Abstract
Objective
To estimate the rate, characteristics and dispositions of hypoglycemia events among persons who received care from Alameda County, California, Emergency Medical Services (EMS).
Methods
This study was based on data for 601,077 Alameda County EMS encounters during 2013–2015. Subjects were defined as having hypoglycemia if EMS personnel recorded a primary impression of hypoglycemia or low blood glucose (<60 mg/dl or “unspecified low”). The outcome of interest was patient transport or non-transport to an emergency department or other care setting; we excluded 33,177 (6%) encounters which lacked clear disposition outcomes.
Results
Among 567,900 eligible encounters, 8,332 (1.47%) were attributed to hypoglycemia, of which 1,125 (13.5%) were not transported. Non-transport was more likely among males, adult patients age <60, initial blood glucose >60 mg/dl or EMS arrival time 18:00 – 6:00.
Conclusions
Without an understanding of EMS encounters and non-transport rates, surveillance based solely on emergency department and hospital data will significantly underestimate rates of severe hypoglycemia. Additionally, given that hypoglycemia is often safely and effectively treated by non-physicians, EMS protocols should provide guidance for non-transport of hypoglycemic patients whose blood glucose levels have normalized.
Keywords: hypoglycemia, blood glucose, diabetes mellitus, public health surveillance, emergency medical services, transportation of patients
Introduction
Hypoglycemia is a common, unintended consequence of glucose-lowering treatment and has become a public health and drug safety concern.1–3 Severe hypoglycemia is defined as a low blood glucose event requiring assistance from another person.4 Severe hypoglycemia has been associated with significant morbidity (poor quality of life,5 serious falls and car accidents,6 ventricular arrhythmia,7 dementia,8 hospitalizations9) and mortality.10,11 Surveillance based on emergency department (ED) or hospital utilization fails to capture up to 95% of hypoglycemic events that occur outside of medical settings, including events for which assistance is typically rendered by family members, other caregivers, or emergency medical services (EMS) personnel.12,13 In the context of EMS encounters, all hypoglycemia events are “severe” by definition since assistance was provided.
Limited data exist on the characteristics of EMS encounters for hypoglycemia and the rate at which patients are transported to the ED. Since most current surveillance methods rely on claims data, patients who are treated by EMS but not transported to the ED are not typically captured in U.S. surveillance of hypoglycemia. Understanding the rate and factors associated with non-transport by EMS are thus vitally important to improving the completeness of hypoglycemia surveillance.
Local EMS protocols vary widely and often determine the likelihood of transport to the ED. A recent study of pre-hospital protocols for hypoglycemia from 185 U.S. EMS agencies found that less than half (49%) permitted non-transport of patients whose hypoglycemia had been corrected.14 However, the actual rates of transport are not known. An EMS encounter for a patient with hypoglycemia is typically initiated by a call to a “911” call center which may dispatch fire department emergency medical technicians, paramedics or an ambulance. Care is provided by the first personnel to arrive on the scene; if indicated and depending on the local EMS protocol, the patient may be treated or transported by ambulance to an ED or another care setting.
We conducted of study of hypoglycemia events encountered by a local EMS agency with a robust data collection system that serves a large and diverse population. This paper will describe the rate, characteristics and disposition of hypoglycemia events among patients who received care from Alameda County Emergency Medical Services (ALCO EMS) during 2013–2015.
Research Design and Methods
Setting
Alameda County is an urban/suburban county in Northern California, 737 square miles in area with a population of 1.6 million. ALCO EMS prescribes county-wide response, treatment and transport protocols, and ongoing quality oversight and improvement strategies. Paramedic-staffed first response engines and transport ambulances respond to approximately 150,000 EMS calls and transport 115,000 patients each year.
Paramedics in the ALCO EMS system use a point of care instrument to measure the blood glucose for those patients with abnormal mentation and for those with other symptoms of hypoglycemia. Prehospital protocols allow the treatment of hypoglycemia with intravenous dextrose, oral dextrose, or intramuscular glucagon.
