Abstract
Cardiovascular disease, particularly the occurrence of myocardial infarction (MI), remains a leading cause of morbidity and mortality (Go et al., Circulation 127: e6–e245, 2013; Go et al. Circulation 129: e28–e292, 2014). There is growing recognition that a key factor for post-MI outcomes is adverse remodeling and changes in the regional structure, composition, and mechanical properties of the MI region itself. However, in vivo assessment of regional mechanics post-MI can be confounded by the species, temporal aspects of MI healing, as well as size, location, and extent of infarction across myocardial wall. Moreover, MI regional mechanics have been assessed over varying phases of the cardiac cycle, and thus, uniform conclusions regarding the material properties of the MI region can be difficult. This review assesses past studies that have performed in vivo measures of MI mechanics and attempts to provide coalescence on key points from these studies, as well as offer potential recommendations for unifying approaches in terms of regional post-MI mechanics. A uniform approach to biophysical measures of import will allow comparisons across studies, as well as provide a basis for potential therapeutic markers.
Keywords: myocardial infarction, myocardial mechanics, in vivo, regional
despite improvements in reperfusion therapy, prolonged periods of ischemia often culminate in permanent injury to the myocardial parenchyma, otherwise known as myocardial infarction (MI) (17, 50, 51, 91, 99, 102, 112, 117, 126). The resultant MI can lead to left ventricular (LV) pump dysfunction due to both a direct loss of contractile units and by placing the viable myocardium at a mechanical disadvantage (103, 120). The MI region itself is not static but rather undergoes significant changes in composition and structure over time. The elapsed time post-MI can be related to the phases of the normal wound healing response: post-acute/inflammation, proliferation, and maturation (28, 29, 33, 34, 38, 43, 44, 107, 119, 131). However, the complete resolution of the wound into a fully formed and contracted scar, which is the end result of a prototypical wound healing response, does not occur in this context. Instead, the MI region undergoes continuous remodeling due to persistent proliferation of fibroblasts and turnover of newly formed extracellular matrix, and as a consequence, is structurally unstable (42, 93, 100, 119). This deviation from prototypical wound healing can be partially attributed to the continuous cyclical loading of the myocardium with resultant stresses and strains governing the activity of resident fibroblast cells (20, 22, 80). Thus, while the remodeling process is certainly complex and multifactorial, it is likely that local alterations in stress and strain patterns that occur within the MI region contribute significantly to structural instability, thinning of the MI region, and increased MI area as a function of time (65, 88, 133, 134). Moreover, the continuous changes in the material properties of the MI coupled with abnormalities in stress and strain result in a “feed-forward” mechanism for progressive MI expansion, LV dilation, and ultimately LV failure, which is called adverse post-MI remodeling (30, 120). Therefore, the continued development of therapeutic strategies to interrupt/attenuate adverse post-MI remodeling requires consideration of the mechanical properties and behavior of the MI region itself (25, 57, 62, 71, 133). For example, mechanical restraint devices that surround part or all of the left ventricle have shown potential to limit MI region dilation up to 8 wk post-MI (71). Accordingly, the overall goal of this review is to evaluate past studies that have examined biophysical properties of the MI region and to coalesce these findings into unifying concepts regarding the relation of these properties to the post-MI remodeling process.
Past studies have utilized different post-MI models, measurement systems, and time points to quantify MI region mechanics, all of which must be taken into consideration for meaningful interpretation of reported results. To that end, this review places past studies in temporal context to the post-MI phases of remodeling identified as post-acute (3–7 days), intermediate (7–14 days), and late remodeling (>14 days). Although these temporal phases are rather arbitrary and overlapping, they serve to demark relevant cellular/extracellular changes that likely impact biophysical properties of the MI region (103, 106). However, it is important to note that for clinical observations, some exceptions have been made for inclusion within the post-acute phase, as most studies approximate the onset of MI and only report the elapsed time since reperfusion. In this review, the acute phase of ischemia will not be considered, as biophysical measurements in this time period are confounded by the effects of reperfusion, differences in myocardial viability, stunning, and significant variances in overall tissue viability. In general, these events have dissipated by ~72 h following the index event (16, 35, 40, 70, 120). A number of landmark studies have been performed, whereby the myocardial mechanical properties have been examined from excised specimens taken from normal and infarcted LV regions (54, 69, 89, 90, 93, 94, 139). These studies have provided critical insight into the development of models that characterize key aspects of cardiac muscle biophysical behavior. However, the appropriate translation of obtained in vitro results to the intact cardiac preparation, specifically in terms of the mechanical properties of the MI region, is much less clear. Accordingly, the reporting of both in vivo cyclical and remodeling strains plays a large part of this review. For clarity, the reference length used to compute a cyclical strain is based on a segmental length measurement made at a specific point in the cardiac cycle. Conversely, the reference length to compute remodeling strain is based on a segmental length measurement made at baseline (pre-MI) and a specific point in the cardiac cycle, with comparison to a phase-matched segmental length measurement made at a specified post-MI time point. This review will focus upon studies that have examined the mechanical properties of the MI region only under in-vivo conditions in the context of the imaging techniques listed below in Table 1, “Summary of imaging techniques.”
Table 1.
Summary of imaging techniques
| Abbreviation | Technique and Description |
|---|---|
| MRI | Magnetic resonance imaging—imaging technique using a magnetic field and radio frequency pulse waves with high spatial resolution of soft tissues. |
| SPAMM/MR tagging | Spatial modulation of magnetization—saturation bands (in a grid) are created by radio frequency pulses, enabling the tracking of segment or line lengths that can be analyzed over cardiac cycles. |
| HARP | Harmonic phase analysis—spectral peaks of tagged MRI (in the Fourier domain) are used to calculate phase images of the inverse Fourier transforms. Motion of points in the resulting images can then be tracked. |
| LG-MRI | Late-gadolinium enhancement MRI—a gadolinium contrast is used for enhanced visualization of the MI region. |
| SRI | Strain rate imaging—echocardiography technique that tracks deformation of myocardium. |
| TDI | Tissue Doppler imaging—echocardiography technique that describes myocardial motion. |
| Biplane cineradiography—imaging technique using an X-ray field to create a three-dimensional coordinate system by use of radio-opaque markers to calculate interpoint distances and deformation. | |
| Ventriculography—imaging technique used in the determination of function of the left ventricle, using catheterization and injection of contrast for definition in X-ray images. |
In terms of assessing intact LV mechanics, particularly in terms of biophysical properties post-MI, the term stiffness is often used. However, this is a fairly generalized term and warrants a more focused definition. Myocardial stiffness is determined by regional changes in stress-strain relationships, and when determined during the diastolic phase of the cardiac cycle, is reflective of changes in cellular and extracellular composition. For example, changes in extracellular matrix content, intracellular or extracellular water content, such as edema, and changes in cellular (myocyte) size, such as with hypertrophy, or changes in intracellular constituents, such as cytoskeletal elements, will all affect diastolic myocardial stiffness. In the post-MI context, diastolic myocardial stiffness within the MI region will be determined primarily by the extracellular matrix composition since the cellular contributions by cardiac myocytes is fundamentally absent. However, even this is an oversimplification as cardiac myocytes contained within the border zone of the MI region can most certainly impact stress-strain relationships. Moreover, in a nontransmural MI, the surviving myocytes will contribute to myocardial stiffness properties. As such, this review will, when possible, examine in vivo diastolic myocardial stiffness in terms of the location of the measurements, as well as transmurality of the MI. Since this review will primarily highlight the importance of post-MI myocardial stiffness/mechanics during diastole, then a consideration of the cardiac cycle and the impact upon overall stiffness properties is warranted. In addition to regional diastolic stiffness computations, it is not uncommon to also examine LV chamber stiffness properties. This can be an additional source of confusion and contribute to difficulties in interpretation of in vivo studies in terms of chamber vs. myocardial stiffness. In contrast to regional diastolic myocardial stiffness properties, LV chamber stiffness is a summation of both the passive mechanical behavior of the myocardium itself (diastolic myocardial stiffness) and active relaxation. Active relaxation is influenced by calcium handling/myofilament dynamics, myocardial oxygen-energy utilization, and to a lesser degree, LV loading conditions (which include the effects of transient changes in microvascular flow). As such, this review will clearly differentiate between regional myocardial diastolic stiffness and LV diastolic chamber stiffness. Because both are highly relevant to overall LV function and geometry post-MI, these parameters will be clearly identified in this review and presented in a temporal fashion.
Post-Acute Phase (3–7 Days)
Significant cardiac myocyte cell loss via necrosis and apoptosis occurs in the post-acute phase, which is initially accompanied by the elaboration of cytokines that diminishes upon egress of inflammatory cells, such as neutrophils and macrophages (34, 43, 44, 109, 122). These biological/cellular events are accompanied by an increased release of a number of proteases that degrade cellular and extracellular components and, thus, contribute to structural remodeling of the MI region (34, 43, 109, 118). Notable physiological results of these cellular and extracellular events are increased vascular permeability and changes in interstitial oncotic pressure, which, in turn, promote localized edema within the MI region (4, 42). Together, these changes in composition, structure, and turgor pressure will significantly affect mechanics within the MI region.
