Abstract
Purpose
The purpose of this study was to compare the visual outcomes and subjective visual quality between bilateral implantation of a diffractive trifocal intraocular lens, Alcon Acrysof IQ® PanOptix® TNFT00 (group A), and blended implantation of an extended depth of focus lens, J&J Tecnis Symfony® ZXR00 with a diffractive bifocal intraocular lens, J&J Vision Tecnis® ZMB00 (group B).
Methods
This prospective, nonrandomized, consecutive, comparative study included the assessment of 40 eyes in 20 patients implanted with multifocal intraocular lens. Exclusion criteria were existence of any corneal, retina, or optic nerve disease, previous eye surgery, illiteracy, previous refractive surgery, high axial myopia, expected postoperative corneal astigmatism of >1.00 cylindrical diopter (D), and intraoperative or postoperative complications. Binocular visual acuity was tested in all cases. Ophthalmological evaluation included the measurement of uncorrected distance visual acuity (UDVA), corrected distance visual acuity (CDVA), uncorrected near visual acuity (UNVA), and uncorrected intermediate visual acuity (UIVA), with the analysis of contrast sensitivity (CS), and visual defocus curve.
Results
Postoperative UDVA was 0.01 and −0.096 logMAR (p<0.01) in groups A and B, respectively; postoperative CDVA was −0.07 and −0.16 logMAR (p<0.01) in groups A and B, respectively; UIVA was 0.14 and 0.20 logMAR (p<0.01) in groups A and B, respectively; UNVA was −0.03 and 0.11 logMAR (p<0.01) in groups A and B, respectively. Under photopic conditions group B had better CS at low frequencies with and without glare.
Conclusion
Both groups promoted good quality of vision for long, intermediate, and short distances. Group B exhibited a better performance for very short distances and for intermediate and long distances ≥−1.50 D of vergence. Group A exhibited a better performance for UIVA at 60 cm and for UNVA at 40 cm.
Keywords: trifocal, multifocal, pseudophakia, cataract
Introduction
The majority of intraocular lenses implanted currently are monofocal, coupled with an increasingly early diagnosis; however, there is a demand from patients, who want to maintain their productivity and daily activities.1
Monofocal intraocular lenses are developed to replace the lens diopter power with a single focal point and are capable of providing good visual function for distance vision. However, pseudophakic patients with monofocal implants ultimately need reading glasses to compensate for the loss of ability to see intermediate or near distances.2–7
Multifocal intraocular lenses were introduced in the 1980s and have the benefit of promoting near and far vision simultaneous and satisfactorily.8,9 However, these initial lenses had the disadvantage of reducing contrast sensitivity (CS) and provoking an ophthalmoscopy more difficult to perform.10 Despite the optical evolution and technology in the manufacture of the lenses, some patients may still present visual discomfort, such as halos, glares and starburst, reduced CS, and unsatisfactory uncorrected distance visual acuity (UDVA); therefore, careful patient selection is crucial to achieve good postoperative results.1,11–13
Acrysof IQ® Panoptix® TFNT00 (Alcon Laboratories, Inc., Fort Worth, TX, USA) is a single-piece, foldable trifocal lens and is a unapodized lens which, theoretically, made this lens more independent of pupil size to generate good quality of near vision, even in lower contrasts.14–16 This lens adds a negative spherical aberration on the anterior face of the lens to compensate for the positive spherical aberration generated by the human cornea. The diffractive zone is in the central portion and occupies 4.5 mm of the optical zone, dividing the light to create an intermediate addition of +2.17 diopters (D) and one near to +3.25 D.17
The Tecnis® ZMB00 lens (Johnson&Johnson Vision, Santa Ana, CA, USA) is a single-piece, bifocal hydrophobic acrylic lens with a posterior diffractive surface and aspheric anterior surface that adds −0.27 μm of spherical aberration to the human eye, presenting an addition of 4 D, corresponding to 3.2 D on the corneal plane.18,19
The Tecnis® Symfony® ZXR00 lens (Johnson&Johnson Vision) is a single-piece, hydrophobic acrylic folding lens with a new design that promotes an extended focus range, it also has a posterior diffractive surface, and the anterior face is aspherical and adds a −0.27 μm spherical aberration to compensate the positive corneal spherical aberration; the concept of extended depth of focus lens (EDOF) promoted by ZXR00 lens can be explained by the splitting of light energy into an elongated focus which could diminish the overlapping of near and far images caused by traditional multifocal IOLs, generating less halos. It also uses a proprietary achromatic diffractive echelette design that corrects the corneal chromatic aberration for enhanced CS.20,26
The purpose of this study was to compare the visual outcomes and CS between the AcrySof IQ Panoptix (trifocal group) and blended implantation of Tecnis Symfony ZXR00 in the dominant eye and Tecnis ZMB00 in the non-dominant eye (mixed EDOF group).
