Abstract
Purpose
To determine the frequency of visits to emergency departments (EDs) for non-urgent and urgent ocular conditions and risk factors associated with utilization of the ED for non-urgent and urgent ocular problems.
Design
Retrospective longitudinal cohort analysis
Participants
All enrollees age ≥ 21 years old in a U.S. managed care network from 2001-2014.
Methods
We identified all enrollees who presented to an ED with ocular conditions identified by International Classification of Diseases, 9th Revision billing codes. We designated each diagnosis as “urgent”, “non-urgent”, or “other”. We assessed the frequency of ED visits for urgent and non-urgent ocular conditions and how they changed over time. Next, we performed multivariable Cox regression modeling to determine factors associated with visiting an ED for urgent or non-urgent ocular conditions.
Main Outcome Measures
Hazard ratios (HR) with 95% confidence intervals (CI) of visiting an ED for urgent or non-urgent ocular conditions.
Results
Of the 11,160,833 enrollees eligible for this study, 376,680 (3.4%) had ≥1 ED visit for an eye-related problem over a mean ± standard deviation of 5.4 ± 3.3 years follow-up. Among the 376,680 enrollees who visited the ED for ocular conditions, 86,473 (23.0%) had ≥1 ED visits with a non-urgent ocular condition and 25,289 (6.7%) had ≥1 ED visit with an urgent ocular condition. ED utilization for non-urgent ocular problems was associated with younger age (p<0.0001 for all comparisons), black race or Latino ethnicity (p<0.0001 for both), male sex (p<0.0001), lower income (p<0.0001 for all comparisons), and those who frequently presented to an ED for non-ophthalmologic medical problems in a given year (p<0.0001). Enrollees with established eye care professionals had a 10% reduced hazard of visiting the ED for non-urgent ocular conditions (adjusted HR=0.90 [CI 0.88-0.92], p<0.0001).
Conclusions
Nearly one quarter of all enrollees in this managed care network who visited the ED for ocular problems were diagnosed with non-urgent conditions. Better educating and incentivizing patients to seek care for non-urgent ocular diseases in an office-based setting instead of an ED could potentially yield considerable cost savings without adversely affecting health outcomes and allow EDs to better serve patients with more severe problems.
Introduction
Emergency departments (EDs) provide acute and after-hours care to millions of Americans each year. Use of the ED by patients has rapidly risen from 108 million visits in 2000 to 130 million visits in 2010.1 In a 2012 systematic review, Uscher-Pines and colleagues reported that nearly 40% of all ED visits were for non-urgent medical conditions.2 A recent study by Channa and coworkers using the US Nationwide Emergency Department Sample found a similar trend in the specialty of ophthalmology, with over 40% of visits to the ED for ocular conditions deemed to be non-urgent.3
There are several reasons why it is important to identify factors associated with utilization of EDs for non-urgent ocular conditions. First, many of these patients can be safely and effectively managed in an outpatient clinical setting instead.1,3,4 Second, ED visits cost, on average, four times more than visits to an office setting for comparable medical problems, resulting in $580 higher costs per visit.5 Third, non-urgent medical conditions may contribute to ED overcrowding, which can lead to delays in the care of other patients with more urgent medical problems.6-10
Outside the specialty of ophthalmology, researchers have identified several characteristics of patients who present to the ED for non-urgent medical conditions, including younger age,11-16 black race,12,15,17,18 and lower income.14,17 Little is known about characteristics of persons who present to the ED for non-urgent ocular problems. By identifying the types of non-urgent ophthalmological problems that are routinely cared for in an ED setting and the characteristics of patients who are most likely to present with non-urgent ocular problems, health care providers can work with health policy-makers and researchers to look for alternative options for managing such conditions. Using a large managed care network database of over 11 million enrollees with commercial health insurance, we studied ED utilization for non-urgent and urgent ocular conditions over a 14 year time period.
Methods
Data Source
The Clinformatics DataMart database (OptumInsight, Eden Prairie, MN) contains detailed records of all beneficiaries enrolled in a nationwide US managed care network. The dataset contains all individuals with ≥1 International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM)19 codes for eye-related diagnoses (360-379.9, 871.XX, 918.XX, 940.XX), ≥1 Current Procedural Terminology (CPT)20 codes for any eye-related visits, diagnostic or therapeutic ocular procedures (65091-68899 or 92002-92499), or any other claim submitted by an ophthalmologist or optometrist from January 1, 2001 through December 31, 2014. For each enrollee, we had access to all medical claims for ocular and non-ocular conditions and sociodemographic information including age, sex, race/ethnicity, education level, and annual income. We have used this data source in the past to study patients with ocular diseases.21-23 The University of Michigan Institutional Review Board approved this study, which uses de-identified claims data.
Sample Selection
We identified all enrollees ≥ 21 years old with ≥ 1 year of continuous enrollment in the plan during 2001-2014. Enrollees with non-continuous enrollment were excluded since we could not determine whether they sought care in an ED during periods of non-enrollment. ED visits were identified based on CPT billing codes 99281-85 which captures visits submitted by an ED provider.
Reasons for Visits to the Emergency Department for Ocular Conditions
We classified all ocular conditions with ICD-9-CM billing codes into 1 of 3 categories: “non-urgent,” “urgent,” or “other.” Table S1 (available at http://www.aaojournal.org) provides a list of specific ocular diagnoses and associated ICD-9-CM codes that we defined as urgent and non-urgent. We defined three ocular conditions as “non-urgent”– blepharitis, conjunctivitis, and chalazion. These conditions were considered non-urgent since they rarely affect visual acuity or cause considerable discomfort that might necessitate urgent medical attention in an ED setting rather than seeking care in an outpatient setting such as a physician office. We identified “urgent” ocular conditions as those that are known to be acutely sight- or life-threatening and often are associated with decreased visual acuity or pain. Examples of urgent conditions include retinal detachment, corneoscleral laceration, and temporal arteritis. We classified the majority of the ocular conditions with ICD-9-CM codes as “other” since, without access to actual medical records, it can be challenging to appreciate the nature of symptoms a patient experienced with these conditions to appropriately categorize the condition as urgent or non-urgent. An example of a diagnosis in this category is a corneal abrasion. Even though most corneal abrasions heal quickly and without sequelae and thus could be viewed as non-urgent, from the patient's perspective, the intense pain and occasional blurred vision caused by corneal abrasions could reasonably justify a visit to an ED for evaluation and management.
