Abstract
Purpose
The mechanisms accounting for anticancer activity of AZD9291 (osimertinib or TAGRISSO™), an approved third generation EGFR inhibitor, in EGFR-mutant non-small cell lung cancer (NSCLC) cells and particularly for the subsequent development of acquired resistance are unclear and thus are the focus of this study.
Experimental design
AZD9219-resistant cell lines were established by exposing sensitive cell lines to AZD9291. Protein alterations were detected with Western blotting. Apoptosis was measured with annexin V/flow cytomentry. Growth-inhibitory effects of tested drugs were evaluated in vitro with cell number estimation and colony formation assay and in vivo with mouse xenogtaft models. Protein degradation was determined by comparing protein half-lives and inhibiting proteasome. Gene knockdown were achieved with siRNA or shRNA.
Results
AZD9291 potently induced apoptosis in EGFR-mutant NSCLC cell lines, in which ERK phosphorylation was suppressed accompanied with Bim elevation and Mcl-1 reduction likely due to enhanced Mcl-1 degradation and increased Bim stability. Blocking Bim elevation by gene knockdown or enforcing Mcl-1 expression attenuated or abolished AZD9291-induced apoptosis. Moreover, AZD9291 lost its ability to modulate Bim and Mcl-1 levels in AZD9291-resistant cell lines. The combination of a MEK inhibitor with AZD9291 restores the sensitivity of AZD9291-resistant cells including those with C797S mutation to undergo apoptosis and growth regression in vitro and in vivo.
Conclusions
Modulation of MEK/ERK-dependent Bim and Mcl-1 degradation critically mediates sensitivity and resistance of EGFR-mutant NSCLC cells to AZD9291 and hence is an effective strategy to overcome acquired resistance to AZD9291.
Keywords: Bim, Mcl-1, apoptosis, MEK, EGFR inhibitors, AZD9291, acquired resistance
Introduction
An important milestone in the treatment of non-small cell lung cancer (NSCLC) is the discovery of epidermal growth factor receptor (EGFR) activating mutations as an effective therapeutic target and the successful development of first generation EGFR tyrosine kinase inhibitors (EGFR-TKIs; e.g., gefitinib and erlotinib). EGFR activating mutations, 90% of which present as an exon 19 deletion (Del19; ~60%) or exon 21 point mutation (L858R; ~30%), occur in Western and Asian NSCLC patient populations at a rate of ~15% and ~40%, respectively (1). These mutations increase the binding affinity of EGFR-TKIs for the mutant receptor, thus conferring enhanced sensitivity to EGFR-TKI treatment. First generation EGFR-TKIs act as competitive reversible inhibitors of ATP and have provided significant clinical benefit for patients. However, the development of acquired resistance to these agents limits their long-term efficacy (1–3).
The most clearly defined mechanisms underlying acquired resistance to 1st generation EGFR-TKIs are the acquisition of a secondary T790M mutation, which accounts for approximately 60% of resistant cases, and MET (or c-MET) gene amplification, which is detectable in approximately 5–22% of resistant tumors (1–3). The threonine to methionine change in codon 790 (T790M) occurs in the tyrosine kinase domain and increases ATP affinity, thus preventing the binding of 1st generation reversible EGFR-TKIs to the EGFR tyrosine kinase domain. MET amplification activates EGFR-independent phosphorylation of ErbB3 and downstream activation of the PI3K/AKT pathway, hence providing a bypass mechanism even in the presence of a 1st generation EGFR inhibitor (4). In general, there is an inverse correlation between T790M and MET amplification, suggesting a complementary or independent role of the two mechanisms in the resistant cells (5).
AZD9291 (osimertinib or TAGRISSO™), CO1686 (rociletinib), HM61713 (Olmutinib), EGF816 (Nazartinib), ASP8273, PF06747775 and AC0010 (Avitinib) represent 3rd generation EGFR-TKIs, which selectively and irreversibly inhibit EGFR with the common activating mutations, Del19 and L858R, as well as the resistant T790M mutation while sparing wild-type EGFR (6,7). AZD9291 is very active in NSCLC patients with the EGFR T790M mutation following disease progression on 1st and 2nd generation EGFR-TKIs (8,9) and is now a FDA-approved drug for the treatment of NSCLC patients with T790M mutation. In addition to targeting NSCLC with T790M EGFR, clinical trials that test the efficacy of 3rd generation EGFR-TKIs (e.g., AZD9291) against treatment-naïve, locally advanced or metastatic EGFR-mutant NSCLC are ongoing (e.g., FLAURA trial; NCT02296125).
Unfortunately, the development of acquired resistance to the 3rd generation EGFR-TKIs has already been described in the clinic. A novel acquired EGFR C797S mutation demonstrated in cultured cell lines and from clinical tumors resistant to AZD9291 was reported recently (10–12). However, this mutation was detected only in a subset of AZD9291-treated NSCLCs with T790M mutation (33–36%) (10,13), and was very rare in cases resistant to CO1686 (< 3%) (13). In addition, MET amplification was demonstrated recently by us (14) and others (13,15,16) as another mechanism of resistance to both AZD9291 and CO1686. Hence, it appears that there are heterogeneous mechanisms mediating resistance to 3rd generation EGFR-TKIs.
Although the success of 3rd generation EGFR-TKIs in the treatment of EGFR T790M NSCLC has been clearly established, other than binding to mutant EGFR and inhibition of EGFR signaling, the precise mechanisms by which these novel EGFR-TKIs exert anticancer efficacy remain largely unknown. We therefore focused our effort on fully understanding the anticancer biology of 3rd generation EGFR-TKIs in order to generate robust scientific rationale that can inform the rational development of effective strategies to prevent and/or overcome acquired resistance to these agents. In this study, we have demonstrated that modulation of ERK-dependent Bim and Mcl-1 degradation are critical events that mediate efficacy of AZD9291 as a targeted therapy of NSCLC harboring EGFR activating mutations. Accordingly we propose an effective strategy to overcome AZD9291 resistance through modulating these events.
Materials and Methods
Reagents
AZD9291 and PF02341066 (crizotinib) were purchased from Active Biochemicals (Maplewood, NJ). AZD6244 (selumetinib) and PD0325901 were purchased from Selleckchem (Houston, TX, USA). GSK1120212 (trametinib) was purchased from LC Laboratories (Woburn, MA). All agents were dissolved in DMSO at a concentration of 10 mM and aliquots were stored at −80°C. Stock solutions were diluted to the appropriate concentrations with growth medium immediately before use. Mcl-1, p-Mcl-1 (S159/T163), p-Bim (S69), caspase-8, PARP, p-ERK1/2 (T202/Y204), and ERK1/2 antibodies were purchased from Cell Signaling Technology, Inc. (Beverly, MA). Caspase-3 antibody was purchased from Imgenex (San Diego, CA). Bcl-2 antibody was purchased from Santa Cruz Biotechnology, Inc (Santa Cruz, CA). Bax and GAPDH antibodies were purchased from Trevigen (Gaithersburg, MD). Bim antibody was purchased from EMD Millipore (Billerica, MA). Actinomycin D (Act D), cycloheximide (CHX), mouse monoclonal anti-actin and anti-tubulin antibodies were purchased from Sigma Chemical Co. (St. Louis, MO).
Cell lines and cell culture
The EGFR-mutant NSCLC cell lines, HCC827, PC-9 and gefitinib-resistant PC-9/GR (T790M), were provided by Dr. P. A. Jänne (Dana Faber Cancer Institute, Boston, MA) in 2009. The EGFR-wild type NSCLC cell lines, H226 and H596, were originally obtained from Dr. R. Lotan (M. D. Anderson Cancer Center, Houston, TX) in 2003. Erlotinib-resistant HCC827/ER and AZD9291-resistant HCC827/AR cell lines were established in our laboratory and described previously (14,17). The AZD9291-resistant cell lines, PC-9/AR and PC-9/GR/AR, were newly established in our laboratory by exposing PC-9 or PC-9/GR cells to gradually increasing concentrations of AZD9291 (starting at 10 nM and ending with 500 nM) for approximately 6 months (Fig. S1). These cell lines were routinely cultured in the presence of 500 nM AZD9291 and maintained resistance to AZD9291 even after withdrawal of AZD9291 from the culture medium for over 6 months, indicating an irreversible phenotype. MET gene amplification and protein hyperactivation were detected in HCC827/ER and HCC827/AR cells (14). Using ICE COLD-PCR developed by Transgenomic, Inc (Omaha, NE), EGFR exon 20 T790M mutation was detected in PC-9/GR/AR cells. However, C797S mutation in EGFR exon 20 and other mutations around codon C797S region and in EGFR exon 21 were not detected in HCC827/AR, PC-9/AR and PC-9/GR/AR cells (Fig. S1). Moreover, no K-RAS exon 2 mutations were detected in these cell lines. HCC827/Mcl-1 and PC-9/Mcl-1 stable cell lines (pooled populations) were generated by infecting cells with lentiviruses carrying ectopic Mcl-1 or vector for 48 h followed with selection with zeocin (500 ng/ml) for another 7 days as described previously (18). PC-9 cell line with EGFR 19del+T790M+C797S triple mutation used in a previous study (12)(we named it PC-9/3M) was kindly provided by Dr. A. N. Hata (Harvard Medical School, Boston, MA) on January of 2017. This cell line was resistant to AZD9291 as well as CO1686 and erlotinib (Fig. S2), thus confirming its resistance to these EGFR inhibitors. These cell lines were not genetically authenticated. Mycoplasma was detected annually or upon receiving using MycoAlert@ Mycoplasma Detection Kit (Lonza; Rockland, ME) to ensure mycoplasma negative. All cell lines were cultured in RPMI 1640 containing 5% fetal bovine serum at 37 °C in a humidified atmosphere of 5% CO2 and 95% air.
