Abstract
Purpose
We determined the safety, pharmacokinetics, pharmacodynamics and recommended phase II dose of the base excision repair blocker methoxyamine combined with fludarabine.
Materials and Methods
This was a phase I study with intravenous fludarabine (25 mg/m2, days 1–5), and methoxyamine (15 mg/m2–120 mg/m2, once). A maximum of six cycles were given. Adult patients with relapsed/refractory hematologic malignancies, excluding acute myeloid leukemia, were eligible.
Results
Twenty patients were treated; diagnoses included CLL/SLL (n = 10), follicular lymphoma (n = 3), DLBCL (n = 3), mantle cell lymphoma (n = 1), anaplastic large cell lymphoma (n = 1) and plasma cell myeloma (n = 2). No DLTs were observed and dose escalation reached the maximum planned dose. Hematologic toxicity was frequent; most common grade 3–4 toxicities were lymphopenia (70%), neutropenia (60%), leukopenia (50%) and anemia (40%). Four patients achieved a partial remission and 8 achieved stable disease. The drug combination resulted in increased DNA damage measured with the Comet assay.
Conclusions
Methoxyamine combined with fludarabine was safe and well tolerated. Hematologic toxicity was comparable to single agent fludarabine. Activity appears to correlate with increased levels of DNA damage. Further studies will examine use of this combination of as part conditioning regimens of stem cell transplant and use of methoxyamine as fludarabine dose-sparing agent.
Keywords: phase I, methoxyamine, base excision repair, hematologic malignancies, pharmacokinetics
INTRODUCTION
The purine analog fludarabine is most commonly used in the treatment of chronic lymphocytic leukemia (CLL) [1, 2] but is also part of the therapeutic armamentarium for indolent lymphomas [3, 4] and myeloid malignancies [5]. In CLL, fludarabine alone achieves superior response rates and progression free survival (PFS) than alkylating agents, albeit without overall survival improvement (OS) [1, 6]. Fludarabine is also an important component of reduced intensity conditioning regimens for allogeneic stem cell transplant [7].
The active metabolite fludarabine triphosphate (F-ara-ATP) exerts its cytotoxic activity through incorporation into DNA. In replicating cells, F-ara-ATP forms abnormal base pairs with thymine (F:T), interferes with DNA chain elongation by DNA polymerase α [8] and inhibits several other enzymes involved in DNA synthesis [9, 10]. In resting cells, F-ara-ATP is incorporated into DNA by the nucleotide excision repair pathway (NER) and terminates the DNA polymerization stage of the NER process [11, 12]. The resulting DNA damage leads to cell death, mediated either by p53 [13, 14] or PARP [10].
The base excision repair pathway (BER) is a DNA repair mechanism distinct from NER, capable of recognizing single base pair abnormalities [15], including those caused by exposure to environmental mutagens and antineoplastic agents [16–19]. The initial step in BER is removal of the abnormal base by a specific DNA glycosylase, forming an apurinic/apyrimidinic (AP) site. The AP site is cleaved by AP endonuclease (APE), generating a single - strand DNA break, followed by incorporation of the correct base and subsequent annealing by DNA polymerase β and DNA ligase, respectively [20]. The activity of the BER system confers resistance against antineoplastic agents that cause DNA damage [21]. More importantly, BER inhibition augments the cytotoxic activity of DNA damaging agents [21–23].
Methoxyamine is a small organic amine that inhibits BER by reacting in a specific fashion with the aldehyde group in the sugar moiety present at the AP site. Methoxyamine-bound AP sites are refractory to the lyase activity of APE, block further actions of BER pathway and result in persistent DNA lesions and arrested DNA replication, causing additional DNA damage by acting as topoisomerase IIα poisons [24]. Methoxyamine enhances the in vitro and in vivo activity of alkylating agents in colon, ovarian and breast cancer cell lines and xenograft models [25–29]. In a previous report, the addition of methoxyamine to fludarabine resulted in increased markers of DNA double strand breaks in cell lines and primary CLL cells, including increased Comet tail length and increased γH2AX expression, and result in induction of topoisomerase II expression [24]. In contrast, methoxyamine alone does not result in DNA double strand breaks or increased apoptosis compared to untreated controls [24, 30]. In mouse xenograft studies, methoxyamine augmented the antitumor activity of fludarabine, while methoxyamine alone did not have an antineoplastic effect [24].
Based on this preclinical data, we conducted a phase I study investigating the safety and tolerability of the combination of methoxyamine and fludarabine in the treatment of advanced hematologic malignancies.
RESULTS
Patient characteristics
Twenty patients were enrolled and treated in this clinical trial. Median age was 64 years (range 45 to 82); 60% of patients were men. The diagnoses included CLL/small lymphocytic lymphoma (SLL) (n = 10) follicular lymphoma (n = 3), diffuse large B cell lymphoma (DLBCL) (n = 3), mantle cell lymphoma (n = 1) and plasma cell myeloma (n = 2). The median number of prior lines of therapy was 3 (range 1 – 5) and 8 out of 10 CLL/SLL patients had received fludarabine, with 2 patients considered fludarabine refractory, relapsing within 6 months after a fludarabine – containing regimen (Table 1). All patients who completed at least one cycle of fludarabine and methoxyamine were considered evaluable for safety.
Table 1. Patient demographic and clinical characteristics.
| Characteristic | No. of patients |
|---|---|
| Patients who received at least one cycle of fludarabine and methoxyamine | 20 |
| Age, years | |
| Median | 64 |
| Range | 45–82 |
| Sex | |
| Male | 12 (60%) |
| Female | 8 (40%) |
| Number of prior treatments | |
| 1 – 2 | 7 (35%) |
| ≥ 3 | 13 (65%) |
| Prior treatment with fludarabine | 8 (40%) |
| Diagnoses | |
| CLL/SLL | 10 (50%) |
| Follicular lymphoma | 3 (15%) |
| Diffuse large B cell lymphoma | 3 (15%) |
| Mantle cell lymphoma | 1 (5%) |
| Plasma cell myeloma | 2 (10%) |
| Eastern Cooperative Oncology Status | |
| 0 | 4 (20%) |
| 1 | 15 (75%) |
| 2 | 1 (5%) |
Treatment
In cycle 1, patients received fludarabine at a dose of 25 mg/m2, intravenously over 1 hour on days 1–5 of each cycle. Methoxyamine was infused on day 2 at the assigned dose level as intravenous infusion over 30 minutes, before fludarabine infusion. In cycle 2 and subsequent cycles, methoxyamine was given on day 1 of each cycle, before the infusion of fludarabine. The median number of cycles administered was 3 (range, 1 to 6). Seventeen patients discontinued treatment before completing the planned 6 cycles of therapy. The reasons for discontinuing therapy included disease progression (n = 7, 35%), adverse events (AEs) (n = 4, 25%: grade 2 fatigue [n = 2]; grade 3 pulmonary infection [n = 1] and prolonged neutropenia [n = 1]); patient choice (n = 4, 20%), continuation to allogeneic stem cell transplant (n = 2, 10%). Three patients completed the full plan of six cycles of treatment.