Our data source captures up to five ICD-9-CM diagnosis codes for a given encounter. For enrollees who received multiple diagnoses at a given visit, if any diagnosis was for an urgent ocular condition (even if there were also non-urgent or “other” conditions listed for that particular visit), the visit was classified as “urgent”. To be classified as a “non-urgent” visit, none of the diagnoses listed on the encounter form could be “urgent”. Finally, each enrollee could have contributed more than one visit to the ED during his or her time in the plan. For those with multiple visits, we classified each visit for that enrollee as “urgent”, “non-urgent”, or “other”.
Analyses
Statistical analyses were performed using SAS software, version 9.4 (SAS Institute, Cary, NC). Participant characteristics were summarized for the entire sample using means and standard deviations (SD) for continuous variables and frequencies and percentages for categorical variables. We used a chi-squared test to evaluate whether the change in the number of enrollees who visited the ED for ocular problems per 10,000 enrollees from 2001 to 2014 was statistically significant. For all analyses, p<0.05 was considered statistically significant.
Multivariable Regression Model
Multivariable Cox proportional hazard regression models were created to identify characteristics of enrollees who presented for care at an ED for 1) any ocular condition; 2) an urgent ocular condition; 3) a non-urgent ocular condition. Predictor variables for the 3 models included age at plan enrollment, sex, race/ethnicity, education level, annual income, residence in an urban or rural community, whether the enrollee had commercial insurance or Medicare Advantage, presence of comorbid depression or dementia, whether the enrollee had records of frequent visits to the ED (> 4 times / year) for non-ophthalmologic conditions, whether the patient was followed regularly by an eye care provider, which we defined as >3 visits to the same ophthalmologist or optometrist with at least one 6 month interval between the visits, and Charlson Comorbidity Index (a measure of overall health).24 Model results are presented as hazard ratios (HRs) with 95% confidence intervals (CIs).
Results
There were 11,160,833 enrollees eligible for the analysis; these persons were enrolled for a mean ± SD of 4.6 ± 3.0 years. Of those eligible, 376,680 persons (3.4%) had at least one ED visit for an ocular condition over a mean ± SD of 5.4 ± 3.3 years follow-up (Figure 1). Among those who visited the ED for ocular problems, 86,473 enrollees (23.0%) had ≥1 visit for a non-urgent ocular condition, 25,289 enrollees (6.7%) had ≥1 visit for an urgent ocular condition, and 273,224 enrollees (72.5%) presented with ≥1 visit for ocular conditions that were not deemed urgent or non-urgent based on our categorization scheme. Examples of common diagnoses among those not categorized as urgent or non-urgent were “other specified visual disturbance (ICD-9-CM 368.8)” and “pain in or around eye (ICD-9-CM 379.91).” For the majority of the visits to the ED for non-urgent eye problems (76.6%), the non-urgent eye problem was listed as the primary diagnosis on the encounter indicating that it was likely the primary reason for presenting to the ED. Because some enrollees visited the ED more than once and for different types of ocular conditions the total number of enrollees who had a visit to the ED for any ocular condition is less than the sum of those who had visits for urgent, non-urgent, and other ocular conditions.
Figure 1. Emergency Department Visits for Urgent, Non-Urgent, and Other Ocular Conditions.
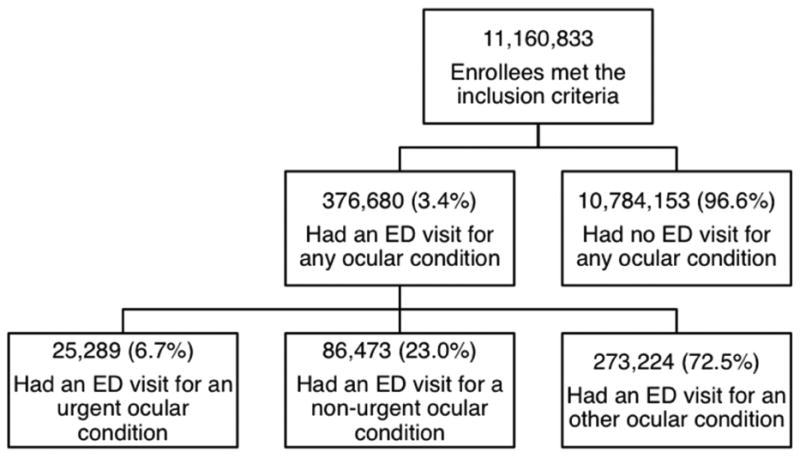
Distribution of eligible enrollees into those with Emergency Department (ED) visits for urgent, non-urgent, and other ocular conditions. Some enrollees had more than one visit and for different types of ocular conditions. Therefore, the total number of enrollees who had a visit to the ED for any ocular condition is less than the sum of those who had visits for urgent, non-urgent, and other ocular conditions.
The total number of enrollees who visited the ED for ocular problems increased 30% from 69.9 per 10,000 enrollees in 2001 to 90.9 per 10,000 enrollees in 2014 (p<0.0001). Rates were relatively stable from 2001-2009. The bulk of this increase took place from 2010 (69.4 per 10,000 enrollees) to 2014 (90.9 per 10,000 enrollees). The number of enrollees who visited the ED for urgent ocular problems was relatively stable, with 4.2 per 10,000 enrollees in 2001 and 6.1 per 10,000 enrollees in 2014. The number of enrollees who visited the ED for non-urgent ocular problems was also stable, with 17.7 per 10,000 enrollees in 2001 and 16.8 per 10,000 enrollees in 2014 (Figure 2).
Figure 2. Frequency of Visits to the Emergency Department Each Year From 2001-2014.
