Abstract
Biological evidence suggests that ethno-racial differences in morning–evening type are possible, whereby Blacks may be more likely to be morning type compared to Whites. However, population-level evidence of ethno-racial difference in morning–evening type is limited. In an earlier study, we reported that morning type was more prevalent in Blacks compared to Whites in the United Kingdom (UK) Biobank cohort (N = 439 933). This study aimed to determine if these ethno-racial differences persisted after accounting for an even broader range of social, environmental and individual characteristics and employing an analytic approach that simulates randomization in observational data, propensity score modeling. Data from UK Biobank participants whose self-identified race/ethnicity was Black/Black British or White; who did not report daytime napping, shift work or night shift work; who provided full mental health information; and who were identified using propensity score matching were used (N = 2044). Each sample was strongly matched across all social, environmental and individual characteristics as indicated by absolute standardized mean differences <0.09 for all variables. The prevalence of reporting nocturnal short, adequate and long sleep as well as morning, intermediate and evening type among Blacks (n = 1022) was compared with a matched sample of Whites (n = 1022) using multinomial logistic regression models. Blacks had a 62% greater odds of being morning type [odds ratio (OR) = 1.620, 95% confidence interval (CI): 1.336–1.964, p < .0001] and a more than threefold greater odds of reporting nocturnal short sleep (OR = 3.453, 95% CI: 2.846–4.190, p < .0001) than Whites. These data indicate that the greater prevalence of morning type and short nocturnal sleep in Blacks compared to Whites is not fully explained by a wide range of social and environmental factors. If sleep is an upstream determinant of health, these data suggest that ethno-racially targeted public health sleep intervention strategies are needed.
Keywords: sleep duration, morning-evening type, chronotype, race, ethnicity
Introduction
Stagnant and widening gaps in health equity between Blacks and Whites persist despite significant efforts to reduce these disparities (DeFranco et al., 2016; U. S. Department of Health and Human Services, 2014). Narrowing this gap requires novel, targeted, population-based approaches that improve social and environmental conditions, as well as individual behavior (Beaudreault, 2015; Heiman & Artiga, 2015). Within this broad framework, sleep has been considered an upstream determinant to health (Grandner et al., 2016).
Several related, yet distinct dimensions of sleep, such as restricted sleep (Buxton et al., 2010; Spiegel et al., 1999), short sleep (Cappuccio et al., 2010; Malone et al., 2016), late chronotype (Merikanto et al., 2013) and irregular sleep times (Taylor et al., 2016; Wong et al., 2015) have been associated with cardio-metabolic diseases. Hypertension is more prevalent in persons reporting short sleep (≤6 h), independent of socioeconomic status (Stranges et al., 2010). Impaired glucose tolerance and reduced resting metabolic rates are caused by restricting sleep to <6 h in healthy adults (Buxton et al., 2010). Both short and restricted sleep have critical implications for Blacks who have been demonstrated to gain more weight and to have higher C-reactive protein associated with these sleep habits than other ethno-racial groups (Grandner et al., 2013; Spaeth et al., 2015). Yet, Blacks are more likely to report short sleep from infancy through adulthood and the prevalence of short sleep in Blacks continues to increase and exceed the prevalence of short sleep reported by Whites (Jean-Louis et al., 2015; Pena et al., 2016). Moreover, social and environmental conditions that contribute to short sleep are more likely borne by Blacks than Whites (e.g. shift work, job-related stress, urban living) (Ertel et al., 2011; Golden, 2001; Jackson et al., 2013). This collective evidence, along with evidence that cardio-metabolic diseases disproportionately impact Blacks (Golden et al., 2012), implies that short sleep and restricted sleep may be contributing factors to ongoing health disparities.
Another dimension of sleep that is associated with health is morning–evening type, or individual preferences for morning or evening activities, including sleep–wake times (Adan et al., 2012). Morning-type persons have earlier sleep–wake times; evening-type persons have later sleep–wake times (Horne & Ostberg, 1976). These differences have important implications for metabolic health, beyond that of sleep duration (Leproult et al., 2014; Merikanto et al., 2013). For example, evening-type persons with type 2 diabetes have poorer glucose control compared to their morning-type counterparts (Reutrakul et al., 2013). This suggests that targeting sleep duration alone may be ineffective in fully mitigating health risks posed by short sleep. Sleep intervention strategies must also be informed by differences in morning–evening type. Yet, little is known about ethno-racial differences in morning–evening type at the population level.
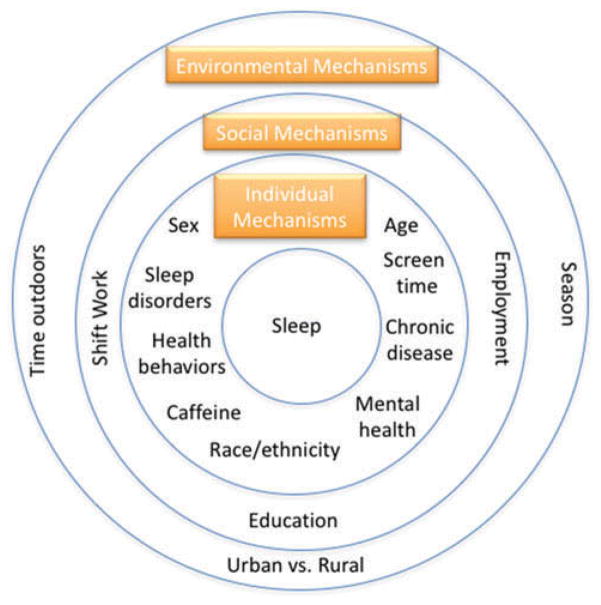
We have reported that morning type is more prevalent in Blacks compared to Whites in the United Kingdom (UK) Biobank cohort (N = 439 933) (Malone et al., 2016). This is congruous with laboratory evidence that Blacks have shorter circadian periods than Whites (Eastman et al., 2012; Smith et al., 2009) because shorter and longer circadian periods are associated with morning and evening types, respectively (Duffy et al., 1999; Jones et al., 1999). Laboratory data also show that exposure to morning light causes Blacks to advance their sleep–wake times three times greater than Whites, whereas exposure to evening light causes Blacks to delay their sleep–wake times only half as much as Whites (Eastman et al., 2015). These ethno-racial differences in circadian periods and light–dark cue responsiveness imply that Blacks may be more likely to have a morning time preference. However, it remains unknown whether this laboratory evidence translates to ethno-racial differences in morning–evening type in community-dwelling adults after accounting for an even broader range of social, environmental and individual characteristics (i.e. Do Blacks have a greater morning sleep timing preference than Whites?). See Figure 1.
Figure 1.
Environmental, social and individual characteristics associated with sleep.