Growth inhibition assay
Cell numbers after various treatments in 96-well plates were estimated by sulforhodamine B (SRB) assay and growth inhibition was calculated as previously described (19). Combination index (CI) for drug interaction (e.g., synergy) was calculated using CompuSyn software (ComboSyn, Inc.; Paramus, NJ).
Colony formation assays
The effects of the given drug treatments on colony formation in 12-well plates were measured as previously described (20).
Detection of apoptosis
Apoptosis was evaluated with an annexin V/7-AAD apoptosis detection kit (BD Biosciences; San Jose, CA) according to the manufacturer's instructions. Caspase and PARP cleavage were also detected by Western blot analysis as additional indicators of apoptosis.
Western blot analysis
Preparation of whole-cell protein lysates and Western blot analysis were described previously (21,22).
Gene knockdown using small interfering RNA (siRNA) or short hairpin RNA (shRNA)
Bim siRNAs I (#6461) and II (#6518) were purchased from Cell Signaling Technology, Inc. Non-silencing control siRNA duplexes were described previously (21). Transfection of these siRNA duplexes was conducted in 6-well plates using the HiPerFect transfection reagent (Qiagen) following the manufacturer’s instructions. Lentiviral Bim shRNAs in pLKO.1 (TRCN0000001051 and TRCN0000001054) were purchased from Open Biosystems (Huntsville, AL) and used according to the manufacturer’s instructions to generate stable Bim knockdown cell lines (pooled populations).
Animal xenograft and treatments
Animal experiments were approved by the Institutional Animal Care and Use Committee (IACUC) of Emory University and conducted as described previously (14). The treatments include vehicle control, AZD9291 (5 mg/kg/day, og), GSK1120212 (3 mg/kg/day; og), and their combination. Tumor volumes were measured using caliper measurements and calculated with the formula V = π(length × width2)/6. At the end of the treatments, mice were weighed and euthanized with CO2 asphyxia. The tumors were then removed, weighed and frozen in liquid nitrogen. Tumor tissue aliquots were homogenized in protein lysis buffer for preparation of whole-cell protein lysates for Western blotting to detect the given proteins.
Statistical analysis
The statistical significance of differences between two experimental groups was analyzed with two-sided unpaired Student's t tests (for equal variances) or with Welch's corrected t test (unequal variances) by use of Graphpad InStat 3 software. Results were considered to be statistically significant at P < 0.05.
Results
AZD9291 effectively induces apoptosis in EGFR-mutant NSCLC cells
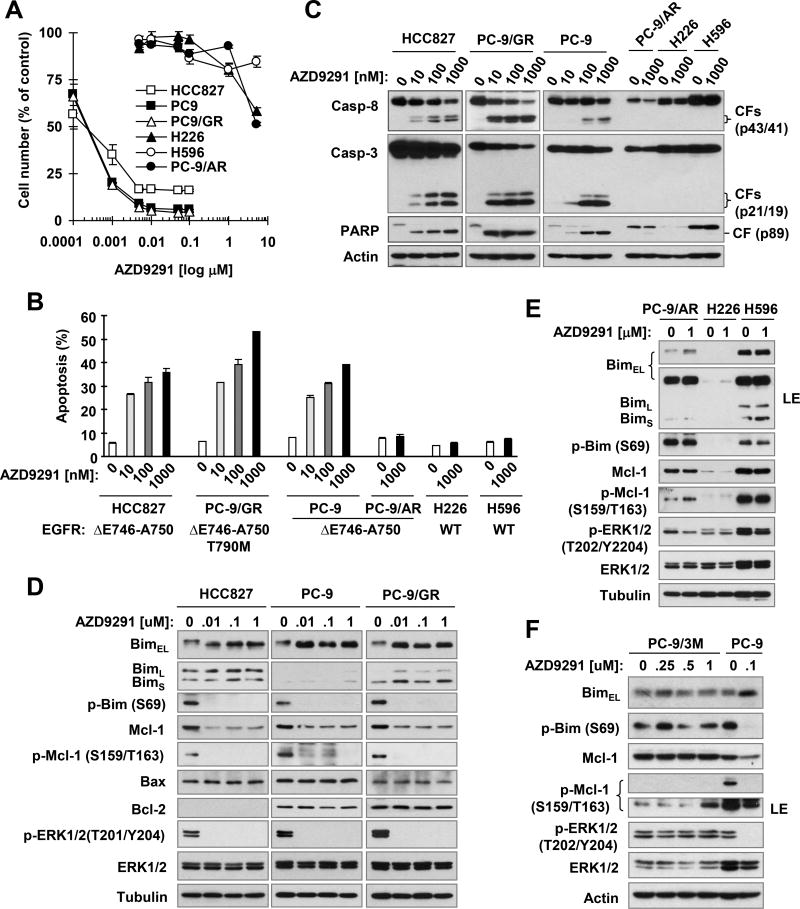
To determine whether and how effectively AZD9291 induces apoptosis in human NSCLC cell lines, we treated a panel of NSCLC cell lines with (HCC827, PC-9, PC-9/GR and PC-9/AR) and without (H226 and H596) activating EGFR mutations for 24 h and then conducted annexin V staining followed by flow cytometry to detect annexin V-positive (apoptotic) cells and Western blot analysis to detect cleavage of caspases and PARP. We observed that HCC827, PC-9 and PC-9/GR cells were highly sensitive to AZD9291, whereas PC-9/AR, H226 and H596 were resistant or insensitive to AZD9291 based on a 3-day cell survival assay (Fig. 1A). AZD9291 at a concentration range of 10 to 1000 nM effectively increased the percentage of annexin V-positive cells (Fig. 1B) and levels of cleaved forms of caspase-8, caspase-3 and PARP (Fig. 1C) in the sensitive HCC827, PC-9 and PC-9/GR cells. However, even at concentrations as high as 1000 nM, AZD9291 did not increase annexin V-positive cells nor induce cleavage of caspase-8, caspase-3 and PARP in the AZD9291 resistant (PC-9/AR) and insensitive (H226 and H596) cells. These results clearly indicate that AZD9291 induces apoptosis in the sensitive EGFR-mutant NSCLC cell lines.
Fig. 1. AZD9291 effectively decreases cell survival (A) and induces apoptosis (B and C) with suppression of ERK phosphorylation and modulation of Bim and Mcl-1 levels (D–F) in sensitive EGFR-mutant NSCLC cell lines.
A, The indicated NSCLC cell lines were exposed to different concentrations of AZD9291 for 3 days. Cell numbers were estimated with SRB assay. The data are means ± SDs of four replicate determinations. B and C, The indicated cell lines were treated with different concentrations of AZD9291 for 30 h and harvested for annexin V staining followed with flow cytometric analysis to detect apoptosis (B) and for Western blotting to detect protein cleavage (C). Data in B represent means ± SDs of duplicate determinations. EGFR mutation status for each tested cell line is indicated (B). D–F, The indicated cell lines were treated with different concentrations of AZD9291 for 8 h and then harvested for preparation of whole-cell protein lysates and subsequent Western blotting to detect the given proteins. WT, wild-type; CF, cleaved form; LE, longer exposure.