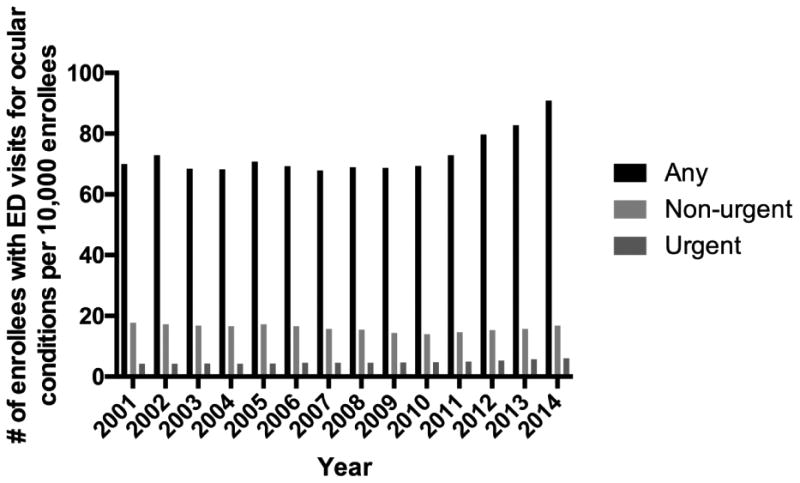
For each year from 2001 to 2014, the figure shows the total number of enrollees visiting the emergency department (ED) for any type of ocular condition per 10,000 enrollees and the total number of enrollees visiting the ED for urgent and non-urgent ocular conditions per 10,000 enrollees.
Characteristics of Enrollees Seeking Care in an ED for Non-urgent and Urgent Ocular Conditions
The mean ± SD age of all eligible enrollees was 47.4 ± 15.1 years. There were 6,320,557 (56.6%) females, 7,713,966 (77.3%) whites, 941,723 (9.4%) blacks, 938,981 (9.4%) Latinos, and 380,251 (3.8%) Asian Americans. The mean ± SD age of those beneficiaries who presented to the ED for an urgent ocular condition was 50.3 ± 17.3 years. There were 12,637 (50.0%) females, 17,513 (76.0%) whites, 2,784 (12.1%) blacks, 2,175 (9.4%) Latinos, and 579 (2.5%) Asian Americans who presented to the ED with an urgent ocular condition. Of those who sought care in an ED for a non-urgent ocular condition, the mean ± SD age was 43.4 ± 15.2 years. There were 46,395 (53.6%) females, 53,355 (68.0%) whites, 13,774 (17.6%) blacks, 9,103 (11.6%) Latinos, and 2,259 (2.9%) Asian Americans who went to the ED for non-urgent ocular problems (Table 2). Aside from a greater proportion of racial minorities in the later years (data not shown), the sociodemographic characteristics of the plan enrollees did not change much from 2001-2014.
Table 2. Sociodemographic characteristics of eligible enrollees.
| Visitors to the ED for non-urgent ocular conditions | Visitors to the ED for urgent ocular conditions | Total | ||||
|---|---|---|---|---|---|---|
| Number of beneficiaries | 86,473 | 25,289 | 11,160,833 | |||
| Mean | SD | Mean | SD | Mean | SD | |
| Age, years | 43.4 | 15.2 | 50.3 | 17.3 | 47.4 | 15.1 |
| n | % | n | % | n | % | |
| Sex | ||||||
| Male | 40,078 | 46.4% | 12,652 | 50.0% | 4,840,276 | 43.4% |
| Female | 46,395 | 53.6% | 12,637 | 50.0% | 6,320,557 | 56.6% |
| Race/Ethnicity | ||||||
| White | 53,355 | 68.0% | 17,513 | 76.0% | 7,713,966 | 77.3% |
| Black | 13,774 | 17.6% | 2,784 | 12.1% | 941,723 | 9.4% |
| Latino | 9,103 | 11.6% | 2,175 | 9.4% | 938,981 | 9.4% |
| Asian American | 2,259 | 2.9% | 579 | 2.5% | 380,251 | 3.8% |
| Education level | ||||||
| <High school | 777 | 1.0% | 197 | 0.8% | 79,186 | 0.8% |
| High school diploma | 28,120 | 34.5% | 7556 | 31.6% | 2,935,341 | 28.2% |
| Some college | 39,790 | 48.8% | 12,384 | 51.8% | 5,383,281 | 51.8% |
| College diploma or more | 12,794 | 15.7% | 3,765 | 15.8% | 2,003,384 | 19.3% |
| Annual Income | ||||||
| <$40K | 11,699 | 22.7% | 3,868 | 23.9% | 1,126,394 | 16.7% |
| $40K-$59K | 8,863 | 17.2% | 2,781 | 17.2% | 1,008,456 | 14.9% |
| $60K-$99K | 13,724 | 26.7% | 4,240 | 26.2% | 1,847,643 | 27.3% |
| >=$100K | 17,183 | 33.4% | 5,322 | 32.8% | 2,777,828 | 41.1% |
Race/ethnicity information was missing for 1,185,912 enrollees, education level was missing for 759,641 enrollees, and annual income was missing for 4,400,512 enrollees. ED = Emergency Department. SD = standard deviation.
Reasons for ED Visits for Non-Urgent and Urgent Ocular Diagnoses
Among the 86,473 enrollees who presented to the ED with diagnoses we classified as non-urgent, the median number of non-urgent visits per enrollee was 1 and ranged from 1 to 15 visits. The most common diagnosis was conjunctivitis (n=60,158; 69.6%). Among the 25,289 enrollees who presented to the ED with ocular conditions we classified as urgent, the median number of urgent visits per enrollee was 1 and ranged from 1 to 13 visits. The three most common urgent ocular diagnoses were orbital cellulitis (n=3,451; 13.6%), corneal ulcer (n=3,102; 12.3%), and giant cell arteritis (n=1,745; 6.9%).
