Abstract
Posttraumatic stress disorder (PTSD) symptoms are associated with disruptions in both couple functioning and parenting, and limited research suggests that, among military couples, perceptions of couple functioning and parenting stress are a function of both one’s own and one’s partner’s mental health symptoms. However, this work has not been generalized to civilian couples, and little is known about the associations between PTSD symptoms and family adjustment in specific family developmental contexts. We examined PTSD symptoms’ associations with perceived couple functioning and parenting stress within a dyadic context in civilian couples who had participated in a randomized controlled trial of a universal, couple-based transition to parenthood program and at least one member of the couple reported having experienced a Criterion A1 traumatic event. Results of actor-partner interdependence models revealed that parents’ own and partners’ PTSD symptoms were negatively associated with perceived couple functioning; contrary to expectation, the association of partners’ PTSD symptoms with perceived couple functioning was strongest among men who received the intervention. A parent’s own PTSD symptoms were positively associated with parenting stress for both men and women and were unexpectedly strongest for men who received the intervention. Partner PTSD symptoms were also positively associated with increased parenting stress for both men and women. Findings support a dyadic conceptualization of the associations between spouses’ PTSD symptoms and family outcomes during the transition to parenthood and suggest that participating in a couple-based, psychoeducational program during this phase in the family life cycle may be particularly salient for men.
Keywords: PTSD, couples, parents, Family Foundations, transition to parenthood
Research indicates that posttraumatic stress disorder (PTSD; American Psychiatric Association, 2013) symptoms manifest within a family context. PTSD symptoms are associated with intimate relationship discord and aggression, dysfunctional couple communication, partner psychological distress, and parenting impairments (Gewirtz, Polusny, DeGarmo, Khaylis, & Erbes, 2010; Lambert, Engh, Hasbun, & Holzer, 2012; Miller et al., 2013; Taft, Watkins, Stafford, Street, & Monson, 2011). However, little is known about how PTSD symptoms relate to intimate relationship functioning in specific family developmental contexts. For many reasons, including prevention and intervention purposes, it is important to understand how these constructs are related during key developmental transitions in the family life cycle, such as the transition to parenthood, to enhance the well-being of trauma survivors, their partners, and their children.
Exposure to a traumatic event is a common occurrence. Studies of nationally representative samples estimate that, across developmental periods, at least 56–62% of individuals have experienced a traumatic event during their lifetimes (Kessler, Sonnega, Bromet, Hughes, & Nelson, 1995; McLaughlin et al., 2013). A relatively small number of individuals who experience a traumatic event will develop PTSD symptoms of sufficient severity to be diagnosed with the disorder. For example, according to Breslau et al. (1998), the conditional risk of developing PTSD after trauma exposure is 9.2%. However, because even subsyndromal symptoms of PTSD are associated with distress and impairment (McLaughlin et al., 2015; Stein, Walker, Hazen, & Forde, 1997), those whose symptoms are elevated but do not meet diagnostic cutoffs should not be overlooked. Indeed, taxometric analyses indicate that PTSD is best understood as an extreme reaction to traumatic life events rather than as a discrete clinical syndrome, thus warranting conceptualization as a dimensional, rather than categorical, construct (e.g., Broman-Fulks et al., 2006; Ruscio, Ruscio, & Keane, 2002).
With respect to romantic relationship distress and impairment, specifically, cognitive-behavioral interpersonal theory of PTSD (Monson, Fredman, & Dekel, 2010) posits that thoughts, feelings, and behaviors within and between partners contribute to and maintain a link between PTSD symptoms and impaired couple functioning. PTSD-related avoidance of feared memories and situations can deprive couples of opportunities to engage in mutually satisfying behavior exchanges (Dekel & Monson, 2010); emotional numbing symptoms can interfere with intimacy by inhibiting emotional expressiveness (Cook et al., 2004); and, hyperarousal symptoms can increase intimate aggression by amplifying the perception of being under threat from one’s partner (Savarese, Suvak, King, & King, 2001). PTSD symptoms can also disrupt a couple’s ability to function effectively as a co-parental unit, which, in turn, predicts lower relationship satisfaction for both partners (Allen, Rhoades, Markman, & Stanley, 2010).
PTSD symptoms are also related to parenting impairments in military and veteran samples, including poorer perceived parent-child relationship quality (Ruscio, Weathers, King, & King, 2002), lower parenting satisfaction (Gold et al., 2007; Samper, Taft, King, & King, 2004), and greater parenting challenges (Gewirtz et al., 2010). More recently, researchers have examined associations between PTSD symptom severity and parenting stress, defined as distress evoked in response to childrearing experiences (Abidin, 1995; Haskett, Ahern, Ward, & Allaire, 2006). Two studies have documented a positive relation between maternal PTSD symptom severity and parenting stress in high risk urban civilian samples (Ammerman, Putnam, Chard, Stevens, & Van Ginkel, 2012; Chemtob, Gudiño, & Laraque, 2013). Given that parenting stress is prospectively associated with harsh parenting practices (Le, Fredman, & Feinberg, 2017) and that harsh parenting practices such as corporal punishment can be a precursor to the perpetration of child physical abuse (Gershoff, 2002), enhanced understanding of the association between PTSD symptoms and parenting stress may provide opportunities to prevent adverse outcomes for children of parents with trauma-related psychopathology.
Recognizing the inherent interdependence among individuals within a family system (Minuchin, 1985), there is a burgeoning effort to characterize the associations between PTSD symptoms and family outcomes within a dyadic context by modeling one’s couple and parenting outcomes as a function of both one’s own PTSD symptoms and one’s partner’s symptoms. For example, Blow et al. (2013) used the Actor-Partner Interdependence Model (APIM; Kenny, Kashy, & Cook, 2006) to examine service member and spouse alcohol misuse, depressive symptoms, and PTSD symptoms as concurrent predictors of both service member and spouse relationship satisfaction and parenting stress. The authors found a marginally significant negative association between service member PTSD symptom severity and spousal relationship satisfaction and a small, positive association between spousal PTSD symptoms and service members’ parenting stress. However, in all three studies documenting an association between PTSD symptoms and parenting stress (i.e., Ammerman et al., 2012; Blow et al., 2013; Chemtob et al., 2013), PTSD symptoms were not the primary focus of the investigations; thus, it is difficult to discern the magnitude of association between PTSD symptoms and parenting stress (and relationship satisfaction, in the case of Blow et al., 2013) outside the context of comorbid symptoms or conditions (e.g., depression, substance use) that were also included in the models.