AZD9291 modulates Bim and Mcl-1 levels and suppresses ERK-dependent phosphorylation of Bim and Mcl-1 in the sensitive EGFR-mutant NSCLC cell lines
To understand the mechanism by which AZD9291 induces apoptosis in the sensitive EGFR-mutant NSCLC cell lines, we determined whether AZD9291 alters the levels of several proteins that critically regulate the apoptotic process including Bim, Mcl-1, Bax and Bcl-2. AZD9291 at a range of 10–1000 nM did not affect the levels of Bax and Bcl-2 in the 3 sensitive cell lines, HCC827, PC-9 and PC-9/GR, but decreased Mcl-1 levels, shifted the BimEL band and enhanced its intensity, and reduced the levels of p-ERK1/2, p-Bim (S69) and p-Mcl-1 (S159/T163) in these cell lines. The intensities of BimL and BimS were not substantially increased by AZD9291 (Fig. 1D). Hence any reference hereafter to Bim pertains only to BimEL. The suppression of ERK, Bim and Mcl-1 phosphorylation, reduction of Mcl-1 and elevation of Bim occurred within 2 h after AZD9291 treatment and were maintained for up to 14 h (the longest time we tested) (Fig. S3A). However, these modulations did not or minimally occur in the resistant (PC-9/AR and PC-9/3M) or insensitive (H226 and H596) cell lines even exposed to 1 µM AZD9291 (Figs. 1E and 1F). Under the same conditions, AZD9291 at 10 nM shifted the Bim band and increased its intensity with reduced Mcl-1 levels in HCC827 cells, but did not reduce Mcl-1 levels in both HCC827/ER and HCC827/AR cell lines even at 1 µM (Fig. S3B), both of which are resistant to AZD9291 (14). AZD9291 at 1 µM it could shift Bim band and increase its intensity in HCC827/AR cells, but failed to do so in HCC827/ER cells (Fig. S3B). Collectively, these results clearly demonstrate that AZD9291 modulates the levels of Bim and Mcl-1 with suppression of ERK and its dependent phosphorylation of Bim and Mcl-1 primarily in the sensitive EGFR-mutant NSCLC cell lines.
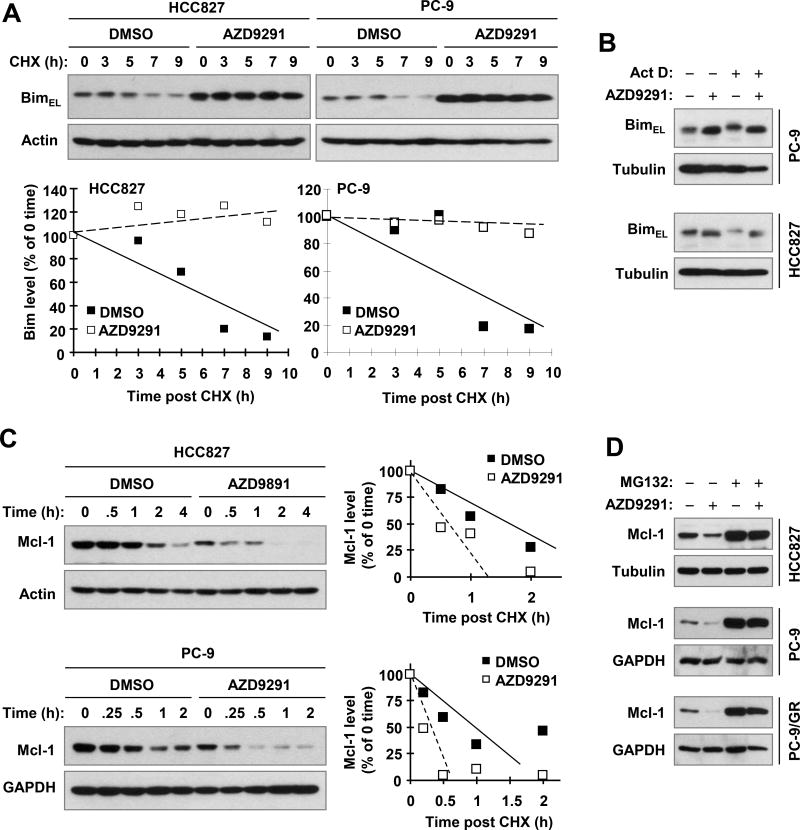
AZD9291 modulates Bim and Mcl-1 levels through regulation of their degradation in the sensitive EGFR-mutant NSCLC cells
Both Bim and Mcl-1 are phosphorylated by ERK, resulting in either enhanced (Bim) or suppressed (Mcl-1) proteasome-dependent degradation (23–28). Hence we determined whether AZD9291 affects Bim and Mcl-1 degradation in order to clarify the mechanism by which AZD9291 modulates Bim and Mcl-1 levels in the sensitive EGFR-mutant NSCLC cells. In both HCC827 and PC-9 cells, AZD9291 substantially slowed the degradation of Bim in comparison with the DMSO control (Fig. 2A), suggesting that Bim is stabilized in AZD9291-treated cells. In support of this finding, we found that inhibition of gene transcription with Act D did not alter the effect of AZD9291 on enhancing Bim band migration and intensity in these cell lines, suggesting a post transcriptional mechanism. In contrast, Mcl-1 was degraded more rapidly in AZD9291-treated HCC827 or PC-9 cells than in DMSO-treated cells (Fig. 2C). Consistently, the presence of the proteasome inhibitor MG132 elevated basal levels of Mcl-1 and also rescued Mcl-1 reduction induced by AZD9291 in these cell lines (Fig. 2D). These results strongly suggest that AZD9291 decreases Mcl-l levels primarily by facilitating its proteasomal degradation.
Fig. 2. AZD9291 stabilizes Bim protein (A) independent of transcription (B), but induces Mcl-1 protein degradation (C and D).
A and C, The given cell lines were exposed to 100 nM AZD9291 for 8 h followed with the addition of 10 µg/ml CHX. The cells were then harvested at the indicated times for Western blotting to detect the indicated proteins. Band intensities were quantified by NIH image J software and Bim and Mcl-1 levels were presented as a percentage of levels at 0 time post CHX treatment. B and D, The indicated cell lines were pre-treated with 2.5 µg/ml Act D (B) or 10 µg/ml MG232 (D) for 30 min and then co-treated with 100 nM AZD9291 for an additional 4 h. The cells were then harvested for Western blotting.
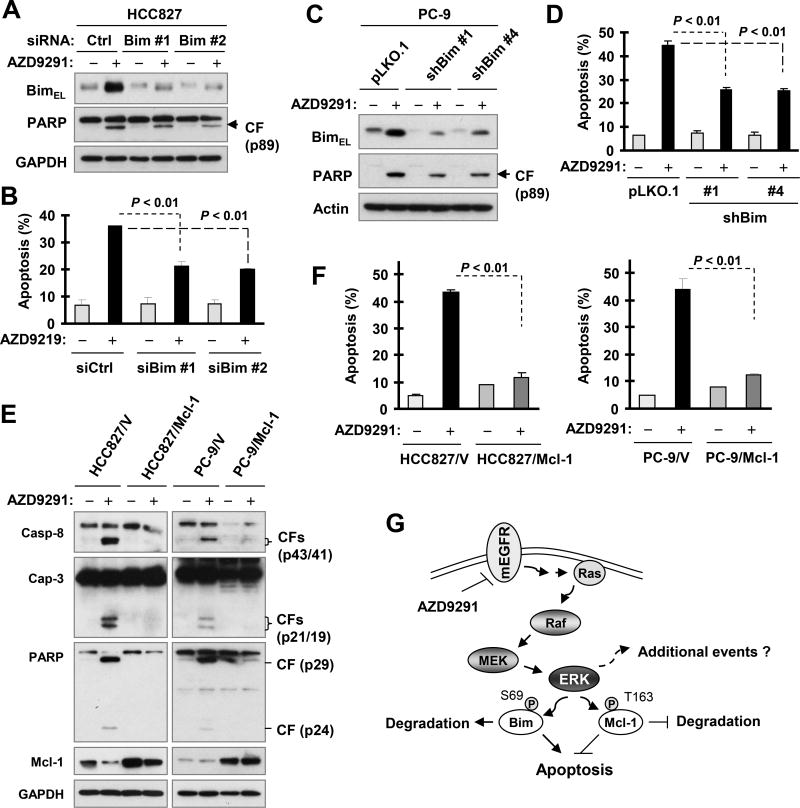
Modulation of Bim and Mcl-1 levels is a critical mechanism accounting for AZD9291-induced apoptosis in the sensitive EGFR-mutant NSCLC cells
To determine whether Bim elevation plays an essential role in mediating AZD9291-induced apoptosis, we used Bim siRNAs to knock down Bim expression and then examined its impact on the ability of AZD9291 to induce apoptosis in HCC827 cells. As detected by Western blotting, both Bim siRNA #1 and #2 effectively blocked Bim elevation induced by AZD9291 (Fig. 3A). Subsequently, we found reduced levels of cleaved PARP in Bim siRNA-transfected cells than in control siRNA-transfected cells (Fig. 3A). Consistent with this observation, we also detected significantly fewer apoptotic cells in HCC827 cells transfected with either of the two Bim siRNAs than in control siRNA-transfected cells (Fig. 3B). These results indicate that blockade of Bim elevation inhibits apoptosis induced by AZD9291. Similar results were also obtained in PC-9 cells in which Bim expression was stably knocked down using Bim shRNAs (Figs. 3C and 3D).