Factors Associated with Visits to the ED for Ocular Problems
Risk Factors Associated with ED Visits for Any Ocular Problems
In the multivariable Cox regression model, several factors were found to increase the hazard of presenting to the ED for any ocular problem (Figure 3). The likelihood of presenting to an ED for any ocular problem decreased with increasing age (p<0.0001 for all comparisons). Compared with whites, blacks had a 24% increased hazard of presenting to the ED for any ocular condition (adjusted HR=1.24, [95% CI 1.22-1.25]) while Latinos had a 7% decreased hazard (adjusted HR=0.93, [CI 0.91-0.94]) and Asian Americans had a 30% decreased hazard (adjusted HR=0.70, [CI 0.69-0.72]). Compared with males, females had a 15% decreased hazard of presenting to the ED for any ocular condition (adjusted HR=0.85, [CI 0.84-0.85]). As an enrollee's level of annual income increased, the hazard of presenting to the ED for any ocular condition decreased, relative to those with the lowest annual income level (<$40,000) (p<0.0001 for all comparisons). Beneficiaries who frequently sought care in the ED for non-ophthalmologic problems had a 345% increased hazard of presenting to the ED for any ocular problem as well (adjusted HR=4.45 [CI 4.38-4.53]) relative to those enrollees who did not seek care in the ED as often for non-ophthalmologic problems. Those enrollees who had a regular eye care provider had a 14% increased hazard of presenting to the ED for any ocular problem (adjusted HR=1.14 [CI 1.13-1.16]) relative to other enrollees who did not have a regular eye care provider.
Figure 3. Factors Associated with Visiting an Emergency Department for Any Ocular Condition.
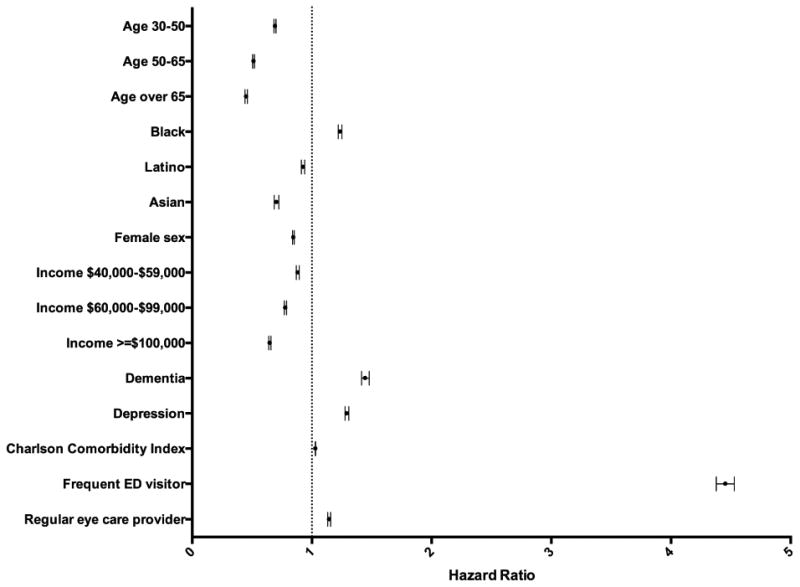
Multivariable Cox regression model identifying factors associated with visiting an emergency department for any ocular condition. Reference groups: age 21-30, white race, male sex, annual income <$40,000. A frequent ED visitor was defined as having > 4 visits / year for non-ophthalmologic conditions. Having a regular eye care provider was defined as >3 visits with an eye care provider with at least one 6-month interval between the visits. The multivariable Cox regression model was also adjusted for education level, urban/rural status, plan type, and dual enrolment status. ED = emergency department.
Risk Factors Associated with ED Visits for Non-urgent Ocular Problems
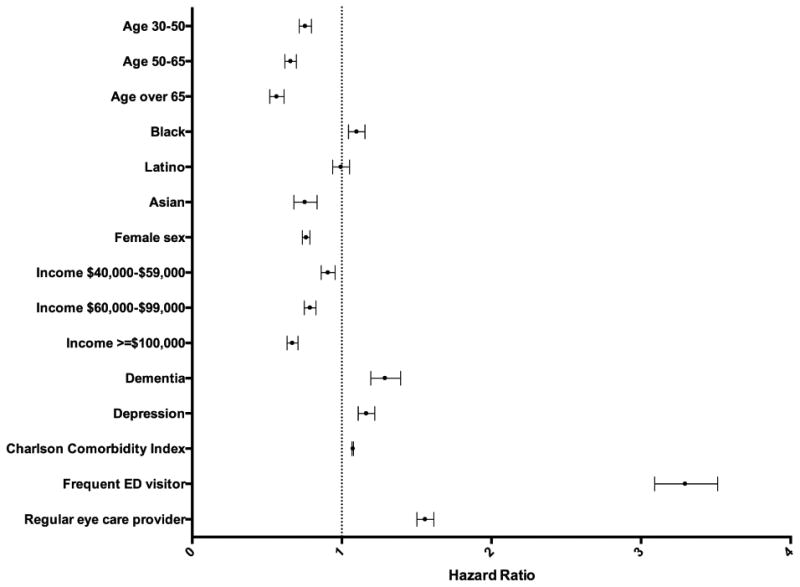
Older age was associated with decreased hazard of presenting to the ED for a non-urgent ocular problem (p<0.0001 for all comparisons). Compared with whites, blacks (adjusted HR=1.77, [CI 1.72-1.81]) and Latinos (adjusted HR=1.23, [CI 1.20-1.27]) had an increased hazard of presenting to the ED for a non-urgent ocular condition, while Asian Americans had a 14% decreased hazard (adjusted HR=0.86, [CI 0.82 - 0.91]). Females had a 14% decreased hazard of presenting to the ED for a non-urgent ocular problem (adjusted HR=0.86, [CI 0.84-0.87]) compared with males. Higher annual income levels were associated with decreased hazard of presenting to the ED for a non-urgent ocular condition (p<0.0001 for all comparisons). Enrollees with a history of frequent ED care for non-ophthalmologic problems had a 353% increased hazard of also presenting to the ED for non-urgent ocular problems (adjusted HR=4.53 [CI 4.36–4.71]) relative to those enrollees who did not seek care in the ED as often for non-ophthalmologic problems. Those enrollees with a regular eye care provider had a 10% decreased hazard of presenting to the ED for a non-urgent ocular condition (adjusted HR=0.90 [CI 0.88 - 0.92]) relative to other enrollees who did not have a regular eye care provider (Figure 4).