ALCO EMS paramedics are empowered to allow patients with normal mental capacity to refuse further medical care against EMS advice. The practice is to encourage transport to the nearest emergency department, but in the setting of an appropriate non-transport, paramedics are encouraged to be certain that the patient is accompanied and can tolerate eating. The paramedic often consults with a base physician regarding specific medical cases.
Data Sources
ALCO EMS maintains a database of all EMS encounters by first responders or ambulance transport; encounter records include data such as location, date and time of encounter, patient sex and date of birth, findings (e.g. glucose test results, primary impression), procedures performed (e.g., oral dextrose administered) and disposition (transport or non-transport to an ED or other care setting). This study was based on data for 601,077 Alameda County EMS encounters during 2013–2015.
Encounters were defined as hypoglycemia if EMS personnel recorded a primary impression of hypoglycemia or a low blood glucose (<60 mg/dl (the cutpoint used in ALCO EMS protocols) or “unspecified low”).
The outcome of interest was patient transport or non-transport to an emergency department or other care setting; thus, we excluded 33,177 (6%) encounters which lacked clear disposition outcomes (unknown/missing, died at scene, no patient found, or flight crew return).
This study was approved by the Kaiser Permanente Northern California (KPNC) Institutional Review Board and was supported by funding from NIH (R01 DK103721).
Results
Among 567,900 eligible encounters, 8,332 (1.47%) were identified as hypoglycemia; 1,125 (13.5%) were not transported. (Table 1) Non-transport was more likely among males, adult patients age <60, initial blood glucose >60 mg/dl, and EMS arrival time 18:00 – 6:00.
Table 1.
Characteristics of Alameda County Emergency Services encounters (2013–2015) for hypoglycemia events, stratified by disposition (N with column % unless otherwise indicated)
| Disposition | ||||
|---|---|---|---|---|
| ALL | Transported | Not transported | p-valuea | |
| All, N (row %) | 8,332 | 7,207 (86.4) | 1,125 (13.5) | |
| Race/ethnicity | 0.20 | |||
| African American | 808 (9.7) | 720 (10.0) | 88 (7.8) | |
| Asian/Filipino | 230 (2.8) | 197 (2.7) | 33 (2.9) | |
| White | 819 (9.8) | 712 (9.9) | 107 (9.5) | |
| Other | 223 (2.7) | 189 (2.6) | 34 (3.0) | |
| Missing/unknown | 6252 (75.0) | 5389 (74.8) | 863 (76.7) | |
| Sex | <0.0001 | |||
| Female | 3692 (44.3) | 3256 (45.2) | 436 (38.8) | |
| Male | 4634 (55.6) | 3949 (54.8) | 685 (60.9) | |
| Unknown | 6 (0.1) | 2 (0.0) | 4 (0.4) | |
| Age (years) | <0.0001 | |||
| 0–18 | 90 (1.1) | 81 (1.1) | 9 (0.8) | |
| 19–39 | 902 (10.8) | 704 (9.8) | 198 (17.6) | |
| 40–59 | 2309 (27.7) | 1906 (26.5) | 403 (35.8) | |
| 60–75 | 2932 (35.2) | 2549 (35.4) | 383 (34.0) | |
| >75 | 2094 (25.1) | 1966 (27.3) | 128 (11.4) | |
| Missing | 5 (0.1) | 1 (0.0) | 4 (0.4) | |
| Primary impression | <0.0001 | |||
| Hypoglycemia | 6515 (78.2) | 5538 (76.8) | 977 (86.8) | |