Fig. 3. Blockage of Bim elevation (A–D) or enforced expression of ectopic Mcl-1 (E and F) protects cancer cells from undergoing apoptosis induced by AZD9291, thus demonstrating a critical role of Bim and Mcl-1 modulation in mediating AZD9291-induced apoptosis in mutant EGFR NSCLC cells (G).
A and B, HCC827 cells were transfected with the indicated siRNAs for 48 h and then exposed to 100 nM AZD9291 for an additional 24 h. Bim knockdown and PARP cleavage were detected by Western blotting (A) and apoptosis was measured by annexin V/flow cytometry (B). C–F, The indicated stable transfectants were exposed to 100 nM AZD9291 for 24 h and then harvested for annexin V staining followed by flow cytometric analysis to detect apoptosis (D and F) and for Western blotting to detect the indicated proteins (C and E). The data are means ± SDs of duplicate (B, D and F) determinations. G, A schematic working model for induction of apoptosis by AZD9291 in mutant EGFR (mEGFR) NSCLC cells through modulating ERK-dependent degradation of Bim and Mcl-1 as well as yet-to-be identified additional mechanisms.
We also determined whether Mcl-1 reduction is involved in AZD9291-induced apoptosis in the sensitive EGFR-mutant NSCLC cell lines. To this end, we enforced expression of ectopic Mcl-1 in both HCC827 and PC-9 cell lines and then tested its impact on AZD9291-induced apoptosis. We observed that AZD9291 effectively induced cleavage of capase-8, caspase-3 and PARP (Fig. 3E) and increased annexin V-positive cells (Fig. 3F) in vector-control cell lines, but not at all or minimally in HCC827/Mcl-1 or PC-9/Mcl-1 cells. These results clearly demonstrate that enforced expression of Mcl-1 protects the cancer cells from AZD9291-induced apoptosis.
We noted that AZD9291 did not decrease Mcl-1 levels in PC-9/V cells (Fig. 3E) under the tested conditions (e.g., 24 h treatment). We thus compared the effect on Mcl-1 levels of prolonged AZD9291 treatment with that of short-time treatment in this cell line. The results show that AZD9291 did decrease Mcl-1 levels at 12 h and 16 h post treatment, but lost this activity at the 24 h post treatment time point (Fig. S4).
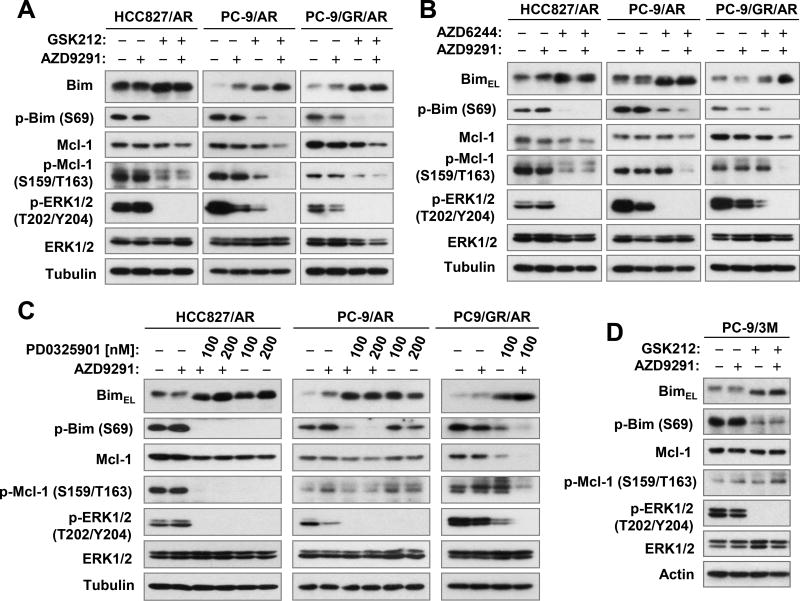
MEK inhibitors restore Bim elevation and Mcl-1 reduction in AZD9291-resistant EGFR-mutant NSCLC cell lines
The data presented so far suggest critical roles for Bim and Mcl-1 modulation in regulating AZD9291-induced apoptosis in the sensitive EGFR-mutant NSCLC cell lines. The inability of AZD9291 to modulate these protein levels in PC-9/AR cells with acquired resistance to AZD9291 led us to speculate whether a strategy that elevates Bim levels with simultaneous suppression of Mcl-1 may lower the threshold for AZD9291-resistant cells to re-respond to AZD9291, resulting in apoptotic cell death. Given that ERK regulates the phosphorylation and degradation of both Bim and Mcl-1 (23–28), we contemplated whether MEK inhibition could suppress ERK signaling leading to the elevation of Bim and reduction of Mcl-1 in AZD9291-resistant EGFR-mutant NSCLC cell lines. In the four AZD9291-resistant cell lines, HCC827/AR, PC-9/AR, PC-9/GR/AR and PC-9/3M, AZD9291 was unable to suppress ERK, Bim and Mcl-1 phosphorylation, increase Bim levels or decrease Mcl-1 levels (Fig. 4), further supporting the importance of suppressing ERK signaling and modulating Bim and Mcl-1 levels in determining cell sensitivity to AZD9291. Each one of three different MEK inhibitors, PD0325901, AZD6244 and GSK1120212, alone or in combination with AZD9291 effectively suppressed ERK, Bim and Mcl-1 phosphorylation accompanied with elevation of Bim and reduction of Mcl-1 in these resistant cell lines. The AZD9291 and AZD6244 combination was even more effective than either single agent in decreasing the levels of p-ERK, p-Bim, p-Mcl-1 and Mcl-1 and in elevating Bim in PC-9/GR/AR cells (Fig. 4B). Moreover, the combination of AZD9291 with GSK1120212 more potently decreased Mcl-1 levels in these resistant cell lines than did each agent alone (Fig. 4A). Interestingly, AZD9291 and GSK1120212 combination enhanced Bim elevation, but did not decrease the levels of both Mcl-1 and p-Mcl-1 in PC-9/3M cells (Fig. 4D), exhibiting a different action pattern. In general, these results confirm that MEK inhibition can effectively suppress ERK phosphorylation and its dependent phosphorylation of Bim and Mcl-1, resulting in Mcl-1 reduction and Bim elevation in these AZD9291-resistant EGFR-mutant NSCLC cell lines.
Fig. 4. MEK inhibitors effectively suppress the phosphorylation of ERK, Bim and Mcl-1 accompanied with elevation of Bim and reduction of Mcl-1 in AZD9291-resistant NSCLC cells.
The indicated cell lines were exposed to the tested agents alone or their combinations for 8 h and then harvested for preparation of whole-cell protein lysates and subsequent Western blotting to detect the given proteins. The concentrations used in A–C were 200 nM (AZD9291), 100 nM (AZD6244) and 25 nM (GSK1120212; GSK212), respectively. The concentrations used in D were 2 µM (AZD9291) and 100 nM (GSK212), respectively.