Figure 4. Factors Associated with Visiting an Emergency Department for a Non-Urgent Ocular Condition.
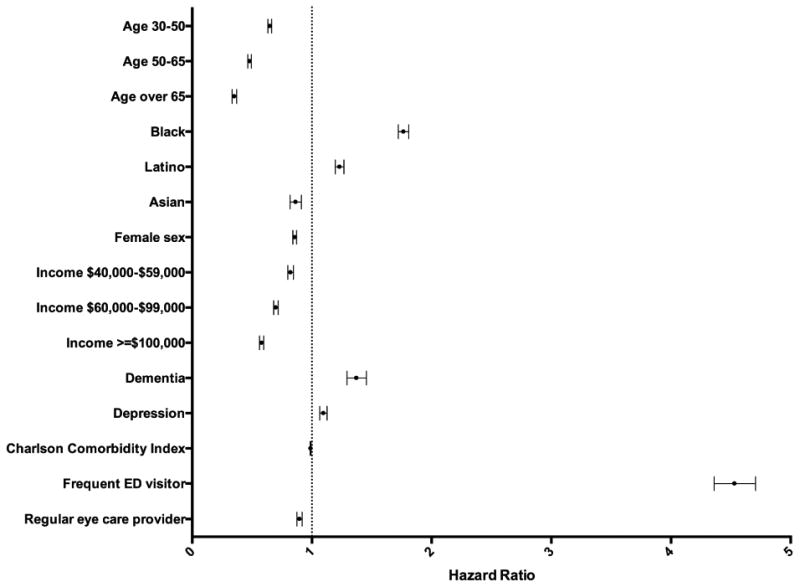
Multivariable Cox regression model identifying factors associated with visiting an emergency department for non-urgent ocular conditions. Reference groups: age 21-30, white race, male sex, annual income <$40,000. A frequent ED visitor was defined as having > 4 visits / year for non-ophthalmologic conditions. Having a regular eye care provider was defined as >3 visits with an eye care provider with at least one 6-month interval between the visits. The multivariable Cox regression model was also adjusted for education level, urban/rural status, plan type, and dual enrolment status. ED = emergency department.
Risk Factors Associated with ED Visits for Urgent Ocular Problems
Older age was associated with a decreased hazard of presenting to the ED for urgent ocular problems (p<0.0001 for all comparisons). Blacks had a greater hazard of presenting to the ED with an urgent ocular condition compared with whites (adjusted HR=1.10 [CI 1.04–1.16]). Females had a 24% decreased hazard of presenting to the ED for an urgent ocular condition (adjusted HR=0.76, [CI 0.74-0.79]) compared with males. Those enrollees with dementia (adjusted HR=1.29 [CI 1.19–1.39]), depression (adjusted HR=1.16 [CI 1.11–1.22]), and worse overall health (adjusted HR=1.07 [CI 1.07–1.08]) all had increased hazard. Frequent ED visitors for non-ophthalmologic diagnoses had a higher likelihood of presenting to the ED for an urgent eye problem (adjusted HR=3.30 [CI 3.09– 3.51]), as were patients with regular eye care providers (adjusted HR=1.56 [CI 1.50–1.62]) (Figure 5).
Figure 5. Factors Associated with Visiting an Emergency Department for an Urgent Ocular Condition.
Multivariable Cox regression model identifying factors associated with visiting an emergency department for urgent ocular conditions. Reference groups: age 21-30, white race, male sex, annual income <$40,000. A frequent ED visitor was defined as having > 4 visits / year for non-ophthalmologic conditions. Having a regular eye care provider was defined as >3 visits with an eye care provider with at least one 6-month interval between the visits. The multivariable Cox regression model was also adjusted for education level, urban/rural status, plan type, and dual enrolment status. ED = emergency department.
Discussion
In this study of over 11 million enrollees who were followed in a large managed care network for an average of over 4 years, we found a 30% rise in the number of enrollees visiting the ED for ocular problems (per 10,000 enrollees) from 2001 to 2014. Nearly one quarter of patients who visited the ED for an ocular condition did so for a non-urgent condition. Of the non-urgent visits, the majority of the patients were diagnosed with conjunctivitis, a condition that is rarely associated with decreased visual acuity or intense pain necessitating urgent management. After adjustment for potential confounding factors, we determined that some factors associated with increased likelihood of visiting an ED for a non-urgent eye problem included younger age, black race, Latino ethnicity, and lower income.
A recent publication by Channa and co-workers also explored visits to the ED for ocular conditions. Our paper differs from theirs in several important ways. Their paper focused on a timeframe from 2006-2011 while ours spanned a longer timeframe, capturing care from 2001-2014. This enabled us to be able to capture trends in ED utilization for ocular problems before versus after the Patient Protection and Affordable Care Act (PPACA) passage. Second, Channa and coworkers analyzed data from the US Nationwide Emergency Department Sample, which includes patients with various types of health insurance as well as a subset (19%) with no health insurance. By comparison, all of the enrollees in our analyses came from the same nationwide managed care network so insurance status was a constant and likely did not have a major impact on the differential patterns of ED use for ocular problems we are observing. Third, we were more restrictive in the sorts of ocular conditions we classified as urgent, limiting them to conditions that are often life or sight-threatening while Channa and colleagues classified a more diverse group of ocular conditions as “emergent”.