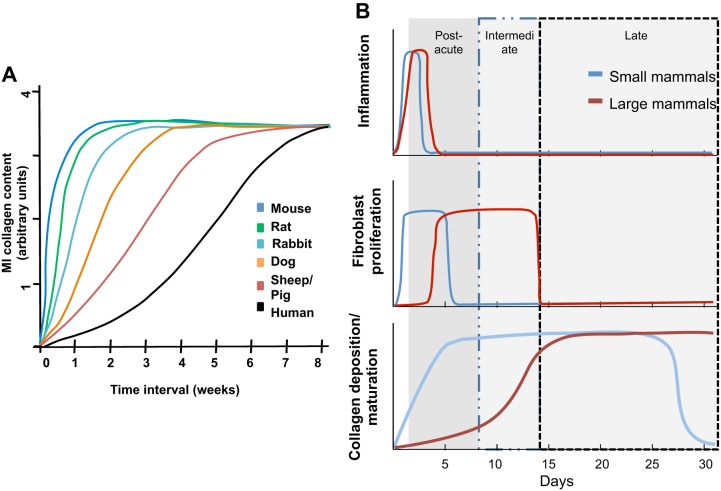
While the generalized inflammatory pathways and cell types can be similar across species, in this post-acute phase, there are temporal differences in the pattern of inflammation between small and large mammals post-MI (33). For example, a robust increase in the cytokine tumor necrosis factor-α is observed early in rodent MI models with a tendency to plateau and resolve by 1 wk post-MI (34, 43, 118). In contrast, a more progressive and sustained increase in tumor necrosis factor-α within the MI region is reported in large animal models (33, 34, 43). The temporal cytokine profile observed in large animal models in this post-MI period is similar to the cytokine profile observed in plasma samples obtained in humans (18, 30, 38, 43, 44, 65). Similarly, temporal differences in the release of matrix proteases and development of local tissue edema have been observed between small and large animal models post-MI. A summary of the temporal changes in some of these post-MI processes is presented in Fig. 1. Perhaps the most striking outcome of interspecies differences is the occurrence of myocardial rupture. Specifically, myocardial rupture is a rare event clinically post-MI and exceedingly uncommon in large animal models (15, 92, 92a). In contrast, rodent models of MI, particularly those of mice, have reported rupture rates between 29 and 53% (23, 118, 122). These observations would suggest significant differences in the cellular and extracellular architecture and composition within the MI region of rodents as opposed to large mammals, which, in turn, would directly influence regional mechanical properties. Accordingly, the type of animal model used will have significant implications for measurements of MI region mechanics in the post-acute phase.
Fig. 1.
Species differences. Temporal representation of biological events post-myocardial infarction (MI) in rodents and large mammals, which can affect physical properties of the MI region. A: summary time plot of the rate of collagen accumulation as a function of time post-MI in different species. Figure adapted with permission from Jugdutt et al. (68) with original research (40, 66, 87a, 106). B: relative to large mammals, rodents exhibit accelerated resolution of the inflammatory phase (top), an earlier and abbreviated fibroblast proliferation phase (middle), and rapid collagen deposition and maturation (bottom). The figure was compiled from reported data (33, 34, 38, 43, 44, 64, 66, 67, 78, 136).
Imaging Studies
A large number of studies have utilized various imaging modalities to examine the function and mechanics of the LV and specifically the MI region. The most common techniques include high spatial and temporal methods, such as magnetic resonance imaging (MRI), as well as ultrasound in both humans and animals (2, 5, 45, 47, 98, 108, 127, 130, 138). The primary goal of most studies has been to identify correlations among MI size, mechanics, and functional measures. Imaging techniques present an attractive opportunity for less invasive and clinically translatable approaches (27, 53).
Ultrasound.
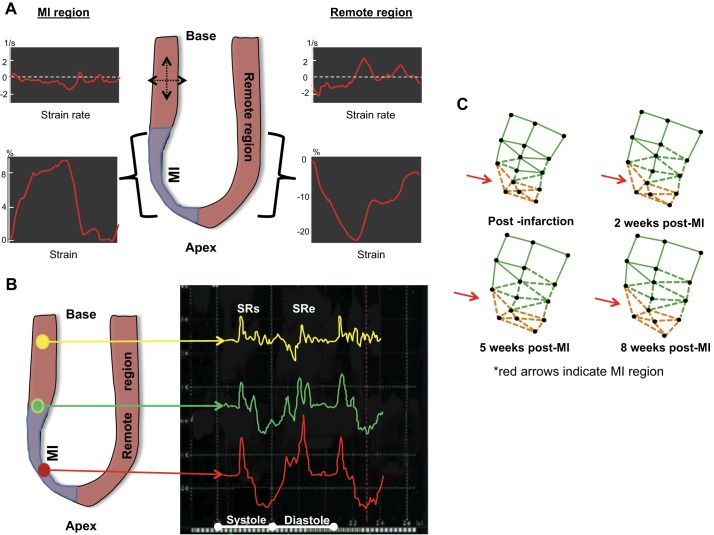
Traditional two-dimensional (2-D) ultrasound measurements have been used extensively to examine LV volumetric and pump function in the post-MI period. For the purposes of focus, studies that have used ultrasound to examine aspects of myocardial strain and, in particular, strain during the filling phase of the cardiac cycle, will be examined to quantify cavity dimensions and extract mechanical measures of the left ventricle post-MI. Tissue Doppler imaging (TDI), a form of ultrasound, is a noninvasive method by which regional indices of myocardial function, such as contraction (from endocardial and epicardial velocities) and wall motion, may be assessed (6, 49, 127, 135). Strain rate imaging (SRI) can be acquired and has proven to be an effective tool in the evaluation of both MI and viable surrounding myocardium (Fig. 2) (36, 49, 124, 141). While the precise post-MI period was not specified, Edvardsen et al. (36) reported that following the acute post-MI period in patients, abnormal deformation patterns exist in the post-MI left ventricle with longitudinal stretching in the MI region compared with shortening (in the same direction) in the remote myocardium. Moreover, radial cycle-dependent strains within the MI region were indicative of localized thinning rather than thickening [Fig. 2A (36, 63, 141)]. The study by Zhang et al. (141) used strain rate imaging to assess various markers of LV function relevant to the mechanics of the region, which included early diastolic strain rate and peak systolic strain rate (reference length at end diastole) in patients with varying extents of infarction across myocardial wall at 2–6 days post-MI. This study determined that the peak systolic strain rate and early diastolic strain rate decreased most markedly in patients where a completely transmural MI was present [Fig. 2B (36, 63, 141)]. In those patients with a transmural MI, the greatest decline in both peak systolic strain rate and early diastolic strain rates occurred. From the results of this study, the influence of infarction across myocardial wall as a factor affecting the mechanics of the MI region can be gleaned.
Fig. 2.
Strain heterogeneity. A: regional heterogeneity of left ventricular (LV) strain following MI in patients (early post-MI period) was examined using tissue Doppler. Both cyclic longitudinal strain and strain rate exhibited significant variation between the MI and remote regions. The figure was adapted with permission from Edvardsen et al. (36) B: representative strain rate (SR) calculations using tissue Doppler in patients during the early post-MI period (2–6 days post index event), including both peak systolic strain rate (SRs) and early diastolic strain rate (SRe). Trace location is demarcated by line color: Yellow trace denotes basal segment, green trace denotes middle segment, and red trace denotes apical segments. Adapted with permission from Zhang et al. (141) C: representative chord reconstructions of a partial left ventricle in adult sheep, whereby sonomicrometry crystals span the MI, border, and remote regions. Occlusion of the distal segment of the left anterior descending coronary artery yielded an MI within the apical LV region (orange chords). Over time, a significant increase in all these chord lengths was observed. The figure was adapted from Jackson et al. (63) with permission. Although remodeling strain was not calculated, the increases in chord lengths are in line with expected increases in remodeling strains.
Magnetic resonance imaging.
MRI has long been heralded as the gold standard technique for assessment of LV mechanics due to its good temporal and spatial resolution and noninvasive nature (3, 46, 111). A common use of MRI involves the tagging of the LV and MI region with a set of horizontal and vertical lines (by saturation) to track points or segments during multiple cardiac cycles, termed spatial modulation of magnetization (SPAMM, or MR tagging). In general, MR tagging strain measurements are derived from radio frequency pulses that produce magnetic saturation, enabling the tracking of segment or line lengths that can be analyzed over cardiac cycles (3, 27). Measurements of tracked points/segments through the cardiac cycle can then be converted to linear dimensions, hence, producing an index of mechanical strain. Using this approach, Walker et al. (128) identified, for example, that a reduction (from referent control values) in peak systolic strain (absolute values) within the MI region is related to the decrease in LV pump performance, whether strain is measured along a longitudinal, circumferential, or radial direction. With consideration of the relatively accelerated remodeling process in rodents, Ross et al. (108) used MRI to assess the extent of wall thickening (among other regional functional measures) at 1 day post-MI. The authors noted that the percentage of wall thickening (presented as a percentage of end-diastolic wall thickness) showed an approximate 60% decline from baseline to roughly 10% after only 1 day post-MI. While wall thickening clearly declined, radial strain at different times post-MI varied significantly, with differences attributed to edema-related changes in the end-diastolic wall thickness. This study also reported the disappearance of such edema at day 7 post-MI, which was accompanied by a further decrease in wall thickening. This change in wall thickening in the MI region could potentially be interpreted as change in strain, likely in the radial direction (here seemingly affected by edema). These changes in MI thickness and motion over a 3–7 day time period are consistent with the inflammatory timeline for rodents [Fig. 1 (33, 34, 38, 43, 44, 64, 66, 67, 78, 136)]. Young et al. (140) reported circumferential and longitudinal cycle-dependent strains in a rodent MI model to exhibit spatial variation throughout the left ventricle, although there is a persistent decrease in magnitude compared with referent strains in normal subjects at all locations. Since there is a relatively collapsed time window for the acute post-MI period and the spatial resolution of MRI in rodents can be limited, this technique is primarily relegated to large animal models to examine regional mechanics post-MI. Using a pig model, Saeed et al. (111) found similar decreases in longitudinal and circumferential cycle-dependent strains at 3 days post-MI (compared with remote myocardium) and also reported “significantly decreased” peak systolic strain in all directions (radial, circumferential, and longitudinal) in the analyzed segments contained within the MI region. Another study in pigs quantified the differences in peak circumferential cycle-dependent strain between the MI region and peri-infarct zone (113). This study used late-gadolinium enhancement-cardiac MR to quantify regional strains, finding that at the 3-day time point, a significant decrease in both MI region and peri-infarct zone strain was found. Such findings of variances in strain in the different regions (MI region, peri-infarct zone, remote, etc.) underscore that the variations in strain occur nonuniformly over time.