| Missing/none | 168 (2.0) | 116 (1.6) | 52 (4.6) | |
| Altered level of consciousness (Not hypoglycemia or seizure) | 299 (3.6) | 285 (3.9) | 14 (1.2) | |
| General weakness | 238 (2.9) | 223 (3.1) | 15 (1.3) | |
| Cardiac arrest | 75 (0.9) | 74 (1.0) | 1 (0.1) | |
| Hyperglycemia | 93 (1.1) | 79 (1.1) | 14 (1.2) | |
| Seizure | 73 (0.9) | 69 (1.0) | 4 (0.4) | |
| Syncope/near syncope | 73 (0.9) | 64 (0.9) | 9 (0.8) | |
| Dizziness/vertigo | 43 (0.5) | 38 (0.5) | 5 (0.4) | |
| Abdominal pain/problems | 68 (0.8) | 66 (0.9) | 2 (0.2) | |
| Traumatic injury - non-activation | 67 (0.8) | 64 (0.9) | 3 (0.3) | |
| Behavioral/psychiatric crisis | 65(0.8) | 64 (0.9) | 1 (0.1) | |
| All other primary impressions | 555 (6.7) | 527 (7.3) | 28 (2.5) | |
| First EMS Blood Glucose (mg/dL) - Categorical | <0.0001 | |||
| <60 (includes “unspecified low”) | 7276 (87.3) | 6362 (88.3) | 914 (81.2) | |
| ≥60 | 775 (9.3) | 604 (8.4) | 171 (15.2) | |
| Missing | 281 (3.4) | 241 (3.3) | 40 (3.6) | |
| Medications (not mutually exclusive) | ||||
| Dextrose 10%b | 1205 (14.5) | 1081 (15.0) | 124 (11.0) | <0.001 |
| Dextrose 25% | 10 (0.1) | 9 (0.12) | 1 (0.1) | 0.75 |
| Dextrose 50%b | 2890 (35.7) | 2536 (35.2) | 354 (31.5) | 0.015 |
| Glucose paste | 0 | 0 | 0 | N/A |
| Glucagon | 1 (0.0) | 1 (0.0) | 0 | 1.00 |
| Pickup location | <0.0001 | |||
| Assisted living/nursing home | 650 (7.8) | 636 (8.8) | 14 (1.2) | |
| Clinic | 156 (1.9) | 146 (2.0) | 10 (0.9) | |
| Home/residence | 5903 (70.9) | 5170 (71.7) | 733 (65.2) | |
| Place of business/school | 741 (8.9) | 574 (8.0) | 167 (14.8) | |
| Street/highway | 517 (6.2) | 464 (6.4) | 53 (4.7) | |
| Other | 222 (2.7) | 184 (2.6) | 38 (3.4) | |
| Missing | 143 (1.7) | 33 (0.5) | 110 (9.8) | |
| Transport destination | ||||
| ED/Hospital | 5680 (78.8) | |||
| Medical office/clinic | 0 | |||
| Home | 0 | |||
| Other | 2 (0.0) | |||
| None | 7 (0.1) | |||
| Missing | 1518 (21.1) | |||
| Alcohol use (yes) | 125 (1.5) | 119 (1.7) | 6 (0.5) | 0.004 |
| EMS Arrival Time | <0.001 | |||
| midnight-5:59 | 1530 (18.4) | 1297 (18.0) | 233 (20.7) | |
| 6:00–11:59 | 2266 (27.2) | 2009 (27.9) | 257 (22.8) | |
| 12:00–17:59 | 2492 (29.9) | 2169 (30.1) | 323 (28.7) | |
| 18:00–23:59 | 2044 (24.5) | 1732 (24.0) | 312 (27.7) | |
Chi-Square for category or row
During the course of this study (2015), the standard intravenous dextrose concentration was changed from a 50% to a 10% solution.
There was imperfect agreement between a primary impression of hypoglycemia and documented low blood glucose (Table 2). Among the 6,515 encounters with a primary impression of hypoglycemia, 5,459 (83.8%) also had documented low blood glucose. In the remaining 1,056 (16.2%) encounters which did not have documented low blood glucose, the patients may have received assistance prior to EMS arrival, had “probable symptomatic hypoglycemia”4 (i.e., symptoms but no documented blood glucose) or had “relative hypoglycemia”4 (i.e., typical symptoms but blood glucose >60 mg/dl).
Table 2.