Methods
This study was conducted in accordance with good clinical practices and was approved by the Institutional Review Board of the Medical Staff of Hospital Oftalmológico de Brasília, Brazil.
This was a prospective, consecutive, nonrandomized, comparative study. All patients underwent an uneventful cataract extraction with IOL implant by the same surgeon (WTH) between May 2015 and October 2016. Informed consent was obtained from patients prior to data collection, when the procedures that would be realized during the study were explained to the patients. Analysis and comparison of the visual outcomes and CS were performed between the trifocal and mixed EDOF groups. Ocular dominance was determined by using the Dolman method.
Exclusion criteria were 1) existence of any corneal, 2) retina or optic nerve disease, 3) previous eye surgery, 4) illiteracy, 5) previous refractive surgery, 6) high axial myopia, 7) expected postoperative corneal astigmatism >1.00 D, and 8) intraoperative or postoperative complications.13
The study consisted of a complete preoperative and postoperative visit from 30 to 180 days after surgery for both the groups. All patients underwent complete ophthalmological examination, including biomicroscopy, mesopic and photopic pupillometry appraised by OPD-Scan III (Nidek, Gamagori, Japan), tonometry, retinoscopy, fundoscopy, near, intermediate, and far visual acuity, defocus curve, and CS. The IOL power was chosen on the preoperative visit based on optical biometry with IOL Master 500 (Carl Zeiss AG, Oberkochen, Germany). Uncorrected and corrected near (40 cm), intermediate (60 cm), and far (4 m) binocular visual acuity were measured using the reading table model of the Early Treatment Diabetic Retinopathy Study charts (ETDRS; Vector Vision, Ltd, Greenville, OH, USA). Preoperative visual acuity data were collected from electronic charts records.
The evaluation included testing of binocular CS under photopic (with and without glare) and mesopic conditions using the CSV-1000 chart (Vector Vision, Inc., Greenville, OH, USA) with spatial frequencies ranging between 3 and 18 cycles/degree for photopic conditions, between 1.5 and 12 cycles/degree for mesopic conditions and using the Functional Acuity Contrast Test chart provided by the manufacturer, which consists of columns that grow at different rates of 0.15 log units, which are then converted into base 10 logarithmic units for statistical analysis.
Visual binocular defocus curves were obtained in long-distance visual acuity, corrected using the same ETDRS charts at a distance of 4 m, at intervals of 0.50 spherical diopters from −5.00 to 0.00 D, with the measurement of luminance with Gossen starlite 2 (Gossen, Nürnberg, Germany), photopic conditions were defined as ~85 cd/m2, ambient luminance was defined as inferior to 21.25 lux and mesopic conditions were defined as 3 cd/m2.
Significance was tested using the Tukey, Wilcoxon, Kruskal–Wallis, analysis of variance, and chi-square tests by adjusting to a level of significance of 5% (p<0.05) and using software R version 3.3.2 (Foundation for Statistical Computing, Vienna, Austria).
Results
This study comprised 40 eyes of 20 patients, 14 women (70%) and 6 men (30%). There was homogeneity in the group distribution of lenses regarding age (p=0.462), gender (p=0.411), preoperative CDVA (p=0.0606) (Table 1).
Table 1.