Various studies have been carried out in a clinical setting with MRI techniques as a basis for the study of the post-MI myocardium. Using MR tagging in patients, Bogaert et al. (14) found that normal and shear strains in the MI region decreased significantly by 5 days post-MI. This study noted a slight increase in edema contributing to MI wall thickness, which has previously been shown to modulate wall stress and strain patterns and lead to an increase in structural stiffness (4). Garot et al. (45) used tagged MRI coupled with harmonic phase imaging (HARP). This dual approach isolates segmental motion of tagged myocardium (MRI tagging), which is then analyzed using a HARP algorithm that produces phase images (based on the spectral peaks in the Fourier domain). In these images, the motion of points can then be tracked along with the accompanying direction of movement (96). In this past clinical study, MRI using HARP was performed ~3 days post-MI while arguably, before the time points of interest in this review, holding relevance in terms of regional mechanics within both normally perfused and MI segments. Specifically, this study identified that regional systolic strain pattern changes in both perfused and nonperfused segments occurred at this early post-MI time point. Gerber et al. (46) also utilized tagged MRI in conjunction with contrast enhanced MRI at 4 days post-MI in patients to analyze the peak circumferential strain (fractional change of length between end diastole and end systole). The authors found that circumferential strain significantly decreased in segments that displayed early hypoenhancement (lower retention of contrast indicative of viable tissue), as well as delayed hyperenhancement (increased retention of contrast indicative of MI) when compared with remote segments. These findings demonstrate that in addition to quantifying the extent of an infarction, hypoenhancement and hyperenhancement can be used to develop MRI-based indices of myocardial function. In this study, the dysfunctional segments contained within the MI region demonstrated a significant relationship of circumferential shortening improvement (increased contractility) dependent on hyper/hypo-enhancement that represented the extent of infarction across myocardial wall of the MI (46).
Mechanical Implications
The post-acute phase is temporally offset across animal models with rodents exhibiting MI region collagen deposition and maturation twice as fast as large mammals. In all animal models, the strain in the MI region decreases as compared with controls, albeit to different extents. It is important to note that the remote myocardial region in treatment groups serves as a referent control in some studies. Although this is a common study design, it is well known that the remote region geometry and properties change throughout the remodeling process (14). Therefore, sham animals should be used for control groups when possible. The MI region exhibits an elevated degree of mechanical anisotropy with respect to normal myocardium, with most studies reporting an increase in the difference in the absolute values of principal strains (directions correspond to zero shear) over the cardiac cycle and throughout the remodeling process. In general, strain magnitudes are decreased relative to normal myocardium, which is often attributed to a change in the material properties of the MI region and has been described in terms of the resultant dyskinetic wall motion with respect to the remote myocardium (121). Studies that utilized various imaging modalities have identified progressive wall thinning and decreased curvature in the left ventricle, both of which contribute to an observed increase in global wall stress. Some studies have focused on the mechanics of the regions adjacent to the MI and likewise found a decrease in recorded strain magnitudes. Post-MI remodeling results in changes to both material and structural properties. The material properties of the MI region are impacted by the local loss of contractile function, as well as the progressive change in myocardial composition (increased collagen content, presence of edema, etc.) and can only be identified on the basis of stress-strain relations. Quantification of MI region material properties (i.e., myocardial stiffness) is most accurate during diastole, when the myocardium can be reasonably modeled as a passively deforming material. In contrast, post-MI changes in LV structural properties depend on the evolution of both material properties and geometry and are typically quantified from pressure-volume relations obtained at the chamber/global level (i.e., chamber stiffness). Structural LV properties, including chamber stiffness, vary significantly over the systolic and diastolic phases and, thus, should always be referenced to a specific point in the cardiac cycle.
Clearly, both local material properties (myocardial stiffness) and chamber-level structural properties (chamber stiffness) are affected by the loss of contractile units in the MI region. Distinction between and accurate quantification of these properties is essential to understanding disease progression, as the stress/strain state within the MI region is a key modulator of the remodeling process and concomitant loss of LV function.
Intermediate Phase (7–14 days)
This post-MI phase is associated with increased expression of anti-inflammatory cytokines and profibrotic molecules, where one of the most notable is transforming growth factor-β (19, 32, 37, 79, 83, 115). Studies involving a range of animal models consistently report increased fibroblast proliferation within the MI region in concurrence with changes in intracellular and intercellular protein expression profiles (33, 34, 38, 57). Fibrillar collagen content within the MI region is elevated in comparison to the border or remote regions, and changes in LV geometry consistent with the MI expansion process occur (132–134). Since this post-MI phase is accompanied by significant transitions in inflammation, signaling molecules, and matrix formation, very dynamic changes also occur in biophysical response variables within the MI region, such as strain, strain rate, and stress (quantity that must be calculated). As stated previously, the duration of biochemical/cellular events that occur in this post-MI phase are also species dependent [Fig. 1A (33, 34, 38, 43, 44, 64, 66, 67, 78, 136)], whereby inflammation and matrix formation/maturation occur with temporal variations (as per the figure) with respect to small and large animals. For example, in mouse MI models, a relatively mature MI region (defined as a thinned, collagen rich region) has been reported to occur within 2 wk post-MI (28, 29). Conversely, the MI region in larger animal models remains highly cellular and structurally dynamic throughout this phase and up through the late phase (28 days post-MI and beyond). Biomechanical response variables (which include stress and strain) are directly affected by the loss of contractile forces in the MI and active viable surrounding myocardium (affecting calculated stress) with architectural changes also impacting strain (8, 28, 41, 86, 87, 95, 100, 104). Thus, the temporal difference in MI region maturation with respect to different animal species constitutes an important consideration when evaluating stiffness in this post-MI time period.
Imaging
Ultrasound.
Modifications and expanded use of ultrasound, such as speckle tracking echocardiography (STE), layer-specific STE (LS-STE), and tissue Doppler imaging (TDI), have been used to refine measurements of segmental length and strain magnitudes within the MI, often at time points beyond this intermediate period. More specifically, these methods allow for computations of strain and strain rates of targeted chords within the MI region based on tracking the relative positions of individual speckles, a defined acoustic marker or pattern that can be tracked over time (53). This section will focus upon the admittedly few studies that have examined relative strain values within the MI region using these techniques in this time frame.
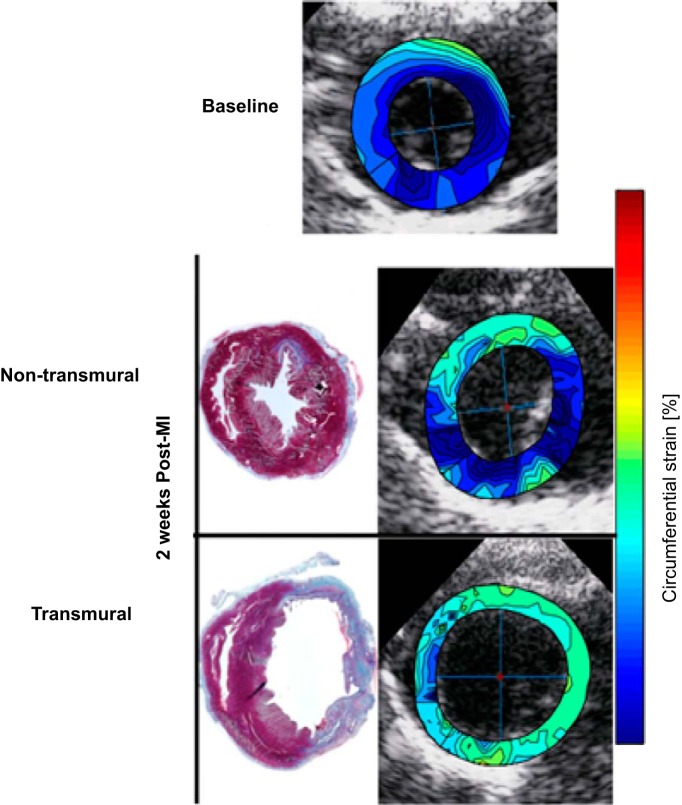
While the use of high-resolution/frequency transducers (ultrasound probes) has improved spatial resolution and, thus, applications in rodent post-MI models, the majority of studies (primarily at acute or later time points) have been performed in large animals and humans. However, a study utilizing LS-STE in a rodent model at two weeks post-MI reported a depth-dependent decrease in the peak circumferential strain compared with baseline values. In transmural infarcts, a significant decrease in peak circumferential strain was found only in the layers spanning the endocardium and midwall. Conversely, nontransmural infarcts exhibited an increase in peak circumferential strain in the endocardial layer. These findings highlight the dependence of strain on extent of infarct across the myocardial wall, a model-specific factor, which, therefore, should be considered and reported along with mechanical measurements of the MI region [Fig. 3 (7)].
Fig. 3.
Extent of infarction across myocardial wall. Top: layer-specific speckle-tracking echocardiography depicting peak strain in a rat MI model with varying degrees of infarction across the myocardial wall. Baseline cyclic strain at systole is nearly homogeneous and depicts contractility (high strain/contractility indicated by blue tones). LV strain maps at 2 wk post-MI of a non-transmural (middle) and completely transmural (bottom) MI depict a reduction in strain magnitudes with contractile loss and uniformity, which is magnified by the depth of infarction across the myocardial wall. The figure was adapted with permission from Bachner-Hinenzon et al. (7).