Primary impression versus low blood glucose
| Low blood glucose | |||
|---|---|---|---|
| No (≥60 mg/dL or missing) | Yes (<60 mg/dL or “unspecified low”) | ||
| Primary impression: hypoglycemia | |||
| No | 0 | 1,817 | 1,817 |
| Yes | 1,056 | 5,459 | 6,515 |
| 1,056 (12.7) | 7,276 (87.3) | 8,332 | |
Among the 7,276 encounters with documented low blood glucose (<60 mg/dL or unspecified low value), 1,817 (25.0%) had a primary impression other than hypoglycemia; in most instances, the primary impression did not rule out hypoglycemia (e.g., missing (n=168), altered level of consciousness (n=299), general weakness (n=238)), but in some instances there were conditions which may have been more salient than hypoglycemia (e.g., cardiac arrest (n=75)) which was accompanied by low blood glucose.
Discussion
In Alameda County during 2013–2015, 1 in 7 (13.5%) EMS encounters for hypoglycemia did not result in transport to an emergency department. These encounters would be missed in typical surveillance studies that rely solely on claims data or emergency department or hospitalization records.
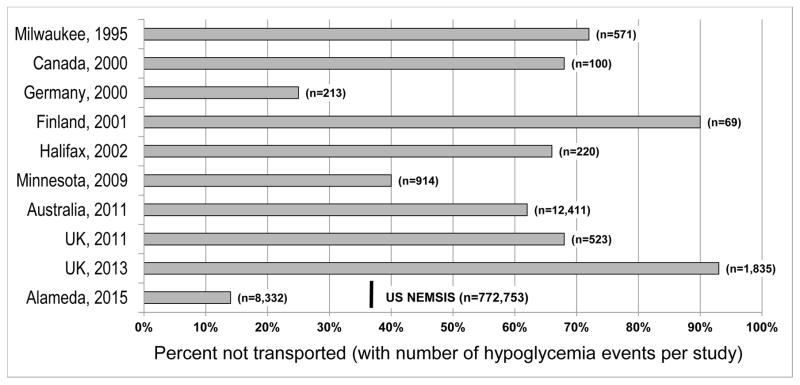
Previous studies found rates of non-transport for hypoglycemia in the range of 25%-93%, though some variations are due to reporting differences (Figure).15–23 The U.S. National EMS Information System (NEMSIS) included over 61 million EMS encounters during 2014 to mid-2016: 772,753 (1.26%) encounters were hypoglycemia events of which 37% were not transported to the ED.24 However the completeness of NEMSIS ascertainment is unclear and we cannot establish whether these data are representative of all US events. Nonetheless, the rate of non-transport for hypoglycemia in Alameda County is well below NEMSIS rates or reports in the literature.
Figure. Non-transport rates for prehospital encounters for hypoglycemia.
Figure caption (for details and variations of specific reporting):
Milwaukee, 1995: 412 of 571 (72%) 911 calls for hypoglycemia were successfully treated and subsequently refused transport.15
Ontario, Canada, 1999–2000: 68 of 100 patients (68%) refused transport.16
Detmold/East Westphalia, Germany, 1997–2000: 25% of 213 events were treated at the scene and not transported.17
Finland, 2001: 62 of 69 patients (90%) were left at the scene after treatment.18
Halifax, 2002: 145 of 220 (66%) EMS encounters were not transported.19
Olmsted County, Minnesota, 2003–2009: 368 of 914 (40%) patients were not transported.20
Victoria, Australia, 2009–2011: 62% of 12,411 hypoglycemia events not transported.21
East Midlands, UK, 2010–2011: 70% of 523 events were not transported.22
Yorkshire, UK, 2005–2013: 93% of 1,835 events were not transported.23
Alameda County, 2013–2015: 13.5% of encounters were not transported.