Pharmacokinetics
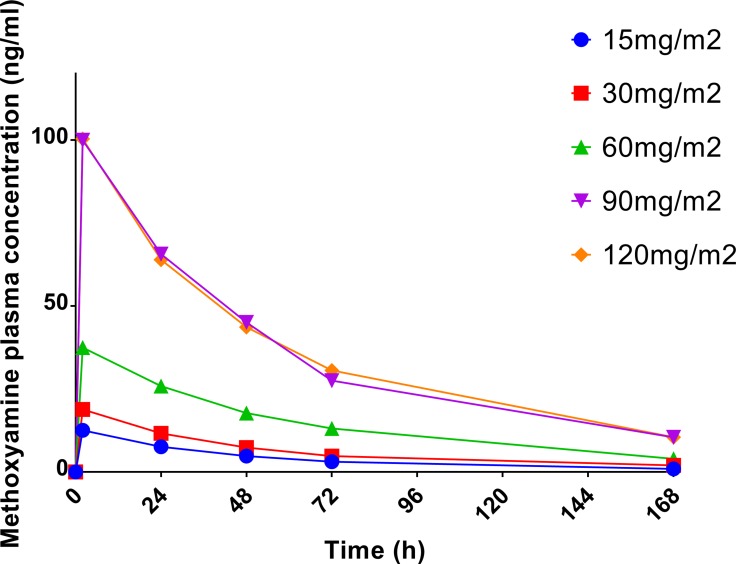
The results of pharmacokinetic analyses are presented in Table 2. The half-life of methoxyamine ranged from 27.8 to 68.5 hours; median half-life was 40.1 hours; there was no statistically significant difference in the average half-life between dose levels. Linear regression analysis demonstrated a statistically significant correlation between methoxyamine dose and area under the curve (AUC) of plasma concentration (p < 0.0001; R2 = 0.67), as well as maximum plasma concentration (Cmax) (p < 0.0001; R2 = 0.73). Figure 1 illustrates the effect of methoxyamine dose on its plasma concentration over time, suggesting exponential decrease over time, compatible with first order elimination kinetics. Modeling with linear regression analysis of the natural logarithm of methoxyamine concentration (Ln[MX]) and time showed statistically significant correlation at each dose level (R2 = 0.901, 0.744, 0.748, 0.801 and 0.785 for 15, 30, 60, 90 and 120mg/m2 dose levels, respectively; p < 0.0001 for all correlations), confirming first order kinetics for methoxyamine.
Table 2. Pharmacokinetic parameters of methoxyamine.
| Dose | Half Life, mean (± SEM) | Cmax, mean (± SEM) | AUC, mean (± SEM) | Clearance, mean (± SEM) |
|---|---|---|---|---|
| (mg/m2) | (h) | (ng/mL) | (hng/mL) | (mL/h/m2) |
| 15 | 40.9 (± 7.0) | 12.6 (± 1.3) | 691.6 (± 44.8) | 22062.0 (± 1445.4) |
| 30 | 41.6 (± 8.9) | 18.8 (± 5.4) | 1044.4 (± 301.3) | 34241.2 (± 9978.7) |
| 60 | 44.9 (± 3.1) | 37.5 (± 8.3) | 2502.4 (± 816.3) | 29014.3 (± 7954.4) |
| 90 | 46.0 (± 5.9) | 100.0 (± 21.3) | 6560.6 (± 1560.1) | 16035.0 (± 4895.5) |
| 120 | 45.0 (± 5.2) | 100.4 (± 13.8) | 6358.2 (± 1042.2) | 22180.8 (± 4371.2) |
AUC: area under the curve of plasma concentration; Cmax: maximum plasma concentration.
Figure 1. Average methoxyamine concentration in plasma over time after a single administration.
Pharmacodynamic studies – comet assay
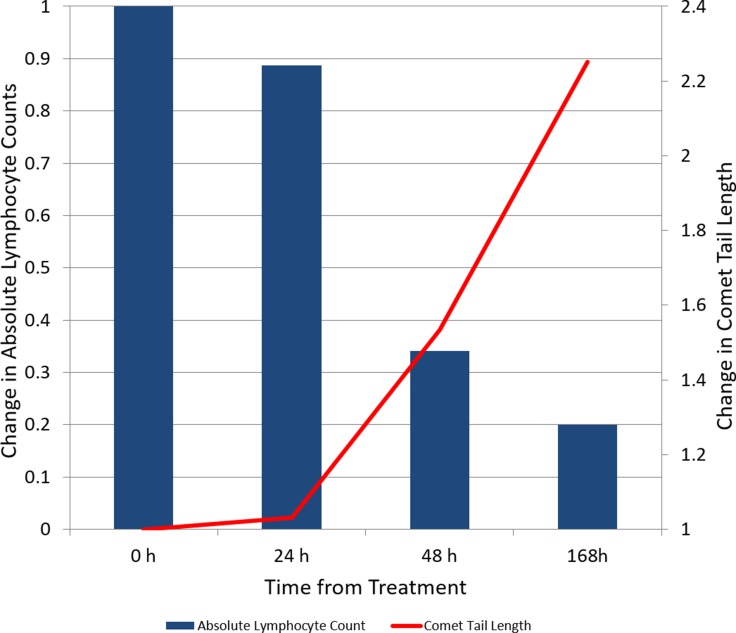
Comet tail length presented a statistically significant increase from baseline measured at 24, 27, 48, 72 and 96 hours after treatment was started (p < 0.0001). There was no difference between comet tail length measured at baseline and 2 hours after first dose of fludarabine. There was no statistically significant difference in comet tail length between methoxyamine dose levels.
Linear regression analysis showed the change in WBC number after 1 week of treatment presented a statistically significant correlation with comet tail length at baseline (p = 0.029), 2 (p = 0.038), 24 (p = 0.030) and 27 (p = 0.032) hours after treatment. Correlation with later time points (48, 72 and 96 hours) was not statistically significant.
In patients with CLL and circulating malignant lymphocytes (n = 7), the average comet tail length increased 2.25 times over the first week of therapy (95% CI 0.81–3.68). The median absolute lymphocyte count decreased from 19.2 × 109 lymphocytes/L (range 3.94–182.7) at baseline to 2.2 × 109 lymphocytes/L (range 0.37–137.2) at day 7 (Figure 4 and Supplementary Table 1). Linear regression showed a statistically significant correlation between the percentage of decrease in circulating lymphocytes after 7 days and comet tail length at 24 (R2 = 0.93, p = 0.0004), 48 (R2 = 0.84, p = 0.004), 72 (R2 = 0.86, p = 0.003), and 96 (R2 = 0.72, p = 0.02) hours.