Using a dog model, Park et al. (97) reported a decrease in radial and longitudinal strain rate at both early and late diastole in concurrence with a reduction in strain magnitudes with respect to control values. The authors reported stiffness indices in the MI region (derived from wall thickness and hemodynamic pressure measurements) to increase in correlation with a decrease in diastolic strain rate and changes in composition. The end diastolic stress in the circumferential direction of the MI region was also noted to have a more drastic decrement compared with longitudinal direction. Here, the authors conclude that diastolic deformation indexes and functional measurements (rather than systolic) of the MI region could be significant metrics of study in future clinical applications.
In patients, it has been established that the extent of infarction across the myocardial wall affects the magnitude of strain changes post-MI (10, 141). To this effect, studies in patient populations using STE and 2D-echocardiography at a time point described as early, but beyond acute occurrence of MI, are here categorized as falling in the intermediate phase. In these studies, the segments with a completely transmural MI resulted in decreased peak systolic strains in both circumferential and radial directions at both short and long axis. A significant decrease compared with referent normal values in strain rates (systolic, same directions) was also associated with extent of infarction across the myocardial wall (10, 24).
Magnetic resonance imaging.
Magnetic resonance imaging (MRI) studies using rat and mouse models in the intermediate time frame have shown a continued decrease in strain (in all directions) compared with the acute time period. This decrease is consistent with the progress toward maturation of the MI [Fig. 1 (33, 34, 38, 43, 44, 64, 66, 67, 78, 136)]. In rats, Young et al. (140) used MRI tagging and late gadolinium enhancement-MRI (LGE-MRI) techniques with a finite element model (FE) to map LV wall strain. At the 7-day time point, the longitudinal, circumferential, and 3D principal strains were found to be most affected (compared with the control) in the apical region and midventricular regions. Here, the 3D principal strain was defined as the maximal contraction at a given point in a direction not usually aligned with a traditional image plane, highlighting regional differences of strain post-MI.
In a dog model, SPAMM-tagged MRI in conjunction with a FE model showed significant decreases in strain in all directions at 10 days post-MI, with circumferential strain at the apex of the left ventricle most affected (77). Studies on pig MI models have sought to define regional strains and regional mechanical dyssynchrony using cardiac MRI and LGE-MRI, with results that are in general agreement with previous findings in large mammals (decreased strain in all directions) (1). Similarly, a pig model studied at 11 days post-MI with LGE-MRI in conjunction with HARP analysis showed MI region strains that were significantly less than baseline healthy segments. The circumferential strain displayed the greatest reduction (of absolute values compared with baseline) in the MI region, although adjacent regions also exhibited significant alteration of principal strains. Here, principal strains are defined along coordinate directions that correspond to zero shear. It is interesting to note that this study eliminated segments that were not completely transmural, thus anticipating and accounting for the possibility of mechanical heterogeneity in the radial direction (116).
Physical Approaches: Sonomicrometry and Markers
In vivo.
Sonomicrometry arrays are formed with ultrasonic crystals that each emit and receive high-frequency pulse waves, enabling the measure of relative distances between crystal pairs when implanted within the myocardium (138). Tissue-embedded arrays can provide high spatial resolution of local deformation fields with some freedom in the creation of a reference coordinate system. A study carried out in a rat model by Fomovsky et al. (41) used seven sonomicrometry crystals to study MI region mechanics from 1 to 6 wk post-MI. The authors found the circumferential and longitudinal strains were significantly decreased from referent normal values at both 1 wk and 2 wk time points. Critically, no collagen fiber alignment was seen in the MI region of the rats and thus it was considered a mechanically isotropic material. While appropriate here, the categorization of MI region mechanical properties as isotropic may not be suitable for larger animal models that exhibit a high degree of fiber alignment (41).
In larger animal models, such as sheep, the implantation of nine sonomicrometry crystals along the MI region showed significant regional differences in strain with a 2-wk time point. In this study, remodeling strain was defined as the change in end-diastolic dimensions from baseline configuration of the crystals on the LV free wall to a deformed configuration at a specific time post-MI. In essence, this remodeling strain is representative of geometric changes rather than cycle -dependent ones post-MI. A significant increase in remodeling strain was observed at the 14-day time point, with a concomitant decrease in MI region end-systolic cyclical strain also promoting akinesis. The authors also found a correlation between markers of apoptosis and measures of remodeling strain and concluded that this is a promising mechanics-based target for interruption of post-MI remodeling (74). Jackson et al. (63) tracked the areas of the MI region, border zone, and remote regions from baseline to 8 wk post-MI and reported nearly 40% expansion (increase in total area) within the MI region after 2 wk compared with the baseline. At the same time point, the border zone experienced a 10% expansion, and the remote showed <5% expansion. [Fig. 2C (36, 63, 141)] Interestingly, the authors note that the rate of expansion immediately following the onset of infarction was similar in all regions (63). Although not reported in this study, a measure of remodeling strain (change from baseline length) would have likely shown an increase as the expansion of the MI region took place.
A combinatorial approach entails implantation of physical markers within the MI region, such as titanium or gold beads, and subsequent utilization of an imaging technique to track their relative positions. Using a sheep model, Blom et al. (13) used MRI tagging and titanium markers along the border zone of the MI region. Obtained results show that systolic border zone radial strain had significantly decreased by 1 wk post-MI and would continue to decline over the next 12 wk, while the MI region area gradually increased in size. Another study by Holmes et al. (59) used gold beads implanted in the LV free wall of pigs and biplane cineradiography to track deformations at 1 and 3 wk post-MI. This study used a Plexiglas phantom with embedded beads to calibrate a coordinated system for calculation of principal and remodeling strains. Reference lengths based on bead locations pre-MI were used for strain calculations along with deformed (post-MI) lengths measured at end diastole. At 1 wk, the authors report a marked circumferential LV expansion, an increase in remodeling strains, and a decrease in cycle-dependent radial and in-plane strains, with the plane of interest defined by the longitudinal and circumferential directions (tangent to the epicardium) (59).
Mechanical implications.
Post-MI healing throughout the intermediate phase significantly differs among animal models, with rodents entering a period of MI region maturation, while larger mammals continue to exhibit fibroblast proliferation and collagen deposition. Numerous factors impact recorded strain patterns, including the presence of edema, the MI size, the extent of infarction across myocardial wall, and its location with respect to the anatomical long axis of the left ventricle. Consistent mechanical observations include a decrease in MI region cyclic strain and an increase in remodeling strain. Direct comparisons among studies show quantitatively different strain magnitudes due to the use of different reference lengths, cardiac axis definition, extent of MI, location, and cardiac points of reference (systolic vs. diastolic), although general trends in strains and strain rates persist. These trends coupled with related qualitative descriptors of wall motion facilitate comparison among studies, although a comprehensive structure-function relationship of in vivo mechanics of the MI region has not yet been reached. Increased remodeling strains were noted to be most prominent in the circumferential direction, with segment lengths changing as the MI region dilates post-MI. Along with changing strain, reports indicate that wall stress is generally increased, with the most significant changes observed in the diastolic pressure range.
Late Remodeling (Beyond 14 Days)
The late-remodeling phase is characterized by lowered or absent cellular inflammatory infiltrate in the MI region (33, 34, 38, 43). The maturation of the MI region is well under way by this time point, irrespective of species. However, this does not imply that the MI region is a static structure, and dynamic changes—both cellular and extracellular—continue to occur within this region, which will, in turn, affect regional stress-strain relationships. While changes in matrix protease expression and activity continue to occur within the MI region, the most notable changes relevant to mechanical properties are likely post-translational modification of the extracellular matrix, such as collagen (32, 33, 37, 41, 42, 117). Specifically, post-translational steps in collagen maturation include cross-linking facilitated in part by lysyl-oxidase, as well as increased alignment and structural organization of the collagen matrix (33, 63, 79). For example, Lerman et al. (78) examined the effects of increased cross-linking density as a result of lysyl oxidase activity and found a correlation with enhanced tensile strength and increased passive stiffness in rabbits. Another study by Omens et al. (95) observed collagen tortuosity at low and high pressures and concluded the high stiffness of the MI region was not affected by collagen uncoiling at low pressures and implied collagen content and other three-dimensional structural arrangements of collagen could be of more import (such as cross-linking density). Moreover, the increased proliferation of fibroblasts, particularly fibroblasts with a secretive phenotype, occurs in this phase of post-MI remodeling. Thus, this phase can be associated with continued/persistent release of matrix proteases, which, in turn, will affect collagen maturation and turnover within the MI region. As a result, the species-dependent temporal differences in healing timelines (Fig. 1) likely impact mechanical measurements within the MI region. While a large body of work has been performed examining specific post-translational and cellular events in the late phase of post-MI remodeling, it remains unclear as to the relative contribution of each factor on regional stiffness. Nevertheless, what is clear about this phase of post-MI remodeling is that it is not static, entails evolving cellular and extracellular events and as such continuous changes in regional MI mechanics, and continues to be species dependent in terms of small and large animal models.
Imaging
Ultrasound.
Popović et al. (103a) used a rat model and STE to characterize segmental dysfunction throughout the left ventricle at a time point of 4–10 wk post-MI. Their results demonstrated lowered absolute values for midwall circumferential and radial strains and strain rates. The authors also report a marked difference in strain among segments, with highly fibrotic segments displaying the lowest strain in the MI region. Peak systolic and early diastolic circumferential and radial strains showed lowered absolute values and strain variations in the MI region (103a). Liao et al. (82) used 2D strain echocardiography at this same time point and animal model to assess the development of the MI region. The authors determined strain and strain rate were decreased at different magnitudes depending on location within the MI region, which was divided into anteroseptal, anterior, and anterolateral sections. The results of these studies are generally consistent in rat models at the 4-wk time point (12, 82, 103a).