U.S. National EMS Information System (NEMSIS) (U.S., 2014–2016): 37% of 772,753 encounters were not transported.24
Consistent with other reports, we found that non-transport was more likely among younger (e.g., adults <60 years)15,16,21,23 or male15,21 patients or for encounters during midnight to 6:00 am.21,22 Other factors which have previously been found to be associated with non-transport but were not available in our study include insulin use,15,17,21,22 type 1 diabetes,20,21,23 not living alone23 and multiple previous episodes.23 We also lacked data on comorbidities, medication use or insurance status; data on race/ethnicity were missing for 75% of encounters. Finally, non-transport may depend on other factors not captured in our data, such as paramedic decision-making, patient preferences or alternative transport modes: Villani et al, for example, reported that 53% of non-transports were due to the EMS deeming transfer unnecessary, 38% were due to the patient refusing transport to hospital, and 8% were transported to hospital by private means or referred to a local medical officer.21 A strength of our study was the full three years of data for Alameda County, which has a large and diverse population.
While many have reported that non-transport can be safe,15–19 little is known about subsequent outcomes or hypoglycemia recurrence after non-transport. A prospective, observational study involving all adult (>15 years) hypoglycemic patients attended to by the EMS system in the Halifax Metropolitan area in Nova Scotia was conducted by Cain et al.19 During a ten-month interval, there were 220 EMS calls for hypoglycemia (66% not transported): while repeat episodes of hypoglycemia were common, recurrences within 48 hours were not, and admission to the hospital was rarely required. There appeared to be no difference in the incidence of recurrences and repeat episodes of hypoglycemia between transported and non-transported insulin-treated patients, regardless of age.
Differences in non-transport rates may be driven largely by local EMS protocols, rather than individual medical necessity. As a result, EMS personnel may have little discretion to release a patient at the scene, even if blood glucose normalizes. However, protocols to reduce unnecessary transport have been tested. In Germany, after the introduction of training in prehospital emergency therapy for severe hypoglycemia, the non-transport of type 1 diabetic patients increased from 8% to 25%.17 In West Hampshire, UK, paramedics were trained to direct the majority of diabetes patients with hypoglycemia to community diabetes services and patients were taken to the ED only when “absolutely necessary;” after the introduction of the protocol, 23% of 291 patients experiencing a hypoglycemic episode were referred to the community diabetes specialist team, and non-transport to hospital increased from 12% to 40% of patients.25
In the US, most EMS agencies are reimbursed only for transporting patients to an ED, but new models of care – such as “mobile integrated healthcare community paramedicine”26 or “mobile health care providers”27 offering additional training, a team approach and an emphasis on preventing unnecessary transport – could reimburse for care and reduce unnecessary transport. Given that hypoglycemia is often safely and effectively treated by non-physicians, EMS protocols should provide guidance for non-transport of hypoglycemia patients whose blood glucose normalizes after treatment.
Conclusion
Among EMS encounters with patients with hypoglycemia in Alameda County, we found a low, but significant rate of non-transport to an emergency department; however, this rate is substantially less that what has been reported elsewhere. Additional research is needed to better understand the frequency and characteristics of non-transport in EMS encounters with hypoglycemia patients. Our study demonstrates that, without an understanding of EMS encounters and non-transport rates, surveillance relying solely on emergency department and hospital data underestimates the true incidence of severe hypoglycemia events. Moreover, given the geographical variation in the rates of non-transport, the degree of under-ascertainment will vary regionally, often substantially.
Acknowledgments
Moffet, Sporer, Warton and Karter conceived the study; Warton and Siegel researched the data; Moffet wrote the manuscript; Warton, Siegel, Sporer, Lipska and Karter reviewed and edited the manuscript.
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
Funding: NIH (R01 DK103721)
Dr. Karter is supported by National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) (P30-DK092924). Dr. Lipska receives support from the Centers for Medicare & Medicaid Services (CMS) to develop and maintain publicly reported quality measures, and from the Yale Claude D. Pepper Older Americans Independence Center (P30AG021342) and the National Institute on Aging through the Paul Beeson Career Development Award (K23AG048359).