Figure 4. Change over time in absolute lymphocyte count and comet tail length in subjects diagnosed with chronic lymphocytic leukemia with peripheral blood lymphocytosis (n = 7).
Safety
Hematologic toxicity was common, including anemia (n = 20, 100%), lymphopenia (n = 16, 80%), neutropenia (n = 15, 75%) and thrombocytopenia (n = 13, 65%). The most common non-hematologic toxicities included fatigue (n = 17, 85%), nausea (n = 13, 65%), hypocalcemia (n = 11, 55%), anorexia (n = 10, 50%) and paresthesias (n = 10, 50%). Regarding grade ≥ 3 AEs, the most common (≥ 10% of patients) grade 3 or 4 AEs observed were hematologic, including lymphopenia (n = 14, 70%), neutropenia (n = 12, 60%), anemia (n = 8, 40%) and thrombocytopenia (n = 5, 25%). Comparison of the incidence of grade ≥ 3 adverse events between patients who received up to three cycles of treatment vs. those that received more than three cycles showed there was only a statistically significant difference in the incidence of leukopenia (p = 0.03), with no difference observed in the incidence of other hematologic toxicities.
Infection was the only common grade 3–4 non-hematologic toxicity (n = 3, 15%). Six patients presented a decrease in haptoglobin without clinical evidence of autoimmune hemolytic anemia or increases in plasma bilirubin and lactate dehydrogenase. All grade ≥ 3 AEs and all AEs occurring in more than one patient are summarized in Table 3.
Table 3. Adverse events in subjects treated with fludarabine and methoxyamine.
| Toxicity | All Grades (%) | Grade 3 – 4 (%) | ||
|---|---|---|---|---|
| Hematologic | N | % | N | % |
| Leukopenia | 17 | 85 | 10 | 50 |
| Neutropenia | 15 | 75 | 12 | 60 |
| Anemia | 20 | 100 | 8 | 40 |
| Thrombocytopenia | 13 | 65 | 5 | 25 |
| Lymphopenia | 16 | 80 | 14 | 70 |
| Gastrointestinal | ||||
| Anorexia | 10 | 50 | 0 | 0 |
| Constipation | 9 | 45 | 0 | 0 |
| Diarrhea | 5 | 25 | 1 | 5 |
| Nausea | 13 | 65 | 0 | 0 |
| Vomiting | 5 | 25 | 0 | 0 |
| Neurologic | ||||
| Insomnia | 7 | 35 | 1 | 5 |
| Dizziness | 2 | 10 | 0 | 0 |
| Paresthesias | 10 | 50 | 0 | 0 |
| Pain | 8 | 40 | 1 | 5 |
| Respiratory | ||||
| Cough | 2 | 10 | 0 | 0 |
| Dyspnea | 7 | 35 | 0 | 0 |
| General | ||||
| Fatigue | 17 | 85 | 0 | 0 |
| Cutaneous/Dermatologic | ||||
| Alopecia | 3 | 15 | 0 | 0 |
| Erythema | 2 | 10 | 0 | 0 |
| Pruritus | 2 | 10 | 0 | 0 |
| Infectious | ||||
| Fever | 6 | 30 | 1 | 5 |
| Infection | 5 | 25 | 3 | 15 |
| Cardiovascular | ||||
| Edema | 3 | 15 | 0 | 0 |
| Laboratory | ||||
| Hyperbilirubinemia | 8 | 40 | 0 | 0 |
| Hypokalemia | 3 | 15 | 0 | 0 |
| Hyperuricemia without TLS | 3 | 15 | 1 | 5 |
| Hypoalbuminemia | 7 | 35 | 1 | 5 |
| Hyponatremia | 8 | 40 | 0 | 0 |
| Hypocalcemia | 11 | 55 | 0 | 0 |
| Transaminase elevation | 5 | 25 | 1 | 5 |
| Creatinine elevation | 5 | 25 | 0 | 0 |
| Haptoglobin decrease | 6 | 30 | 0 | 0 |
Efficacy and survival
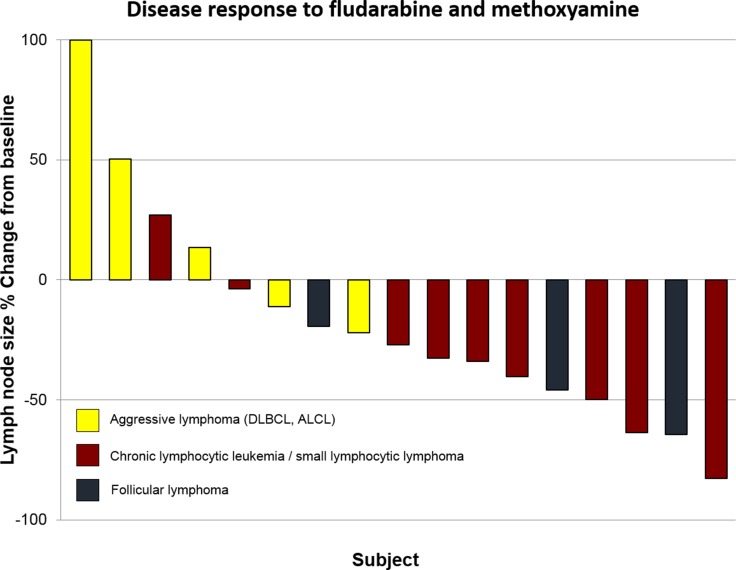
Four patients (20%) achieved partial response (CLL/SLL = 3, follicular lymphoma = 1), and 8 patients (40%) exhibited stable disease (CLL/SLL = 6, follicular lymphoma = 2, DLBCL = 1) (Figure 2). Six CLL/SLL subjects had lymphocyte counts over 5 × 109 lymphocytes/L and 5 presented normalization of lymphocytosis, with a median decrease of 95% in the first 7 days of therapy (range 29 – 99%, median baseline lymphocyte count = 72 × 109 lymphocytes/L; median lymphocyte count on day 8 = 1.75 × 109 lymphocytes/L).
Figure 2. Waterfall plots of best overall response according to response criteria in 17 patients with measurable disease (patients excluded include one subject with CLL and no measurable lymph nodes and two subjects with plasma cell myeloma) (ALCL: anaplastic large cell lymphoma; DLBCL: diffuse large B cell lymphoma; MCL: mantle cell lymphoma).
Two subjects (CLL, follicular lymphoma) proceeded to reduced intensity allogeneic stem cell transplant and have not relapsed. One subject received maintenance rituximab for two years and has not progressed. All remaining subjects have either progressed (n = 6) or died (n = 11).