Taken together, these findings highlight that PTSD symptoms are associated with poorer family adjustment with respect to both perceived couple functioning and parenting. Nonetheless, there remain unanswered questions about the association between PTSD symptoms and family adjustment within a couple context. With the exception of Blow et al. (2013), whose primary focus was the association between alcohol misuse and family functioning in a military sample, we are not aware of any published studies on the contributions of both partners’ PTSD symptoms to the prediction of each partner’s perception of couple functioning and parenting stress. Thus, it is difficult to determine the extent to which there are both actor effects (i.e., how one’s PTSD symptoms relate to one’s own perceptions of family functioning) and partner effects (i.e., how one’s PTSD symptoms relate to one’s partner’s perceptions of family functioning) in a given sample, particularly civilian samples. Second, as suggested by social structure theory and identity theory, family identity tends to be more salient for women than men, especially during the transition to parenthood (Katz-Wise, Priess, & Hyde, 2010); thus, there may be gender differences in actor and/or partner effects in the association between PTSD symptoms and family functioning during the early parenting years. Third, in most studies of the association between PTSD symptoms and family functioning, the age of the participants’ children is heterogeneous, with some including children who may differ from one another by more than a decade (e.g., Gold et al., 2007; Ruscio et al., 2002). From a translational research perspective, the heterogeneity of family developmental stage (as indexed by child age) in prior studies may complicate the development of couple-based interventions that seek to enhance family functioning among trauma survivors with elevated PTSD symptoms. The focus of parenting tasks and challenges may differ considerably depending on whether the child is an infant who requires a high degree of physical care taking, a late toddler/early preschooler who desires autonomy but possesses relatively immature emotion regulation skills, or an adolescent whose peer relationships are relatively more salient than those with family members but still relies on parents for financial and emotional support.
The transition to parenthood, defined as pregnancy through the first year of a child’s life among primiparous couples, is a potentially valuable developmental period in which to examine the associations between PTSD symptoms and family functioning for a number of reasons. First, given that the transition to parenthood is often considered a high stress period (Doss, Rhoades, Stanley, & Markman, 2009; Shapiro, Gottman, & Carrère, 2000), associations between PTSD symptoms and family functioning may be more salient. Second, as the children of participants are approximately the same age, reduced sample heterogeneity may enhance the ability to detect associations. Third, the transition to parenthood is an especially opportune period for prevention, as dysfunctional co-parenting and parenting patterns have not yet been firmly established, and new parents are uniquely open to guidance, education, and support to enhance family functioning during this period (Feinberg, 2002). This may be also be a time to engage high risk couples who might not otherwise seek care (Petch, Creedy, Halford, Gamble, 2012). Indeed, a number of transition to parenthood programs have demonstrated positive outcomes with respect to couple functioning and parenting, with effects particularly salient for couples identified as being high risk by virtue of individual or relational vulnerabilities (e.g., individual psychopathology or relationship distress; Doss, Cicila, Hsueh, Morrison, & Carhart, 2014; Feinberg & Kan, 2008; Petch, Halford, Creedy, & Gamble, 2012). Insights gleaned from understanding these associations could have important implications for designing interventions to target PTSD symptoms within a family context at the transition to parenthood and/or to prevent parent-child relational impairments and adverse child outcomes associated with parental PTSD symptoms (Lambert, Holzer, & Hasbun, 2014).
The purpose of the current study is two-fold. First, we sought to investigate actor and partner effects for the association between civilian men and women’s PTSD symptoms and perceived couple functioning during the transition to parenthood. Second, we sought to investigate actor and partner effects for the associations between PTSD symptoms and parenting stress within the same context. To this end, we had two hypotheses. Hypothesis 1 is that one’s PTSD symptoms will be negatively associated with one’s perceived couple functioning (actor effect) and one’s partner’s perceived couple functioning (partner effect). Hypothesis 2 is that one’s PTSD symptoms will be positively associated with one’s parenting stress (actor effect) and one’s partner’s parenting stress (partner effect). Given that the current investigation took place within the context of a randomized controlled trial of a transition to parenthood program focused on enhancing heterosexual couples’ ability to work better as a co-parental unit, it was possible that the intervention would buffer the effect of PTSD symptoms on family functioning. Thus, moderation by intervention and gender in the strength of these hypothesized associations was also explored.
Method
Participants and Procedures
Participants were a subsample (N = 250) of heterosexual couples who had participated in a randomized controlled trial (RCT) of Family Foundations (FF; Feinberg et al., 2016; N = 399), a universal, couple-based transition to parenthood program. FF consists of five prenatal and four postnatal sessions focused on strengthening the co-parenting relationship and includes psychoeducation and skills training designed to enhance co-parental conflict resolution and problem-solving, communication, and mutual support strategies. The prenatal classes also included standard childbirth education material. The control condition consisted of mailed written materials pertaining to selecting quality childcare and the stages of child development.
Couples were recruited through childbirth education programs and OB/GYN clinics in or near one of five hospitals in three mid-Atlantic states and one southern state. Couples were included in the RCT (i.e., the parent study) if both members of the couple were 18 years or older, expecting their first child together, and cohabiting. All participants provided written informed consent, and all study procedures were approved by the Institutional Review Board at the Pennsylvania State University. Couples were included in the current study if at least one member of the dyad reported having experienced a Criterion A1 traumatic event (i.e., threat of actual or threatened death or serious injury, or a threat to the physical integrity of self or others) according to the Diagnostic and Statistical Manual for Mental Disorders-4th Edition (DSM-IV; American Psychiatric Association, 2000) and completed the PTSD Checklist - Civilian Version (PCL-C; Blanchard, Jones-Alexander, Buckley, & Forneris, 1996, described below).1 The PCL-C was administered at the second wave of assessment for the RCT, when the couple’s first child was 10 months old. Participants reported a diverse range of index traumatic events, including natural disasters, motor vehicle accidents, sexual assault, childhood sexual abuse, miscarriages, combat/warfare, witnessing family violence, robbery, and stalking. Within the subsample, 140 couples were assigned to the intervention condition and 110 to the control condition. Based on demographic information collected at Wave 1 (approximately 4 months prior to birth), the couples included for the current study were significantly older, had more years of education, and were more likely to be non-Hispanic than were the couples in which neither partner reported having experienced a Criterion A1 traumatic event (ps < .03). They did not differ with respect to annual income or proportions assigned to FF versus the control condition (ps > .10).
At the 10-month assessment, the average age of mothers was 30.92 years (SD = 4.27), and the average age of fathers was 32.81 years (SD = 5.24). On average, participants completed 15.55 years (SD = 1.33) of education, and the median household income was $87,500. Ninety percent of couples were married, and 89% of participants self-identified as non-Hispanic White.
Measures
For all continuous measures, means, standard deviations, and Cronbach’s alphas are reported in Table 1.
Table 1.