To address this gap, propensity score modeling was used to determine if nocturnal sleep duration and morning–evening type differed in a sample of Black and White adults from the UK Biobank cohort study. Propensity score matching simulates randomization in observational data by making two groups (Blacks and Whites, in this study) as comparable as possible with respect to relevant confounding variables (Williamson & Forbes, 2014). Thus, ethnicity/race (Black versus White) was the independent variable; nocturnal sleep duration and morning–evening type the dependent variables. Blacks and Whites were matched on a broad range of factors known to impact the ability to obtain sleep or to influence sleep–wake timing. This included sociodemographic characteristics (age, sex, attending college, employment) (Dahlgren et al., 2005; Hagen et al., 2016; Hale and Phuong, 2007; Johnson et al., 2016; Lane et al., 2016), environmental characteristics (time outdoors, urban living, season of birth, season of assessment) (Allebrandt et al., 2014; Hale and Phuong, 2007) and individual characteristics (chronic health conditions, smoking, physical activity, caffeine, computer/TV time) (Lane et al., 2016). Should ethno-racial differences in morning–evening type and sleep duration be observed from this rigorous, population-level analysis, there would be a platform to suggest that ethno-racially targeted public health sleep intervention strategies are needed.
Methods
Study design and population
Data from the UK Biobank, a large cohort study, were used for these analyses. From 2006 to 2010, 502 642 adults registered with the National Health Services and living within a 25-mile radius of a UK Biobank assessment center were recruited for baseline assessments. The UK Biobank Project’s methodology, surveys and procedures are available on the UK Biobank Project website (UK Biobank). The UK Biobank approved all protocols and each participant gave an informed consent (UK Biobank). This study was approved by the University of Pennsylvania Institutional Review Board.
Measures
Ethnicity
Participants responded to the touchscreen question “What is your ethnic group?” with one of the following eight options: (1) White (British, Irish or other White background), (2) Black or Black British (Caribbean, African or any other Black background), (3) Asian or Asian British (Indian, Pakistani, Bangladeshi or any other Asian background), (4) Chinese, (5) Mixed (White and Black Caribbean, White and Black African, White and Asian or any other Mixed background), (6) other ethnic group, (7) do not know or (8) prefer not to answer. For this analysis, only participants whose self-identified ethnicity was White or Black/Black British were included.
Nocturnal sleep duration
Sleep duration was assessed with the touchscreen survey item “About how many hours of sleep do you get in every 24 hours? (Please include naps)”. Responses were given as integers and categorized as short (≤6 h), adequate (7–8 h) and long (≥9 h) (Grandner et al., 2014). To align with this categorization for nocturnal sleep duration described by Grandner et al. (2014), we excluded individuals reporting daytime naps. Self-reported sleep duration is correlated with actigraphy-estimated sleep duration (Cespedes et al., 2016; Lauderdale et al., 2008).
Morning–evening type
Morning–evening type was measured by a single touchscreen survey item “Do you consider yourself to be … definitely a morning person, more a morning than evening person, more an evening than a morning person, or definitely an evening person?” Response options included (1) definitely morning (coded as morning), (2) more a morning than evening person (coded as intermediate), (3) more an evening than morning person (coded as intermediate) and, (4) definitely evening (coded as evening). This single question explains the greatest variance in sleep–wake time preferences (Taillard et al., 2004).
Sociodemographic, environmental and individual characteristics associated with sleep duration or morning–evening type were also included. Current sociodemographic characteristics were derived from responses to touchscreen survey questions including (1) age (years), (2) sex (male/female), (3) attended college (coded as yes/no), (4) employment (coded as employed/unemployed/retired), (5) shift work (coded as yes/no) and (6) night shift work (coded as yes/no). Environmental and individual characteristics were derived from responses to touchscreen survey questions including (1) daytime naps (coded as yes/no), (2) insomnia (coded as yes/no), (3) narcolepsy (coded as yes/no), (4) currently smoking (coded as yes/no), (5) caffeine consumption (coded as “no” for decaffeinated coffee, coded as “yes” for instant coffee, ground coffee and other types of coffee), (6) physical activity (minutes per week walking, moderate, vigorous), (7) computer use (h/day), (8) TV (h/day), (9) time spent outdoors in summer (h/day), (10) time spent outdoors in winter (h/day), (11) home density population (coded as urban/rural), (12) season of assessment (spring/summer/winter/fall) and (13) season of birth coded as spring (March, April, May), summer (June, July, August), fall (September, October, November), winter (December, January, February). For all questions, “prefer not to answer” and “do not know responses” were coded as missing. Participants who reported daytime napping, shift work or night shift work were excluded from this analysis.
Participants also responded to several touchscreen survey questions about physical and mental health. Physical health diagnoses queried included hypertension, angina, heart attack, stroke and diabetes (coded as yes/no/don’t know). Measured height and weight was used to calculate body mass index (BMI) (kg/m2) (Keys et al., 1972). Participants with a BMI ≥25 kg/m2 were classified as overweight/obese (Centers for Disease Control and Prevention). Mental health diagnoses queried included bipolar and major depression status (coded as bipolar disorder or depression (yes/no)). Only participants that had full information available to accurately assess their mental health status were included in this analysis. Touchscreen survey questions and response options for each item can be found on the UK Biobank website (UK Biobank).
Data analysis
Cross-sectional data from 502 642 participants were obtained. Participants that provided full mental health information whose self-identified ethnicity was White or Black/Black British and did not report daytime napping, shift work or night shift work were included leaving 53 420 participants in the final sample prior to matching. Continuous variables were described using means and standard deviations, categorical variables as frequencies and percentages.
Several steps were taken to match Black and White participants on a propensity score so that ethno-racial differences in morning–evening type, nocturnal sleep duration and morning–evening type/nocturnal sleep duration combinations could be examined. First, three logistic regression models were used to estimate a propensity score using variables known to be associated with morning–evening type or nocturnal sleep duration. These variables included age, sex, college attendance, employment, insomnia, narcolepsy, current smoking, caffeine intake, physical activity, computer and TV use, time spent outdoors (summer and winter), home density population, season (assessment and birth), bipolar and major depression status, overweight/obesity, comorbidities (diabetes, hypertension, angina, heart attack, stroke) and sleep disorders (narcolepsy, insomnia) for all propensity score-matched analyses. Nocturnal sleep duration was added as a matching variable to test ethno-racial differences in morning–evening type (Model 1). Morning–evening type as added as a matching variable to test ethnic differences in nocturnal sleep duration (Model 2). Nocturnal sleep duration and morning–evening type were both excluded as matching variables to test ethno-racial differences in morning–evening type/nocturnal sleep duration combinations (Model 3).
Second, the propensity scores from the logistic regression models were used to match each Black participant to a White participant with the closest propensity score on a ratio of 1:1 using a nearest neighbor approach with no replacements. Absolute standardized mean differences (ASMDs) were used as a balance statistic for individual covariates, where an ASMD below 0.20 is desirable for all variables (Cohen, 1988).
Third, the association between morning–evening type and ethnicity/race (Model 1), nocturnal sleep duration and ethnicity/race (Model 2) and morning–evening type/nocturnal sleep duration combinations (Model 3) with ethnicity/race were analyzed using multinomial logistic regression models in each appropriate matched sample. These final multinomial logistic regression models were unadjusted as all matching variables demonstrated balance according to the ASMD estimates. To account for multiplicity, statistical significance was considered at the 0.05/3 = 0.017 level (Wright, 1992, December).