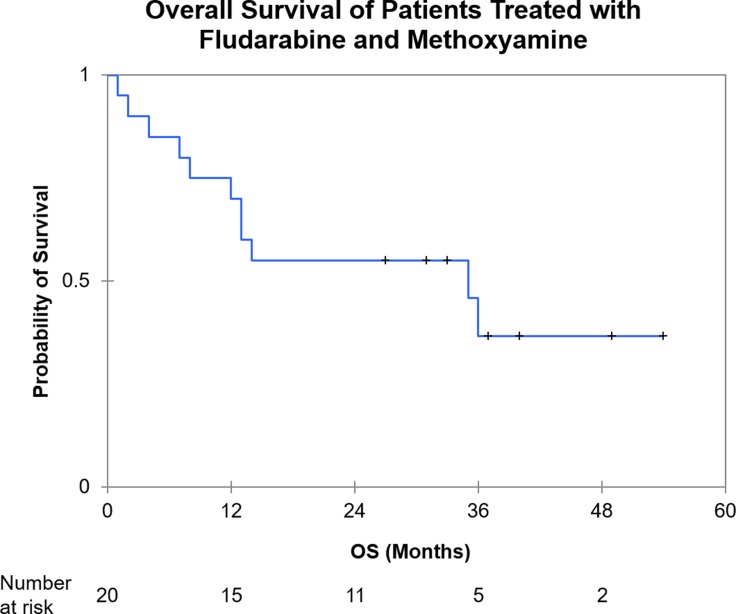
After a median follow up of 27 months, 2–year OS was 55% (95% CI 33–77%) (Figure 3). For patients who achieved at least stable disease, 2 - year OS estimate is 92% (95% CI 76–100%) with a median time to next therapy of 9 months (95% CI 2–28).
Figure 3. Kaplan Meier analysis of overall survival from treatment initiation.
(OS: Overall Survival).
DISCUSSION
The BER system represents a potential mechanism of resistance to fludarabine. Methoxyamine is a first in class inhibitor of BER. The results of this phase I trial demonstrate that this drug can be safely administered in combination with fludarabine. There were no dose limiting toxicities and the maximum tolerated dose was not reached.
In vitro and animal studies suggest that the addition of methoxyamine to fludarabine increases the antitumor effect of the latter without added cytotoxicity to normal hematopoietic cells [24]. In accordance with these preclinical observations, the rate and severity of neutropenia (grade ≥ 3 = 60%) and thrombocytopenia (grade ≥ 3 = 25%) observed in our study were comparable to those previously reported for fludarabine. In a phase I–II study of single agent fludarabine for relapsed/refractory CLL [31], the rates of grade ≥ 3 neutropenia and thrombocytopenia were 56% and 25%, respectively. Leiby and colleagues reported the results of a phase I study of fludarabine monotherapy for subjects with relapsed non-Hodgkin lymphoma [32]; grade 3–4 leukopenia occurred in 4 of 21 subjects and 2 cases of grade 3 thrombocytopenia were observed. Fludarabine was given in continuous infusion, with a smaller total dose per cycle than in our study (initial loading dose of 20mg/m2 followed by continuous infusion of 30 mg/m2/day for 48 hours). Several randomized, controlled studies compared fludarabine with alkylating agents or combination chemotherapy [1, 6, 33]. In these trials, hematologic toxicity was common (grade ≥ 3 neutropenia: 19–38%; grade ≥ 3 thrombocytopenia: 13–15%; grade ≥ 3 anemia: 7–18%). The incidence and severity of anemia observed in our study was higher than that observed with first – line fludarabine monotherapy; this could be secondary to extensive prior therapy in our patient population, but could also be secondary to red blood cell membrane damage by methoxyamine, causing low-grade hemolysis and providing an explanation for decreases in haptoglobin observed in 6 subjects. Grade 3 anemia was observed in previous phase I studies of methoxyamine in combination with pemetrexed [34] or temozolomide [35]. Animal toxicology studies observed extravascular hemolysis at methoxyamine doses 20 times higher than those required for efficacy. Fludarabine has known cumulative hematologic toxicity [36] and it is possible that methoxyamine increases marginally the incidence of this group adverse events. While only 11 of 20 patients received at least three cycles of therapy, we observed that patients who received more than three cycles of the combination therapy had a higher incidence of leukopenia. Treatment duration did not increase the incidence of other hematologic toxicities, again suggesting that the addition of methoxyamine to fludarabine results in limited additional toxicity, with most of the hematologic adverse events manifesting in the first cycles of treatment. In our study, as in previously reported phase I studies of methoxyamine combinations, severe non-hematologic toxicities were rare and not different from reported for single agent fludarabine. Based on these observations and without clear increase in the incidence of toxicity with increasing dose, we concluded 120 mg/m2 as the recommended phase II dose of methoxyamine when studied in combination with fludarabine.
Previous studies have shown that addition of methoxyamine to fludarabine increased DNA double-strand breaks [24]. In our study, we observed cumulative increases in comet tail length throughout the first week of therapy, indicating progressive DNA damage. The observation of a correlation between decreases in circulating malignant lymphocytes and comet tail length highlights the relevance of DNA double-strand break measurements as a surrogate marker of the antineoplastic effect of methoxyamine and fludarabine.
As expected, responses were observed in subjects with indolent lymphoid malignancies, including three patients with CLL and one with FL. Among partial responders, two subjects had received prior fludarabine. Patients who achieved at least stable disease included only subjects with lymphoid malignancies. Both plasma cell myeloma subjects presented progressive disease after 2 cycles of therapy, suggesting methoxyamine did not overcome the absence of antimyeloma activity of fludarabine [37]. The concentration of responses and stable disease in cases with indolent lymphoma, and the rapid normalization of lymphocytosis in CLL patients reflects the selective lymphotoxicity of the combination.
Previous studies have demonstrated the safety of methoxyamine when combined with the antimetabolite pemetrexed in solid tumors [38]; phase II studies are evaluating the efficacy of the combination of methoxyamine with pemetrexed, cisplatin and radiation for treatment of non-small cell lung cancer (ClinicalTrials.gov NCT02535325 and NCT02535312). A phase I study investigating the combination of methoxyamine and the alkylator temozolomide for treatment of solid tumors and CNS malignancies has recently been completed [35]. Our present study shows methoxyamine can be safely combined with yet an additional class of antineoplastic agents. Additional in vitro studies are evaluating the combination of methoxyamine with other purine and pyrimidine analogs as well as bendamustine, an alkylating agent with purine analog – like properties used frequently for treatment of indolent lymphoid malignancies [39].