We noticed a rise in number of ED visits for ocular conditions per 10,000 enrollees over the 14-year study period. This correlates well with the increase in overall ED visits across the country.25, 26 The study by Channa and coworkers found a slight decrease in the annual number of ED visits for ocular problems during 2006-2011. In the present study, ED visits for ocular problems were relatively stable during 2006-2011. After 2011 however, we noticed a marked increase in such visits (Figure 2). While it is not fully clear why ED visits for ocular problems began to increase starting in 2011, this increase coincides with the enactment of the PPACA. This act, which was signed in 2010, helped increase the number of Americans with health insurance.27 As such, many insurance plans had an influx of young adults as well as racial minorities and less affluent persons who previously did not have health insurance. Given that many of these patients may have gone years without eye care prior to obtaining health insurance it is not surprising that use of eye care services, including visits to the ED for eye problems, increased after the passage of this legislation. Similar to what we are observing in our study, researchers in other areas of medicine have demonstrated that improving health insurance coverage increased the rates of ED use.28 Other authors have speculated this is because patients feel more comfortable presenting to the ED for medical problems when they know they have financial coverage for the care they are going to receive.28
We found that younger enrollees were more likely to present to the ED for non-urgent eye problems compared to older persons. This aligns with several studies in other areas of medicine looking at use of the ED for non-urgent medical conditions.11-16 Younger patients tend to have fewer chronic ocular diseases and thus are less likely to have an established eye care provider to go to for routine ocular problems. Younger patients may also not be as aware that costs of care tend to be higher in an ED setting and that EDs often are not routinely staffed by eye care professionals and thus seeking care in an office setting is often preferable for non-urgent eye conditions. Younger patients are more likely to have work responsibilities during the hours when eye care providers' offices are open. These persons may be unwilling to miss work to seek care in an office setting and find it more convenient to come to an ED after hours instead. In contrast, older patients may have regular eye care providers who are caring for them for cataracts and other common ocular diseases and would know to contact them when they experience non-urgent problems. Targeted educational initiatives to help younger persons understand the types of services offered and not offered in EDs and how costs are often much higher for care received in EDs may help steer them to care in outpatient clinics instead.
All persons in this study had the same health insurance and thus theoretically should have had similar access to eye care providers. Yet, despite possessing the same health insurance, we still found that less affluent patients and racial minorities were more likely to present to the ED for non-urgent ocular problems. Outside the field of ophthalmology, two prior studies evaluating use of EDs for non-urgent medical problems also found that lower income was associated with increased ED use.14,17 Several studies have also demonstrated that blacks tended to use the ED for non-urgent medical problems more than whites.12,15,17,18 Although it is unclear why patients with lower socioeconomic status are more likely to seek ED care for non-urgent medical conditions, prior studies suggest the reasons for this are multifactorial.29-33 Less affluent patients may have increased difficulty getting off work to go an appointment during regular clinic hours.29 Additionally, they may have less of an understanding of what symptoms do and do not require urgent attention.34 Public transportation to clinics may be more difficult, making it more convenient to go to an ED instead.31 Arranging for a clinic visit may require a more nuanced understanding of the healthcare system than simply presenting to the ED.30 Less affluent patients may also live in communities where there are fewer outpatient clinics and providers available, making it more convenient to seek care in the ED.32,33
Patients who have established eye care providers were less likely to visit an ED for a non-urgent ocular problem. We suspect this may be because they had an eye care professional whose office they could go to for assistance with their non-urgent ocular problems. However, we found increased rates of ED use for urgent ocular conditions among persons with established eye care providers. A likely explanation for this is that persons who have regular eye care providers are more likely to have chronic ocular diseases that may flare up or transition from less severe to more severe states (i.e. diabetic retinopathy leading to neovascular glaucoma) which would necessitate an urgent visit to the ED.
In our analyses, evidence of frequent use of the ED for other medical problems was, by far, the strongest predictor of ED use for ocular problems as well. Patients who use the ED for much of their healthcare needs irrespective of the nature of the medical problems can be a major burden to EDs and caring for such patients can be very costly. As such, researchers and health policymakers have targeted this population to try to reduce ED use for non-urgent medical problems.35 Ways to decrease ED use by this population that have been tried include case management and patient education initiatives.35 Similar efforts may be useful to decrease use of the ED for non-urgent ocular problems as well.
There are various ways to minimize the use of the ED for non-urgent conditions. One possibility is improving patient access to clinics by incentivizing eye care providers to offer after hours care and to expand the number of offices where patients can be seen. Insurers could increase reimbursement to eye care providers for seeing patients after hours in an office setting rather than an ED. By doing so, it may decrease overall costs to the insurer and likely also improve quality of care. Guidelines regarding what is considered urgent versus non-urgent could be made more readily available for patients to help better educate patients about the urgency of the condition they are experiencing and whether a visit to an ED is necessary versus seeking care in an office setting instead. Multidisciplinary case management efforts directed at frequent ED visitors may reduce additional visits as well.36
When patients present to an ED with ocular complaints, there are often no eye care professionals on site to evaluate and manage them there. This puts the onus on ED providers to distinguish benign conditions such as conjunctivitis from potentially serious conditions that may look a little like conjunctivitis such as scleritis or neovascular glaucoma. Given our finding that a sizable number of patients are opting to seek care at an ED for ocular problems, these results may substantiate an expanded role of using teleophthalmogy to enhance the evaluation of these patients.37 In fact, a recent survey revealed that many ED providers are interested in using teleophthalmology to remotely connect the patient with an ophthalmologist to help triage patients with eye conditions.38 Direct communication from patients to eye care providers using telemedicine can reduce the number of unnecessary visits to the ED for ocular problems. This trend may already be taking place. For example, Woodward and coworkers recently reported that over 50% of eye care providers they surveyed had received external eye photographs directly from patients or other health care professionals for interpretation via email within a 3 month period.39
Our study used a large health care claims database that captures the care of millions of patients residing in communities throughout the US. The database includes information on an array of different patient-level and community-level variables and has information on all the different ocular conditions that patients presented to the ED with, not just those who presented with ocular trauma. The large number of enrollees allowed for sophisticated modeling to account for potential confounding factors. The diagnoses in this database were made by a healthcare provider, which is considered more reliable than patient self-report.40
Our study has limitations. Our data source lacks information on the symptoms and exam findings and access to the actual medical records from the ED visits was not possible. Since these conditions were diagnosed by ED providers and not all the enrollees were seen by an eye professional to confirm the diagnosis made, some patients may have been misdiagnosed. While this limitation is acknowledged, the diagnoses we classified as non-urgent can often be diagnosed without extensive examination and are within the scope of practice of ED providers. Visits to EDs, especially for more urgent ocular problems, may be driven by factors related to specific underlying ocular diseases such as glaucoma, macular degeneration, or diabetic retinopathy. More focused analyses assessing factors associated with ED visits for subgroups of patients, such as those with selected pre-existing chronic eye diseases may yield additional knowledge about how persons with these conditions make use of ED services. Finally, since all participants had commercial health insurance, results may not be generalizable to individuals with other forms of health insurance or without health insurance.2
In conclusion, nearly one quarter of enrollees visiting the ED for ocular conditions do so for non-urgent conditions. These analyses identified that, despite possessing health insurance, younger patients, racial minorities, and less affluent patients were more likely to visit an ED for a non-urgent eye condition. Policy makers, insurers, and clinicians should direct future efforts to steer patients with non-urgent diagnoses away from EDs and to other settings.