Propensity score and matching procedures were conducted using the MatchIt package in R, which required no missing values in the data before matching (Ho et al., 2011). Missingness was 41% for vigorous activity, 22% for moderate activity, 21% for caffeine intake, 13% for college and no more than 1% of the final sample for all other matching variables. In order to deal with missing entries, the mode was replaced for missing categorical variables and the mean for missing continuous variables prior to matching (Little & Rubin, 1987). All other analyses were conducted using SAS 9.4 (SAS Institute Inc., Cary, NC).
Results
Unmatched sample
Baseline characteristics of participants in the unmatched sample
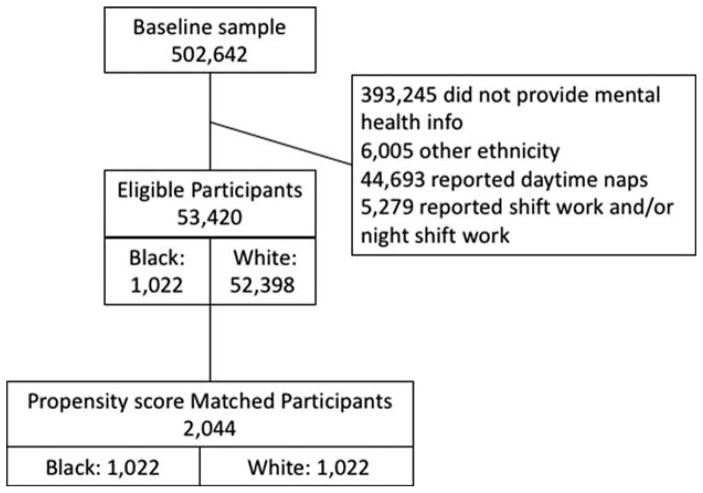
Analyses were restricted to participants reporting White or Black/Black British ethnicity providing full mental health status information and reporting no daytime napping, shift work or night shift work. This reduced the baseline sample from 502 642 to an unmatched sample of 53 420 (see Figure 2). In the unmatched sample, 98% were White with a mean age of 56 (SD = 8) years, 61% were female, 37% attended college and 58% were employed. For nocturnal sleep duration, 24% reported short sleep, 71% reported adequate sleep and 5% reported long sleep. For morning–evening type, 26% reported morning type, 65% reported intermediate type and 8% reported evening type. Table 1 displays all baseline characteristics of the unmatched and matched Black and White participants.
Figure 2.
Flowchart of participants.
Table 1.
Characteristics of unmatched and matched samples.
| Unmatched sample
|
Matched sample
|
||||||
|---|---|---|---|---|---|---|---|
| Total (N = 53 420) | Black (N = 1022) | White (N = 52 398) | Black for all Models (N = 1022) | Model 1: White (N = 1022) | Model 2: White (N = 1022) | Model 3: White (N = 1022) | |
| Age [mean (SD)] | 56.4 (8.1) | 52.0 (7.7) | 56.5 (8.1) | 52.0 (7.7) | 51.8 (8.1) | 51.7 (8.2) | 52.0 (8.1) |
| Sex [N (%)] | |||||||
| Female | 32 506 (60.8) | 701 (68.6) | 31 805 (60.7) | 701 (68.6) | 692 (67.7) | 678 (66.3) | 697 (68.2) |
| Male | 20 914 (39.2) | 321 (31.4) | 20 593 (39.3) | 321 (31.4) | 330 (32.3) | 344 (33.7) | 325 (31.8) |
| Attended college [N (%)] | |||||||
| Yes | 19 549 (36.6) | 403 (39.4) | 19 146 (36.5) | 403 (39.4) | 396 (38.8) | 379 (37.1) | 405 (39.6) |
| No | 33 871 (63.4) | 619 (60.6) | 33 252 (63.5) | 619 (60.6) | 626 (61.2) | 643 (62.9) | 617 (60.4) |
| Employment status [N (%)] | |||||||
| Unemployed | 4130 (7.7) | 151 (14.8) | 3979 (7.6) | 151 (14.8) | 136 (13.3) | 103 (10.1) | 121 (11.8) |
| Retired | 18 256 (34.2) | 135 (13.2) | 18 121 (34.6) | 135 (13.2) | 186 (18.2) | 194 (19.0) | 203 (19.9) |
| Employed | 31 034 (58.1) | 736 (72.0) | 30 298 (57.8) | 736 (72.0) | 700 (68.5) | 725 (70.9) | 698 (68.3) |
| Nocturnal sleep duration [N (%)] | |||||||
| Short (≤6 h) | 12 978 (24.3) | 513 (50.2) | 12 465 (23.8) | 513 (50.2) | 522 (51.1) | 233 (22.8) | 233 (22.8) |
| Adequate (7–8 h) | 37 730 (70.6) | 468 (45.8) | 37 262 (71.1) | 468 (45.8) | 430 (42.1) | 734 (71.8) | 735 (71.9) |
| Long (≥9 h) | 2712 (5.1) | 41 (4.0) | 2671 (5.1) | 41 (4.0) | 70 (6.8) | 55 (5.4) | 54 (5.3) |
| Morning–evening type [N (%)] | |||||||
| Morning | 14 011 (26.2) | 376 (36.8) | 13 635 (26.0) | 376 (36.8) | 274 (26.8) | 391 (38.3) | 278 (27.2) |
| Intermediate | 34 939 (65.4) | 549 (53.7) | 34 390 (65.6) | 549 (53.7) | 648 (63.4) | 524 (51.3) | 633 (61.9) |
| Evening | 4470 (8.4) | 97 (9.5) | 4373 (8.4) | 97 (9.5) | 100 (9.8) | 107 (10.5) | 111 (10.9) |
| Current smoker [N (%)] | |||||||
| Yes | 2943 (5.5) | 73 (7.1) | 2870 (5.5) | 73 (7.1) | 66 (6.5) | 70 (6.8) | 87 (8.5) |
| No | 50 477 (94.5) | 949 (92.9) | 49 528 (94.5) | 949 (92.9) | 956 (93.5) | 952 (93.2) | 935 (91.5) |
| Caffeine [N (%)] | |||||||
| Yes | 45 795 (85.7) | 912 (89.2) | 44 883 (85.7) | 912 (89.2) | 913 (89.3) | 914 (89.4) | 897 (87.8) |
| No | 7625 (14.3) | 110 (10.8) | 7515 (14.3) | 110 (10.8) | 109 (10.7) | 108 (10.6) | 125 (12.2) |
| Computer use (h/day) [mean (SD)] | 1.2 (1.4) | 1.8 (2.0) | 1.2 (1.4) | 1.8 (2.0) | 1.8 (2.2) | 1.8 (2.2) | 1.7 (2.2) |
| TV use (h/day) [mean (SD)] | 2.6 (1.5) | 3.0 (2.1) | 2.6 (1.5) | 3.0 (2.1) | 2.9 (1.7) | 3.1 (2.0) | 3.0 (1.9) |
| Time spent outdoors (h/day) [mean (SD)] | |||||||
| Summer | 3.6 (2.4) | 3.7 (2.7) | 3.6 (2.4) | 3.7 (2.7) | 3.6 (2.6) | 3.7 (2.8) | 3.7 (2.7) |
| Winter | 1.7 (1.7) | 2.0 (2.2) | 1.7 (1.7) | 2.0 (2.2) | 2.0 (2.2) | 2.2 (2.5) | 2.1 (2.4) |
| Physical activity (min/week) [mean (SD)] | |||||||