Demographic characteristics of patients by group
| Characteristics | Acrysof IQ Panoptix TFNT00 | Tecnis Symfony ZXR00/Tecnis ZMB00 | p-value |
|---|---|---|---|
| Gender (male/female) | 2/10 | 4/10 | 0.35 |
| Age (years) | 64.2±8.34 (51–75) | 64.4±7.65 (53–80) | 0.93 |
| Pre-CDVA | 0.24±0.18 (0.00–0.54) | 0.16±0.19 (0.00–0.70) | 0.063 |
Notes: Data are shown as mean ± standard deviation (lower bound – upper bound). Acrysof IQ® Panoptix® TFNT00: Alcon Laboratories, Inc., Fort Worth, TX, USA); Tecnis® Symfony® ZXR00 and Tecnis® ZMB00: Johnson&Johnson Vision, Santa Ana, CA, USA.
Abbreviation: Pre-CDVA, preoperative best corrected distance visual acuity.
Postoperative UDVA was better in the mixed EDOF group (−0.096 vs 0.010 logMAR, p=0.0295); this difference was statistically significant (Table 2). Corrected distance visual acuity (CDVA) was better in the mixed EDOF group (−0.16 vs −0.07, p=0.01). There were no statistically significant differences in postoperative data of SE (Table 2).
Table 2.
Descriptive measures for implanted IOL refractive power (diopters), postoperative spherical equivalent, postoperative visual acuities, and mesopic pupillometry for Acrysof IQ Panoptix TFNT00 and Tecnis Symfony ZXR00/Tecnis ZMB00 lenses
| Measurement | TFNT00 (n=20) |
ZXR00/ZMB00 (n=20) |
p-value |
|---|---|---|---|
| Diopters | 22.23±1.51 (20.00–25.50) |
21.00±2.66 (16.50–26.50) |
>0.05 |
| Postoperative UDVA | 0.01±0.04 (−0.04–0.10) |
−0.10±0.15 (−0.30–0.18) |
<0.05* |
| Postoperative UIVA | 0.14±0.05 (0.06–0.22) |
0.20±0.05 (0.14–0.32) |
<0.01* |
| Postoperative UNVA | −0.03±0.04 (−0.1–0.06) |
0.11±0.07 (0.00–0.24) |
<0.01* |
| Postoperative SE | −0.07±0.23 (−0.50–0.25) |
−0.09±0.27 (−0.50–0.50) |
>0.05 |
| Postoperative CDVA | −0.07±0.06 (−0.10–0.16) |
−0.16±0.11 (−0.30–0.12) |
<0.01¥ |
| Pupilometry (mesopic) | 4.78±0.64 (3.50–5.50) |
4.90±0.77 (3.50–6.50) |
>0.05 |
Notes:
ANOVA;
Kruskal–Wallis. Data shown as mean ± SD (min–max). Acrysof IQ® Panoptix® TFNT00: Alcon Laboratories, Inc., Fort Worth, TX, USA); Tecnis® Symfony® ZXR00 and Tecnis® ZMB00: Johnson&Johnson Vision, Santa Ana, CA, USA.
Abbreviations: ANOVA, analysis of variance; CDVA, corrected distance visual acuity; Cyl, cylinder; IOL, intraocular lens; SE, spherical equivalent; Sph, sphere; UDVA, uncorrected distance visual acuity; UIVA, uncorrected intermediate visual acuity; UNVA, uncorrected near visual acuity.
Considering short-distance vision, there was a significant difference in the average short-distance visual acuity, as analyzed with correction for long-distance (uncorrected near visual acuity [UNVA]) between the mixed EDOF and the trifocal groups (0.11 vs −0.03 logMAR, p=0.01), and in the intermediate vision (uncorrected intermediate visual acuity [UIVA]) (0.20 vs 0.14 logMAR, p=0.01). None of the patients required any type of short- or long-distance correction in their everyday life following surgery.
CS under photopic conditions without glare was better at a low frequency (3 and 6 cycles per degree [cpd]) for the mixed EDOF group (p<0.01); however, at high frequencies (12 and 18 cpd), there were no statistically significant differences. Under photopic conditions with glare, the trifocal group performed better at 3 cpd frequency with p=0.0233 and the mixed EDOF performed better at 6 cpd frequency with p=0.036. Under mesopic conditions without glare, the mixed EDOF group exhibited a better behavior for the frequencies of 1.5 (p<0.01), 6 (p=0.0117), and 12 (p<0.01) cpd (Figures 1–3).