References
- 1.Pogach L, Aron D. Balancing hypoglycemia and glycemic control: a public health approach for insulin safety. JAMA. 2010;303(20):2076–2077. doi: 10.1001/jama.2010.655. [DOI] [PubMed] [Google Scholar]
- 2.Lee SJ. So much insulin, so much hypoglycemia. JAMA Intern Med. 2014;174(5):686–688. doi: 10.1001/jamainternmed.2013.13307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lipska KJ. Improving safety of diabetes mellitus management. JAMA Intern Med. 2014;174(10):1612–1613. doi: 10.1001/jamainternmed.2014.3290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Defining and reporting hypoglycemia in diabetes: a report from the American Diabetes Association Workgroup on Hypoglycemia. Diabetes Care. 2005;28(5):1245–1249. doi: 10.2337/diacare.28.5.1245. [DOI] [PubMed] [Google Scholar]
- 5.Laiteerapong N, Karter AJ, Liu JY, Moffet HH, Sudore R, Schillinger D, John PM, Huang ES. Correlates of quality of life in older adults with diabetes: the diabetes & aging study. Diabetes Care. 2011;34(8):1749–1753. doi: 10.2337/dc10-2424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Signorovitch JE, Macaulay D, Yan Y, Wu EQ, Gruenberger JB, Frier BM, Diener M. Hypoglycaemia and accident risk in people with type 2 diabetes mellitus treated with non-insulin antidiabetes drugs. Diabetes, obesity & metabolism. 2013;15(4):335–341. doi: 10.1111/dom.12031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stahn A, Pistrosch F, Ganz X, Teige M, Koehler C, Bornstein S, Hanefeld M. Relationship between hypoglycemic episodes and ventricular arrhythmias in patients with type 2 diabetes and cardiovascular diseases: silent hypoglycemias and silent arrhythmias. Diabetes Care. 2014;37(2):516–520. doi: 10.2337/dc13-0600. [DOI] [PubMed] [Google Scholar]
- 8.Whitmer RA, Karter AJ, Yaffe K, Quesenberry CP, Jr, Selby JV. Hypoglycemic episodes and risk of dementia in older patients with type 2 diabetes mellitus. JAMA: the journal of the American Medical Association. 2009;301(15):1565–1572. doi: 10.1001/jama.2009.460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Majumdar SR, Hemmelgarn BR, Lin M, McBrien K, Manns BJ, Tonelli M. Hypoglycemia associated with hospitalization and adverse events in older people: population-based cohort study. Diabetes Care. 2013;36(11):3585–3590. doi: 10.2337/dc13-0523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McCoy RG, Van Houten HK, Ziegenfuss JY, Shah ND, Wermers RA, Smith SA. Increased mortality of patients with diabetes reporting severe hypoglycemia. Diabetes Care. 2012;35(9):1897–1901. doi: 10.2337/dc11-2054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zoungas S, Patel A, Chalmers J, de Galan BE, Li Q, Billot L, Woodward M, Ninomiya T, Neal B, MacMahon S, Grobbee DE, Kengne AP, Marre M, Heller S ADVANCE Collaborative Group. Severe hypoglycemia and risks of vascular events and death. N Engl J Med. 2010;363(15):1410–1418. doi: 10.1056/NEJMoa1003795. [DOI] [PubMed] [Google Scholar]
- 12.Lipska KJ, Warton EM, Huang ES, Moffet HH, Inzucchi SE, Krumholz HM, Karter AJ. HbA1c and risk of severe hypoglycemia in type 2 diabetes: the Diabetes and Aging Study. Diabetes Care. 2013;36(11):3535–3542. doi: 10.2337/dc13-0610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sarkar U, Karter AJ, Liu JY, Moffet HH, Adler NE, Schillinger D. Hypoglycemia is more common among type 2 diabetes patients with limited health literacy: the Diabetes Study of Northern California (DISTANCE) Journal of general internal medicine. 2010;25(9):962–968. doi: 10.1007/s11606-010-1389-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rostykus P, Kennel J, Adair K, Fillinger M, Palmberg R, Quinn A, Ripley J, Daya M. Variability in the Treatment of Prehospital Hypoglycemia: A Structured Review of EMS Protocols in the United States. Prehosp Emerg Care. 2016;20(4):524–530. doi: 10.3109/10903127.2015.1128031. [DOI] [PubMed] [Google Scholar]