| Walking | 327.0 (345.8) | 275.3 (291.2) | 328.0 (346.7) | 275.3 (291.2) | 277.9 (276.0) | 271.1 (261.1) | 286.0 (295.5) |
| Moderate | 289.4 (327.3) | 250.0 (281.7) | 290.2 (328.1) | 250.0 (281.7) | 241.6 (264.6) | 250.1 (272.6) | 253.7 (293.6) |
| Vigorous | 136.9 (137.9) | 146.5 (150.5) | 136.7 (137.7) | 146.5 (150.5) | 147.4 (175.8) | 142.3 (152.5) | 146.4 (166.9) |
| Home density [N (%)] | |||||||
| Urban | 45 754 (85.7) | 1016 (99.4) | 44 738 (85.4) | 1016 (99.4) | 1013 (99.1) | 1009 (98.7) | 1015 (99.3) |
| Rural | 7666 (14.3) | 6 (0.6) | 7660 (14.6) | 6 (0.6) | 9 (0.9) | 13 (1.3) | 7 (0.7) |
| Bipolar/major depression status [N (%)] | |||||||
| Yes | 14 032 (26.3) | 211 (20.7) | 13 821 (26.4) | 211 (20.7) | 230 (22.5) | 218 (21.3) | 227 (22.2) |
| No | 39 388 (73.7) | 811 (79.3) | 38 577 (73.6) | 811 (79.3) | 792 (77.5) | 804 (78.7) | 795 (77.8) |
| Overweight/obese [N (%)] | |||||||
| Yes | 33 229 (62.2) | 801 (78.4) | 32 428 (61.9) | 801 (78.4) | 804 (78.7) | 801 (78.4) | 817 (79.9) |
| No | 20 191 (37.8) | 221 (21.6) | 19 970 (38.1) | 221 (21.6) | 218 (21.3) | 221 (21.6) | 205 (20.1) |
| Diabetes [N (%)] | |||||||
| Yes | 1763 (3.3) | 85 (8.3) | 1678 (3.2) | 85 (8.3) | 85 (8.3) | 85 (8.3) | 95 (9.3 |
| No | 51 657 (96.7) | 937 (91.7) | 50 720 (96.8) | 937 (91.7) | 937 (91.7) | 937 (91.7) | 927 (90.7) |
| Hypertension [N (%)] | |||||||
| Yes | 12 664 (23.7) | 346 (33.4) | 12 318 (23.5) | 346 (33.4) | 343 (33.6) | 340 (33.3) | 354 (34.6) |
| No | 40 697 (76.2) | 671 (65.7) | 40 026 (76.4) | 671 (65.7) | 678 (66.3) | 679 (66.4) | 662 (64.8) |
| Don’t know | 59 (0.1) | 5 (0.5) | 54 (0.1) | 5 (0.5) | 1 (0.1) | 3 (0.3) | 6 (0.6) |
| Angina [N (%)] | |||||||
| Yes | 1092 (2.0%) | 21 (2.1) | 1071 (2.0%) | 21 (2.1) | 17 (1.7) | 23 (2.3) | 17 (1.7) |
| No | 52 269 (97.9) | 996 (97.5) | 51 273 (97.9) | 996 (97.5) | 1004 (98.2) | 996 (97.5) | 999 (97.7) |
| Don’t know | 59 (0.1) | 5 (0.5) | 54 (0.1) | 5 (0.5) | 1 (0.1) | 3 (0.3) | 6 (0.6%) |
| Heart attack [N (%)] | |||||||
| Yes | 763 (1.4) | 15 (1.5%) | 748 (1.4%) | 15 (1.5%) | 18 (1.8%) | 11 (1.1%) | 11 (1.1%) |
| vNo | 52 598 (98.5) | 1002 (98.0) | 51 596 (98.5) | 1002 (98.0) | 1003 (98.1) | 1008 (98.6) | 1005 (98.3) |
| Don’t know | 59 (0.1) | 5 (0.5) | 54 (0.1) | 5 (0.5) | 1 (0.1) | 3 (0.3) | 6 (0.6) |
| Stroke [N (%)] | |||||||
| Yes | 581 (1.1) | 8 (0.8) | 573 (1.1) | 8 (0.8) | 6 (0.6) | 6 (0.6) | 9 (0.9) |
| No | 52 780 (98.8) | 1009 (98.7) | 51 771 (98.8) | 1009 (98.7) | 1015 (99.3) | 1013 (99.1) | 1007 (98.5) |
| Don’t know | 59 (0.1) | 5 (0.5) | 54 (0.1) | 5 (0.5) | 1 (0.1%) | 3 (0.3) | 6 (0.6) |
| Narcolepsy [N (%)] | |||||||
| Yes | 291 (0.5) | 20 (2.0) | 271 (0.5) | 20 (2.0) | 17 (1.7) | 23 (2.3) | 16 (1.6) |
| No | 53 129 (99.5) | 1002 (98.0) | 52 127 (99.5) | 1002 (98.0) | 1005 (98.3) | 999 (97.7) | 1006 (98.4) |
| Insomnia [N (%)] | |||||||
| Yes | 13 992 (26.2) | 221 (21.6) | 13 771 (26.3) | 221 (21.6) | 212 (20.7) | 231 (22.6) | 216 (21.1) |
| No | 39 428 (73.8) | 801 (78.4) | 38 627 (73.7) | 801 (78.4) | 810 (79.3) | 791 (77.4) | 806 (78.9) |
| Season of birth [N (%)] | |||||||
| Spring | 14 251 (26.7) | 277 (27.1) | 13 974 (26.7) | 277 (27.1) | 270 (26.4) | 260 (25.4) | 287 (28.1) |
| Summer | 13 557 (25.4) | 241 (23.6) | 13 316 (25.4) | 241 (23.6) | 244 (23.9) | 258 (25.2) | 237 (23.2) |
| Fall | 12 634 (23.7) | 240 (23.5) | 12 394 (23.6) | 240 (23.5) | 257 (25.2) | 243 (23.8) | 250 (24.5) |
| Winter | 12 978 (24.3) | 264 (25.8) | 12 714 (24.3) | 264 (25.8) | 251 (24.6) | 261 (25.5) | 248 (24.3) |
| Season of assessment [N (%)] | |||||||
| Spring | 13 919 (26.1) | 304 (29.8) | 13 615 (26.0) | 304 (29.8) | 265 (25.9) | 284 (27.8) | 264 (25.8) |
| Summer | 15 913 (29.8) | 214 (20.9) | 15 699 (29.9) | 214 (20.9) | 233 (22.8) | 261 (25.5%) | 267 (26.1) |
| Fall | 14 522 (27.2) | 266 (26.0) | 14 256 (27.2) | 266 (26.0) | 323 (31.6) | 304 (29.8) | 298 (29.2) |
| Winter | 9066 (17.0) | 238 (23.3) | 8828 (16.9) | 238 (23.3) | 201 (19.7) | 173 (16.9) | 193 (18.9) |
Matched sample
Characteristics of participants in the matched samples
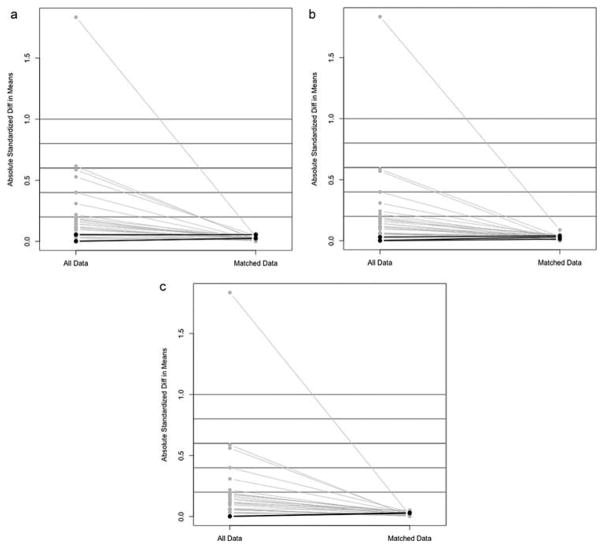