Figure 1.
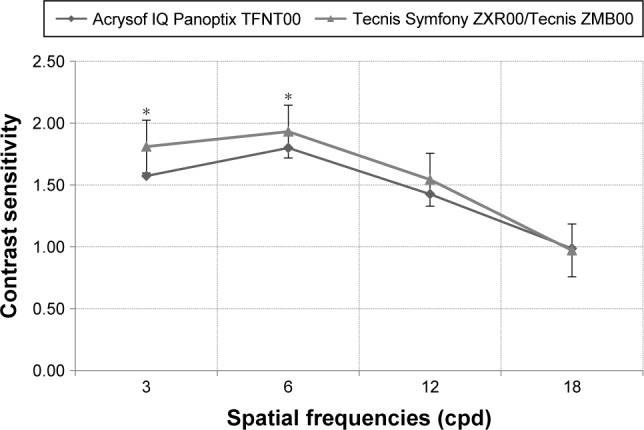
Photopic without glare situation comparison between TFNT00 and ZXR00/ZMB00 lenses.
Notes: *Statistically significant difference (p<0.05). Acrysof IQ® Panoptix® TFNT00: Alcon Laboratories, Inc., Fort Worth, TX, USA); Tecnis® Symfony® ZXR00 and Tecnis® ZMB00: Johnson&Johnson Vision, Santa Ana, CA, USA.
Abbreviation: cpd, cycles per degree.
Figure 2.
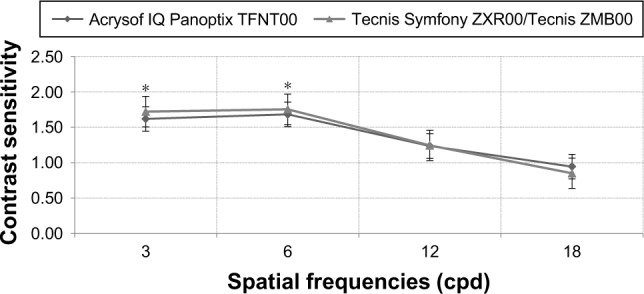
Photopic with glare situation comparison between Acrysof IQ Panoptix TFNT00 and Tecnis Symfony ZXR00/Tecnis ZMB00 lenses.
Notes: *Statistically significant difference (p<0.05). Acrysof IQ® Panoptix® TFNT00: Alcon Laboratories, Inc., Fort Worth, TX, USA); Tecnis® Symfony® ZXR00 and Tecnis® ZMB00: Johnson&Johnson Vision, Santa Ana, CA, USA.
Abbreviation: cpd, cycles per degree.
Figure 3.
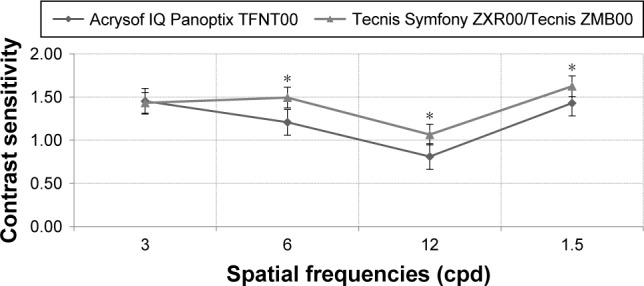
Mesopic without glare situation comparison between Acrysof IQ Panoptix TFNT00 and Tecnis Symfony ZXR00/Tecnis ZMB00 lenses.
Notes: *Statistically significant difference (p<0.05). Acrysof IQ® Panoptix® TFNT00: Alcon Laboratories, Inc., Fort Worth, TX, USA); Tecnis® Symfony® ZXR00 and Tecnis® ZMB00: Johnson&Johnson Vision, Santa Ana, CA, USA.
Abbreviation: cpd, cycles per degree.