Fludarabine remains a central component of reduced intensity conditioning regimens for hematopoietic progenitor cell transplant. These regimens have more limited antitumor activity, and are primarily designed to be immunosuppressive, primarily through lymphodepletion, relying on the graft to eradicate the underlying neoplasm. Studies are planned to investigate the addition of methoxyamine to fludarabine – containing conditioning regimens, hypothesizing that the combination may result both in increased lymphodepletion as well as improved antineoplastic activity. Additional studies are planned to investigate the use of methoxyamine with alkylating agents used in stem cell transplant conditioning regimens, melphalan and busulfan.
With the introduction of new signaling inhibitors, the role of fludarabine in the treatment of indolent lymphomas and especially CLL has come into question [40, 41]. However, regimens containing this drug have excellent activity against CLL and remain relevant as preferred first line therapy for certain patient subsets [42]. Our study demonstrates that the addition of methoxyamine is safe and well tolerated and has activity against lymphoid malignancies, including subjects previously treated with fludarabine. The potential of methoxyamine to increase the antineoplastic activity of fludarabine with limited additional toxicity should be evaluated in further studies, both as a means of achieving higher antineoplastic activity and as a dose – sparing strategy.
Enhanced fludarabine activity may broaden its use in lymphoid malignancies as well as in stem cell transplant conditioning regimens, where increase activity of reduced intensity regimens can result in improved disease control.
MATERIALS AND METHODS
Study population
Eligible patients were adults older than 18 years of age with hematologic malignancies (excluding acute myeloid leukemia), relapsed after at least one line of therapy (no maximum), Eastern Cooperative Oncology Group performance status ≤ 2, adequate organ and bone marrow function (creatinine < 1.5 mg/dl or creatinine clearance > 60 ml/min/1.72 m2; total bilirubin < 1.5 mg/dl, AST < 2.5 times upper limit of normal; absolute neutrophil count > 750; absolute neutrophil count > 750/μl; platelets > 50,000/μl and hemoglobin > 9.0 g/dl). Patients who had progression after fludarabine therapy were eligible. Patients were excluded if they had received treatment within 3 weeks before starting treatment, if they had a history of uncontrolled heart failure (NYHA class III or IV), CNS or leptomeningeal involvement by disease, or if they had known HIV, hepatitis B or C infection.
The study protocol was approved by the institutional review board of University Hospitals Cleveland Medical Center. All patients gave written informed consent. The study was conducted according to good clinical practice and the declaration of Helsinki. It is registered at ClinicalTrials.gov (NCT01658319).
Study design
This was a single center, open label, dose escalation trial designed to assess the safety and pharmacokinetics of methoxyamine when given in combination with fludarabine. Treatment cycles lasted 28 days. Fludarabine, 25 mg/m2 was given intravenously daily from day 1 through 5; methoxyamine was given intravenously on day 2 of cycle 1 to facilitate pharmacokinetic analysis, and then on day 1 of subsequent cycles. Methoxyamine dose escalation was done in 3 + 3 design, in five dose levels between 15 and 120 mg/m2. For further assessment of safety endpoints, the final cohort (120 mg/m2) was expanded to a total of 6 subjects.
Study assessments
Adverse events were graded for severity according to the National Cancer Institute Common Terminology Criteria for Adverse Events (version 4.0). Dose limiting toxicities were defined as those occurring during the first cycle of therapy and included: grade ≥ 3 non-hematologic toxicities (with the exception of alopecia); grade 4 neutropenia lasting 14 or more days; febrile neutropenia (grade 4 neutropenia with fever > 38.5°C); neutropenic infection (grade ≥ 3 neutropenia with grade ≥ 3 infection); grade ≥ 3 hemolysis and grade ≥ 4 thrombocytopenia (or grade ≥ thrombocytopenia with grade ≥ 3 hemorrhage).
Baseline tumor measurements included complete blood count, bone marrow aspirate and biopsy and computed tomography (CT) imaging studies. Positron emission tomography imaging was done in patients with lymphomas known to be FDG avid, as delineated by Cheson and colleagues [43]. Serum and urine protein electrophoresis were done in plasma cell myeloma patients. Restaging laboratory and imaging studies were done every 8 weeks and at the end of treatment. The overall response rate was assessed by the investigator based on disease specific criteria [43–45]. Patients were observed for up to 1 year or until disease progression, death, or initiation of new anticancer therapy, whichever occurred first.
Pharmacokinetic studies
Researchers from the Case Comprehensive Cancer Center developed and validated a liquid chromatography tandem mass spectrometry (LC-MS/MS) method for determining methoxyamine concentration in human plasma samples [46]. Blood samples for pharmacokinetic analysis were collected before methoxyamine infusion and 2, 24, 48, 96 and 168 hours after infusion. The maximum plasma concentration (Cmax), elimination half-life, and area under the curve for methoxyamine concentration were determined. All pharmacokinetic studies were performed by the Translational Research and Pharmacology Core of the Case Comprehensive Cancer Center.
DNA damage measurements by comet assay
Peripheral blood samples were obtained at baseline, 2 hours after treatment with fludarabine alone on day 1, immediately before and 2 hours after methoxyamine and fludarabine infusion on day 2 and immediately before infusion of fludarabine on days 3, 4 and 5.
Peripheral blood mononuclear cells were isolated by Ficoll density gradient centrifugation.
The single cell comet electrophoresis assay was performed using Comet Assay kit (Trevigen, Gaithersburg, MD). Approximately 5000 mononuclear cells (in 50 μl) were mixed with 250 μl of 1% low melting point agarose in 1X PBS at 37°C. The mixture (75 μl) was pipetted onto a Comet slide (Trevigen, Gaithersburg, MD) and allowed to solidify at 4°C. Slides were then immersed for 30 minutes in prechilled lysis buffer (2.5 mM sodium chloride, 100 mM EDTA pH 10, 10 mM Tris Base, 1% sodium lauryl sarcosinate, 0.01% Triton X-100) at 4°C. After lysis, slides were incubated for 20 minutes in alkaline solution (0.3M NaOH, 1mM EDTA) at room temperature, to allow DNA unwinding, followed by alkaline electrophoresis for the next 30 minutes. The Comet shape in individual mononuclear cells was visualized by staining with the Comet silver staining kit (Trevigen, Gaithersburg, MD). Fifty cells per sample were analyzed using Komet Analysis software (Andor Technology, Belfast, UK). Cellular DNA damage was expressed as the tail “length”, tail DNA content, and tail “moment”, a measure that combines the length of DNA migration and the relative DNA content therein [47]. All pharmacodynamic assays were performed by the Translational Research and Pharmacology Core of the Case Comprehensive Cancer Center.