Each propensity score-matched sample included 2044 participants (1022 Blacks, 1022 Whites). The final sample of 1022 Blacks was matched to 1022 Whites with a similar propensity score for each appropriate model (Model 1: not matched on morning–evening type, Model 2: not matched on nocturnal sleep duration, Model 3: morning–evening type/nocturnal sleep duration combination). Before matching, there were differences in the proportion of Blacks and Whites across all morning–evening and nocturnal sleep duration categories (see Table 1 Unmatched sample). To obtain closely matched samples for each model, 2875 different White participants were matched to 1022 Black participants. Although the number of White participants that were the same for all three models was low (0.4%), the descriptive statistics in Table 1 do not suggest that these different participants were very different from one another and excellent matching was achieved by using this approach. In sum, Blacks and Whites were balanced on all baseline characteristics for each appropriate model after matching (see Table 1 Matched sample). In the matched samples, all ASMD estimates were below 0.09 indicating Blacks and Whites were well-matched. See Figure 3A–3C. Please note that an ASMD below 0.20 is an indicator of balance between groups (Cohen, 1988).
Figure 3.
A – Absolute standardized mean differences for Model 1 (not matched on morning–evening type). B – Absolute standardized mean differences for Model 2 (not matched on sleep duration). C – Absolute standardized mean differences for Model 3 (not matched on morning–evening type or sleep duration).
Association between morning–evening type and ethnicity/race in the matched sample (Model 1)
After matching on variables associated with morning–evening type (including nocturnal sleep duration), morning type was reported by 36.8% Blacks and 26.8% Whites; intermediate type was reported by 53.7% Blacks and 63.4% Whites; and evening type was reported by 9.5% Blacks and 9.8% Whites. Compared to Whites, Blacks had a 62% increased odds of being a morning than an intermediate type [odds ratio (OR) = 1.620, 95% confidence interval (CI): 1.336–1.964, p < .0001]. No significant ethnic differences between intermediate and evening types were observed after matching (Table 2).
Table 2.
Multinomial logistic regression models for morning–evening type, nocturnal sleep duration and morning–evening type nocturnal sleep duration combinations for a matched sample of Black and White participants (N = 2044).
| OR (95% CI) | p Value | |
|---|---|---|
| Model 1: Morning–evening type | ||
| Morning | 1.620 (1.336–1.964) | <.0001 |
| Intermediate | REFERENCE | |
| Evening | 1.145 (0.847–1.548) | 0.3791 |
| Model 2: Nocturnal sleep duration | ||
| Short (≤6 h) | 3.453 (2.846–4.190) | <.0001 |
| Adequate (7–8 h) | REFERENCE | |
| Long (≥9 h) | 1.169 (0.768–1.781) | 0.4666 |
| Model 3: Morning–evening type/nocturnal sleep duration combinations | ||
| Morning type | ||
| Short sleep (≤6 h) | 4.596 (3.381–6.248) | <.0001 |
| Adequate sleep (7–8 h) | 1.627 (1.260–2.102) | 0.0002 |
| Long sleep (≥9 h) | 1.484 (0.736–2.992) | 0.2700 |
| Intermediate type | ||
| Short sleep (≤6 h) | 3.676 (2.831–4.774) | <.0001 |
| Adequate sleep (7–8 h) | REFERENCE | |
| Long sleep (≥9 h) | 1.425 (0.816–2.487) | 0.2132 |
| Evening type | ||
| Short sleep (≤6 h) | 3.358 (2.171–5.194) | <.0001 |
| Adequate sleep (7–8 h) | 0.738 (0.467–1.166) | 0.1928 |
| Long sleep (≥9 h) | 0.594 (0.119–2.961) | 0.5247 |
OR: odds ratio; CI: confidence interval
Association between nocturnal sleep duration and ethnicity/race in the matched sample (Model 2)
After matching on variables associated with sleep duration (including morning–evening type), nocturnal short sleep was reported by 50% Blacks and 23% Whites, nocturnal adequate sleep was reported by 46% Blacks and 72% Whites and nocturnal long sleep was reported by 4% Blacks and 5% Whites. Compared to Whites, Blacks had a more than threefold increased odds of reporting nocturnal short than adequate sleep (OR = 3.453, 95% CI: 2.846–4.190, p < .0001). No significant ethnic differences between nocturnal adequate and long sleep were observed after matching (Table 2).
Associations between morning–evening type/nocturnal sleep duration groups and ethnicity/race in the matched sample (Model 3)
Across all morning–evening preferences, Blacks had a greater odds of reporting nocturnal short sleep than Whites. Compared to Whites, Blacks had over a fourfold increased odds of reporting morning type/nocturnal short sleep, (OR = 4.596, 95% CI: 3.381–6.248, p < 0.001), an almost fourfold increased odds of reporting intermediate type/nocturnal short sleep (OR = 3.676, 95% CI 2.831–4.774, p < 0.001) and an over a threefold increased odds of reporting evening type/nocturnal short sleep (OR = 3.358, 95% CI 2.171–5.194, p < 0.001) combinations than intermediate type/nocturnal adequate sleep combinations. Compared to Whites, Blacks also had a 63% increased odds of reporting morning type/nocturnal adequate sleep (OR = 1.627, 95% CI: 1.260–2.102, p = 0.0002) than intermediate type/nocturnal adequate sleep combinations (Table 2).