Regarding the defocus curve, there was a difference in almost all of the distances assessed between lenses (converted into diopters, p<0.001). The mixed EDOF showed peaks close to −3.0 D (33 cm) and −1.50 D forward, with an average visual acuity of −0.03 and −0.05 logMAR, respectively. At the vergence of 0.00 D, the average visual acuity was −0.16 logMAR. The line corresponding to the trifocal group showed peaks at −2.0 and 0.0 D, with visual acuity of −0.02 and −0.07 logMAR, respectively, and maintaining a plateau near the visual acuity of 0.0 logMAR from −2.50 to −1.50 D. None of the lenses had intermediate deflection vision. Regarding deflection of long-distance vision, the trifocal group occurred at −1.0 D, with a visual acuity of 0.17 logMAR; nevertheless, the mixed EDOF group had no deflection of long-distance vision (Figure 4).
Figure 4.
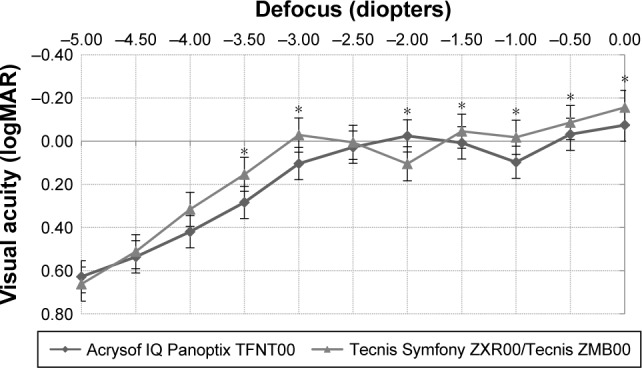
Binocular defocus curve of Acrysof IQ Panoptix TFNT00 and Tecnis Symfony ZXR00/Tecnis ZMB00 lenses, with distance correction in place.
Notes: *Statistically significant difference (p<0.05). Acrysof IQ® Panoptix® TFNT00: Alcon Laboratories, Inc., Fort Worth, TX, USA); Tecnis® Symfony® ZXR00 and Tecnis® ZMB00: Johnson&Johnson Vision, Santa Ana, CA, USA.
Discussion
This is the first study to compare the visual outcomes of a diffractive trifocal intraocular lens with a blend of an EDOF lens and a diffractive bifocal intraocular lens. The group analysis distribution demonstrates homogeneity and enables comparisons between groups, indicating its suitability in comparison with other publications (Table 2).5,6,13,19,21,22
The mixed EDOF group provided successful visual restoration after cataract surgery with excellent visual outcomes across all distances, in accordance with the previous results.21,22 Targeting for micro-monovision (−0.50 to −0.75 of residual myopia in the nondominant eye) seemed to improve UDVA and spectacle independence as well as patient satisfaction with near vision in the Concerto study.21
The good quality of distance and intermediate vision was evidenced in both the groups. The improvement in UDVA for both long and intermediate distances confirmed the efficacy of the treatment and provided independence from glasses in our study, compared to other results.5,21–23 Aforesaid corollary is evident when acknowledging postoperative SE.
Wang et al compared multifocal IOLs with three different additions: group A (+3.00 D), group B (+3.75 D), and group C (+4.00 D) and the highest near-visual peaks were −0.06 logMAR at a vergence of −2.50 D (40 cm) in group A, −0.07 logMAR at −3.00 D (33 cm) in group B, and −0.06 logMAR at −3.50 D (29 cm) in group C.23 Analysis of UNVA highlighted the advantages of the trifocal lens (p<0.01). This statement could be assured on account that the near focal point of ZMB00 is at ~30 cm as the addition of this lens is +4.00 D at the lens plane. Moreover, analysis of UIVA also featured advantages of the trifocal group in comparison with the mixed EDOF (p<0.01). Furthermore, this allegation could be settled with regard to the commencement of ZXR00 elongated focus approximately at −1.50 D of vergence (67.5 cm).21 These results marked a supportive parameter at 20/40, indicating a good range of vision across a wide range of distances in both the groups, especially in the blended group as the interval measured for near and intermediate (40–60 cm) vision within the study does not aim the main foci of any of the lenses of this group.