A variation of STE was used in a dog model by Wong et al. (135), where speckle tracking displacement estimates in the midwall were combined with shape tracking using compactly supported radial basis functions to improve quantitative deformation analyses. At a 6-wk post-MI time point, acquired radial strain maps were consistent with previous reports of reduced MI region strains.
Sakamoto et al. (112) utilized 2D echocardiography and a sheep model to compare reperfused vs. nonreperfused MIs at 8 wk post-MI. The authors extended their measurements of remodeling strain (defined as the ratio of a baseline reference length to a deformed length post-MI) and wall motion to qualitatively assess the extent to which reperfusion impacted MI region stiffness. The authors found that although thinning still occurred, the animals in the reperfusion group had MI regions that trended toward akinesis, signifying greater stiffening in contrast to the quantified dyskenesis in the nonreperfused group (112). Comparably, a previously mentioned study in a dog model by Park et al. (97) at a similar time point reported the radial diastolic strain rates significantly decreased (by more than half in the case of radial late diastolic strain) compared with baseline values. The decrease in strain rate prompted the authors to suggest an increase in MI region stiffness in the presented sheep study, although it is important to note contractility also inherently plays a role in the calculated strain rate.
In clinical observations, Thorstensen et al. (125) used 3D echocardiography to compare global function in patients with small and large MI volume fractions (large >12% infarct volume fraction). They report decreased 3D global strain rate values in all directions (longitudinal, circumferential, and radial) that were significant in patients with large MI as compared with healthy controls. Helle-valle et al. (56) used STE at 6 mo post-MI to analyze strain, rotation, and wall motion in the segments within the MI region, border zone, and remote myocardium. This study found that the center of the MI region displayed the greatest dyskenesis with a concomitant decrease (from referent normal values) in strain, i.e., abnormal motion is most extreme at the center of the infarct with a tendency to normal motion toward the edges. Assuming a clock-face orientation, the authors observed an interesting pattern in rotation, with the counter-clockwise border zone showing hyper-rotation. The pattern of rotation then begins to shift toward the center of the MI region and trends toward hypo-rotation at the clockwise MI border. The authors suggest that systolic strain is reflective of regional contractile function and focus on this portion of the cardiac phase. Experimental findings from this study were combined with a finite element model to resolve the apparent inconsistencies between regional apical rotation and strain. The authors conclude from simulation results that an imbalance in active contractile forces from the interaction of the MI region and surrounding viable myocardium is the cause for the oppositely directed rotations at the two MI border regions and low strain in the center of the MI region (56).
MRI.
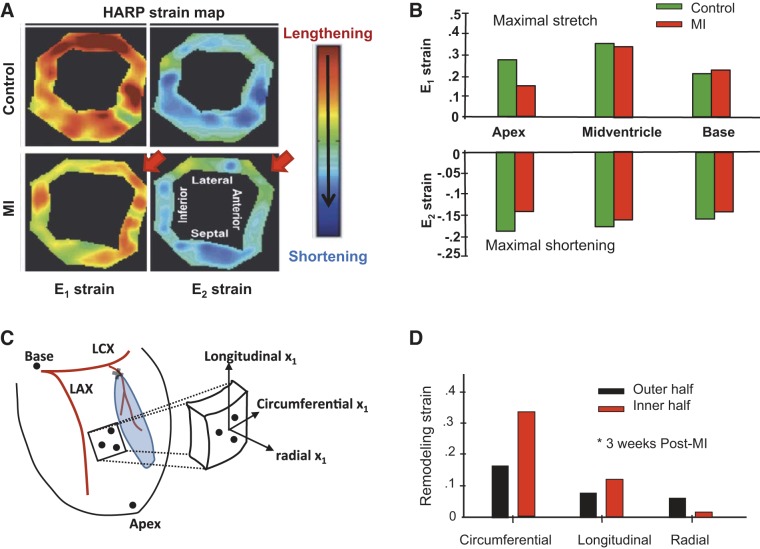
A mouse model study by Ross et al. (108) used MRI and reported that the percent change in wall thickness at 4 wk post-MI was negative in the MI region, indicative of local thinning and increased remodeling strain. This study also reported systolic wall bulging, which is representative of dyskinetic motion in the MI region. Liu et al. (84) found post-MI heterogeneous changes in strain (presented as maximal stretch and maximal shortening independent of any coordinate system) in rats at a 4-wk time point. This study used SPAMM tagging along with HARP analysis and found a reduction (compared with control values) in strain at the apex, while the strain at the LV base increased [Fig. 4, A and B (84, 142)]. These results suggest regionally dependent changes in strain occur in this late time period, as the apex and base of the left ventricle were noted to have opposing changes post-MI in a model with an anteroapical infarct (84). Espe et al. (39) studied the LV motion in a rat model at 6 wk post-MI by using phase contrast-MRI (PC-MRI). This study calculated regional circumferential strain from the acquired PC-MRI velocity data and found the peak circumferential strain to decrease both globally and in the MI region with significant heterogeneity throughout the left ventricle. This study measured the systolic portion of the cardiac phase, thus obtaining peak strain for both global and regional measurements. From these rodent studies, it can be concluded that mechanical changes (strains and other mechanical descriptors) post-MI in the late remodeling period occur in a heterogeneous manner through the MI region and the left ventricle as a whole. These changes are expressed in structural, functional (loss of contractility), and compositional variation that effectively reduces strain (with implications of an increase in stiffness) and concomitantly affects motion in the MI region.
Fig. 4.
Directional dependence. A: magnetic resonance imaging (MRI) coupled with harmonic phase analysis (HARP) yields LV strain maps from a rat immediately following induction of an MI, with MI location denoted by the red arrows. B: calculated maximal stretch (top) and maximal shortening (bottom) by HARP analysis at distinct anatomical locations (base to apex). E1 and E2 represent principal stresses independent of coordinate system. The figure panels were adapted with permission from Liu et al. (84) C: schematic of an experimental MI model in pigs, whereby radio-opaque markers (●) were implanted to allow for directional measurements of strain using biplane cineradiography. D: remodeling strain depends on direction and depth across the LV wall. The figure was adapted with permission from Zimmerman et al. (142).
Larger animal models, such as pigs used in a study by Saeed et al. (111), have indicated a reduction in MI region strain in all directions (compared with control absolute strain values), which peaked at the 5-wk point, and interestingly, slightly recovered in the circumferential and longitudinal directions by 10 wk. Similarly, Schuleri et al. (113) found that circumferential strain decreased in the MI region of pigs and demonstrated the lowest values at 30 days post-MI (instead of 5 wk) with a similar trend in the peri-infarct zone. The assertion that changes in the cycle-dependent strain are different between the MI and the peri-infarct region (border zone around MI) was the prime conclusion of that study. The authors go on to suggest that the differences in peak circumferential strain at the border of the peri-infarct zone and the MI ultimately contributes to continued remodeling (113). In a pig model, elevated dyssynchrony and a significant decrease in global peak circumferential strain were observed from 7 to 33 days post-MI in the infarct and border regions (1). Dyssynchrony refers to the abnormal activation of tissue elements in the myocardium during a normal cardiac cycle. This study showed this index of motion at an early time point (1 wk post-MI) to be a potential indicator of the extent to which MI affects mechanical synchrony at longer periods post-MI and other mechanical descriptors, such as strain. Further, the authors suggest this finding could affect therapeutic options (such as cardiac resynchronization therapy) (1).
In sheep, Walker et al. (128) used tagged MRI to build and validate an FE model at 22 wk post-MI. The model was populated with material properties acquired from biaxial mechanical testing of excised myocardium and was validated by comparison of predicted and measured (via MRI) wall stress. The results of the simulation were found to be in agreement with stress calculated from MRI data and included a dramatic increase in midwall systolic stress in the fiber and cross-fiber directions in the border zone. Using this methodology, the authors demonstrated model accuracy in terms of predicted circumferential strains in the MI, border zone, and remote regions, as well as systolic stress in the MI region (128).
Ventriculography.
Clinical observations by groups such as Mitchell et al. (91) used ventriculography to study the LV geometry, contractility, and effects of treatment at 3 wk and 1 yr post-MI. Digitized silhouettes of the left ventricle were used to quantify wall motion via tracking of demarcated chords, ultimately showing that contractile segment length (defined as the length spanning the LV wall) increased after 1 yr. Such an increase is consistent with larger end-diastolic volumes. The authors speculate that the global increase in sphericity coupled with MI region flattening together redistribute wall tension in a manner that compensates for the less compliant MI region. Hayashida et al. (55) also compared digitized silhouettes of the left ventricle over multiple cardiac cycles, and further related measured deformation to chamber pressure to generate a regional stiffness coefficient. The stiffness coefficient at 1 yr significantly increased from baseline in the MI region (apex) but slightly decreased at the base of the left ventricle.
Physical Approaches: Sonomicrometry and Markers.
Fomovsky et al. integrated sonomicrometry with imaging and biochemical analysis in a rat MI model (41). The authors report that at 6 wk post-MI, the circumferential and longitudinal strains decrease compared with normal values. However, in contrast to aforementioned findings in pigs, the MI region exhibited mechanical isotropy. The authors note that the typical shape of the MI region is different than that seen in larger animal models and suggest a causal relationship to the differential rates of cellular infiltration and inflammation between species (41). In sheep, Yankey et al. (137) used sonomicrometry crystals from 2 to 8 wk post-MI to assess MI and surrounding region deformations. Metrics of end-systolic strain and remodeling strain (using baseline reference lengths) were calculated from the sonomicrometry data. At 2 wk post-MI, fractional contraction of the MI region significantly decreased, while remodeling strain increased. Using a dog model, Theroux et al. (123) found that at 4 wk post-MI, the percent shortening of segments (determined by crystal pair lengths) was dramatically reduced in the MI region compared with normal myocardium.