Discussion
This study investigated ethno-racial differences in nocturnal sleep duration and morning–evening type in a population sample of Black and White adults across sociodemographic, environmental and individual characteristics known to contribute to variation in sleep duration and morning–evening type. The novel finding was that morning type was significantly more prevalent in Blacks compared to Whites in this fully matched population sample. As expected, nocturnal short sleep was more prevalent in Blacks than Whites across all morning–evening categories. Blacks report greater morning-type preferences than Whites. Greater prevalence of morning type reported by Blacks compared to Whites at the population level corroborates our earlier finding (Malone et al., 2016) and extends it by showing that this relationship is retained even when the Black and White cases in the analytic sample are strongly matched for sociodemographic, environmental and individual factors. The implication of this finding is that Black and White differences in morning–evening type cannot be attributed to these external variables, and perhaps give rise to greater consideration of biological hypotheses. Such biological hypotheses may consider the mechanisms of circadian periods and genetic factors. Shorter circadian periods in Blacks compared to Whites have been reported (Eastman et al., 2012, 2015; Smith et al., 2009), which would converge with the current data showing Blacks more likely to be morning type. While we relied on self-reports to determine ethno-racial groups in this study, some of these earlier studies relied on genetic ancestry (Eastman et al., 2015). In our sample, Black participants self-reported their ethnic backgrounds as Caribbean (71%), African (27%) and other Black ethnicity (2%); White participants self-reported their ethnic backgrounds as British (91%), Irish (4%) and other White ethnicity (5%). Thus, our participants’ ethnic backgrounds may differ from the sub-Saharan African ethnicity and European ethnicity determined using genetic ancestry of participants in earlier studies (Eastman et al., 2015). However, genetic correlates of morning–evening type have been reported near core circadian clock and light sensing pathways that influence sleep timing in persons with European ancestry (Hu et al., 2016; Lane et al., 2016). The extent to which these genetic variants may relate to ethno-racial differences in morning–evening type is not yet known.
Blacks report shorter nocturnal sleep than Whites
Self-reported short nocturnal sleep was more prevalent in Blacks than Whites in this strongly matched sample of Black and White adults. These findings converge with earlier studies demonstrating attenuated but persistent shorter sleep in Blacks than Whites after accounting for socioeconomic factors (e.g. income, education, employment, household living conditions) (Cunningham et al., 2015; Krueger & Friedman, 2009; Nunes et al., 2008; Stamatakis et al., 2007). Our data imply that shorter nocturnal sleep in Blacks compared to Whites is not fully explained by a wide range of social and environmental factors.
Our findings are inconsistent with evidence that ethno-racial differences in sleep duration dissolve after accounting for social and environmental factors. These differences may stem from a more nuanced relationship between race/ethnicity and sleep than previously considered. Gamaldo et al. (2015) reported that Blacks were not more likely to report short sleep than Whites when urban neighborhood characteristics, such as graffiti, drug dealers and gang violence, were considered. Jackson et al. (2013) reported that higher educational attainment and greater professional responsibility was associated with longer sleep in Whites, but shorter sleep in Blacks. These differences suggest that perceived discrimination and limited social support for Blacks in higher socioeconomic positions may underlie sleep disparities (Tomfohr et al., 2012). Aggregated measures, such as urban versus rural living, may fail to capture a more nuanced relationship between socioeconomic status and sleep. This may include vast differences in urban neighborhoods, such as exposure to violence, or individual perceptions, such as feelings of safety (Gamaldo et al., 2015). Advancing this work at the population level includes identifying better estimates to capture nuanced relationships between race/ethnicity, sleep and social determinants of sleep, as well as determining whether Blacks reporting short sleep are sleep deprived.
Blacks report short nocturnal sleep across all morning–evening-type preferences
Across all morning–evening-type categories, Blacks were more likely to report nocturnal short sleep than Whites. Compared to Whites, morning type/nocturnal short sleep, intermediate type/nocturnal short sleep and evening type/nocturnal short sleep were more prevalent in Blacks compared to intermediate type/nocturnal adequate sleeping. Relative to Whites, Blacks were also more likely to report morning type/nocturnal adequate sleep compared to intermediate type/nocturnal adequate sleep. To our knowledge this is the first report of ethno-racial differences in morning–evening type/nocturnal sleep duration combinations and underscores the greater prevalence of morning type, as well as short nocturnal sleep among Blacks compared to Whites. Hu et al. (2016) reported morning persons of European ancestry are less likely to require >8 h of sleep per day and are less likely to sleep soundly, albeit these associations have not been generalized to other ethno-racial groups.
The current study findings have implications for informing population level health disparity research. It is well documented that Blacks have earlier chronic disease onset, greater disease severity and shorter life expectancy than Whites (Anderson et al., 2008; Arias, 2007; Bibbins-Domingo et al., 2009; Hertz et al., 2005). A plethora of previous work has also consistently demonstrated that adequate sleep duration and morning type is associated with better health behaviors (Kanerva et al., 2012; Lakerveld et al., 2016; Patterson et al., 2016) and outcomes (Anujuo et al., 2015; Jackowska & Steptoe, 2015; Merikanto et al., 2013). That Blacks are significantly more likely than Whites to be morning type, but less likely to have adequate sleep duration, suggests a complex paradigm between race/ethnicity, sleep and health. It may be that Blacks fail to reap the health benefits associated with morning type that have been widely reported by ourselves and others because of nuanced differences in social and environmental factors that interfere with early sleep onsets (e.g. polluted sleep environments, multiple jobs, job-related stress, discrimination). Important steps for advancing this work include exploring ethno-racial differences in sleep related to more nuanced social and environmental factors.
Data from the current study should be interpreted with consideration of several study limitations. Our findings are limited by the cross-sectional nature of these data. Hence, causation cannot be inferred. Our original sample size was significantly reduced after excluding persons reporting daytime naps, shift work/night shift work and missing mental health status data. However, a sample size of 2044 participants is one of the largest studies to examine ethno-racial differences in morning–evening type. While we were interested in estimating ethno-racial differences in nocturnal sleep duration, future work should determine if there are ethno-racial differences in daytime napping. Other limitations include the self-reported nature of these data, particularly morning–evening type and sleep duration. Moreover, participants were asked to respond to one sleep duration question that did not differentiate between workday and free day sleep. It has been reported that evening types have shorter workday sleep durations and longer free day sleep durations. Thus, responding to one question about sleep duration may have biased sleep duration self-reports, particularly in evening type.
Despite the aim of the morning–evening-type question to assess morning–evening preference, responses may have been influenced by other lifestyle factors, such as occupational demands. Hence, restricted work schedules impacting one’s adherence to preferred morningness or eveningness may have led to misclassification for some persons. Finally, we could not account for certain factors such as individual perceptions of neighborhoods or violence within communities which may differ by race and may not be fully captured by aggregated data, such as income and educational attainment.
Despite these limitations, these epidemiological data support ethno-racial differences in morning–evening type, an issue that remains understudied but is important for optimizing sleep and may play a role in advancing health equity. These data continue to support greater prevalence of self-reported short sleep by Blacks compared to Whites. Designing approaches that capitalize on the increased prevalence of morning type reported by Blacks and the potential health benefits typically associated morning-type persons may be a particularly novel step toward achieving health equity.
Acknowledgments
Funding
This research was conducted using the UK Biobank Resource (application 3474). This work was supported by the Robert Wood Johnson Health and Society Scholars program at the University of Pennsylvania under grant number 69251 (AH), the National Institutes of Health under grant T32 HL 7953 (SKM), the Institutional Development Award (IDeA) Center of Biomedical Research Excellence from the National Institute of General Medical Sciences of the National Institutes of Health under grant number P20GM113125 (FP), the University of Pennsylvania’s University Research Foundation (AH) and the University of Delaware’s Research Foundation (FP).