Descriptive Statistics for Study Variables
| Name | Intervention Group | Control Group | Total Sample | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Men | Women | Men | Women | Men | Women | |||||||||
| M | SD | M | SD | M | SD | M | SD | M | SD | α | M | SD | α | |
| PTSD | ||||||||||||||
| Reexperiencing | 6.65 | 2.06 | 7.31 | 2.65 | 6.93 | 2.59 | 7.35 | 2.66 | 6.77 | 2.30 | .82 | 7.33 | 2.65 | .83 |
| Effortful Avoidance | 2.86 | 1.24 | 3.13 | 1.49 | 2.93 | 1.24 | 3.09 | 1.50 | 2.89 | 1.24 | .62 | 3.11 | 1.49 | .71 |
| Emotional Numbing | 6.43 | 1.96 | 6.34 | 2.34 | 6.73 | 3.01 | 6.10 | 1.84 | 6.56 | 2.47 | .78 | 6.24 | 2.14 | .79 |
| Hyperarousal | 6.45 | 1.75 | 6.93 | 3.06 | 7.46 | 3.59 | 6.75 | 2.75 | 6.89 | 2.76 | .82 | 6.85 | 2.92 | .85 |
| Total PTSD | 22.41 | 5.34 | 23.70 | 8.05 | 24.04 | 9.22 | 23.24 | 7.43 | 23.13 | 7.33 | .90 | 23.51 | 7.78 | .92 |
| Couple Functioning | ||||||||||||||
| Co-Parenting | 5.24 | .70 | 5.22 | .83 | 5.36 | .64 | 5.23 | .72 | 5.29 | .68 | .85 | 5.2 | .78 | .88 |
| Ineffective Arguing | 23.06 | 2.83 | 22.68 | 3.21 | 23.41 | 2.99 | 22.52 | 3.00 | 23.21 | 2.89 | .90 | 22.6 | 3.11 | .90 |
| Relationship Efficacy | 4.71 | .87 | 4.77 | .76 | 4.71 | .79 | 4.90 | .76 | 4.71 | .83 | .86 | 4.83 | .76 | .86 |
| Marital Quality | 37.07 | 7.88 | 34.16 | 10.20 | 37.95 | 7.61 | 37.26 | 8.53 | 37.45 | 7.76 | .96 | 35.52 | 9.61 | .96 |
| Sexual Satisfaction | 2.24 | 1.0 | 1.98 | 1.07 | 2.26 | 1.04 | 2.07 | 1.11 | 2.25 | 1.02 | .87 | 2.02 | 1.09 | .82 |
| Parenting Stress | ||||||||||||||
| Parental Distress | 1.98 | .61 | 2.11 | .63 | 2.06 | .57 | 2.05 | .73 | 2.02 | .59 | .85 | 2.08 | .67 | .88 |
| Parent-Child | ||||||||||||||
| Dysfunctional Interaction | 1.38 | .42 | 1.39 | .51 | 1.38 | .42 | 1.35 | .43 | 1.38 | .42 | .77 | 1.37 | .47 | .79 |
| Difficult Child | 1.75 | .58 | 1.77 | .63 | 1.72 | .62 | 1.75 | .69 | 1.74 | .60 | .86 | 1.76 | .65 | .86 |
Note. α = Cronbach’s alpha. N ranges from 184 to 245 for men and from 188 to 250 for women.
Trauma exposure
Participants completed a modified version of the Traumatic Life Events Questionnaire (TLEQ; Kubany et al., 2000) to assess their prior exposure to potentially traumatic events. The original 21-item measure was modified in two ways. Participants indicated if each event ever occurred (a dichotomous yes/no response) rather than indicating the number of times each event occurred. Additionally, assessment of similar types of trauma were combined into single items, including 1) abortions and miscarriages, 2) life-threatening illnesses and life-threatening or permanently disabling events for a loved one, 3) assault by caregivers, intimate partners, or acquaintances or strangers, and 4) sexual abuse by individuals of varying ages at varying points in development (originally comprising four items).
PTSD symptom severity
The PCL-C (Blanchard et al., 1996) is a 17-item self-report measure used to assess the severity of DSM-IV symptoms of PTSD experienced in response to the most distressing traumatic event identified on the TLEQ (see above). The PCL-C is a widely used measure that has demonstrated good internal consistency and construct validity. Based on factor analytic studies that support disaggregating the effortful avoidance and emotional numbing symptoms into two distinct clusters (e.g., King, Leskin, King, & Weathers, 1998), four PTSD symptom clusters were examined: Re-experiencing (e.g. “Repeated, disturbing memories, thoughts, or images, of the stressful experience;” 5 items), effortful avoidance (e.g. “Avoiding thinking about or talking about the stressful experience or avoiding having feelings related to it;” 2 items), emotional numbing (e.g. “Feeling emotionally numb or being unable to have loving feelings for those close to you;” 5 items), and hyperarousal (e.g. “Being ‘super-alert’ or watchful or on guard;” 5 items). Participants were asked to rate how much they were bothered by each of the 17 trauma-related symptoms in the past month on a 5-point Likert-type scale (1 = Not at All, 5 = Extremely). Sum scores for each symptom cluster were calculated, with higher scores indicating greater symptom severity (range = 17–56 for men and 17 to 59 for women).
Perceived couple functioning
Relationship satisfaction
The Quality of Marriage Index (Norton, 1983) assesses participants’ relationship satisfaction (e.g., “My relationship with my partner makes me happy”). Five items are rated on a 7-point Likert scale (1 = Very Strongly Disagree, 7 = Very Strongly Agree), and one item is rated on a 10-point Likert-type scale (1 = Unhappy, 10 = Perfectly Happy). Items were summed, with higher scores indicating greater relationship satisfaction.
Relationship efficacy
The Relationship Efficacy Measure (Fincham, Harold, & Gano-Phillips, 2000) includes seven items (e.g., “I am able to do things needed to settle our conflicts.”) rated on a 7-point Likert scale (1 = Strongly Disagree, 7 = Strongly Agree). Mean scores were calculated, with higher scores indicating greater perceived efficacy in one’s relationship.
Conflict communication
The Ineffective Arguing Inventory (Kurdek, 1994) is an 8-item self-report measure used to assess couples’ strategies for resolving relationship conflict (e.g., “Our arguments are left hanging and unresolved.”). All items are rated on a 5-point Likert-type scale (1 = Strongly Disagree, 5 = Strongly Agree) and summed, with higher scores indicating more ineffective arguing.
Sexual satisfaction
Satisfaction with sex and romance was measured with four items rated on a 9-point Likert-type scale (1 = Not Enough, 5 = Just Right, 9 = Too Much). The four items are “Regarding your sex life with your partner, would you say that there is 1) enough sex, 2) cuddling and touching, 3) romance, and 4) passion and excitement?” (Maas, McDaniel, Feinberg, & Jones, 2015). The absolute deviance from the midpoint for each item was calculated and reversed scored, with 0 indicating very dissatisfied (either too little or too much) and 4 indicating very satisfied (just about right). The mean of the four items was used, with higher scores indicating greater satisfaction with sex and romance.
Co-parenting functioning
Co-parenting adjustment was assessed with the 12-item brief version of the Co-parenting Relationship Scale (CRS; Feinberg, Brown, & Kan, 2012; e.g., “My partner and I have the same goals for our child”). All items were rated on a 7-point Likert scale (0 = Not True of Us, 6 = Very True of Us). Mean scores were calculated, with higher scores indicating better co-parenting functioning.
Parenting stress
The Parenting Stress Index-Short Form (PSI-SF; Abidin, 1995) measures three dimensions of parenting stress: parental distress (e.g., “I feel trapped by my responsibilities as a parent;” 12 items), parent-child dysfunctional interactions (e.g., “Sometimes I feel my child doesn’t like me and doesn’t want to be close to me;” 6 items) and perceived difficult child (e.g., “My child makes more demands on me than most children;” 9 items). Nine of the original 36 items were not assessed due to relatively low factor loadings on the corresponding dimensions of parenting stress (Abidin, 1995). All items were rated on a 5-point Likert-type scale (1 = Strongly Agree, 5 = Strongly Disagree), reverse coded, and then averaged within scales. Higher scores indicate greater parenting stress.
Statistical Analyses
First, separate measurement models were tested for the three latent variables reflecting PTSD symptom severity, perceived couple functioning, and parenting stress. A series of structural models were then run to assess actor and partner effects for the associations between PTSD symptoms and couple functioning, as well as to test for moderation by intervention status and gender. The process was repeated for the outcome of parenting stress.