Considering CS under photopic conditions, the mixed EDOF lenses showed better results at low spatial frequencies (p<0.01). Hida et al compared the SN60D3 IOL to the ZM900 IOL and stated that the ZM900 IOL group had better results at high spatial frequencies, which is applicable to this study since TNFT00 and ZMB00 lenses are the evolution of the SN60D3 and ZM900 IOLs.24 Ye et al compared the ZA9003 (AMO, Santa Ana, CA, USA) with the ZMA00 and stated that the latter one had worse results under photopic conditions, with and without glare, mainly at low special frequencies, similar to our study, when the mixed EDOF group was compared to the trifocal group, under photopic conditions.5 Wang et al made a comparison between a group implanted bilaterally with SN6AD3, a group implanted with BB MF 613 or BB MFM 611 and another group implanted with SN6AD1. The latter group was statistically superior to the first one at a visual angle of 4.0°, under photopic conditions. There was no statistical significance when both the groups were compared under mesopic conditions.23 In our study, CS under photopic conditions without glare was better at a low frequency (3 and 6 cpd) for the mixed EDOF lenses (p<0.01).
It must be deliberated that the mixed EDOF group presented a more emulated behavior to their corresponding monofocal IOL peers at low frequencies, under photopic or mesopic conditions, than the trifocal group.4 ZA9003 IOL has been considered better than the ZMA00 IOL, considering CS.4,5 A phenomenon of similarity could be explained through the analysis of the concept of EDOF promoted by ZXR00 explained previously in this paper.21
Regarding visual defocus curve, it was clear that mixed EDOF group reached two peaks of improved visual acuity corresponding to near (at the vergence of −3.00 D) and intermediate/far distances (at the vergence of −1.50 D, enhancing to reach its highest at 0.00 D). Considering near vision, the mixed EDOF group presented significantly better vision close to −3.00 D of vergence than the trifocal group (p<0.01), nevertheless the triffocal lens demonstrated greater near vision at the vergence of −2.00 D, with statistical significance when compared with the mixed EDOF group at this focal point, in accordance with previous results.21,22,25
When assessing intermediate vision of 60 cm, the mixed EDOF group showed lower performances compared with the trifocal group. Schmickler et al reached similar values when individually assessing the ZMB00 lens.18
Furthermore, analysis of the two IOL defocus patterns suggests that there should be a relative permanence of the curve near the better vision peaks, which indicates a reasonable depth of focus around these two top focal points, mainly in the mixed EDOF group, as it maintain a plateau from −1.50 D enhancing to the top at 0.00 D. In the mixed EDOF group, this phenomenon can also be perceived at the best near focal point at 30 cm, where the reading distance is confined not only at −3.00 D vergence but also at −2.50 D vergence, reaching amplitude around the peak.
Regarding the results of aberrometry, the comparison of both the groups was not statistically significant, which ratify other results in the literature.13,25
The limitations of our study are the small number of eyes included and the absence of a reading speed, which is an important indicator of near visual performance, withal, it was not estimated in the current study. This might also be a limitation in terms of assessing the functional vision.
Another limitation was the elaboration of the defocus curve to reach the infinite, expressed as the vergence of 0.00 D. We did not assess the positive diopters at the defocus curve in this study; therefore, it does not have the power to infer about the tolerability of both the groups to myopic refractive errors postoperatively.