Footnotes
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this article.
References
- Adan A, Archer SN, Hidalgo MP, et al. Circadian typology: A comprehensive review. Chronobiol Int. 2012;29:1153–75. doi: 10.3109/07420528.2012.719971. [DOI] [PubMed] [Google Scholar]
- Allebrandt KV, Teder-Laving M, Kantermann T, et al. Chronotype and sleep duration: The influence of season of assessment. Chronobiol Int. 2014;31:731–40. doi: 10.3109/07420528.2014.901347. [DOI] [PubMed] [Google Scholar]
- Anderson WF, Rosenberg PS, Menashe I, et al. Age-related crossover in breast cancer incidence rates between black and white ethnic groups. J Natl Cancer Inst. 2008;100:1804–14. doi: 10.1093/jnci/djn411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anujuo K, Stronks K, Snijder MB, et al. Relationship between short sleep duration and cardiovascular risk factors in a multi-ethnic cohort: The Helius study. Sleep Med. 2015;16:1482–88. doi: 10.1016/j.sleep.2015.08.014. [DOI] [PubMed] [Google Scholar]
- Arias E. United States life tables, 2004. Natl Vital Stat Rep. 2007;56:1–39. [PubMed] [Google Scholar]
- Beaudreault AR. U.S. Chronic disease prevention approaches and recommendations. J Community Med Health Educ. 2015:05. doi: 10.4172/2161-0711.1000382. [DOI] [Google Scholar]
- Bibbins-Domingo K, Pletcher MJ, Lin F, et al. Racial differences in incident heart failure among young adults. N Engl J Med. 2009;360:1179–90. doi: 10.1056/NEJMoa0807265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buxton OM, Pavlova M, Reid EW, et al. Sleep restriction for 1 week reduces insulin sensitivity in healthy men. Diabetes. 2010;59:2126–33. doi: 10.2337/db09-0699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cappuccio FP, D’Elia L, Strazzullo P, Miller MA. Quantity and quality of sleep and incidence of type 2 diabetes: A systematic review and meta-analysis. Diabetes Care. 2010;33:414–20. doi: 10.2337/dc09-1124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cespedes EM, Hu FB, Redline S, et al. Comparison of self-reported sleep duration with actigraphy: Results from the Hispanic community health study/study of Latinos Sueno ancillary study. Am J Epidemiol. 2016;183:561–73. doi: 10.1093/aje/kwv251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. Hillsdale: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- Cunningham TJ, Ford ES, Chapman DP, et al. Independent and joint associations of race/ethnicity and educational attainment with sleep-related symptoms in a population-based US sample. Prev Med. 2015;77:99–105. doi: 10.1016/j.ypmed.2015.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dahlgren A, Kecklund G, Åkerstedt T. Different levels of work-related stress and the effects on sleep, fatigue, and cortisol. Scand J Work Environ Health. 2005;31:277–85. doi: 10.5271/sjweh.883. [DOI] [PubMed] [Google Scholar]
- DeFranco EA, Hall ES, Muglia LJ. Racial disparity in previable birth. Am J Obstet Gynecol. 2016;214:394e391–397. doi: 10.1016/j.ajog.2015.12.034. [DOI] [PubMed] [Google Scholar]
- Duffy JF, Dijk DJ, Hall EF, Czeisler CA. Relationship of endogenous circadian melatonin and temperature rhythms to self-reported preference for morning or evening activity in young and older people. J Investig Med. 1999;47:141–50. [PMC free article] [PubMed] [Google Scholar]
- Eastman CI, Molina TA, Dziepak ME, Smith MR. Blacks (African Americans) have shorter free-running circadian periods than whites (Caucasian Americans) Chronobiol Int. 2012;29:1072–77. doi: 10.3109/07420528.2012.700670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eastman CI, Suh C, Tomaka VA, Crowley SJ. Circadian rhythm phase shifts and endogenous free-running circadian period differ between African-Americans and European-Americans. Sci Rep. 2015;5:8381. doi: 10.1038/srep08381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ertel K, Berkman L, Buxton O. Socioeconomic status, occupational characteristics, and sleep duration in African/Caribbean immigrants and US White health care workers. Sleep. 2011;34:509–18. doi: 10.1093/sleep/34.4.509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gamaldo AA, McNeely JM, Shah MT, et al. Racial differences in self-reports of short sleep duration in an urban-dwelling environment. J Gerontol B Psychol Sci Soc Sci. 2015;70:568–75. doi: 10.1093/geronb/gbt117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golden L. Flexible work schedules: What are we trading off to get them? Monthly Labor Review, March 2001. 2001:50–67. [Google Scholar]
- Golden SH, Brown A, Cauley JA, et al. Health disparities in endocrine disorders: Biological, clinical, and nonclinical factors–an Endocrine Society scientific statement. J Clin Endocrinol Metab. 2012;97:E1579–1639. doi: 10.1210/jc.2012-2043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grandner MA, Buxton OM, Jackson N, et al. Extreme sleep durations and increased C-reactive protein: Effects of sex and ethnoracial group. Sleep. 2013;36:769–779E. doi: 10.5665/sleep.2646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grandner MA, Chakravorty S, Perlis ML, et al. Habitual sleep duration associated with self-reported and objectively determined cardiometabolic risk factors. Sleep Med. 2014;15:42–50. doi: 10.1016/j.sleep.2013.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grandner MA, Williams NJ, Knutson KL, et al. Sleep disparity, race/ethnicity, and socioeconomic position. Sleep Med. 2016;18:7–18. doi: 10.1016/j.sleep.2015.01.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hagen EW, Barnet JH, Hale L, Peppard PE. Changes in sleep duration and sleep timing associated with retirement transitions. Sleep. 2016;39:665–73. doi: 10.5665/sleep.5548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hale L, Phuong D. Racial differences in self-reports of sleep duration in a population-based study. Sleep. 2007;30:1096–103. doi: 10.1093/sleep/30.9.1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heiman H, Artiga S. Beyond Health Care: The role of social determinants in promoting health and health equity. Washington, DC: The Henry J. Kaiser Family Foundation; 2015. [Google Scholar]
- Hertz R, Unger A, Cornell J, Saunders E. Racial disparities in hypertension prevalence, awareness, and management. Arch Intern Med. 2005;165:2098–104. doi: 10.1001/archinte.165.18.2098. [DOI] [PubMed] [Google Scholar]
- Ho DE, Imai K, King G, Stuart E. MatchIt: Nonparametric preprocessing for parametric causal inference. J Stat Softw. 2011;42:1–28. [Google Scholar]
- Horne JA, Ostberg O. A self-assessment questionnaire to determine morningness-eveningness in human circadian rhythms. Int J Chronobiol. 1976;4:97–110. [PubMed] [Google Scholar]
- Hu Y, Shmygelska A, Tran D, et al. GWAS of 89,283 individuals identifies genetic variants associated with self-reporting of being a morning person. Nat Commun. 2016;7:10448. doi: 10.1038/ncomms10448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackowska M, Steptoe A. Sleep and future cardiovascular risk: Prospective analysis from the English Longitudinal Study of Aging. Sleep Med. 2015;16:768–74. doi: 10.1016/j.sleep.2015.02.530. [DOI] [PubMed] [Google Scholar]