Model estimation
Specifications of measurement and structural models were conducted using Mplus 7 (Muthén & Muthén, 2012). Consistent with the non-clinical nature of the sample, variables were not normally distributed. To account for this, robust maximum likelihood estimation (MLR) was used, which generates standard maximum likelihood estimates using standard errors that are robust to non-normality and missing data (Muthén & Asparouhov, 2002; Yuan & Bentler, 2000). Following Hu and Bentler (1999), good model fit in measurement models was inferred by: (a) a small and non-significant chi-square test, although this can be difficult to achieve with large samples (Bollen & Curran, 2006); (b) the root mean square error of approximation (RMSEA) less than or equal to .06; and (c) the comparative fit index (CFI) and the Tucker-Lewis index (TLI) greater than or equal to .95, with values above .90 indicating acceptable fit (Bollen, 1989; Loehlin, 1998).
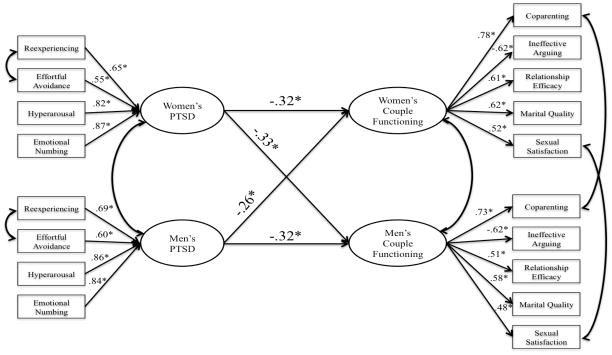
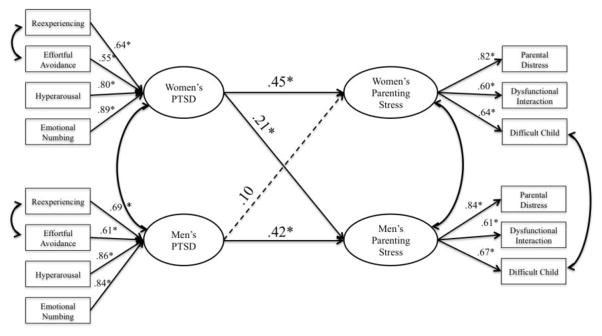
Measurement models
Measurement models were created for PTSD symptom severity, perceived couple functioning, and parenting stress as described above. Within a couple, each corresponding factor (e.g. fathers' and mothers' parenting stress) was permitted to correlate to account for interdependence between members of a dyad. Measurement models were optimized for goodness of fit based on modification indices, such that some indicators were allowed to correlate across gender to account for potential shared method variance (see Figures 1 and 2).
Figure 1.
Actor and partner associations between men’s and women’s PTSD symptom severity and perceived couple functioning.
Note. Standardized parameter estimates are presented. *p < .05. N = 250 dyads.
Figure 2.
Actor and partner associations between men’s and women’s PTSD symptom severity and parenting stress.
Note. Standardized parameter estimates are presented. *p < .05. N = 250 dyads.
Moderation by intervention status (i.e., control versus intervention group) and gender were evaluated by testing each measurement model for factorial invariance across groups. Invariance was assumed in any case where constraining factor loadings to be equivalent between groups did not result in a significant degradation of fit on a chi-square test adjusted for the use of MLR.
Structural models
A series of Actor-Partner Interdependence Models (APIM; Kenny, Kashy, & Cook, 2006) were used to systematically test associations between PTSD symptom severity and each domain of family functioning (perceived couple functioning and parenting stress).
To examine the overall effects of PTSD symptom severity, one initial confirmatory model was fit to the data for all participants predicting each form of family functioning from PTSD symptom severity. This model followed the standard APIM structure, predicting the outcome for each person from both one’s own and one’s partner's PTSD symptom severity. Additional covariances between the two partners' PTSD symptom severities and between their family functioning measures were also modeled. In this first “fully constrained” model, all variances, covariances, and regression loadings were constrained to be the same across the control and intervention groups for both partners.
A sequential model selection approach was taken to test for possible differences between intervention groups and between men and women. In this approach, each step began with a selected baseline model. Parameters from this model were first freed between the intervention and control conditions and then systematically constrained between male and female parents within each condition. A chi-square likelihood ratio test was performed between the new model with those parameters freed or constrained and the selected baseline model. A statistically significant result indicated a difference in the given parameters between groups. Those parameters that differed between groups remained free to vary in all subsequent analyses.
Results
Bivariate associations among latent variables for men and women are presented in Table 2. With the exception of the small correlation between men and women’s PTSD symptoms and a non-significant correlation between men’s PTSD symptoms and women’s parenting stress, correlations among the latent variables were all significant and moderate or large in size.
Table 2.
Correlations among Latent Factors (N = 250 Dyads)
| 1 | 2 | 3 | 4 | 5 | 6 | |
|---|---|---|---|---|---|---|
| 1. Women PTSD | -- | |||||
| 2. Women Couple Functioning | −.37*** | -- | ||||
| 3. Women Parenting Stress | .47*** | −.53*** | -- | |||
| 4. Men PTSD | .23* | -.33*** | .17 | -- | ||
| 5. Men Couple Functioning | −.39*** | .76*** | −.46*** | −.36*** | -- | |
| 6. Men Parenting Stress | .31*** | −.38*** | .39*** | .44*** | −.66*** | -- |
Note. PTSD = posttraumatic stress disorder.
p < .05;
p < .001
Measurement Models
Goodness of fit indices for each of the measurement models are presented in Table 3. With the exception of significant chi-square tests for the PTSD and perceived couple functioning measurement models, there was acceptable to good overall model fit for the measurement models, and measurement invariance was not violated across intervention status (PTSD: χ2(8) = 4.01, p = .86; couple functioning: χ2(10) = 15.74, p = .11; parenting stress: χ2(6) = 6.05, p = .42) or gender (PTSD: χ2(4) = 7.27, p = .12; couple functioning: χ2(4) = 6.96, p = .14; parenting stress: χ2(4) = 6.47, p = .17).
Table 3.
Fit of Measurement and Structural Models (N = 250 Dyads)
| Model | χ2(df) | RMSEA (90% CI) | CFI | TLI |
|---|---|---|---|---|
| Measurement Models | ||||
| PTSD | 40.20* (21) | .060 (.031 – .089) | .96 | .94 |
| Couple Functioning | 60.27* (36) | .054 (.030 – .076) | .95 | .94 |
| Parenting Stress | 11.60 (9) | .034 (.000 – .083) | .99 | .99 |
| Structural Models | ||||
| Couple Functioning | 430.84*(318) | .054 (.040 – .066) | .91 | .91 |
| Parenting Stress | 254.10*(187) | .054 (.035 – .069) | .94 | .94 |
Note.
p < .05.
df = degrees of freedom; RMSEA = Root Mean Square Error of Approximation; CFI = Comparative Fit Index; TLI = Tucker-Lewis Index; Chi-square are adjusted values for the use of robust maximum likelihood (MLR) estimation.
Structural Models: Associations between PTSD and Couple Functioning
Fully Constrained Model
In a model with actor effects, partner effects, and all variances and covariances constrained to be the same across intervention groups, significant actor and partner effects were found for men and women. Effects were in the predicted direction and generally moderate in size (see Figure 1).