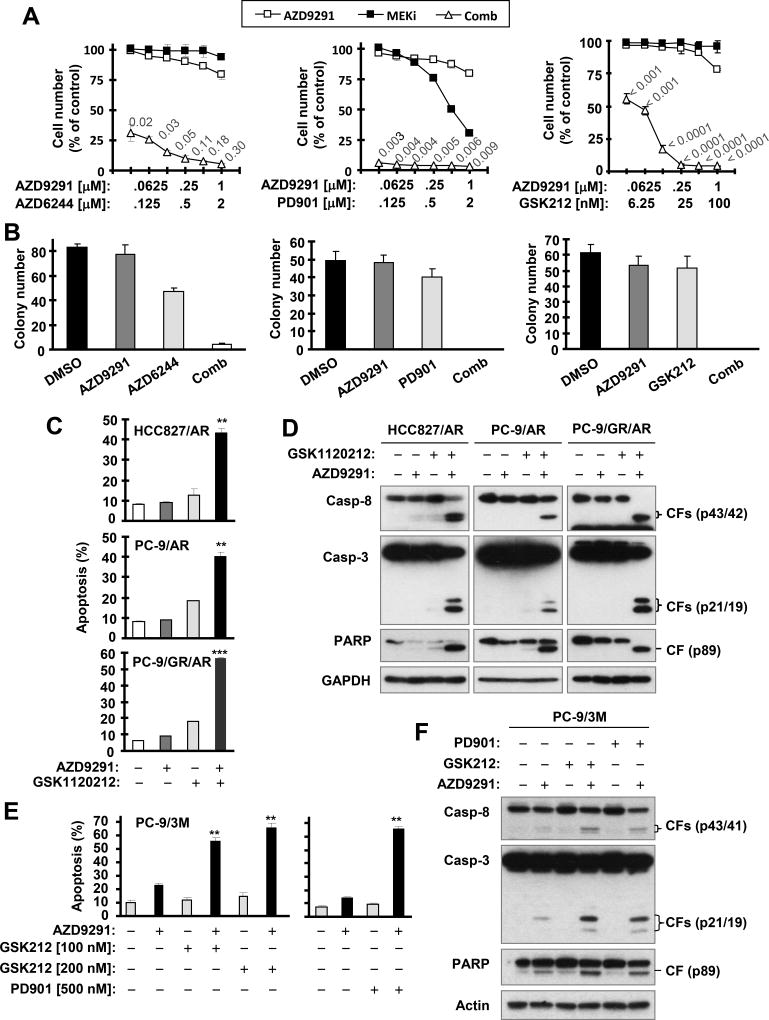
MEK inhibitors effectively overcome acquired resistance of EGFR-mutant NSCLC cells to AZD9291
We then determined whether MEK inhibition with a MEK inhibitor indeed restores the sensitivity of an AZD9291-resistant NSCLC cell line to AZD9291. The three MEK inhibitors, PD0325901, AZD9244 and GSK1120212, at the tested concentration ranges did not or only weakly suppressed the growth of PC-9/AR cells. As expected, this cell line was resistant to AZD9291. However the combination of AZD9291 with each one of the MEK inhibitors very effectively inhibited the growth of PC-9/AR cells (Fig. 5A). The CIs were far < 1, indicating highly synergistic growth inhibitory effects. Identical results were also generated in HCC827/AR, PC-9/GR/AR and PC-9/M cells (Figs. S5A and S6). In a long-term colony formation assay, we found that the combination of AZD9291 with each of the three MEK inhibitors eliminated colonies, whereas either agent alone weakly inhibited the formation and growth of colonies in PC-9/AR (Fig. 5B) and HCC827/AR cells (Fig. S5D). These results together demonstrate that MEK inhibitors restore sensitivity of AZD9291-resistant cells to AZD9291 or effectively overcome AZD9291 resistance.
Fig. 5. The combination of AZD9291 with a MEK inhibitor effectively inhibits the growth (A and B) and induces apoptosis (C–F) of AZD9291-resistant NSCLC cell lines.
A, PC-9/AR cells seeded in 96-well plates were exposed to varied concentrations of AZD9291 alone, the tested MEK inhibitor alone or their combinations for 3 days. Cell numbers were then estimated with SRB assay. The data are means ± SDs of four replicate determinations. The numbers in the graphs are CIs for different combinations. B, PC-9/AR cells seeded in 12-well plates were treated with 200 nM AZD9291, 100 nM (AZD6244) or 25 nM (PD0325901 and GSK1120212) tested MEK inhibitor or the combination of AZD9291 with a MEK inhibitor. Treatments were repeated every 3 days. After 12 days, the plates were stained for cell colonies with crystal violet dye. The colonies were then counted and representative pictures of colonies were taken with a digital camera. Columns represent means ± SDs of triplicate determinations. C–F, The indicated cell lines were exposed to 200 nM (C and D) or 2 µM (E and F) AZD9291 alone, 25 nM (C and D) or 100 nM (E and F) GSK1120212 alone, and the combination of AZD9291 with a MEK inhibitor for 24 h (HCC827/AR and PC-9/AR) or 48 h (PC-9/GR/AR and PC-9/3M). The cells were then harvested for annexin V staining followed with flow cytometric analysis to detect apoptosis (C and E) and for Western blotting to detect protein cleavage (D and F). Columns represent means ± SDs of duplicate determinations. CF, cleaved form. ** P < 0.01 at least compared with each tested agent alone; *** P < 0.001 at least compared with each tested agent alone.
The combination of AZD9291 with a MEK inhibitor effectively induces apoptosis of AZD9291-resistant NSCLC cells
Furthermore, we examined the effects of AZD9291 combined with a MEK inhibitor on the induction of apoptosis in AZD9291-resistant NSCLC cells. AZD9291 and GSK1120212 as single agents did not or minimally increased apoptotic cells (Fig. 5C) and induced cleavage of caspase-8, caspase-3 and PARP (Fig. 5D) in HCC827/AR, PC-9/AR and PC-9/GA/AR cells. However, their combination significantly increased apoptotic cell populations (Fig. 5C) and cleavage of caspase-8, caspase-3 and PARP (Fig. 5D) in these cell lines. Similar results were also obtained with the other two MEK inhibitors, PD0325901 and AZD6244, in these cell lines (Fig. S7). In the C797S mutant PC-9/3M cells, the combination of AZD9291 with GSK1120212 or PD-0325901 was also much more effective than either agent alone in inducing apoptosis including cleavage of capases and PARP (Figs. 5E and 5F). These results collectively demonstrate that the combination of AZD9291 with a MEK inhibitor potently induces apoptosis in AZD9291-resistant NSCLC cells.
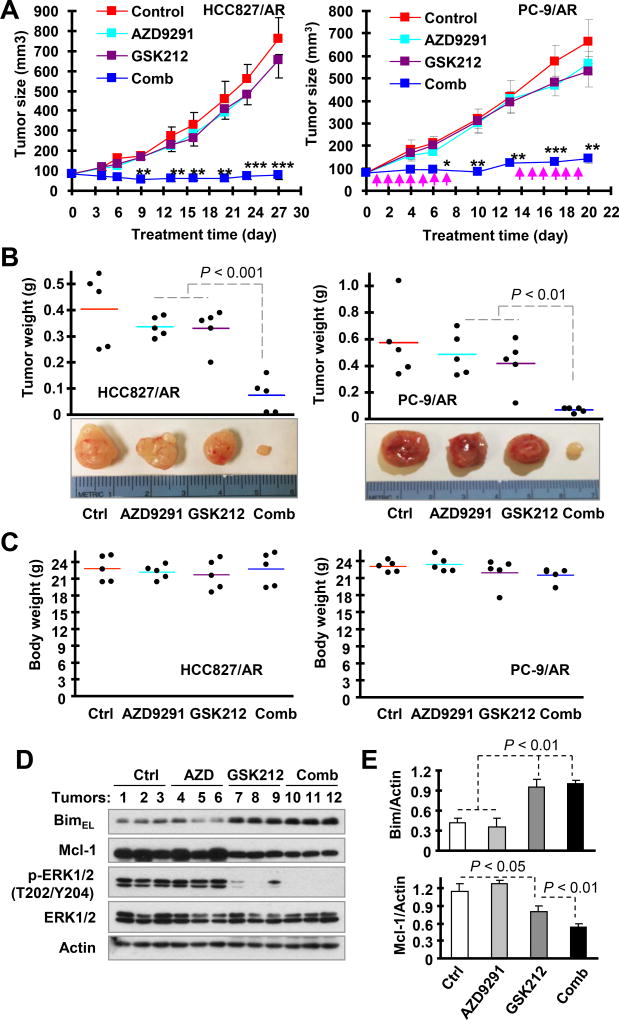
The combination of AZD9291 with GSK1120212 effectively inhibits the growth of AZD9291-resistant NSCLC xenografts in nude mice
Following these in vitro findings of the promising therapeutic activity of AZD9291 combined with a MEK inhibitor against AZD9291-resistant NSCLC cells, we then validated the efficacy of the combination in suppressing the growth of AZD9291-resistant xenograft tumors in vivo. As demonstrated in vitro, both AZD9291 and GSK1120122 alone when administered daily for almost 4 weeks had no or minimal effect on inhibiting the growth of HCC827/AR tumors; however their combination under the tested conditions significantly suppressed the growth of these xenografts (Figs. 6A and 6B; left panels) with no significant additive toxicity as measured by mouse body weight (Fig. 6C; left panel). In anticipation of possible increased toxicity when this combination is tested in human subjects with continuous dosing, we repeated the experiment with PC-9/AR xenografts where we employed an intermittent treatment schedule with one week on treatment, one week off treatment and followed with another week treatment and observed similar results (Figs. 6A–6C; right panels). Hence, it is clear that the combination effectively inhibits the growth of AZD9291-resistant tumors in vivo without apparent toxicity.
Fig. 6. The combination of AZD9291 and GSK1120212 effectively inhibits the growth of HCC827/AR and PC-9/AR xenografts in vivo (A and B) with limited toxicity (C) and modulation of Bim and Mcl-1 levels (D and E).