Statistical analysis
To determine whether increasing doses of methoxyamine affect drug clearance we examined the difference among methoxyamine elimination half-lives of each cohort of this study using one-way ANOVA. For the analysis of the Comet assay, two-way ANOVA (with Bonferroni correction for multiple comparisons) was used to compare the means of tail length values at different time points as well as the effect of methoxyamine dose on tail length at different time points. The correlations of tail length values with changes in WBC and absolute lymphocyte count were estimated using linear regression. All tests were two sided and p-values were considered statistically significant if lower than 0.05. Statistical analyses were performed using XLSTAT (Addinsoft, New York, NY) and SAS Software (SAS Institute Inc., Cary, NC).
SUPPLEMENTARY MATERIALS TABLE
Abbreviations
- AP
Apurinic/apyrimidinic
- APE
Apurinic/apyrimidinic site endonuclease
- BER
Base excision repair pathway
- CLL
Chronic lymphocytic leukemia
- Cmax
Maximum plasma concentration
- CT
Computed tomography
- DLBCL
Diffuse large B cell lymphoma
- F-ara-ATP
Fludarabine triphosphate
- FDG
Fludeoxyglucose (18F)
- FL
Follicular lymphoma
- LC-MS/MS
Liquid chromatography tandem mass spectrometry
- NER
Nucleotide excision repair pathway
- OS
Overall survival
- PFS
Progression free survival
- SLL
Small lymphocytic lymphoma
- WBC
White blood cell
Author contributions
Caimi: Designed trial, conducted research, analyzed data, wrote manuscript; Cooper: Conducted research, reviewed manuscript; William: Conducted research, reviewed manuscript; Dowlati: Designed trial, oversaw trial conduction, reviewed manuscript; Barr: Designed trial, reviewed manuscript; Fu: Analyzed data, reviewed manuscript; Pink: Conducted pharmacodynamic assays, reviewed manuscript; Xu: Conducted pharmacokinetic assays, reviewed manuscript; Lazarus: Designed trial, conducted research, reviewed manuscript; de Lima: Conducted research, reviewed manuscript; Gerson: Designed trial, reviewed manuscript.
CONFLICTS OF INTEREST
SLG holds patents under Case Western Reserve University for the use of methoxyamine, is compensated for service on the Scientific Advisory Board for Tracon, holds shares, and has a royalty and milestone interest through Case Western Reserve University for Methoxyamine (TRC-102). All other authors have no relevant conflicts of interest to disclose.
FUNDING
Case Comprehensive Cancer Center, Early Phase Clinical Research Support (EPCRS). Principal Investigator: Paolo F. Caimi.
NIH: 5K12CA076917-13; 5K12CA076917-14; 5K12CA076917-15; Physician Scientist Award (Program) (PSA) (K12). Principal Investigator: Stanton L. Gerson.
REFERENCES
- 1.Rai KR, Peterson BL, Appelbaum FR, Kolitz J, Elias L, Shepherd L, Hines J, Threatte GA, Larson RA, Cheson BD, Schiffer CA. Fludarabine compared with chlorambucil as primary therapy for chronic lymphocytic leukemia. N Engl J Med. 2000;343:1750–1757. doi: 10.1056/NEJM200012143432402. [DOI] [PubMed] [Google Scholar]
- 2.Hallek M, Fischer K, Fingerle-Rowson G, Fink AM, Busch R, Mayer J, Hensel M, Hopfinger G, Hess G, von Grunhagen U, Bergmann M, Catalano J, Zinzani PL, et al. Addition of rituximab to fludarabine and cyclophosphamide in patients with chronic lymphocytic leukaemia: a randomised, open-label, phase 3 trial. Lancet. 2010;376:1164–1174. doi: 10.1016/S0140-6736(10)61381-5. [DOI] [PubMed] [Google Scholar]
- 3.Zinzani PL, Pellegrini C, Broccoli A, Gandolfi L, Stefoni V, Casadei B, Maglie R, Argnani L, Pileri S. Fludarabine-Mitoxantrone-Rituximab regimen in untreated indolent non-follicular non-Hodgkin’s lymphoma: experience on 143 patients. Hematol Oncol. 2015;33:141–146. doi: 10.1002/hon.2151. [DOI] [PubMed] [Google Scholar]
- 4.Forstpointner R, Dreyling M, Repp R, Hermann S, Hanel A, Metzner B, Pott C, Hartmann F, Rothmann F, Rohrberg R, Bock HP, Wandt H, Unterhalt M, et al. The addition of rituximab to a combination of fludarabine, cyclophosphamide, mitoxantrone (FCM) significantly increases the response rate and prolongs survival as compared with FCM alone in patients with relapsed and refractory follicular and mantle cell lymphomas: results of a prospective randomized study of the German Low-Grade Lymphoma Study Group. Blood. 2004;104:3064–3071. doi: 10.1182/blood-2004-04-1323. [DOI] [PubMed] [Google Scholar]
- 5.Guolo F, Minetto P, Clavio M, Miglino M, Di Grazia C, Ballerini F, Pastori G, Guardo D, Colombo N, Kunkl A, Fugazza G, Rebesco B, Sessarego M, et al. High feasibility and antileukemic efficacy of fludarabine, cytarabine, and idarubicin (FLAI) induction followed by risk-oriented consolidation: A critical review of a 10-year, single-center experience in younger, non M3 AML patients. Am J Hematol. 2016;91:755–762. doi: 10.1002/ajh.24391. [DOI] [PubMed] [Google Scholar]
- 6.Johnson S, Smith AG, Loffler H, Osby E, Juliusson G, Emmerich B, Wyld PJ, Hiddemann W. Multicentre prospective randomised trial of fludarabine versus cyclophosphamide, doxorubicin, and prednisone (CAP) for treatment of advanced-stage chronic lymphocytic leukaemia. The French Cooperative Group on CLL. Lancet. 1996;347:1432–1438. doi: 10.1016/s0140-6736(96)91681-5. [DOI] [PubMed] [Google Scholar]
- 7.Kekre N, Marquez-Malaver FJ, Cabrero M, Pinana J, Esquirol A, Soiffer RJ, Caballero D, Terol MJ, Martino R, Antin JH, Lopez-Corral L, Solano C, Armand P, et al. Fludarabine/Busulfan versus Fludarabine/Melphalan Conditioning in Patients Undergoing Reduced-Intensity Conditioning Hematopoietic Stem Cell Transplantation for Lymphoma. Biol Blood Marrow Transplant. 2016;22:1808–1815. doi: 10.1016/j.bbmt.2016.07.006. [DOI] [PubMed] [Google Scholar]