Moderation by Intervention Status
Moderation by intervention status was evaluated in two steps. First, the variances and co-variances for the study variables were freed from the fully constrained model. Allowing the variance of men’s PTSD symptom severity to vary across intervention groups resulted in significant improvement in model fit (χ2(1) = 32.7, p < .001). No other variances or covariances yielded significant improvement in fit and therefore remained constrained across intervention groups in all following analyses.
Next, actor and partner effects for men and women were freely estimated for each intervention group. There were no significant differences in actor effects for men or women across intervention conditions, nor were there group differences in the partner effect from men’s PTSD symptoms to women’s perceived couple functioning. However, the partner effect from women’s PTSD symptoms to men’s perceived couple functioning was significantly stronger for couples in FF compared to those in the control condition (χ2(1) = 8.40, p = .004).
Moderation by Gender
Within each intervention group, a model in which actor and partner effects freely varied across gender was compared to a model in which these effects were constrained to be equivalent for men and women. There were no significant gender differences in actor effects in either the FF or control group, nor were there gender differences in partner effects in the control group. However, there was a significant gender difference in partner effects in the FF group such that the association between women’s PTSD symptoms and men’s perceived couple functioning was stronger than the association between men’s PTSD symptoms and women’s perceived couple functioning (χ2(1) = 6.22, p = .013).
Final Model
The final model for perceived couple functioning is presented in Table 4. Because of the intervention group difference in variances in men’s PTSD symptom severity at the latent level, it was not meaningful to compare standardized coefficients for actor and partner effects for the FF and control conditions. Thus, we present raw (unstandardized) coefficients, along with the standard errors of these estimates, to convey similarities and differences in actor and partner effects as a function of intervention group and gender.
Table 4.
Unstandardized Coefficients for the Actor and Partner Associations between PTSD Symptom Severity and Perceived Couple Functioning and between PTSD Symptom Severity and Parenting Stress
| Perceived Couple Functioning
|
||||||
|---|---|---|---|---|---|---|
| Men | Women | |||||
| Effect | B | SE | p-value | B | SE | p-value |
| Intervention | ||||||
| Actor | −.108 | .029 | <.001 | −.108 | .029 | <.001 |
| Partner | −.068 | .031 | .025 | −.152 | .032 | <.001 |
| Control | ||||||
| Actor | −.108 | .029 | <.001 | −.108 | .029 | <.001 |
| Partner | −.068 | .031 | .025 | −.068 | .031 | .025 |
|
| ||||||
| Parenting Stress
|
||||||
| Men | Women | |||||
| B | SE | p-value | B | SE | p-value | |
|
| ||||||
| Intervention | ||||||
| Actor | .286 | .069 | <.001 | .113 | .029 | <.001 |
| Partner | .061 | .024 | .012 | .061 | .024 | .012 |
| Control | ||||||
| Actor | .113 | .029 | <.001 | .113 | .029 | <.001 |
| Partner | .061 | .024 | .012 | .061 | .024 | .012 |
Note. Partner effect refers to the association between one’s PTSD symptom and one’s partner’s family functioning.
Associations between PTSD and Parenting Stress
Fully Constrained Model
In the fully constrained model, significant moderate-sized actor effects were found for both men and women, and a significant small-sized partner effect was found from women’s PTSD symptom severity to men’s parenting stress but not vice versa. All effects were in the predicted direction. Standardized coefficients are presented in Figure 2.
Moderation by Intervention Status
Freely estimating the variances and covariances from the fully constrained model, the variances of men’s PTSD severity and women’s parenting stress at the latent level, and the manifest variable measuring women’s parent-child dysfunctional interaction across intervention groups resulted in significant improvement in model fit (χ2(3) = 55.67, p <.001). Chi-square difference tests indicated no intervention group differences in actor effects for women’s parenting stress or in partner effects for either gender. However, the actor effect from men’s PTSD symptom severity to men’s parenting stress was significantly stronger in the intervention group compared to the control condition (χ2(1) = 12.35, p < .001).
Moderation by Gender
In light of a difference in actor effects for men across the intervention groups, moderation by gender was formally tested within each intervention group separately. There was no evidence of gender differences in actor effects in the control group or in partner effects in either intervention condition. However, there were gender differences in actor effects within FF such that the association between a person's PTSD symptoms and his or her own parenting stress was stronger for men than women (χ2(1) = 11.28, p < .001).
Final Model
The subsequent final model for parenting stress, including the unstandardized coefficients and the standard errors of these estimates, is presented in Table 4.
Discussion
Despite well documented connections between PTSD symptoms and impaired family functioning, there is an absence of published work situating these associations within a family developmental context. Prior work has also tended to focus on military/veteran couples and high risk urban mothers, raising questions about the extent to which previous findings generalize to civilian samples. Further, these associations have not been examined during high stress phases of the family life cycle, such as the transition to parenthood, or, importantly, determined whether couple-based universal transition to parenthood programs mitigate these associations. In addition, few studies have taken into account both actor and partner effects for the association between PTSD symptoms and family adjustment (see Blow et al., 2013, and Miller et al., 2013, for exceptions). The goal of the present study was to address these gaps in the literature by examining the associations of PTSD symptoms with perceived couple functioning and parenting stress within a dyadic context during the transition to parenthood and to explore moderating effects of intervention and gender. As such, it represents the first attempt to characterize these associations in a community sample of couples at the same stage of the family life cycle and to determine whether these patterns of associations differ as a function of gender and participation in an RCT of an empirically supported, couple-based universal transition to parenthood program.
Findings from this sample of relatively high functioning civilian couples unselected for trauma exposure in the parent study and assessed 10 months after birth are comparable to those observed in other, higher risk samples. For example, the magnitude of the actor effects for the association between PTSD symptoms and perceived couple functioning in the present study is on par with that reported in Taft et al.’s (2011) meta-analysis for the association between one’s PTSD symptoms and one’s perception of relationship discord among civilians (r = .31). By comparison, we observed partner effects that are larger than that reported for civilians in Lambert et al.’s (2012) meta-analysis of the association between PTSD symptoms and one’s partners’ perceived relationship quality (r = −.15) but comparable to those observed for the association between PTSD symptoms and partners’ perceived relationship quality in military samples (r = −.26; also see Allen et al., 2010). That similar, or even larger, effect sizes were observed in this relatively low-risk sample may speak to the stressful nature of the early years of parenthood, particularly for individuals with elevated PTSD symptoms and their partners.
Consistent with other studies demonstrating an association between PTSD symptom severity and parenting stress (e.g., Chemtob et al., 2013), actor effects for the relation between one’s PTSD symptom severity and one’s parenting stress in this study were positive and significant but were larger than those reported in other samples. For example, the associations found in the present investigation were twice as large as the bivariate associations reported for these variables in Blow et al.’s (2013) military sample (rs = .22 and .21 for service members and spouses, respectively). Differences could be due to the stress of first time parenting experienced by participants in the current sample. That is, although not reported in Blow et al.’s study, it is possible that participants in that sample had multiple children and were more experienced in navigating the demands and stresses of parenting infants and, therefore, less vulnerable to the impact of PTSD symptoms on their own parenting stress. Being in the military may also have conferred some degree of protection for couples in the Blow et al. (2013) study. Specifically, participants may have felt relatively less isolated and more connected to their (military) community, as couples were recruited from reintegration weekends taking place within 3 months of the service members’ return from deployment. Interestingly, with respect to partner effects, the size and patterns of the effects were comparable to those observed in the Blow et al. study. In both studies, women’s PTSD symptoms predicted men’s parenting stress but not vice versa, suggesting that men may be especially vulnerable to the effects of partners’ psychological distress on their parenting stress. That is, given women’s typical role as the primary caregiver, especially during the early years of child development, it may be particularly stressful for men if they feel obligated to compensate for their partners’ inability to fulfill their parenting responsibilities due to PTSD symptoms.