Using a pig model, Holmes et al. (142) combined gold bead implantation, biplane cineradiography, and a finite element modeling to study the mechanical outcomes of remodeling 3 wk post-MI. The authors report a significant decrease in the magnitude of circumferential strain, while the longitudinal and radial strain remained similar to that of viable myocardium (58). Zimmerman et al. (142) used a similar model and technique with a bead set and a phantom to establish fiber and fiber-sheet reference coordinate systems. These reference systems allowed for calculation of remodeling strains (in principal normal directions) of the area adjacent to the MI region [Fig. 4, C and D (84, 142)]. The remodeling strains were calculated from the difference between the control and 3 wk post-MI diastolic bead configurations. Findings report differences in all directions (circumferential, radial, and longitudinal) between the outer and inner halves of the LV wall. The radial remodeling strain of the inner half was most affected, and the transmural remodeling strains showed differences depending on the depth of the myocardial wall. In the fiber coordinate system, the average transmural fiber remodeling strain was most different near the endocardium, while in the fiber sheet coordinate system, there was minor sheet reduction at the endocardium (142).
Mechanical Implications
The late remodeling phase is characterized by a highly fibrous and mature MI region across all animal models and clinical studies. The mechanical response of the MI region continues to be modulated by its size, location, extent of infarction across myocardial wall, collagen content, organization, and edema. Wall motion analyses at time points beyond 2 wk and up to a year have shown the MI to be dyskinetic with respect to adjacent or referent normal myocardium, including abnormalities in both expansion and rotation. Global strain and strain rate are consistently decreased, most notably in conjunction with large MI regions. Regional strain measurements using both physical and image-based measurements indicate mechanical anisotropy and heterogeneity within the MI region in small and large mammals, as well as a reduced strain response in the adjacent and remote myocardium. Consistent among studies is the reported increase in end-diastolic wall stress within the MI region. Bulging in the MI region was noted to decrease at the 1-yr time point, indicative of structural stiffening.
Summary
Because of temporal differences across animal models, MI region size, and location, the presence of edema, extent of infarction across myocardial wall, and measurement approaches, unifying concepts relating geometrical and compositional changes within the MI region to stiffness and other mechanical metrics, have not been forthcoming. By focusing on species- and time-dependent differences, this review underscores both the complexity and the inherent need to develop standard mechanics-based metrics.
The fundamental focus of this evaluative review was to examine regional mechanical assessment of the discrete injury following MI. As a consequence, a number of clinically relevant cardiac disease states in which ischemia plays a prominent role were not considered. This includes multifocal MI and the ischemic cardiomyopathies. With respect to ischemic cardiomyopathy, the more common clinical phenotype is that associated with a metabolic syndrome with diffuse microinfarctions and fibrosis. Whether and to what degree the observations made in terms of the temporal changes in regional mechanics discussed in this review can be translated to that of ischemic cardiomyopathy is not clear. One of the sequelae of continued adverse remodeling and dysfunction of the MI region is the progression to LV pump failure and, subsequently, the clinical spectrum of HF. With the progression of LV failure, more global changes in myocardial performance occur, which include abnormalities in contraction and relaxation within the viable remote myocardium, as well as the MI region. Moreover, with progressive LV dilation secondary to adverse post-MI remodeling, a plateau in the LV ejection-preload relation can occur, which has also been termed exhaustion of the Frank-Starling relationship (48, 76). While a multifactorial process, changes within the ECM likely contribute to the shift in these LV functional relationships, which include a loss of normal collagen architecture and support within the myocardium (26, 114). It must be recognized that these more global events, such as LV dilation and failure, were not taken into account in this review, as these are multifactorial processes, and as such, this review only examined one small dimension of this complex pathophysiological phenotype.
The majority of past studies focused upon systolic strain/stiffness measurements in the post-MI period, which reflect the loss of contractile units or have examined strain in the post-MI period without a focus on the timing of the cardiac cycle or region (Table 2). In this review, we focus on how continuum mechanical quantities (i.e., stress and strain) vary over the cardiac cycle in the post-MI context and how reported changes are related to both local loss of contractility and alterations in myocardial composition. Using these factors as guiding principles, we put forth the following recommendations to be considered to improve the standardization and interpretation of post-MI remodeling [Fig. 5 (137)].
Table 2.
Tabulated studies
| Animal Model | Study | Time Frame Post-MI | Post-MI Mechanical Variables | Technique |
|---|---|---|---|---|
| Mouse | (108) | Early–Late | ↓ ER | MRI |
| Rat | (140) | Early–Late | ↓Global E | MRI/SPAMM |
| Rat | (7) | Early–Intermediate | ↓ Global EC, ER, EL | LS-STE |
| Rat | (103a) | Late | ↓ EC dependent on fibrosis | STE |
| Rat | (82) | Early–Late | ↓ End-diastolic ER, EC, SRC, SRR | 2D SE |
| Rat | (12) | Early–Late | ↓ Global and regional ER, SR | STE |
| Rat | (84) | Early–Late | ↓ E1, E2 | MRI/SPAMM |
| Rat | (39) | Late | ↓ Global peak EC | PC-MR |
| Rat | (41) | Intermediate–Late | ↓ EC, EL | Sonomicrometry |
| Dog | (97) | Intermediate–Late | ↓ Diastolic SRR, SRL | Doppler |
| Dog | (77) | Intermediate | ↓E1 apical region | MRI/SPAMM |
| Dog | (135) | Late | ↓ ER | 4DSE/MRI |
| Sheep | (74) | Late | ↓ Peak E | Sonomicrometry |
| Sheep | (63) | Intermediate | ↓ ES | Sonomicrometry |
| Sheep | (13) | Early–Late | ↓ Systolic ER | MRI |
| Sheep | (112) | Early–Late | ↓ Stretch | 2D SE |
| Sheep | (137) | Late | ↑ RE in MI and border zone | Sonomicrometry |
| Pig | (111) | Early–Late | ↓ Peak ER, EL, EC | MRI |
| Pig | (113) | Late | ↓ Peak EC | MRI |
| Pig | (116) | Intermediate–Late | ↓ EC. ER, EL | MRI/SPAMM |
| Pig | (59) | Early–Late | ↓ EC, ER, EL | Biplane cineradiography |
| Pig | (1) | Early–Late | ↓Global and regional peak EC | CMR |
| Pig | (142) | Late | ↑ REC, RER | Biplane cineradiography |
| Human | (36) | Early | ↓ EL, EC | TDI,SDE,MRI |
| Human | (141) | Early | ↓ SRS, SRD, SRA | TDI, SRI, Ce-MRI, |
| Human | (14) | Early | ↓ ER, EC, EL in MI and border zone | MRI |
| Human | (46) | Early | ↓ EC | MRI |
| Human | (47) | Early | ↓ EC in segments with early hypo/delayed hyper enhancement. | Ce-MRI |
| Human | (9) | Intermediate | ↓ Peak EC, ER, SRC, SRR | 2DSE/Ce-MRI |
| Human | (124) | Late | ↓ End systolic global EL, EC, ER | STE |
| Human | (56) | Late | ↓ End systolic regional E | TDI |
| Human | (55) | Late | ↑ Regional wall stress | Left ventriculography |
Studies are grouped by species, time frame, mechanical variables of note, along with techniques used for quick reference from the text. All strains reported are cycle-dependent strains, unless otherwise noted, and time periods are defined in the article. EC, circumferential strain; ER, radial strain; EL, longitudinal strain; RE, remodeling strain; REC, remodeling circumferential strain; RER, remodeling radial strain; SRC, circumferential strain rate; SRR, radial strain rate; SRL, longitudinal strain rate. Principal strains are defined within the text and denoted as E1 and E2.
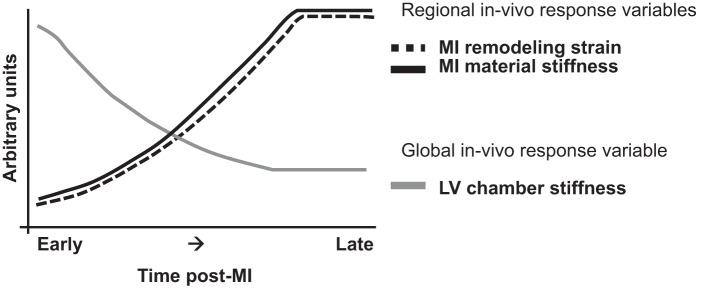
Fig. 5.
Summary recommendations. Regional and global measurements were recommended for inclusion in future experimental studies. From the data contained in this review, this figure underscores the inverse trends in post-MI changes in local material properties and behavior (MI remodeling strain and stiffness) and global mechanical behavior post-MI (LV chamber stiffness). It is important to note that this figure only shows a general view of these trends, as we have stated throughout this review. Data representing the diastolic phase of the cardiac cycle are not as well reported as the systolic and do not, therefore, allow for a more detailed comparison with respect to the different cardiac phases. Although the specific time course of these changes is animal model-dependent, the trends represented by this figure are universal from the references currently contained in this review (73, 112, 137, 142).
Recommendation One: Remodeling Strain
The reporting of strain as a primary metric of value has been a constant among the literature cited. The Lagrangian strain is (in the literature contained herein) often calculated with a reference length taken at a specific point in the cardiac cycle and time post-MI, thus, representing a cyclic strain. Largely, the trends in cyclic strain post-MI show regionally and directionally dependent decreases, while remodeling strain (where reported) shows an opposing trend (increasing with time) [Fig. 5 (137)]. Remodeling strain is reflective of the changing geometry (dilation post-MI) and perhaps better characterizes the underlying transitions of the damaged myocardium. In light of this, we make our first recommendation on the consistent reporting of remodeling strain in experimental studies. Although not a new concept, only a handful of in vivo studies report this metric, in which the reference length is defined at baseline and used thereafter for calculations (59, 63, 74).