HCC827/AR or PC-9/AR xenografts were treated (once a day) with vehicle control, AZD9291, GSK1120212 (GSK212) and their combination starting on the same day after grouping for 27 consecutive days (HCC827/AR) or following the intermittent treatment schedules indicated by arrows for 3 weeks (PC-9/AR). Tumor sizes were measured as indicated (A). Each measurement is mean ± SEM (n = 5). At the end of the treatment, the mice were sacrificed and the tumors were removed and weighed (B). Mouse body weights were also compared (C). * P < 0.05 at least compared with all other groups; ** P < 0.01 at least compared with all other groups; *** P < 0.001 at least compared with all other groups. D and E, Whole-protein cell lysates were prepared randomly from 3 tumors in each group for Western blotting to detect the indicated proteins. Band intensities were quantified with NIH Image J software.
We also assessed p-ERK, Bim and Mcl-1 levels in xenograft tumors receiving the indicated treatments. In agreement with the in vitro findings, GSK1120212 alone significantly increased Bim levels with reduced levels of Mcl-1 and p-ERK whereas AZD9291 alone did not modulate the levels of these proteins. The combination of AZD9291 and GSK1120212 was not more potent than GSK1120212 in elevating Bim levels, but significantly decreased Mcl-1 levels (Figs. 6D and 6E). Hence we demonstrated the in vivo modulation of Bim and Mcl-1 levels by the combination of AZD9291 with a MEK inhibitor.
Discussion
The current study has clearly demonstrated that AZD9291 effectively induces apoptosis in EGFR-mutant NSCLC cell lines, but not in AZD9291-insensitive NSCLC cell lines with wild-type EGFR or with acquired resistance to AZD9291. Hence, the induction of apoptosis appears to be an important mechanism accounting for the therapeutic efficacy of AZD9291 against EGFR-mutant NSCLCs. Our findings that AZD9291 elevates Bim levels and reduces Mcl-1 levels in the sensitive EGFR-mutant NSCLC cells, but not in AZD9291-insenstive or resistant cell lines including PC-9/AR, PC-9/GR/GR, PC-9/3M, HCC827/AR and HCC827/ER strongly suggest that the modulation of both Bim and Mcl-1 levels is a critical event that mediates AZD9291-induced apoptosis (Fig. 3G). This is supported by our findings that either blockade of Bim elevation or enforced expression of ectopic Mcl-1 in the sensitive EGFR-mutant NSCLC cells significantly protects them from undergoing AZD9291-induced apoptosis. Hence, the essential role of Bim elevation in mediating AZD9291-induced apoptosis is consistent with its role in mediating apoptosis induced by 1st generation EGFR inhibitors such as erlotinib, as previously documented (29–31). In addition to this mechanism, our current study has revealed another equally important mechanism: the essential role of Mcl-1 reduction in mediating AZD9291-induced apoptosis in EGFR-mutant NSCLC cells.
In addition to increased intensity, we noted that the BimEL band was shifted with faster migration in AZD9291-treated cells than in control cells, suggesting possible posttranslational modification. Bim is known to be phosphorylated by ERK at S69, undergoing proteasome-dependent degradation (25,32). Indeed, AZD9291 elevated Bim levels accompanied with suppression of ERK and Bim S69 phosphorylation. In contrast to a previous study where erlotinib-induced Bim elevation could be inhibited by Act D (31), there was no effect of Act D on Bim elevation induced by AZD9291 in our study (Fig. 2B). Rather, AZD9291 clearly suppressed Bim degradation as evaluated in the CHX chase assay (Fig. 2A). Therefore we conclude that AZD9291 increases Bim levels by suppressing ERK-dependent phosphorylation and degradation of Bim (Fig. 3G). In contrast to Bim, ERK phosphorylates Mcl-1 at T163, suppressing its degradation (26–28). We found that AZD9291 decreased Mcl-1 levels accompanied with suppression of Mcl-1 phosphorylation at S159/T163 (Fig. 1). Moreover, AZD9291 enhanced the rate of Mcl-1 degradation (Fig. 2C) and inhibition of the proteasome with MG132 rescued the reduction in Mcl-1 induced by AZD9291 (Fig. 2D). Hence we suggest that AZD9291 decreases Mcl-1 levels through enhanced ERK-dependent degradation (Fig. 3G). This model of modulation of Bim and Mcl-1 degradation is also supported by the findings that different MEK inhibitors effectively elevate Bim levels and reduce Mcl-1 levels accompanied by suppression of ERK, Bim S69 and Mcl-1 S159/T163 phosphorylation in AZD9291-resistant EGFR-mutant NSCLC cells (Fig. 4). Hence our findings in this regard have provided a novel mechanism for AZD9291 modulation of Bim and Mcl-1 levels, resulting in induction of apoptosis (Fig. 3G).
Accordingly, the inability of AZD9291 to alter Bim and Mcl-1 levels by modulating ERK-dependent Bim and Mcl-1 degradation AZD9291-resistant cells represents a critical mechanism by which sensitive EGFR-mutant NSCLC cells could become resistant to apoptosis induction by AZD9291. This mechanism is clearly independent of different genetic alterations including c-Met amplification, C797S mutation and unknown changes because it happens in the tested resistance cell lines with varied genetic alterations. Currently we do not know why the MEK/ERK singling pathway in AZD9291-resistant cell lines becomes irresponsive to AZD9291 treatment, but will address this question as a future direction. Nonetheless, we do provide a therapeutic strategy based on this feature of AZD9291-resistant cells to overcome the resistance by co-targeting MEK/ERK signaling. By elevating Bim levels and reducing Mcl-1 levels through suppression of ERK-dependent phosphorylation of Bim and Mcl-1 with a MEK inhibitor, we could restore the sensitivity of AZD9291-resistant EGFR-mutant NSCLC cells to undergo apoptotic death, achieving promising therapeutic efficacy against the growth of AZD9291-resistant NSCLC cells both in vitro and in vivo (Figs. 5, 6, S3–S5). We generated identical results with 3 different MEK inhibitors, thus demonstrating the rationale for overcoming AZD9291 resistance by targeting MEK/ERK signaling. There are previous studies documenting the efficacy of a third generation EGFR inhibitor combined with a MEK inhibitor (e.g., AZD9291 plus AZD6244 or WZ4002 plus GSK1120212) on the growth of EGFR-mutant/T790M NSCLC cells and tumors (33,34). However, these studies primarily focused on preventing or delaying the development of resistance to AZD9291 or to WZ4002 by blockade of activated Ras signaling during AZD9291 treatment (33) or ERK reactivation (34). Moreover, the underlying scientific rationales are clearly different. We believe that MEK inhibition lowers the threshold for NSCLC cells with acquired resistance to AZD9291 to re-respond to AZD9291 therapy.
We noted that the combinations of AZD9291 with different MEK inhibitors in general enhanced Mcl-1 reduction in different resistant cell lines (Fig. 4) and in vivo tumors (Fig. 6) in comparison with MEK inhibitors alone, while they had no such effects on further elevating Bim levels. Hence it seems that Mcl-1 reduction plays a more important role than Bim elevation in mediating enhanced induction of apoptosis by the combinations in the resistant cell lines. In agreement, either GSK1120212 or its combination with AZD9291 failed to reduce Mcl-1 levels although they elevated Bim levels in the C797S mutant PC-9/3M cells (Fig. 4D), in which the AZD9291 and GSK1120212 combination exhibited a relatively weak enhanced effect on decreasing cell survival (Fig. S6). Nonetheless, the enhanced reduction of Mcl-1 levels will lead to enhanced ratio change of Bim to Mcl-1 (Bim:Mcl-1) in a given resistant cell line and finally augmented induction of apoptosis and suppression of tumor growth.