The current study also extends previous findings by examining intervention and gender differences. First, findings indicated that there was less variability in PTSD symptoms for men in FF compared with those in the control group. However, because PTSD symptoms were not assessed at baseline (i.e., before randomization), it is possible that this difference existed at selection time and thus was not caused by the intervention itself. Although the randomized design of the study suggests a causal explanation, we believe that replication is required before a definitive causal statement can be made. Second, we observed gender differences as a function of intervention status whereby the associations between women’s PTSD symptoms and men’s perceived couple functioning (partner effect) and between men’s PTSD symptoms and their own parenting stress (actor effects) were strongest for men in FF. (That is, these effects were stronger for men in FF than they were for women in the intervention group or for men and women in the control group.) It is possible that FF increased fathers’ attunement to their partners’ psychological states. To the extent that men are more aware of their partners’ PTSD symptoms, they may also be sensitized to the relational comorbidities of the disorder in the form of poorer perceived couple functioning. However, in the absence of psychoeducation about PTSD and its relational context, they may not attribute women’s PTSD-related behaviors (e.g., irritability, feeling distant or cut off from others) to the disorder; instead, they may experience more negative attributions such as partner blame. In addition, the association between PTSD symptoms and parenting stress may have been stronger for fathers in FF as a result of men’s increased involvement in child care. FF emphasizes the co-parenting relationship and the importance of both parents’ engaging with the child. As a result, these effects may have been more salient for men than women because women typically assume the primary caretaking role and are already highly involved in parenting. As such, the intervention may not have increased the degree of women’s involvement with the children to the same extent it did for men. Nonetheless, because we did not hypothesize these associations a priori in the present study, these assertions are speculative until results are replicated in other samples.
Findings from this study have several potentially important clinical implications. First, given the actor and partner effects found for PTSD symptoms’ associations with perceived couple functioning and parenting stress, assessment of both partners’ mental health symptoms during the perinatal period by health care providers may be a valuable investment in the health and well-being of all members of a new family. The transition to parenthood is an opportune time to repair disrupted couple functioning and to improve the psychological health of both members of the couple. Relatedly, to the degree that a healthy co-parenting relationship facilitates healthy parent-child relationships (Feinberg, 2002), it may also be a unique window of opportunity to prevent disruptions in the parent-child relationship and the adverse impacts on children of having parent with PTSD-related psychopathology (Lambert et al., 2014). Second, given that maternal PTSD symptoms are associated with an increased risk of child psychological abuse and child exposure to traumatic events during early childhood (Chemtob et al., 2013), amelioration of parental PTSD symptoms and their associations with family adjustment during the perinatal period has important public health implications for both parents and children alike. Furthermore, our results suggest that expanding the focus to include civilian fathers’ mental health during the transition to parenthood will be important as well.
From a translational perspective, a trauma-informed couple-based approach during the transition to parenthood may be an efficient and effective intervention format for trauma survivors. Couples tend to be most receptive to interventions during this phase of the family life cycle, as it represents the chance for a fresh start and the opportunity to “do right by their kids” (Feinberg, 2002). Such interventions could integrate components of empirically supported transition to parenthood programs focused on strengthening the couple’s relationship and co-parenting alliance (e.g., Doss et al., 2014; Feinberg et al., 2016; Halford, Petch, & Creedy, 2010) with components of empirically supported couple-based treatments for PTSD (Monson et al., 2012; Sautter, Glynn, Cretu, Senturk, & Vaught, 2015). This type of program could also be an important way to involve fathers, as most transition to parenthood programs for parents considered to be high risk by virtue of individual psychopathology (e.g., depression) are focused on mothers.
Findings suggest that focusing exclusively on the co-parenting relationship, with attendant increases in men’s attunement to the impact of their own and their partners’ PTSD symptoms on family functioning, is not sufficient to address the relational comorbidities of PTSD symptoms during this period. Instead, trauma survivors and their partners may require PTSD-specific psychoeducation and concrete skills designed to address the intersection between PTSD symptoms and couple/family functioning during this phase of the family life cycle. For example, providing psychoeducation about how both PTSD symptoms and relationship distress may be amplified as a result of increased demands on both partners and the ways in which this amplification could impact the couple’s parenting alliance may facilitate parents’ ability to make PTSD-relevant attributions for their own and their partners’ behaviors (where applicable); this, in turn, could decrease relationship distress and increase motivation to work together as co-parental unit. Relatedly, activities that involve both parents and the baby (e.g., bathing the baby together, going on outings as a threesome) are likely to decrease PTSD-related avoidance and numbing symptoms while simultaneously promoting positive bonding between partners and between each parent and the child, in addition to strengthening the overall family unit.
There are limitations associated with the current investigation. First, and similar to other studies assessing the association between PTSD symptoms and parenting stress (e.g., Ammerman et al., 2012; Blow et al., 2013; Chemtob et al., 2013), we relied on participants’ self-reported PTSD severity. Measurement of PTSD symptoms via clinician interview could enhance assessment of PTSD symptom severity and diagnosis. Second, this sample consisted of heterosexual couples who were predominantly White, Non-Hispanic and, although demonstrating a wide range of education and income, relatively high mean levels of education and socio-economic status. Findings might differ in populations experiencing more chronic environmental stress, such as couples dealing with ongoing trauma in the form of community violence. Examining these associations in samples that are more diverse with respect to race, ethnicity, sexual orientation, education, socio-economic status, and environmental stressors will be helpful in confirming if the pattern of findings observed in this study generalize to other populations with respect to both actor and partner effects for the associations between PTSD symptoms and family adjustment during this family developmental context.
In sum, findings from the present study demonstrate associations between PTSD symptoms and family impairments for oneself and one’s partner during the transition to parenthood in a community sample unselected for trauma exposure at the time of recruitment into the parent study. This suggests that couple-based interventions for trauma-related psychopathology during the transition to parenthood may be indicated even if participants do not meet formal diagnostic criteria for PTSD. The development of trauma-informed interventions for couples grappling with the effects of PTSD symptoms in one or both partners at this critical juncture in the family life cycle also raises the possibility that treatment may serve as prevention and offers the hope of improved quality of life for trauma survivors, their partners, and their children.
Acknowledgments
This research was supported in part by a grant from the Fran and Holly Soistman Faculty Endowment from the College of Health and Human Development, The Pennsylvania State University to Steffany J. Fredman, a grant from the National Institute of Child Health and Development (HD058529) to Mark E. Feinberg, a grant from the National Center for Advancing Translational Sciences (UL1 TR000127) to the Pennsylvania State University to support Timothy R. Brick’s time, and startup funds from the Pennsylvania State University to Steffany J. Fredman.