Recommendation Two: Strain in the Diastolic Phase
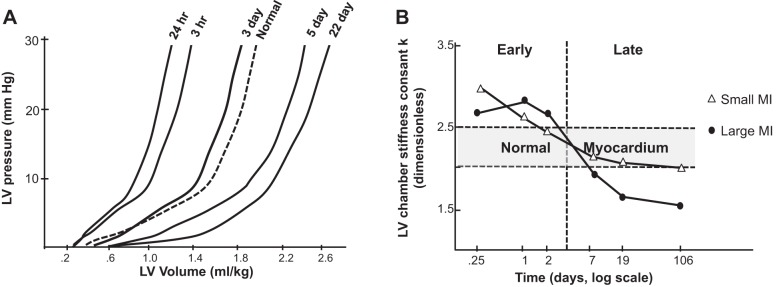
Our second recommendation pertains to the acquisition of strain data during the diastolic phase, which we view as essential to both experimental and clinical studies that aim to characterize MI-induced changes in myocardial mechanical properties. Many studies report systolic strain as an index of contractility/ejection performance, the utility of which is established. However, mechanical behavior in this cardiac phase can be influenced by significant forces exerted on the MI region by the surrounding viable myocardium, therefore, complicating true delineation of regional stress-strain relationships and, thus, mechanical property identification. In recommending diastole (vs. systole) as an informative phase over which to gather material property data on the MI region, we contend that this approach minimizes the confounding influence of active contractive forces from surrounding viable myocardium on obtained measurements. However, it is important to note that even in the diastolic phase, in vivo measurements of stiffness (chamber level, derived from load–dimension relations, and regional, derived from local stress-strain relationships) can still be affected by dyskinesis, microvascular blood volume, and impaired myocyte relaxation. Therefore, carefully designed ex vivo studies that can fully isolate passive material properties remain an important complementary approach with respect to a comprehensive evaluation of the material properties of the MI region. Often, ex vivo studies are used to isolate variables of interest (such as stiffness) and to perhaps amplify the observable effects by means of control over applied loads. Canonical examples of ex vivo experiments with intact heart preparations include those represented in Fig. 6 (21, 81, 95, 101). These few examples of ex vivo intact preparation studies on rodent models support the important factors derived from in vivo findings with the compiled results corroborating the potential effects of important variables in the isolated case of passive deformation, such as time, species, size, composition, and loading conditions (here, pressure range). The net effect of the MI region transitions includes a visible and measurable difference in strain at a low pressure range and a local reduction (from a control value) in peak strain over the cardiac cycle, despite the dilation known to occur in the remodeling process (the latter is addressed by our first recommendation).
Fig. 6.
In vivo chamber stiffness. Summary of reported LV pressure-volume relationships with passive filling and derived calculations of chamber stiffness following MI. The representation of passive stiffness is not wholly encompassing of mechanics in vivo, as the components of active contractility have been removed. A: in a rat MI model, the passive pressure-volume curves initially shifted to the left (days 0–3) and later to the right (days 5–22) with respect to the referent normal response. Adapted with permission from Raya et al. (105). B: temporal variation in LV chamber stiffness was reported in a rat MI model and was found to depend on the absolute MI size. The figure was adapted with permission from Pfeffer et al. (101).
Recommendation Three: Data Repository and Modeling
The final recommendation is the establishment of an appropriate database for data from ex vivo and in vivo studies. This would be an important asset to ease comparisons and perhaps validate emerging techniques for the purposes of computational/mathematical modeling. More recently, data from ex vivo experiments of both intact preparations and tensile testing are being incorporated into predictive computational models, wherein acquired mechanical measurements are used to develop and validate simulations of MI region behavior (31, 60, 61, 130). Already, findings from studies using FE models have shown predictive value when results were compared with those from imaging approaches (52, 110, 128, 140). Other in silico studies have used in vivo parameters for their geometric basis and for comparison, as well as for using material parameters from biaxial tensile experiments (73, 75, 129). To successfully integrate data from experimental and clinical studies, fastidious cataloging must take place, while paying close attention to the factors identified throughout this review. In doing so, a scaling factor between species stemming from the differences in healing timetables can perhaps be standardized. The fundamental advantage of these models is the possibility to examine in isolation the effect of key variables in the complex remodeling process (110, 128). Thus, invaluable insight can be gained that would otherwise be costly (due to the requisite study size) or be unattainable in animal studies/clinical observation, emphasizing the need for a readily available database from which mechanical properties of the post-MI myocardium of different species, size, location, and maturity can be obtained. Ultimately, these models could aid in the design and evaluation of therapeutic strategies intended to alter LV mechanics in a post-MI context.
GRANTS
This work was supported by the National Heart, Lung, and Blood Institute Grants HL-11090, HL-089944, HL-43617, HL-67922, and a Merit Award from the Veterans’ Affairs Health Administration.
DISCLOSURES
No conflicts of interest, financial or otherwise, are declared by the authors.
AUTHOR CONTRIBUTIONS
E.R. and F.G.S. performed experiments; E.R., T.S., and F.G.S. analyzed data; E.R., T.S., and F.G.S. interpreted results of experiments; E.R. prepared figures; E.R. and T.S. drafted manuscript; E.R., T.S., and F.G.S. edited and revised manuscript; E.R., T.S., and F.G.S. approved final version of manuscript.
ACKNOWLEDGMENTS
The authors express sincere appreciation to Ashley Sapp for editorial assistance.
REFERENCES
- 1.Abd-Elmoniem KZ, Tomas MS, Sasano T, Soleimanifard S, Vonken E-JP, Youssef A, Agarwal H, Dimaano VL, Calkins H, Stuber M, Prince JL, Abraham TP, Abraham MR. Assessment of distribution and evolution of mechanical dyssynchrony in a porcine model of myocardial infarction by cardiovascular magnetic resonance. J Cardiovasc Magn Reson 14: 1, 2012. doi: 10.1186/1532-429X-14-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Al-Mallah MH, Shareef MN. The role of cardiac magnetic resonance imaging in the assessment of non-ischemic cardiomyopathy. Heart Fail Rev 16: 369–380, 2011. doi: 10.1007/s10741-010-9221-3. [DOI] [PubMed] [Google Scholar]
- 3.Amini AA, Chen Y, Elayyadi M, Radeva P. Tag surface reconstruction and tracking of myocardial beads from SPAMM-MRI with parametric B-spline surfaces. IEEE Trans Med Imaging 20: 94–103, 2001. doi: 10.1109/42.913176. [DOI] [PubMed] [Google Scholar]
- 4.Amirhamzeh MM, Hsu DT, Cabreriza SE, Jia CX, Spotnitz HM. Myocardial edema: comparison of effects on filling volume and stiffness of the left ventricle in rats and pigs. Ann Thorac Surg 63: 1293–1297, 1997. doi: 10.1016/S0003-4975(97)00080-5. [DOI] [PubMed] [Google Scholar]
- 5.Ananthasubramaniam K, Dhar R, Cavalcante JL. Role of multimodality imaging in ischemic and non-ischemic cardiomyopathy. Heart Fail Rev 16: 351–367, 2011. doi: 10.1007/s10741-010-9218-y. [DOI] [PubMed] [Google Scholar]
- 6.Artis NJ, Oxborough DL, Williams G, Pepper CB, Tan LB. Two-dimensional strain imaging: a new echocardiographic advance with research and clinical applications. Int J Cardiol 123: 240–248, 2008. doi: 10.1016/j.ijcard.2007.02.046. [DOI] [PubMed] [Google Scholar]
- 7.Bachner-Hinenzon N, Ertracht O, Malka A, Leitman M, Vered Z, Binah O, Adam D. Layer-specific strain analysis: investigation of regional deformations in a rat model of acute versus chronic myocardial infarction. Am J Physiol Heart Circ Physiol 303: H549–H558, 2012. doi: 10.1152/ajpheart.00294.2012. [DOI] [PubMed] [Google Scholar]
- 8.Baxter SC, Morales MO, Goldsmith EC. Adaptive changes in cardiac fibroblast morphology and collagen organization as a result of mechanical environment. Cell Biochem Biophys 51: 33–44, 2008. doi: 10.1007/s12013-008-9013-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Becker M, Bilke E, Kühl H, Katoh M, Kramann R, Franke A, Bücker A, Hanrath P, Hoffmann R. Analysis of myocardial deformation based on pixel tracking in two dimensional echocardiographic images enables quantitative assessment of regional left ventricular function. Heart 92: 1102–1108, 2006. doi: 10.1136/hrt.2005.077107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Becker M, Hoffmann R, Kühl HP, Grawe H, Katoh M, Kramann R, Bücker A, Hanrath P, Heussen N. Analysis of myocardial deformation based on ultrasonic pixel tracking to determine transmurality in chronic myocardial infarction. Eur Heart J 27: 2560–2566, 2006. doi: 10.1093/eurheartj/ehl288. [DOI] [PubMed] [Google Scholar]