- 8.Huang P, Chubb S, Plunkett W. Termination of DNA synthesis by 9-beta-D-arabinofuranosyl-2-fluoroadenine. A mechanism for cytotoxicity. J Biol Chem. 1990;265:16617–16625. [PubMed] [Google Scholar]
- 9.Gandhi V, Plunkett W. Cellular and clinical pharmacology of fludarabine. Clin Pharmacokinet. 2002;41:93–103. doi: 10.2165/00003088-200241020-00002. [DOI] [PubMed] [Google Scholar]
- 10.Galmarini CM, Mackey JR, Dumontet C. Nucleoside analogues: mechanisms of drug resistance and reversal strategies. Leukemia. 2001;15:875–890. doi: 10.1038/sj.leu.2402114. [DOI] [PubMed] [Google Scholar]
- 11.Sandoval A, Consoli U, Plunkett W. Fludarabine-mediated inhibition of nucleotide excision repair induces apoptosis in quiescent human lymphocytes. Clin Cancer Res. 1996;2:1731–1741. [PubMed] [Google Scholar]
- 12.Yamauchi T, Nowak BJ, Keating MJ, Plunkett W. DNA repair initiated in chronic lymphocytic leukemia lymphocytes by 4-hydroperoxycyclophosphamide is inhibited by fludarabine and clofarabine. Clin Cancer Res. 2001;7:3580–3589. [PubMed] [Google Scholar]
- 13.Rosenwald A, Chuang EY, Davis RE, Wiestner A, Alizadeh AA, Arthur DC, Mitchell JB, Marti GE, Fowler DH, Wilson WH, Staudt LM. Fludarabine treatment of patients with chronic lymphocytic leukemia induces a p53-dependent gene expression response. Blood. 2004;104:1428–1434. doi: 10.1182/blood-2003-09-3236. [DOI] [PubMed] [Google Scholar]
- 14.Rao VA, Plunkett W. Activation of a p53-mediated apoptotic pathway in quiescent lymphocytes after the inhibition of DNA repair by fludarabine. Clin Cancer Res. 2003;9:3204–3212. [PubMed] [Google Scholar]
- 15.Fromme JC, Verdine GL. Base excision repair. Adv Protein Chem. 2004;69:1–41. doi: 10.1016/S0065-3233(04)69001-2. [DOI] [PubMed] [Google Scholar]
- 16.Srivastava DK, Berg BJ, Prasad R, Molina JT, Beard WA, Tomkinson AE, Wilson SH. Mammalian abasic site base excision repair. Identification of the reaction sequence and rate-determining steps. J Biol Chem. 1998;273:21203–21209. doi: 10.1074/jbc.273.33.21203. [DOI] [PubMed] [Google Scholar]
- 17.Fortini P, Parlanti E, Sidorkina OM, Laval J, Dogliotti E. The type of DNA glycosylase determines the base excision repair pathway in mammalian cells. J Biol Chem. 1999;274:15230–15236. doi: 10.1074/jbc.274.21.15230. [DOI] [PubMed] [Google Scholar]
- 18.Sokhansanj BA, Rodrigue GR, Fitch JP, Wilson DM., 3rd A quantitative model of human DNA base excision repair. I. Mechanistic insights. Nucleic Acids Res. 2002;30:1817–1825. doi: 10.1093/nar/30.8.1817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hoeijmakers JH. Genome maintenance mechanisms for preventing cancer. Nature. 2001;411:366–374. doi: 10.1038/35077232. [DOI] [PubMed] [Google Scholar]
- 20.Liu Y, Prasad R, Beard WA, Kedar PS, Hou EW, Shock DD, Wilson SH. Coordination of steps in single-nucleotide base excision repair mediated by apurinic/apyrimidinic endonuclease 1 and DNA polymerase beta. J Biol Chem. 2007;282:13532–13541. doi: 10.1074/jbc.M611295200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Trivedi RN, Almeida KH, Fornsaglio JL, Schamus S, Sobol RW. The role of base excision repair in the sensitivity and resistance to temozolomide-mediated cell death. Cancer Res. 2005;65:6394–6400. doi: 10.1158/0008-5472.CAN-05-0715. [DOI] [PubMed] [Google Scholar]
- 22.Goellner EM, Grimme B, Brown AR, Lin YC, Wang XH, Sugrue KF, Mitchell L, Trivedi RN, Tang JB, Sobol RW. Overcoming temozolomide resistance in glioblastoma via dual inhibition of NAD+ biosynthesis and base excision repair. Cancer Res. 2011;71:2308–2317. doi: 10.1158/0008-5472.CAN-10-3213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bulgar AD, Weeks LD, Miao Y, Yang S, Xu Y, Guo C, Markowitz S, Oleinick N, Gerson SL, Liu L. Removal of uracil by uracil DNA glycosylase limits pemetrexed cytotoxicity: overriding the limit with methoxyamine to inhibit base excision repair. Cell Death Dis. 2012;3:e252. doi: 10.1038/cddis.2011.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bulgar AD, Snell M, Donze JR, Kirkland EB, Li L, Yang S, Xu Y, Gerson SL, Liu L. Targeting base excision repair suggests a new therapeutic strategy of fludarabine for the treatment of chronic lymphocytic leukemia. Leukemia. 2010;24:1795–1799. doi: 10.1038/leu.2010.166. [DOI] [PubMed] [Google Scholar]
- 25.Liu L, Taverna P, Whitacre CM, Chatterjee S, Gerson SL. Pharmacologic disruption of base excision repair sensitizes mismatch repair-deficient and -proficient colon cancer cells to methylating agents. Clin Cancer Res. 1999;5:2908–2917. [PubMed] [Google Scholar]
- 26.Liu L, Nakatsuru Y, Gerson SL. Base excision repair as a therapeutic target in colon cancer. Clin Cancer Res. 2002;8:2985–2991. [PubMed] [Google Scholar]
- 27.Taverna P, Hwang HS, Schupp JE, Radivoyevitch T, Session NN, Reddy G, Zarling DA, Kinsella TJ. Inhibition of base excision repair potentiates iododeoxyuridine-induced cytotoxicity and radiosensitization. Cancer Res. 2003;63:838–846. [PubMed] [Google Scholar]
- 28.Rinne M, Caldwell D, Kelley MR. Transient adenoviral N-methylpurine DNA glycosylase overexpression imparts chemotherapeutic sensitivity to human breast cancer cells. Mol Cancer Ther. 2004;3:955–967. [PubMed] [Google Scholar]
- 29.Fishel ML, He Y, Smith ML, Kelley MR. Manipulation of base excision repair to sensitize ovarian cancer cells to alkylating agent temozolomide. Clin Cancer Res. 2007;13:260–267. doi: 10.1158/1078-0432.CCR-06-1920. [DOI] [PubMed] [Google Scholar]
- 30.Yan L, Bulgar A, Miao Y, Mahajan V, Donze JR, Gerson SL, Liu L. Combined Treatment with Temozolomide and Methoxyamine: Blocking Apurininc/Pyrimidinic Site Repair Coupled with Targeting Topoisomerase IIα. Clin Cancer Res. 2007;13:1532–1539. doi: 10.1158/1078-0432.CCR-06-1595. [DOI] [PubMed] [Google Scholar]