Footnotes
Of the 250 couples, 124 (49.6%) consisted of couples in which both experienced a Criterion A1 traumatic event.
Dr. Feinberg created Family Foundations and is the owner of a private company that disseminates the program. Dr. Feinberg’s company has been reviewed by the Institutional Review Board and the Conflict of Interest Committee at the Pennsylvania State University for potential financial gain. The other authors declare no potential conflict of interest.
Results of this study were presented at the 2016 conference for the Association of Behavioral and Cognitive Therapies, New York, NY.
References
- Allen ES, Rhoades GK, Stanley SM, Markman HJ. Hitting home: Relationships between recent deployment, posttraumatic stress symptoms, and marital functioning for army couples. Journal of Family Psychology. 2010;24:280–288. doi: 10.1037/0893-3200.21.4.572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abidin RR. Parenting Stress Index: Professional Manual. 3. Lutz, FL: Psychological Assessment Resources, Inc; 1995. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: Author; 2000. text revision. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5. Arlington, VA: American Psychiatric Publishing; 2013. [Google Scholar]
- Ammerman RT, Putnam FW, Chard KM, Stevens J, Van Ginkel JB. PTSD in depressed mothers in home visitation. Psychological Trauma: Theory, Research, Practice, and Policy. 2012;4:186–195. doi: 10.1037/a0023062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blanchard EB, Jones-Alexander J, Buckley TC, Forneris CA. Psychometric properties of the PTSD Checklist (PCL) Behaviour Research and Therapy. 1996;34:669–673. doi: 10.1016/0005-7967(96)00033-2. [DOI] [PubMed] [Google Scholar]
- Blow AJ, Gorman L, Ganoczy D, Kees M, Kashy DA, Valenstein M, … Chermack S. Hazardous drinking and family functioning in National Guard veterans and spouses postdeployment. Journal of Family Psychology. 2013;27:303–313. doi: 10.1037/a0031881. [DOI] [PubMed] [Google Scholar]
- Bollen KA. Structural equations with latent variables. New York, NY: Wiley; 1989. [Google Scholar]
- Bollen KA, Curran PJ. Latent curve models: A structural equation perspective. Hoboken, New Jersey: John Wiley & Sons; 2006. [Google Scholar]
- Broman-Fulks JJ, Ruggiero KJ, Green BA, Kilpatrick DG, Danielson CK, Resnick HS, Saunders BE. Taxometric investigation of PTSD: Data from two nationally representative samples. Behavior Therapy. 2006;37:364–380. doi: 10.1016/j.beth.2006.02.006. [DOI] [PubMed] [Google Scholar]
- Chemtob CM, Gudiño OG, Laraque D. Maternal posttraumatic stress disorder and depression in pediatric primary care: association with child maltreatment and frequency of child exposure to traumatic events. JAMA Pediatrics. 2013;167:1011–1118. doi: 10.1001/jamapediatrics.2013.2218. [DOI] [PubMed] [Google Scholar]
- Cook JM, Riggs DS, Thompson R, Coyne JC, Sheikh JI. Posttraumatic stress disorder and current relationship functioning among World War II ex-prisoners of war. Journal of Family Psychology. 2004;18:36–45. doi: 10.1037/0893-3200.18.1.36. [DOI] [PubMed] [Google Scholar]
- Dekel R, Monson CM. Military-related post-traumatic stress disorder and family relations: Current knowledge and future directions. Aggression and Violent Behavior. 2010;15:303–309. doi: 10.1016/j.avb.2010.03.001. [DOI] [Google Scholar]
- Doss BD, Rhoades GK, Stanley SM, Markman HJ. The effect of the transition to parenthood on relationship quality: An 8-year prospective study. Journal of Personality and Social Psychology. 2009;96:601–619. doi: 10.1037/a0013969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doss BD, Cicila LN, Hsueh AC, Morrison KR, Carhart K. A randomized controlled trial of brief coparenting and relationship interventions during the transition to parenthood. Journal of Family Psychology. 2014;28:483–494. doi: 10.1037/a0037311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feinberg ME. Coparenting and the transition to parenthood: A framework for prevention. Clinical Child and Family Psychology Review. 2002;5:173–195. doi: 10.1023/a:1019695015110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feinberg ME, Jones DE, Hostetler ML, Roettger ME, Paul IM, Ehrenthal DB. Couple-focused prevention at the transition to parenthood, a randomized trial: Effects on coparenting, parenting, family violence, and parent and child adjustment. Prevention Science. 2016;17:751–764. doi: 10.1007/s11121-016-0674-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feinberg ME, Kan ML. Establishing family foundations: Intervention effects on coparenting, parent/infant well-being, and parent-child relations. Journal of Family Psychology. 2008;22:253–263. doi: 10.1037/0893-3200.22.2.253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fincham FD, Harold GT, Gano-Phillips S. The longitudinal association between attributions and marital satisfaction: Direction of effects and role of efficacy expectations. Journal of Family Psychology. 2000;14:267–285. doi: 10.1037/0893-3200.14.2.267. [DOI] [PubMed] [Google Scholar]
- Gershoff ET. Corporal punishment by parents and associated child behaviors and experiences: A meta-analytic and theoretical review. Psychological Bulletin. 2002;128:539–579. doi: 10.1037//0033-2909.128.4.539. [DOI] [PubMed] [Google Scholar]
- Gewirtz AH, Polusny MA, DeGarmo DS, Khaylis A, Erbes CR. Posttraumatic stress symptoms among National Guard soldiers deployed to Iraq: associations with parenting behaviors and couple adjustment. Journal of Consulting and Clinical Psychology. 2010;78:599–610. doi: 10.1037/a0020571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gold JI, Taft CT, Keehn MG, King DW, King LA, Samper RE. PTSD symptom severity and family adjustment among female Vietnam veterans. Military Psychology. 2007;19:71–81. doi: 10.1080/08995600701323368. [DOI] [Google Scholar]
- Halford WK, Petch J, Creedy DK. Promoting a positive transition to parenthood: a randomized clinical trial of couple relationship education. Prevention Science. 2010;11:89–100. doi: 10.1007/s11121-009-0152-y. [DOI] [PubMed] [Google Scholar]
- Haskett ME, Ahern LS, Ward CS, Allaire JC. Factor structure and validity of the parenting stress index-short form. Journal of Clinical Child and Adolescent Psychology. 2006;35:302–312. doi: 10.1207/s15374424jccp3502_14. [DOI] [PubMed] [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. doi: 10.1080/10705519909540118. [DOI] [Google Scholar]
- Katz-Wise SL, Priess HA, Hyde JS. Gender-role attitudes and behavior across the transition to parenthood. Developmental Psychology. 2010;46:18–28. doi: 10.1037/a0017820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kenny DA, Kashy DA, Cook WL. The analysis of dyadic data. New York: Guilford Press; 2006. [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Archives of General Psychiatry. 1995;52:1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- King DW, Leskin GA, King LA, Weathers FW. Confirmatory factor analysis of the clinician-administered PTSD Scale: Evidence for the dimensionality of posttraumatic stress disorder. Psychological Assessment. 1998;10:90–96. doi: 10.1037/1040-3590.10.2.90. [DOI] [Google Scholar]