Supplementary Material
Acknowledgments
Financial Support: Michigan Institute for Clinical and Health Research; Research to Prevent Blindness “Physician Scientist” Award (JDS); W.K. Kellogg Foundation; National Eye Institute, K23 Mentored Clinical Scientist Award K23EY023596-01 (MAW); National Clinician Scholars Program (BCS)
Abbreviations and Acronyms
- ED
Emergency Department
- HRR
Hospital Referral Region
- HR
Hazard Ratio
- ICD-9-CM
International Classification of Diseases, Ninth Revision, Clinical Modification
- CPT
Current Procedural Terminology
Footnotes
Conflict of Interests: no conflicting relationship exists for any author
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Cunningham P. Center for Studying Health System Change. [Accessed August 26, 2016];Nonurgent Use of Hospital Emergency Departments. 2011 http://www.hschange.com/CONTENT/1204/1204.pdf.
- 2.Uscher-Pines L, Pines J, Kellermann A, et al. Emergency department visits for nonurgent conditions: systematic literature review. Am J Manag Care. 2013;19(1):47–59. [PMC free article] [PubMed] [Google Scholar]
- 3.Channa R, Zafar SN, Canner JK, et al. Epidemiology of eye-related emergency department visits. JAMA Ophthalmol. 2016;134:312–9. doi: 10.1001/jamaophthalmol.2015.5778. [DOI] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention. National Hospital Ambulatory Medical Care Survey: 2010 Emergency Department Summary Tables. [Accessed August 26, 2016];2013 https://www.cdc.gov/nchs/data/ahcd/nhamcs_emergency/2010_ed_web_tables.pdf.
- 5.Network for Excellence in Health Innovation. A matter of urgency: reducing emergency department overuse. [Accessed August 26, 2016];2010 http://www.nehi.net/writable/publication_files/file/nehi_ed_overuse_issue_brief_032610finaledits.pdf.
- 6.Afilalo J, Marinovich A, Afilalo M, et al. Nonurgent emergency department patient characteristics and barriers to primary care. Acad Emerg Med. 2004;11:1302–10. doi: 10.1197/j.aem.2004.08.032. [DOI] [PubMed] [Google Scholar]
- 7.Grumbach K, Keane D, Bindman A. Primary care and public emergency department overcrowding. Am J Public Health. 1993;83:372–8. doi: 10.2105/ajph.83.3.372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hoot NR, Aronsky D. Systematic review of emergency department crowding: causes, effects, and solutions. Ann Emerg Med. 2008;52:126–36. doi: 10.1016/j.annemergmed.2008.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Howard MS, Davis BA, Anderson C, et al. Patients' perspective on choosing the emergency department for nonurgent medical care: a qualitative study exploring one reason for overcrowding. J Emerg Nurs. 2005;31:429–35. doi: 10.1016/j.jen.2005.06.023. [DOI] [PubMed] [Google Scholar]
- 10.Bernstein SL, Aronsky D, Duseja R, et al. The effect of emergency department crowding on clinically oriented outcomes. Acad Emerg Med. 2009;16:1–10. doi: 10.1111/j.1553-2712.2008.00295.x. [DOI] [PubMed] [Google Scholar]
- 11.Davis JW, Fujimoto RY, Chan H, Juarez DT. Identifying characteristics of patients with low urgency emergency department visits in a managed care setting. Manag Care. 2010;19:38–44. [PubMed] [Google Scholar]
- 12.Liu T, Sayre MR, Carleton SC. Emergency medical care: types, trends, and factors related to nonurgent visits. Acad Emerg Med. 1999;6:1147–52. doi: 10.1111/j.1553-2712.1999.tb00118.x. [DOI] [PubMed] [Google Scholar]
- 13.Petersen LA, Burstin HR, O'Neil AC, et al. Nonurgent emergency department visits: the effect of having a regular doctor. Med Care. 1998;36:1249–55. doi: 10.1097/00005650-199808000-00012. [DOI] [PubMed] [Google Scholar]
- 14.Sarver JH, Cydulka RK, Baker DW. Usual source of care and nonurgent emergency department use. Acad Emerg Med. 2002;9:916–23. doi: 10.1111/j.1553-2712.2002.tb02193.x. [DOI] [PubMed] [Google Scholar]
- 15.Schappert SM. The urgency of visits to hospital emergency departments: data from the National Hospital Ambulatory Medical Care Survey (NHAMCS), 1992. Stat Bull Metrop Insur Co. 1995;76:10–9. [PubMed] [Google Scholar]
- 16.Honigman LS, Wiler JL, Rooks S, Ginde AA. National study of non-urgent emergency department visits and associated resource utilization. West J Emerg Med. 2013;14:609–16. doi: 10.5811/westjem.2013.5.16112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cunningham PJ, Clancy CM, Cohen JW, Wilets M. The use of hospital emergency departments for nonurgent health problems: a national perspective. Med Care Res Rev. 1995;52:453–74. doi: 10.1177/107755879505200402. [DOI] [PubMed] [Google Scholar]
- 18.Doty MM, Holmgren AL. Health care disconnect: gaps in coverage and care for minority adults. Findings from the Commonwealth Fund Biennial Health Insurance Survey (2005) Issue Brief (Commonw Fund) 2006;21:1–12. [PubMed] [Google Scholar]
- 19.Physician International Classification of Diseases Clinical Modification (ICD-9-CM), 9th Revision. Chicago, IL: American Medical Association Press; 2006. [Google Scholar]