We have recently shown that MET inhibition with a MET inhibitor overcomes acquired resistance to AZD9291 in HCC827 cells with acquired resistance to either erlotinib (i.e., HCC827/ER) or AZD9291 (i.e., HCC827/AR), which exhibit both MET gene amplification and hyperactivate MET protein, suggesting an effective strategy to treat EGFR-mutant NSCLCs that develop resistance to 3rd generation EGFR inhibitors through MET amplification and protein hyperactivation mechanisms (14). Our data show that the combination of AZD9291 and the MET inhibitor PF02341066 exhibited minimally enhanced suppression of the growth of PC-9/AR and PC-9/GR/AR cells (Fig. S8). Thus this strategy is ineffective in treating resistant EGFR-mutant NSCLCs that arise through other mechanisms. However the combination of AZD9291 with a MEK inhibitor works equally well against the growth of AZD9291-resistant EGFR-mutant NSCLC cell lines with MET amplification (e.g., HCC827/AR), C797S mutation (e.g., PC-9/3M) or unknown mechanisms (e.g., PC-9/AR and PC-9/GR/AR). This strategy therefore has a clear advantage over the strategy of combining AZD9291 with a MET inhibitor in overcoming resistance to 3rd generation EGFR inhibitors regardless of the underlying mechanisms. Therefore clinical validation of this strategy to overcome resistance to 3rd generation EGFR inhibitors is clearly justified. In this regard, our findings are clearly different from a previous study reporting that the combination of WZ4002 with GSK1120212 was ineffective in EGFR-mutant NSCLC cell lines with non-T790M TKI resistance mechanisms (e.g., Met amplification or activation) (34). There are two layers of major differences between our and the published studies: 1) different 3rd generation EGFR inhibitors were used (AZD9291 versus WZ4002) and 2) different cell lines were used. Here we used different AZD9291-resistant NSCLC cell lines generated from their corresponding sensitive EGFR-mutant NSCLC cell lines, whereas the published study used only resistant cell lines to 1st or 2nd generation EGFR-TKIs. We are now planning a clinical trial to test the efficacy of AZD9291 and GSK1120212 combination on overcoming AZD9291 resistance as well as on preventing or delaying development of resistance to AZD9291.
In this study, we noted that AZD9291 effectively activated caspase-8 by inducing its cleavage in the sensitive EGFR-mutated NSCLC cell lines (Fig. 1C). In agreement, the combination of AZD9291 with the tested MEK inhibitors (e.g., GSK1120212) strongly induced caspase-8 cleavage as well (Figs. 5D and S4B). The underlying mechanism for AZD9291 activation of caspase-8 has not been addressed in this study. Caspase-8 has long been recognized as an initiator caspase that mediates the extrinsic apoptotic pathway (35). A previous study even showed that knockdown of Fas, a well-known death receptor that initiates apoptosis upon activation, sensitized insensitive EGFR-mutant NSCLC cells to the 1st generation EGFR inhibitor erlotinib (36). Nonetheless, whether activation of the death receptor-mediated extrinsic apoptotic pathway is involved in mediating apoptosis by AZD9291 or its combination with a MEK inhibitor in EGFR-mutant NSCLC cells deserves further investigation and hence is our ongoing focus.
In contrast to AZD9291, we noted that the three different MEK inhibitors alone at the tested conditions only weakly suppressed the growth of ADZ9291-resistant NSCLC cell lines including induction of apoptosis although they effectively elevated Bim and decreased Mcl-1 levels (Figs. 4 and 5). So did GSK1120212 in vivo (Fig. 6). These results suggest that the modulation of Bim and Mcl-1 levels alone may not be sufficient to trigger massive apoptotic cell death that will result in effective growth suppression in AZD9291-resistant NSCLC cells. Hence it is very likely that additional mechanisms beyond the modulation of Bim and Mcl-1 may also exist to account for the induction of apoptosis by AZD9291 in the sensitive EGFR-mutant NSCLC cells (Fig. 3G) or by the combination of AZD9291 with a MEK inhibitor in AZD9291-resistant NSCLC cell lines. Further study in this direction is also warranted.
In summary, the current study has demonstrated the critical role of Bim and Mcl-1 modulation in mediating the induction of apoptosis by AZD9291 in sensitive EGFR-mutant NSCLC cell lines. Based on this important finding, we suggest that co-targeting MEK/ERK signaling will be an effective therapeutic strategy to overcome acquired resistance to AZD9291, and likely to other 3rd generation EGFR inhibitors.
Supplementary Material
Translational relevance.
Development of acquired resistance to AZD9291, an approved 3rd generation EGFR inhibitor for treatment of EGFR-mutant non-small cell lung cancer with T790M mutation has become a major obstacle in the clinic for a long-term efficacy. Hence effective strategies that can overcome the acquired resistance are urgently needed clinically. Our finding in this study on the critical role of modulation of MEK/ERK-dependent Bim and Mcl-1 degradation in mediating sensitivity and resistance to AZD9291 provides a strong rationale for the clinical investigation of the combination of AZD9219 with a MEK inhibitor as a strategy to overcome acquired resistance to AZD9291 or other 3rd generation EGFR inhibitors.
Acknowledgments
We are grateful to Drs. P. A. Jänne, R. Lotan and A. N. Hata for providing some cell lines. We also thank Dr. A. Hammond in our department for editing the manuscript.
Grant Support: NIH/NCI R01 CA160522 (to SYS), R01 CA118450 (to SYS) and K23 CA164015 (to TKO), 2016 Friends of Winship Fashion Research Scholars Award (to SSR), Winship Invest$/lung cancer pilot award (SYS) and China Scholarship Council (to PS).
Abbreviations
- NSCLC
non-small cell lung cancer
- EGFR
epidermal grwoth factor receptor
- EGFR-TKIs
EGFR-tyrosine kinase inhibitors
- CI
combination index
- Act D
actinomycin D
- CHX
cycloheximide
- siRNA
small-interfering RNA
- shRNA
short-hairpin RNA
Footnotes
Note: SSR, TKO and SYS are Georgia Research Alliance Distinguished Cancer Scientists.
References
- 1.Tartarone A, Lerose R. Clinical approaches to treat patients with non-small cell lung cancer and epidermal growth factor receptor tyrosine kinase inhibitor acquired resistance. Therapeutic advances in respiratory disease. 2015;9:242–50. doi: 10.1177/1753465815587820. [DOI] [PubMed] [Google Scholar]
- 2.Juchum M, Gunther M, Laufer SA. Fighting cancer drug resistance: Opportunities and challenges for mutation-specific EGFR inhibitors. Drug resistance updates : reviews and commentaries in antimicrobial and anticancer chemotherapy. 2015;20:10–28. doi: 10.1016/j.drup.2015.05.002. [DOI] [PubMed] [Google Scholar]
- 3.Remon J, Moran T, Majem M, Reguart N, Dalmau E, Marquez-Medina D, et al. Acquired resistance to epidermal growth factor receptor tyrosine kinase inhibitors in EGFR-mutant non-small cell lung cancer: A new era begins. Cancer Treat Rev. 2014;40:93–101. doi: 10.1016/j.ctrv.2013.06.002. [DOI] [PubMed] [Google Scholar]
- 4.Engelman JA, Zejnullahu K, Mitsudomi T, Song Y, Hyland C, Park JO, et al. MET amplification leads to gefitinib resistance in lung cancer by activating ERBB3 signaling. Science. 2007;316:1039–43. doi: 10.1126/science.1141478. [DOI] [PubMed] [Google Scholar]
- 5.Suda K, Murakami I, Katayama T, Tomizawa K, Osada H, Sekido Y, et al. Reciprocal and complementary role of MET amplification and EGFR T790M mutation in acquired resistance to kinase inhibitors in lung cancer. Clin Cancer Res. 2010;16:5489–98. doi: 10.1158/1078-0432.CCR-10-1371. [DOI] [PubMed] [Google Scholar]
- 6.Pirker R. Third-generation epidermal growth factor receptor tyrosine kinase inhibitors in advanced nonsmall cell lung cancer. Current opinion in oncology. 2016;28:115–21. doi: 10.1097/CCO.0000000000000260. [DOI] [PubMed] [Google Scholar]
- 7.Barnes TA, O'Kane GM, Vincent MD, Leighl NB. Third-Generation Tyrosine Kinase Inhibitors Targeting Epidermal Growth Factor Receptor Mutations in Non-Small Cell Lung Cancer. Frontiers in oncology. 2017;7:113. doi: 10.3389/fonc.2017.00113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Janne PA, Yang JC, Kim DW, Planchard D, Ohe Y, Ramalingam SS, et al. AZD9291 in EGFR inhibitor-resistant non-small-cell lung cancer. N Engl J Med. 2015;372:1689–99. doi: 10.1056/NEJMoa1411817. [DOI] [PubMed] [Google Scholar]