- Kubany ES, Haynes SN, Leisen MB, Owens JA, Kaplan AS, Watson SB, Burns K. Development and preliminary validation of a brief broad-spectrum measure of trauma exposure: the Traumatic Life Events Questionnaire. Psychological Assessment. 2000;12:210–224. doi: 10.1037/1040-3590.12.2.210. [DOI] [PubMed] [Google Scholar]
- Kurdeck LA. Conflict resolution styles in gay, lesbian, heterosexual nonparent, and heterosexual parent couples. Journal of Marriage and the Family. 1994;56:705–722. doi: 10.2307/352880. [DOI] [Google Scholar]
- Lambert JE, Engh R, Hasbun A, Holzer J. Impact of posttraumatic stress disorder on the relationship quality and psychological distress of intimate partners: A meta-analytic review. Journal of Family Psychology. 2012;26:729–37. doi: 10.1037/a0029341. [DOI] [PubMed] [Google Scholar]
- Lambert JE, Holzer J, Hasbun A. Association between parents' PTSD severity and children's psychological distress: A meta-analysis. Journal of Traumatic Stress. 2014;27:9–17. doi: 10.1002/jts.21891. [DOI] [PubMed] [Google Scholar]
- Le Y, Fredman SJ, Feinberg ME. Parenting stress mediates the association between negative affectivity and harsh parenting: A longitudinal dyadic analysis. Journal of Family Psychology. 2017 Mar 20; doi: 10.1037/fam0000315. Advance online publication. 20 March 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loehlin JC. Latent variable models: An introduction to factor, path, and structural analysis. Hillsdale, NJ: Erlbaum; 1998. [Google Scholar]
- Maas MK, McDaniel BT, Feinberg ME, Jones DE. Division of labor and multiple domains of sexual satisfaction among first-time parents. Journal of Family Issues. 2015 0192513X15604343. [Google Scholar]
- McLaughlin KA, Koenen KC, Friedman MJ, Ruscio AM, Karam EG, Shahly V, … Kessler RC. Subthreshold posttraumatic stress disorder in the world health organization world mental health surveys. Biological Psychiatry. 2015;77:375–384. doi: 10.1016/j.biopsych.2014.03.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA, Koenen KC, Hill ED, Petukhova M, Sampson NA, Zaslavsky AM, Kessler RC. Trauma exposure and posttraumatic stress disorder in a national sample of adolescents. Journal of the American Academy of Child and Adolescent Psychiatry. 2013;52:815–830. e14. doi: 10.1016/j.jaac.2013.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller MW, Wolf EJ, Reardon AF, Harrington KM, Ryabchenko K, Castillo D, Freund R, Heyman RE. PTSD and conflict behavior between veterans and their intimate partners. Journal of Anxiety Disorders. 2013;27:240–251. doi: 10.1016/j.janxdis.2013.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minuchin P. Families and individual development: Provocations from the field of family therapy. Child Development. 1985;56:289–302. doi: 10.2307/1129720. [DOI] [PubMed] [Google Scholar]
- Monson CM, Fredman SJ, Dekel R. Posttraumatic stress disorder in an interpersonal context. In: Beck JG, editor. Interpersonal processes in the anxiety disorders: Implications for understanding psychopathology and treatment. Washington, DC: American Psychological Association; 2010. pp. 179–208. [Google Scholar]
- Monson CM, Fredman SJ, Macdonald AM, Pukay-Martin ND, Resick PA, Schnurr PP. Effect of cognitive-behavioral couple therapy for PTSD: A randomized controlled trial. Journal of the American Medical Association. 2012;308:700–709. doi: 10.1001/jama.2012.9307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén B, Asparouhov T. Latent variable analysis with categorical outcomes: Multiple-group and growth modeling in Mplus. Mplus Web Notes. 2002;4:1–22. [Google Scholar]
- Muthén LK, Muthén BO. Mplus User’s Guide. 7. Los Angeles, CA: Muthén & Muthén; 1998–2012. [Google Scholar]
- Norton R. Measuring marital quality: A critical look at the dependent variable. Journal of Marriage and the Family. 1983;45:141–151. doi: 10.2307/351302. [DOI] [Google Scholar]
- Petch J, Halford WK, Creedy DK, Gamble J. Couple relationship education at the transition to parenthood: A window of opportunity to reach high-risk couples. Family Process. 2012;51:498–511. doi: 10.1111/j.1545-5300.2012.01420.x. [DOI] [PubMed] [Google Scholar]
- Petch JF, Halford WK, Creedy DK, Gamble J. A randomized controlled trial of a couple relationship and coparenting program (Couple CARE for Parents) for high- and low-risk new parents. Journal of Consulting and Clinical Psychology. 2012;80:662–673. doi: 10.1037/a0028781. [DOI] [PubMed] [Google Scholar]
- Ruscio AM, Ruscio J, Keane TM. The latent structure of posttraumatic stress disorder: A taxometric investigation of reactions to extreme stress. Journal of Abnormal Psychology. 2002;111:290–301. doi: 10.1037//0021-843x.111.2.290. [DOI] [PubMed] [Google Scholar]
- Ruscio AM, Weathers FW, King LA, King DW. Male war-zone veterans' perceived relationships with their children: The importance of emotional numbing. Journal of Traumatic Stress. 2002;15:351–357. doi: 10.1023/a:1020125006371. [DOI] [PubMed] [Google Scholar]
- Samper RE, Taft CT, King DW, King LA. Posttraumatic stress disorder symptoms and parenting satisfaction among a national sample of male Vietnam veterans. Journal of Traumatic Stress. 2004;17:311–315. doi: 10.1023/B:JOTS.0000038479.30903.ed. [DOI] [PubMed] [Google Scholar]
- Sautter FJ, Glynn SM, Cretu JB, Senturk D, Vaught AS. Efficacy of structured approach therapy in reducing PTSD in returning veterans: A randomized clinical trial. Psychological Services. 2015;12:199–212. doi: 10.1037/ser0000032. [DOI] [PubMed] [Google Scholar]
- Savarese VW, Suvak MK, King LA, King DW. Relationships among alcohol use, hyperarousal, and marital abuse and violence in Vietnam veterans. Journal of Traumatic Stress. 2001;14:717–732. doi: 10.1023/a:1013038021175. [DOI] [PubMed] [Google Scholar]
- Shapiro AF, Gottman JM, Carrère S. The baby and the marriage: Identifying factors that buffer against decline in marital satisfaction after the first baby arrives. Journal of Family Psychology. 2000;14:59–70. doi: 10.1037/0893-3200.14.1.59. [DOI] [PubMed] [Google Scholar]
- Stein MB, Walker JR, Hazen AL, Forde DR. Full and partial posttraumatic stress disorder: Findings from a community survey. American Journal of Psychiatry. 1997;154:1114–1119. doi: 10.1176/ajp.154.8.1114. [DOI] [PubMed] [Google Scholar]
- Taft CT, Watkins LE, Stafford J, Street AE, Monson CM. Posttraumatic stress disorder and intimate relationship problems: A meta-analysis. Journal of Consulting and Clinical Psychology. 2011;79:22–33. doi: 10.1037/a0022196. [DOI] [PubMed] [Google Scholar]
- Yuan KH, Bentler PM. Three likelihood-based methods for mean and covariance structure analysis with nonnormal missing data. Sociological Methodology. 2000;30:165–200. doi: 10.1111/0081-1750.00078. [DOI] [Google Scholar]