- Jackson CL, Redline S, Kawachi I, et al. Racial disparities in short sleep duration by occupation and industry. Am J Epidemiol. 2013;178:1442–51. doi: 10.1093/aje/kwt159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jean-Louis G, Grandner MA, Youngstedt SD, et al. Differential increase in prevalence estimates of inadequate sleep among black and white Americans. BMC Public Health. 2015;15:1185. doi: 10.1186/s12889-015-2500-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson DA, Lisabeth L, Hickson D, et al. The social patterning of sleep in African Americans: Associations of socioeconomic position and neighborhood characteristics with sleep in the Jackson heart study. Sleep. 2016;39:1749–59. doi: 10.5665/sleep.6106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones CR, Campbell SS, Zone SE, et al. Familial advanced sleep-phase syndrome: A short-period circadian rhythm variant in humans. Nat Med. 1999;5:1062–65. doi: 10.1038/12502. [DOI] [PubMed] [Google Scholar]
- Kanerva N, Kronholm E, Partonen T, et al. Tendency toward eveningness is associated with unhealthy dietary habits. Chronobiol Int. 2012;29:920–27. doi: 10.3109/07420528.2012.699128. [DOI] [PubMed] [Google Scholar]
- Keys A, Fidanza F, Karvonen MJ, et al. Indices of relative weight and obesity. J Chronic Dis. 1972;25:329–43. doi: 10.1016/0021-9681(72)90027-6. [DOI] [PubMed] [Google Scholar]
- Krueger PM, Friedman EM. Sleep duration in the United States: A cross-sectional population-based study. Am J Epidemiol. 2009;169:1052–63. doi: 10.1093/aje/kwp023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lakerveld J, Mackenbach JD, Horvath E, et al. The relation between sleep duration and sedentary behaviours in European adults. Obes Rev. 2016;17:62–67. doi: 10.1111/obr.12381. [DOI] [PubMed] [Google Scholar]
- Lane JM, Vlasac I, Anderson SG, et al. Genome-wide association analysis identifies novel loci for chronotype in 100,420 individuals from the UK Biobank. Nat Commun. 2016;7:10889. doi: 10.1038/ncomms10889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lauderdale DS, Knutson KL, Yan LL, et al. Self-reported and measured sleep duration: How similar are they? Epidemiology. 2008;19:838–45. doi: 10.1097/EDE.0b013e318187a7b0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leproult R, Holmback U, Van Cauter E. Circadian misalignment augments markers of insulin resistance and inflammation, independently of sleep loss. Diabetes. 2014;63:1860–69. doi: 10.2337/db13-1546/-/DC1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Little RJ, Rubin DB. Single imputation methods. In: Little Roderick JA, Rubin Donald B., editors. Statistical analysis with missing data. New York, NY: John Wiley and Sons; 1987. pp. 59–74. [Google Scholar]
- Malone SK, Patterson F, Lu Y, et al. Ethnic differences in sleep duration and morning-evening type in a population sample. Chronobiol Int. 2016;33:10–21. doi: 10.3109/07420528.2015.1107729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merikanto I, Lahti T, Puolijoki H, et al. Associations of chronotype and sleep with cardiovascular diseases and type 2 diabetes. Chronobiol Int. 2013;30:470–77. doi: 10.3109/07420528.2012.741171. [DOI] [PubMed] [Google Scholar]
- Nunes J, Jean-Louis G, Zizi F, et al. Sleep duration among Black and White Americans: Results of the National Health Interview Survey. J Natl Med Assoc. 2008;100:317–22. doi: 10.1016/s0027-9684(15)31244-x. [DOI] [PubMed] [Google Scholar]
- Patterson F, Malone SK, Lozano A, Hanlon A. Smoking, screen-based, sedentary behavior, and diet associated with habitual sleep duration and chronotype: Data from the UK Biobank. Ann Behav Med. 2016;50:715–726. doi: 10.1007/s12160-016-9797-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pena MM, Rifas-Shiman SL, Gillman MW, et al. Racial/ethnic and socio-contextual correlates of chronic sleep curtailment in childhood. Sleep. 2016;39:1653–61. doi: 10.5665/sleep.6086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reutrakul S, Hood MM, Crowley SJ, et al. Chronotype is independently associated with glycemic control in type 2 diabetes. Diabetes Care. 2013;36:2523–29. doi: 10.2337/dc12-2697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith M, Burgess HJ, Fogg LF, Eastman CI. Racial differences in the human endogenous circadian period. PLoS One. 2009;4:e6014. doi: 10.1371/journal.pone.0006014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spaeth AM, Dinges DF, Goel N. Resting metabolic rate varies by race and by sleep duration. Obesity. 2015;23:2349–56. doi: 10.1002/oby.21198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spiegel K, Leproult R, Van Cauter E. Impact of sleep debt on metabolic and endocrine function. Lancet. 1999;354:1435–39. doi: 10.1016/s0140-6736(99)01376-8. [DOI] [PubMed] [Google Scholar]
- Stamatakis KA, Kaplan GA, Roberts RE. Short sleep duration across income, education, and race/ethnic groups: Population prevalence and growing disparities during 34 years of follow-up. Ann Epidemiol. 2007;17:948–55. doi: 10.1016/j.annepidem.2007.07.096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stranges S, Dorn JM, Cappuccio FP, et al. A population-based study of reduced sleep duration and hypertension: The strongest association may be in premenopausal women. J Hypertens. 2010;28:896–902. doi: 10.1097/HJH.0b013e328335d076. [DOI] [PubMed] [Google Scholar]
- Taillard J, Philip P, Chastang JF, Bioulac B. Validation of Horne and Ostberg morningness-eveningness questionnaire in a middle-aged population of French workers. J Biol Rhythms. 2004;19:76–86. doi: 10.1177/0748730403259849. [DOI] [PubMed] [Google Scholar]
- Taylor BJ, Matthews KA, Hasler BP, et al. Bedtime variability and metabolic health in midlife women: The SWAN Sleep Study. Sleep. 2016;39:457–65. doi: 10.5665/sleep.5464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomfohr L, Pung MA, Edwards KM, Dimsdale JE. Racial differences in sleep architecture: The role of ethnic discrimination. Biol Psychol. 2012;89:34–38. doi: 10.1016/j.biopsycho.2011.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U. S. Department of Health and Human Services. Healthy people 2020: Foundation health measures. 2016 Nov 10; 2014. Available from: https://www.healthypeople.gov/2020/about/foundation-health-measures/Disparities.
- Williamson EJ, Forbes A. Introduction to propensity scores. Respirology. 2014;19:625–35. doi: 10.1111/resp.12312. [DOI] [PubMed] [Google Scholar]
- Wong PM, Hasler BP, Kamarck TW, et al. Social jetlag, chronotype, and cardiometabolic risk. J Clin Endocrinol Metab. 2015;100:4612–20. doi: 10.1210/jc.2015-2923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright SP. Adjusted p-values for simultaneous inference. Biometrics. 1992 Dec;48:1005–13. doi: 10.2307/2532694. [DOI] [Google Scholar]