- 9.Sequist LV, Soria JC, Goldman JW, Wakelee HA, Gadgeel SM, Varga A, et al. Rociletinib in EGFR-mutated non-small-cell lung cancer. N Engl J Med. 2015;372:1700–9. doi: 10.1056/NEJMoa1413654. [DOI] [PubMed] [Google Scholar]
- 10.Thress KS, Paweletz CP, Felip E, Cho BC, Stetson D, Dougherty B, et al. Acquired EGFR C797S mutation mediates resistance to AZD9291 in non-small cell lung cancer harboring EGFR T790M. Nat Med. 2015;21:560–2. doi: 10.1038/nm.3854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ercan D, Choi HG, Yun CH, Capelletti M, Xie T, Eck MJ, et al. EGFR mutations and resistance to Irreversible pyrimidine based EGFR inhibitors. Clin Cancer Res. 2015;21:3913–23. doi: 10.1158/1078-0432.CCR-14-2789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Niederst MJ, Hu H, Mulvey HE, Lockerman EL, Garcia AR, Piotrowska Z, et al. The allelic context of the C797S mutation acquired upon treatment with third generation EGFR inhibitors impacts sensitivity to subsequent treatment strategies. Clin Cancer Res. 2015;21:3924–33. doi: 10.1158/1078-0432.CCR-15-0560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chabon JJ, Simmons AD, Lovejoy AF, Esfahani MS, Newman AM, Haringsma HJ, et al. Circulating tumour DNA profiling reveals heterogeneity of EGFR inhibitor resistance mechanisms in lung cancer patients. Nature communications. 2016;7:11815. doi: 10.1038/ncomms11815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shi P, Oh YT, Zhang G, Yao W, Yue P, Li Y, et al. Met gene amplification and protein hyperactivation is a mechanism of resistance to both first and third generation EGFR inhibitors in lung cancer treatment. Cancer Lett. 2016;380:494–504. doi: 10.1016/j.canlet.2016.07.021. [DOI] [PubMed] [Google Scholar]
- 15.Ou SH, Agarwal N, Ali SM. High MET amplification level as a resistance mechanism to osimertinib (AZD9291) in a patient that symptomatically responded to crizotinib treatment post-osimertinib progression. Lung Cancer. 2016;98:59–61. doi: 10.1016/j.lungcan.2016.05.015. [DOI] [PubMed] [Google Scholar]
- 16.Ortiz-Cuaran S, Scheffler M, Plenker D, Dahmen I, Scheel A, Fernandez-Cuesta L, et al. Heterogeneous mechanisms of primary and acquired resistance to third-generation EGFR inhibitors. Clin Cancer Res. 2016 doi: 10.1158/1078-0432.CCR-15-1915. [DOI] [PubMed] [Google Scholar]
- 17.Li Y, Fan S, Koo J, Yue P, Chen ZG, Owonikoko TK, et al. Elevated expression of eukaryotic translation initiation factor 4E is associated with proliferation, invasion and acquired resistance to erlotinib in lung cancer. Cancer Biol Ther. 2012;13:272–80. doi: 10.4161/cbt.18923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ren H, Zhao L, Li Y, Yue P, Deng X, Owonikoko TK, et al. The PI3 kinase inhibitor NVP-BKM120 induces GSK3/FBXW7-dependent Mcl-1 degradation, contributing to induction of apoptosis and enhancement of TRAIL-induced apoptosis. Cancer Lett. 2013;338:229–38. doi: 10.1016/j.canlet.2013.03.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sun SY, Yue P, Dawson MI, Shroot B, Michel S, Lamph WW, et al. Differential effects of synthetic nuclear retinoid receptor-selective retinoids on the growth of human non-small cell lung carcinoma cells. Cancer Res. 1997;57:4931–9. [PubMed] [Google Scholar]
- 20.Wang X, Hawk N, Yue P, Kauh J, Ramalingam SS, Fu H, et al. Overcoming mTOR inhibition-induced paradoxical activation of survival signaling pathways enhances mTOR inhibitors' anticancer efficacy. Cancer Biol Ther. 2008;7:1952–8. doi: 10.4161/cbt.7.12.6944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Liu X, Yue P, Zhou Z, Khuri FR, Sun SY. Death receptor regulation and celecoxib-induced apoptosis in human lung cancer cells. J Natl Cancer Inst. 2004;96:1769–80. doi: 10.1093/jnci/djh322. [DOI] [PubMed] [Google Scholar]
- 22.Sun SY, Yue P, Wu GS, El-Deiry WS, Shroot B, Hong WK, et al. Mechanisms of apoptosis induced by the synthetic retinoid CD437 in human non-small cell lung carcinoma cells. Oncogene. 1999;18:2357–65. doi: 10.1038/sj.onc.1202543. [DOI] [PubMed] [Google Scholar]
- 23.Ley R, Ewings KE, Hadfield K, Cook SJ. Regulatory phosphorylation of Bim: sorting out the ERK from the JNK. Cell Death Differ. 2005;12:1008–14. doi: 10.1038/sj.cdd.4401688. [DOI] [PubMed] [Google Scholar]
- 24.Ley R, Ewings KE, Hadfield K, Howes E, Balmanno K, Cook SJ. Extracellular signal-regulated kinases 1/2 are serum-stimulated "Bim(EL) kinases" that bind to the BH3-only protein Bim(EL) causing its phosphorylation and turnover. J Biol Chem. 2004;279:8837–47. doi: 10.1074/jbc.M311578200. [DOI] [PubMed] [Google Scholar]
- 25.Ley R, Balmanno K, Hadfield K, Weston C, Cook SJ. Activation of the ERK1/2 signaling pathway promotes phosphorylation and proteasome-dependent degradation of the BH3-only protein, Bim. J Biol Chem. 2003;278:18811–6. doi: 10.1074/jbc.M301010200. [DOI] [PubMed] [Google Scholar]
- 26.Nifoussi SK, Vrana JA, Domina AM, De Biasio A, Gui J, Gregory MA, et al. Thr 163 phosphorylation causes Mcl-1 stabilization when degradation is independent of the adjacent GSK3-targeted phosphodegron, promoting drug resistance in cancer. PLoS One. 2012;7:e47060. doi: 10.1371/journal.pone.0047060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Domina AM, Vrana JA, Gregory MA, Hann SR, Craig RW. MCL1 is phosphorylated in the PEST region and stabilized upon ERK activation in viable cells, and at additional sites with cytotoxic okadaic acid or taxol. Oncogene. 2004;23:5301–15. doi: 10.1038/sj.onc.1207692. [DOI] [PubMed] [Google Scholar]
- 28.Ding Q, Huo L, Yang JY, Xia W, Wei Y, Liao Y, et al. Down-regulation of myeloid cell leukemia-1 through inhibiting Erk/Pin 1 pathway by sorafenib facilitates chemosensitization in breast cancer. Cancer Res. 2008;68:6109–17. doi: 10.1158/0008-5472.CAN-08-0579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Costa DB, Halmos B, Kumar A, Schumer ST, Huberman MS, Boggon TJ, et al. BIM mediates EGFR tyrosine kinase inhibitor-induced apoptosis in lung cancers with oncogenic EGFR mutations. PLoS medicine. 2007;4:1669–79. doi: 10.1371/journal.pmed.0040315. discussion 80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cragg MS, Kuroda J, Puthalakath H, Huang DC, Strasser A. Gefitinib-induced killing of NSCLC cell lines expressing mutant EGFR requires BIM and can be enhanced by BH3 mimetics. PLoS medicine. 2007;4:1681–89. doi: 10.1371/journal.pmed.0040316. discussion 90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gong Y, Somwar R, Politi K, Balak M, Chmielecki J, Jiang X, et al. Induction of BIM is essential for apoptosis triggered by EGFR kinase inhibitors in mutant EGFR-dependent lung adenocarcinomas. PLoS medicine. 2007;4:e294. doi: 10.1371/journal.pmed.0040294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Luciano F, Jacquel A, Colosetti P, Herrant M, Cagnol S, Pages G, et al. Phosphorylation of Bim-EL by Erk1/2 on serine 69 promotes its degradation via the proteasome pathway and regulates its proapoptotic function. Oncogene. 2003;22:6785–93. doi: 10.1038/sj.onc.1206792. [DOI] [PubMed] [Google Scholar]
- 33.Eberlein CA, Stetson D, Markovets AA, Al-Kadhimi KJ, Lai Z, Fisher PR, et al. Acquired Resistance to the Mutant-Selective EGFR Inhibitor AZD9291 Is Associated with Increased Dependence on RAS Signaling in Preclinical Models. Cancer Res. 2015;75:2489–500. doi: 10.1158/0008-5472.CAN-14-3167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tricker EM, Xu C, Uddin S, Capelletti M, Ercan D, Ogino A, et al. Combined EGFR/MEK Inhibition Prevents the Emergence of Resistance in EGFR mutant Lung Cancer. Cancer Discov. 2015 doi: 10.1158/2159-8290.CD-15-0063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kruidering M, Evan GI. Caspase-8 in apoptosis: the beginning of "the end"? IUBMB Life. 2000;50:85–90. doi: 10.1080/713803693. [DOI] [PubMed] [Google Scholar]
- 36.Bivona TG, Hieronymus H, Parker J, Chang K, Taron M, Rosell R, et al. FAS and NF-kappaB signalling modulate dependence of lung cancers on mutant EGFR. Nature. 2011;471:523–6. doi: 10.1038/nature09870. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.