- 15.Socransky SJ, Pirrallo RG, Rubin JM. Out-of-hospital treatment of hypoglycemia: refusal of transport and patient outcome. Acad Emerg Med. 1998;5(11):1080–1085. doi: 10.1111/j.1553-2712.1998.tb02666.x. [DOI] [PubMed] [Google Scholar]
- 16.Carter AJ, Keane PS, Dreyer JF. Transport refusal by hypoglycemic patients after on-scene intravenous dextrose. Acad Emerg Med. 2002;9(8):855–857. doi: 10.1111/j.1553-2712.2002.tb02179.x. [DOI] [PubMed] [Google Scholar]
- 17.Holstein A, Plaschke A, Vogel MY, Egberts EH. Prehospital management of diabetic emergencies--a population-based intervention study. Acta Anaesthesiol Scand. 2003;47(5):610–615. doi: 10.1034/j.1399-6576.2003.00091.x. [DOI] [PubMed] [Google Scholar]
- 18.Mattila EM, Kuisma MJ, Sund KP, Voipio-Pulkki LM. Out-of-hospital hypoglycaemia is safely and cost-effectively treated by paramedics. Eur J Emerg Med. 2004;11(2):70–74. doi: 10.1097/00063110-200404000-00003. [DOI] [PubMed] [Google Scholar]
- 19.Cain E, Ackroyd-Stolarz S, Alexiadis P, Murray D. Prehospital hypoglycemia: the safety of not transporting treated patients. Prehosp Emerg Care. 2003;7(4):458–465. doi: 10.1080/312703002193. [DOI] [PubMed] [Google Scholar]
- 20.Parsaik AK, Carter RE, Pattan V, Myers LA, Kumar H, Smith SA, Russi CS, Levine JA, Basu A, Kudva YC. Population-based study of severe hypoglycemia requiring emergency medical service assistance reveals unique findings. J Diabetes Sci Technol. 2012;6(1):65–73. doi: 10.1177/193229681200600109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Villani M, Nanayakkara N, Ranasinha S, Tan CY, Smith K, Morgans A, Soldatos G, Teede H, Zoungas S. Utilisation of emergency medical services for severe hypoglycaemia: An unrecognised health care burden. J Diabetes Complications. 2016;30(6):1081–1086. doi: 10.1016/j.jdiacomp.2016.04.015. [DOI] [PubMed] [Google Scholar]
- 22.Khunti K, Fisher H, Paul S, Iqbal M, Davies MJ, Siriwardena AN. Severe hypoglycaemia requiring emergency medical assistance by ambulance services in the East Midlands: a retrospective study. Prim Care Diabetes. 2013;7(2):159–165. doi: 10.1016/j.pcd.2013.01.001. [DOI] [PubMed] [Google Scholar]
- 23.Elwen FR, Huskinson A, Clapham L, Bottomley MJ, Heller SR, James C, Abbas A, Baxter P, Ajjan RA. An observational study of patient characteristics and mortality following hypoglycemia in the community. BMJ Open Diabetes Res Care. 2015;3(1):e000094. doi: 10.1136/bmjdrc-2015-000094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. [last accessed Oct 5, 2016];NEMSIS National Event Data Cube. http://www.nemsis.org/reportingTools/reports/nationalReports/createAReport.html.
- 25.Novel Pathway for Ambulance Crew Halves Hypoglycemia Admissions. Medscape. 2015 Mar 24; [Google Scholar]
- 26.Kizer KW, Shore K, Moulin A. Community Paramedicine: A Promising Model for Integrating Emergency and Primary Care. UC-Davis Institute for Population Health Improvement; Jul, 2013. [last accessed Nov 21 2016]. https://www.ucdmc.ucdavis.edu/iphi/publications/reports/resources/IPHI_CommunityParamedicineReport_Final%20070913.pdf. [Google Scholar]
- 27.Span P. Going to the Emergency Room Without Leaving the Living Room. [Accessed Nov 29 2016];New York Times. 2016 http://www.nytimes.com/2016/11/08/health/older-patients-community-paramedics.html.