- 31.Keating MJ, Kantarjian H, Talpaz M, Redman J, Koller C, Barlogie B, Velasquez W, Plunkett W, Freireich EJ, McCredie KB. Fludarabine: a new agent with major activity against chronic lymphocytic leukemia. Blood. 1989;74:19–25. [PubMed] [Google Scholar]
- 32.Leiby JM, Snider KM, Kraut EH, Metz EN, Malspeis L, Grever MR. Phase II trial of 9-beta-D-arabinofuranosyl-2-fluoroadenine 5’-monophosphate in non-Hodgkin’s lymphoma: prospective comparison of response with deoxycytidine kinase activity. Cancer Res. 1987;47:2719–2722. [PubMed] [Google Scholar]
- 33.Leporrier M, Chevret S, Cazin B, Boudjerra N, Feugier P, Desablens B, Rapp MJ, Jaubert J, Autrand C, Divine M, Dreyfus B, Maloum K, Travade P, et al. Randomized comparison of fludarabine, CAP, and ChOP in 938 previously untreated stage B and C chronic lymphocytic leukemia patients. Blood. 2001;98:2319–2325. doi: 10.1182/blood.v98.8.2319. [DOI] [PubMed] [Google Scholar]
- 34.Weiss GJ, Gordon MS, Rosen S, Savvides P, Adams BJ, Alvarez L, Liu L, Xu Y, Gerson SL, Leigh BR. Final results from a phase I study of oral TRC102 (methoxyamine HCl), an inhibitor of base-excision repair, to potentiate the activity of pemetrexed in patients with refractory cancer. J Clin Oncol. 2010;28:2576. [Google Scholar]
- 35.Eads JR, Krishnamurthi SS, Saltzman JN, Meropol NJ, Bokar JA, Koon HB, Sharma N, Savvides P, Pink J, Xu Y, Beumer JH, Fu P, Beatty K, et al. Phase I clinical trial temozolomide and methoxyamine (TRC-102) in patients. J Clin Oncol. 2015;33:2558. doi: 10.1007/s10637-020-00962-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bouvet E, Borel C, Oberic L, Compaci G, Cazin B, Michallet AS, Laurent G, Ysebaert L. Impact of dose intensity on outcome of fludarabine, cyclophosphamide, and rituximab regimen given in the first-line therapy for chronic lymphocytic leukemia. Haematologica. 2013;98:65–70. doi: 10.3324/haematol.2012.070755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kraut EH, Crowley JJ, Grever MR, Keppen MD, Bonnet JD, Hynes HE, Salmon SE. Phase II study of fludarabine phosphate in multiple myeloma. A Southwest Oncology Group study. Invest New Drugs. 1990;8:199–200. doi: 10.1007/BF00177259. [DOI] [PubMed] [Google Scholar]
- 38.Gordon MS, Rosen LS, Mendelson D, Ramanathan RK, Goldman J, Liu L, Xu Y, Gerson SL, Anthony SP, Figg WD, Spencer S, Adams BJ, Theuer CP, et al. A phase 1 study of TRC102, an inhibitor of base excision repair, and pemetrexed in patients with advanced solid tumors. Invest New Drugs. 2013;31:714–723. doi: 10.1007/s10637-012-9876-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hiraoka N, Kikuchi J, Yamauchi T, Koyama D, Wada T, Uesawa M, Akutsu M, Mori S, Nakamura Y, Ueda T, Kano Y, Furukawa Y. Purine analog-like properties of bendamustine underlie rapid activation of DNA damage response and synergistic effects with pyrimidine analogues in lymphoid malignancies. PLoS One. 2014;9:e90675. doi: 10.1371/journal.pone.0090675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Byrd JC, Jones JJ, Woyach JA, Johnson AJ, Flynn JM. Entering the era of targeted therapy for chronic lymphocytic leukemia: impact on the practicing clinician. J Clin Oncol. 2014;32:3039–3047. doi: 10.1200/JCO.2014.55.8262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Jain N, O’Brien S. Targeted therapies for CLL: Practical issues with the changing treatment paradigm. Blood Rev. 2016;30:233–244. doi: 10.1016/j.blre.2015.12.002. [DOI] [PubMed] [Google Scholar]
- 42.Eichhorst B, Fink AM, Bahlo J, Busch R, Kovacs G, Maurer C, Lange E, Koppler H, Kiehl M, Sokler M, Schlag R, Vehling-Kaiser U, Kochling G, et al. First-line chemoimmunotherapy with bendamustine and rituximab versus fludarabine, cyclophosphamide, and rituximab in patients with advanced chronic lymphocytic leukaemia (CLL10): an international, open-label, randomised, phase 3, non-inferiority trial. Lancet Oncol. 2016;17:928–942. doi: 10.1016/S1470-2045(16)30051-1. [DOI] [PubMed] [Google Scholar]
- 43.Cheson BD, Pfistner B, Juweid ME, Gascoyne RD, Specht L, Horning SJ, Coiffier B, Fisher RI, Hagenbeek A, Zucca E, Rosen ST, Stroobants S, Lister TA, et al. Revised response criteria for malignant lymphoma. J Clin Oncol. 2007;25:579–586. doi: 10.1200/JCO.2006.09.2403. [DOI] [PubMed] [Google Scholar]
- 44.Durie BG, Harousseau JL, Miguel JS, Blade J, Barlogie B, Anderson K, Gertz M, Dimopoulos M, Westin J, Sonneveld P, Ludwig H, Gahrton G, Beksac M, et al. International uniform response criteria for multiple myeloma. Leukemia. 2006;20:1467–1473. doi: 10.1038/sj.leu.2404284. [DOI] [PubMed] [Google Scholar]
- 45.Hallek M, Cheson BD, Catovsky D, Caligaris-Cappio F, Dighiero G, Dohner H, Hillmen P, Keating MJ, Montserrat E, Rai KR, Kipps TJ, International Workshop on Chronic Lymphocytic Leukemia Guidelines for the diagnosis and treatment of chronic lymphocytic leukemia: a report from the International Workshop on Chronic Lymphocytic Leukemia updating the National Cancer Institute-Working Group 1996 guidelines. Blood. 2008;111:5446–5456. doi: 10.1182/blood-2007-06-093906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Yang S, Savvides P, Liu L, Gerson SL, Xu Y. Development and validation of an LC-MS/MS method for pharmacokinetic study of methoxyamine in phase I clinical trial. J Chromatogr B Analyt Technol Biomed Life Sci. 2012;901:25–33. doi: 10.1016/j.jchromb.2012.05.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lovell DP, Omori T. Statistical issues in the use of the comet assay. Mutagenesis. 2008;23:171–182. doi: 10.1093/mutage/gen015. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.