In conclusion, both the groups promoted good quality of vision for long, intermediate, and short distances and had a range of focus, especially in the mixed EDOF group after 67 cm, where it maintained a plateau. This group also recorded better results under photopic and mesopic conditions, at low frequencies, emulating their monofocal peers.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Maxwell WA, Cionni RJ, Lehmann RP, Modi SS. Functional outcomes after bilateral implantation of apodized diffractive aspheric acrylic intraocular lenses with a +3.0 or +4.0 diopter addition power randomized multicenter clinical study. J Cataract Refract Surg. 2009;35(12):2054–2061. doi: 10.1016/j.jcrs.2009.06.041. [DOI] [PubMed] [Google Scholar]
- 2.Nishi T, Taketani F, Ueda T, Ogata N. Comparisons of amplitude of pseudoaccommodation with aspheric yellow, spheric yellow, and spheric clear monofocal intraocular lenses. Clin Ophthalmol Auckl NZ. 2013;7:2159–2164. doi: 10.2147/OPTH.S52771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gundersen KG, Potvin R. Comparative visual performance with mono-focal and multifocal intraocular lenses. Clin Ophthalmol Auckl NZ. 2013;7:1979–1985. doi: 10.2147/OPTH.S52922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yamauchi T, Tabuchi H, Takase K, Ohsugi H, Ohara Z, Kiuchi Y. Comparison of visual performance of multifocal intraocular lenses with same material monofocal intraocular lenses. PLoS One. 2013;8(6):e68236. doi: 10.1371/journal.pone.0068236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ye P-P, Li X, Yao K. Visual outcome and optical quality after bilateral implantation of aspheric diffractive multifocal, aspheric monofocal and spherical monofocal intraocular lenses: a prospective comparison. Int J Ophthalmol. 2013;6(3):300–306. doi: 10.3980/j.issn.2222-3959.2013.03.08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bartol-Puyal F de A, Talavero P, Giménez G, et al. Reading and quality of life differences between Tecnis ZCB00 monofocal and Tecnis ZMB00 multifocal intraocular lenses. Eur J Ophthalmol. 2017;27(4):443–453. doi: 10.5301/ejo.5000925. [DOI] [PubMed] [Google Scholar]
- 7.Liang J-L, Tian F, Zhang H, Teng H. Combination of toric and multifocal intraocular lens implantation in bilateral cataract patients with unilateral astigmatism. Int J Ophthalmol. 2016;9(12):1766–1771. doi: 10.18240/ijo.2016.12.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.el-Maghraby A, Marzouky A, Gazayerli E, Van der Karr M, DeLuca M. Multifocal versus monofocal intraocular lenses. Visual and refractive comparisons. J Cataract Refract Surg. 1992;18(2):147–152. doi: 10.1016/s0886-3350(13)80921-2. [DOI] [PubMed] [Google Scholar]
- 9.Vanderschueren I, Zeyen T, D’heer B. Multifocal IOL implantation: 16 cases. Br J Ophthalmol. 1991;75(2):88–91. doi: 10.1136/bjo.75.2.88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Slagsvold JE. 3M diffractive multifocal intraocular lens: eight year follow-up. J Cataract Refract Surg. 2000;26(3):402–407. doi: 10.1016/s0886-3350(99)00437-x. [DOI] [PubMed] [Google Scholar]
- 11.de Vries NE, Webers CAB, Touwslager WRH, et al. Dissatisfaction after implantation of multifocal intraocular lenses. J Cataract Refract Surg. 2011;37(5):859–865. doi: 10.1016/j.jcrs.2010.11.032. [DOI] [PubMed] [Google Scholar]
- 12.Gundersen KG, Potvin R. Comparison of visual outcomes and subjective visual quality after bilateral implantation of a diffractive trifocal intraocular lens and blended implantation of apodized diffractive bifocal intraocular lenses. Clin Ophthalmol Auckl NZ. 2016;10:805–811. doi: 10.2147/OPTH.S107162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chaves MAPD, Hida WT, Tzeliks PF, et al. Comparative study on optical performance and visual outcomes between two diffractive multifocal lenses: AMO Tecnis ® ZMB00 and AcrySof ® IQ ReSTOR ® Multifocal IOL SN6AD1. Arq Bras Oftalmol. 2016;79(3):171–176. doi: 10.5935/0004-2749.20160050. [DOI] [PubMed] [Google Scholar]
