan F, Saltoglu N, Mete B, Mert A. Recurrent Staphylococcus warnerii prosthetic valve endocarditis: a case report and review. Ann Clin Microbiol Antimicrob. 2011;10:14. doi: 10.1186/1476-0711-10-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bhardwaj B, Bhatnagar UB, Conaway DG. An Unusual Presentation of Native Valve Endocarditis Caused by Staphylococcus warneri. Rev Cardiovasc Med. 2016;17(3-4):140–143. doi: 10.3909/ricm0823. [DOI] [PubMed] [Google Scholar]
- 8.Abgrall S, Meimoun P, Buu-Hoi A, Couetil JP, Gutmann L, Mainardi JL. Early prosthetic valve endocarditis due to Staphylococcus warneri with negative blood culture. J Infect. 2001;42(2):166. doi: 10.1053/jinf.2001.0805. [DOI] [PubMed] [Google Scholar]
- 9.Baddour LM, Wilson WR, Bayer AS, Fowler VG Jr, Tleyjeh IM, Rybak MJ, Barsic B. et al. Infective endocarditis in adults: diagnosis, antimicrobial therapy, and management of complications: a scientific statement for healthcare professionals from the American heart association. Circulation. 2015;132(15):1435–1486. doi: 10.1161/CIR.0000000000000296. [DOI] [PubMed] [Google Scholar]
- 10.Becker K, Heilmann C, Peters G. Coagulase-negative staphylococci. Clin Microbiol Rev. 2014;27(4):870–926. doi: 10.1128/CMR.00109-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Norman DC. Fever in the elderly. Clin Infect Dis. 2000;31(1):148–151. doi: 10.1086/313896. [DOI] [PubMed] [Google Scholar]