- 20.Current Procedural Terminology (CPT) Professional Edition. Chicago, IL: American Medical Association Press; 2006. [Google Scholar]
- 21.Stein JD, Lum F, Lee PP, et al. Use of health care claims data to study patients with ophthalmologic conditions. Ophthalmology. 2014;121:1134–41. doi: 10.1016/j.ophtha.2013.11.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kauh CY, Blachley TS, Lichter PR, et al. Geographic variation in the rate and timing of cataract surgery among us communities. JAMA Ophthalmol. 2016;134:267–76. doi: 10.1001/jamaophthalmol.2015.5322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wubben TJ, Talwar N, Blachley TS, et al. Rates of vitrectomy among enrollees in a united states managed care network, 2001-2012. Ophthalmology. 2016;123:590–8. doi: 10.1016/j.ophtha.2015.11.001. [DOI] [PubMed] [Google Scholar]
- 24.Quan H, Li B, Couris CM, et al. Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am J Epidemiol. 2011;173:676–82. doi: 10.1093/aje/kwq433. [DOI] [PubMed] [Google Scholar]
- 25.The Henry J, Kaiser Family Foundation. Hospital emergency room visits per 1,000 population by ownership type. [Accessed August 26, 2016];2014 http://kff.org/other/state-indicator/emergency-room-visits-by-ownership/?currentTimeframe=0&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D.
- 26.Pines JM, Mullins PM, Cooper JK, et al. National trends in emergency department use, care patterns, and quality of care of older adults in the United States. J Am Geriatr Soc. 2013;61:12–7. doi: 10.1111/jgs.12072. [DOI] [PubMed] [Google Scholar]
- 27.Obama B. United States health care reform: progress to date and next steps. JAMA. 2016;316:525–32. doi: 10.1001/jama.2016.9797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Taubman SL, Allen HL, Wright BJ, et al. Medicaid increases emergency-department use: evidence from Oregon's Health Insurance Experiment. Science. 2014;343:263–8. doi: 10.1126/science.1246183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tsai JC, Liang YW, Pearson WS. Utilization of emergency department in patients with non-urgent medical problems: patient preference and emergency department convenience. J Formos Med Assoc. 2010;109:533–42. doi: 10.1016/S0929-6646(10)60088-5. [DOI] [PubMed] [Google Scholar]
- 30.Wilkin HA, Cohen EL, Tannenbaum MA. How low-income residents decide between emergency and primary health care for non-urgent treatment. Howard J Commun (HJC) 2012;23:157–74. [Google Scholar]
- 31.Koziol-McLain J, Price DW, Weiss B, et al. Seeking care for nonurgent medical conditions in the emergency department: through the eyes of the patient. J Emerg Nurs. 2000;26:554–63. doi: 10.1067/men.2000.110904. [DOI] [PubMed] [Google Scholar]
- 32.Lowe RA, Fu R, Ong ET, et al. Community characteristics affecting emergency department use by Medicaid enrollees. Med Care. 2009;47:15–22. doi: 10.1097/MLR.0b013e3181844e1c. [DOI] [PubMed] [Google Scholar]
- 33.Khan Y, Glazier RH, Moineddin R, Schull MJ. A population-based study of the association between socioeconomic status and emergency department utilization in Ontario, Canada. Acad Emerg Med. 2011;18:836–43. doi: 10.1111/j.1553-2712.2011.01127.x. [DOI] [PubMed] [Google Scholar]
- 34.Wilkin HA, Tannebaum MA, Cohen EL, et al. How community members and health professionals conceptualize medical emergencies: implications for primary care promotion. Health Educ Res. 2012;27:1031–42. doi: 10.1093/her/cys090. [DOI] [PubMed] [Google Scholar]
- 35.Pines JM, Asplin BR, Kaji AH, et al. Frequent users of emergency department services: gaps in knowledge and a proposed research agenda. Acad Emerg Med. 2011;18:e64–9. doi: 10.1111/j.1553-2712.2011.01086.x. [DOI] [PubMed] [Google Scholar]
- 36.Phillips GA, Brophy DS, Weiland TJ, et al. The effect of multidisciplinary case management on selected outcomes for frequent attenders at an emergency department. Med J Aust. 2006;184:602–6. doi: 10.5694/j.1326-5377.2006.tb00412.x. [DOI] [PubMed] [Google Scholar]
- 37.Woodward MA, Bavinger JC, Amin S, et al. Telemedicine for ophthalmic consultation services: use of a portable device and layering information for graders. J Telemed Telecare. 2016 doi: 10.1177/1357633X16634544. [published online Mar 1 2016] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wedekind L, Sainani K, Pershing S. Supply and perceived demand for teleophthalmology in triage and consultations in california emergency departments. JAMA Ophthalmol. 2016 doi: 10.1001/jamaophthalmol.2016.0316. [published online Mar 24 2016] [DOI] [PubMed] [Google Scholar]
- 39.Woodward MA, Ple-Plakon P, Blachley T, et al. Eye care providers' attitudes towards tele-ophthalmology. Telemed J E Health. 2015;21:271–3. doi: 10.1089/tmj.2014.0115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Patty L, Wu C, Torres M, et al. Validity of self-reported eye disease and treatment in a population-based study: the Los Angeles Latino Eye Study. Ophthalmology. 2012;119:1725–30. doi: 10.1016/j.ophtha.2012.02.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