- 14.Mojzis P, Studeny P, Werner L, Piñero DP. Late opacification of a hydrophilic acrylic intraocular lens in Europe. Eur J Ophthalmol. 2016;26(2):e24–e26. doi: 10.5301/ejo.5000704. [DOI] [PubMed] [Google Scholar]
- 15.Mojzis P, Studeny P, Werner L, Piñero DP. Opacification of a hydrophilic acrylic intraocular lens with a hydrophobic surface after air injection in Descemet-stripping automated endothelial keratoplasty in a patient with Fuchs dystrophy. J Cataract Refract Surg. 2016;42(3):485–488. doi: 10.1016/j.jcrs.2016.02.004. [DOI] [PubMed] [Google Scholar]
- 16.Werner L, Stover JC, Schwiegerling J, Das KK. Effects of intraocular lens opacification on light scatter, stray light, and overall optical quality/performance. Invest Ophthalmol Vis Sci. 2016;57(7):3239–3247. doi: 10.1167/iovs.16-19514. [DOI] [PubMed] [Google Scholar]
- 17.Carson D, Xu Z, Alexander E, Choi M, Zhao Z, Hong X. Optical bench performance of 3 trifocal intraocular lenses. J Cataract Refract Surg. 2016;42(9):1361–1367. doi: 10.1016/j.jcrs.2016.06.036. [DOI] [PubMed] [Google Scholar]
- 18.Schmickler S, Bautista CP, Goes F, Shah S, Wolffsohn JS. Clinical evaluation of a multifocal aspheric diffractive intraocular lens. Br J Ophthalmol. 2013;97(12):1560–1564. doi: 10.1136/bjophthalmol-2013-304010. [DOI] [PubMed] [Google Scholar]
- 19.Cillino G, Casuccio A, Pasti M, Bono V, Mencucci R, Cillino S. Working-age cataract patients: visual results, reading performance, and quality of life with three diffractive multifocal intraocular lenses. Ophthalmology. 2014;121(1):34–44. doi: 10.1016/j.ophtha.2013.06.034. [DOI] [PubMed] [Google Scholar]
- 20.Gatinel D, Loicq J. Clinically relevant optical properties of bifocal, trifocal, and extended depth of focus intraocular lenses. J Refract Surg Thorofare NJ 1995. 2016;32(4):273–280. doi: 10.3928/1081597X-20160121-07. [DOI] [PubMed] [Google Scholar]
- 21.Cochener B, Concerto Study Group Clinical outcomes of a new extended range of vision intraocular lens: International Multicenter Concerto Study. J Cataract Refract Surg. 2016;42(9):1268–1275. doi: 10.1016/j.jcrs.2016.06.033. [DOI] [PubMed] [Google Scholar]
- 22.Kaymak H, Höhn F, Breyer DRH, et al. [Functional results 3 months after implantation of an “extended range of vision” intraocular lens] Funktionelle Ergebnisse 3 Monate nach Implantation einer “Extended-Range-of-Vision”. Intraokularlinse Klin Monatsbl Augenheilkd. 2016;233(8):923–927. doi: 10.1055/s-0042-104064. German. [DOI] [PubMed] [Google Scholar]
- 23.Wang M, Corpuz CCC, Fujiwara M, Tomita M. Visual and optical performances of multifocal intraocular lenses with three different near additions: 6-month follow-up. Open Ophthalmol J. 2015;9:1–7. doi: 10.2174/1874364101509010001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hida WT, Motta AFP, Kara-José Júnior N, et al. Comparison between OPD-scan results and visual outcomes of Tecnis ZM900 and Restor SN60D3 diffractive multifocal intraocular lenses. Arq Bras Oftalmol. 2008;71(6):788–792. doi: 10.1590/s0004-27492008000600004. [DOI] [PubMed] [Google Scholar]
- 25.Lee S, Choi M, Xu Z, Zhao Z, Alexander E, Liu Y. Optical bench performance of a novel trifocal intraocular lens compared with a multifocal intraocular lens. Clin Ophthalmol Auckl NZ. 2016;10:1031–1038. doi: 10.2147/OPTH.S106646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.TECNIS_ Symfony Extended Range of Vision IOL, Z310939, Rev. 03 [package insert] Santa Ana, CA: Abbott Medical Optics, Inc; [Accessed February 2, 2017]. Revision date: March 10, 2014. Available from: http://www.tecnisiol.com/eu/tecnis-symfony-iol/files/symfony-dfu.pdf. [Google Scholar]