- 12.Bhan A, Sirker A, Zhang J, Protti A, Catibog N, Driver W, Botnar R, Monaghan MJ, Shah AM. High-frequency speckle tracking echocardiography in the assessment of left ventricular function and remodeling after murine myocardial infarction. Am J Physiol Heart Circ Physiol 306: H1371–H1383, 2014. doi: 10.1152/ajpheart.00553.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Blom AS, Pilla JJ, Arkles J, Dougherty L, Ryan LP, Gorman JH III, Acker MA, Gorman RC. Ventricular restraint prevents infarct expansion and improves borderzone function after myocardial infarction: a study using magnetic resonance imaging, three-dimensional surface modeling, and myocardial tagging. Ann Thorac Surg 84: 2004–2010, 2007. doi: 10.1016/j.athoracsur.2007.06.062. [DOI] [PubMed] [Google Scholar]
- 14.Bogaert J, Bosmans H, Maes A, Suetens P, Marchal G, Rademakers FE. Remote myocardial dysfunction after acute anterior myocardial infarction: impact of left ventricular shape on regional function: a magnetic resonance myocardial tagging study. J Am Coll Cardiol 35: 1525–1534, 2000. doi: 10.1016/S0735-1097(00)00601-X. [DOI] [PubMed] [Google Scholar]
- 15.Bogen DK, McMahon TA. Do cardiac aneurysms blow out? Biophys J 27: 301–316, 1979. doi: 10.1016/S0006-3495(79)85219-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Braunwald E, Kloner RA. The stunned myocardium: prolonged, postischemic ventricular dysfunction. Circulation 66: 1146–1149, 1982. doi: 10.1161/01.CIR.66.6.1146. [DOI] [PubMed] [Google Scholar]
- 17.Braunwald E, Kloner RA. Myocardial reperfusion: a double-edged sword? J Clin Invest 76: 1713–1719, 1985. doi: 10.1172/JCI112160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Braunwald E. Biomarkers in heart failure. N Engl J Med 358: 2148–2159, 2008. doi: 10.1056/NEJMra0800239. [DOI] [PubMed] [Google Scholar]
- 19.Bujak M, Frangogiannis NG. The role of TGF-β signaling in myocardial infarction and cardiac remodeling. Cardiovasc Res 74: 184–195, 2007. doi: 10.1016/j.cardiores.2006.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Butt RP, Bishop JE. Mechanical load enhances the stimulatory effect of serum growth factors on cardiac fibroblast procollagen synthesis. J Mol Cell Cardiol 29: 1141–1151, 1997. doi: 10.1006/jmcc.1996.0347. [DOI] [PubMed] [Google Scholar]
- 21.Capasso JM, Li P, Zhang X, Anversa P. Heterogeneity of ventricular remodeling after acute myocardial infarction in rats after acute. Am J Physiol Heart Circ Physiol 262: H486–H495, 1992. [DOI] [PubMed] [Google Scholar]
- 22.Carver W, Nagpal ML, Nachtigal M, Borg TK, Terracio L. Collagen expression in mechanically stimulated cardiac fibroblasts. Circ Res 69: 116–122, 1991. doi: 10.1161/01.RES.69.1.116. [DOI] [PubMed] [Google Scholar]
- 23.Cavasin MA, Sankey SS, Yu A-L, Menon S, Yang X-P. Estrogen and testosterone have opposing effects on chronic cardiac remodeling and function in mice with myocardial infarction. Am J Physiol Heart Circ Physiol 284: H1560–H1569, 2003. doi: 10.1152/ajpheart.01087.2002. [DOI] [PubMed] [Google Scholar]
- 24.Chan J, Hanekom L, Wong C, Leano R, Cho G-Y, Marwick TH. Differentiation of subendocardial and transmural infarction using two-dimensional strain rate imaging to assess short-axis and long-axis myocardial function. J Am Coll Cardiol 48: 2026–2033, 2006. doi: 10.1016/j.jacc.2006.07.050. [DOI] [PubMed] [Google Scholar]
- 25.Christman KL, Lee RJ. Biomaterials for the treatment of myocardial infarction. J Am Coll Cardiol 48: 907–913, 2006. doi: 10.1016/j.jacc.2006.06.005. [DOI] [PubMed] [Google Scholar]
- 26.Chung CS, Granzier HL. Contribution of titin and extracellular matrix to passive pressure and measurement of sarcomere length in the mouse left ventricle. J Mol Cell Cardiol 50: 731–739, 2011. doi: 10.1016/j.yjmcc.2011.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Clark NR, Reichek N, Bergey P, Hoffman EA, Brownson D, Palmon L, Axel L. Circumferential myocardial shortening in the normal human left ventricle. Assessment by magnetic resonance imaging using spatial modulation of magnetization. Circulation 84: 67–74, 1991. doi: 10.1161/01.CIR.84.1.67. [DOI] [PubMed] [Google Scholar]
- 28.Cleutjens JP, Kandala JC, Guarda E, Guntaka RV, Weber KT. Regulation of collagen degradation in the rat myocardium after infarction. J Mol Cell Cardiol 27: 1281–1292, 1995. doi: 10.1016/S0022-2828(05)82390-9. [DOI] [PubMed] [Google Scholar]
- 29.Cleutjens JP, Verluyten MJ, Smiths JF, Daemen MJ. Collagen remodeling after myocardial infarction in the rat heart. Am J Pathol 147: 325–338, 1995. [PMC free article] [PubMed] [Google Scholar]
- 30.Cohn JN, Ferrari R, Sharpe N, Forum I. Cardiac remodeling—concepts and clinical implications : a consensus paper from an international forum on cardiac remodeling. J Am Coll Cardiol 35: 569–582, 2000. [DOI] [PubMed] [Google Scholar]
- 31.Costa KD, Holmes JW, Mcculloch AD. Modelling cardiac mechanical properties in three dimensions. Philos Trans R Soc A Math Phys Eng Sci 359: 1233–1250, 2001. doi: 10.1098/rsta.2001.0828. [DOI] [Google Scholar]
- 32.Desmoulière A, Geinoz A, Gabbiani F, Gabbiani G. Transforming growth factor-β1 induces alpha-smooth muscle actin expression in granulation tissue myofibroblasts and in quiescent and growing cultured fibroblasts. J Cell Biol 122: 103–111, 1993. doi: 10.1083/jcb.122.1.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dobaczewski M, Bujak M, Zymek P, Ren G, Entman ML, Frangogiannis NG. Extracellular matrix remodeling in canine and mouse myocardial infarcts. Cell Tissue Res 324: 475–488, 2006. doi: 10.1007/s00441-005-0144-6. [DOI] [PubMed] [Google Scholar]
- 34.Dobaczewski M, Gonzalez-Quesada C, Frangogiannis NG. The extracellular matrix as a modulator of the inflammatory and reparative response following myocardial infarction. J Mol Cell Cardiol 48: 504–511, 2010. doi: 10.1016/j.yjmcc.2009.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Eaton LW, Weiss JL, Bulkley BH, Garrison JB, Weisfeldt ML. Regional cardiac dilatation after acute myocardial infarction. N Engl J Med 300: 57–62, 1979. [DOI] [PubMed] [Google Scholar]
- 36.Edvardsen T, Gerber BL, Garot J, Bluemke DA, Lima JAC, Smiseth OA. Quantitative assessment of intrinsic regional myocardial deformation by Doppler strain rate echocardiography in humans: validation against three-dimensional tagged magnetic resonance imaging. Circulation 106: 50–56, 2002. doi: 10.1161/01.CIR.0000019907.77526.75. [DOI] [PubMed] [Google Scholar]
- 37.Eghbali M, Tomek R, Sukhatme VP, Woods C, Bhambi B. Differential effects of transforming growth factor-β1 and phorbol myristate acetate on cardiac fibroblasts. Regulation of fibrillar collagen mRNAs and expression of early transcription factors. Circ Res 69: 483–490, 1991. doi: 10.1161/01.RES.69.2.483. [DOI] [PubMed] [Google Scholar]
- 38.Ertl G, Frantz S. Healing after myocardial infarction. Cardiovasc Res 66: 22–32, 2005. doi: 10.1016/j.cardiores.2005.01.011. [DOI] [PubMed] [Google Scholar]
- 39.Espe EKS, Aronsen JM, Skårdal K, Schneider JE, Zhang L, Sjaastad I. Novel insight into the detailed myocardial motion and deformation of the rodent heart using high-resolution phase contrast cardiovascular magnetic resonance. J Cardiovasc Magn Reson 15: 82, 2013. doi: 10.1186/1532-429X-15-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Fishbein MC, Maclean D, Maroko PR. Experimental myocardial infarction in the rat: qualitative and quantitative changes during pathologic evolution. Am J Pathol 90: 57–70, 1978. [PMC free article] [PubMed] [Google Scholar]
- 41.Fomovsky GM, Holmes JW. Evolution of scar structure, mechanics, and ventricular function after myocardial infarction in the rat. Am J Physiol Heart Circ Physiol 298: H221–H228, 2010. doi: 10.1152/ajpheart.00495.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Fomovsky GM, Thomopoulos S, Holmes JW. Contribution of extracellular matrix to the mechanical properties of the heart. J Mol Cell Cardiol 48: 490–496, 2010. doi: 10.1016/j.yjmcc.2009.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Frangogiannis NG, Smith CW, Entman ML. The inflammatory response in myocardial infarction. Cardiovasc Res 53: 31–47, 2002. doi: 10.1016/S0008-6363(01)00434-5. [DOI] [PubMed] [Google Scholar]
- 44.Frantz S, Bauersachs J, Ertl G, Klinik M, Würzburg U. Post-infarct remodelling: Contribution of wound healing and inflammation. Cardiovasc Res 81: 474–481, 2009. doi: 10.1093/cvr/cvn292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Garot J, Bluemke DA, Osman NF, Rochitte CE, McVeigh ER, Zerhouni EA, Prince JL, Lima JA. Fast determination of regional myocardial strain fields from tagged cardiac images using harmonic phase MRI. Circulation 101: 981–988, 2000. doi: 10.1161/01.CIR.101.9.981. [DOI] [PubMed] [Google Scholar]
- 46.Gerber BL, Garot J, Bluemke DA, Wu KC, Lima JAC. Accuracy of contrast-enhanced magnetic resonance imaging in predicting improvement of regional myocardial function in patients after acute myocardial infarction. Circulation 106: 1083–1089, 2002. doi: 10.1161/01.CIR.0000027818.15792.1E. [DOI] [PubMed] [Google Scholar]
- 47.Geyer H, Caracciolo G, Abe H, Wilansky S, Carerj S, Gentile F, Nesser H-J, Khandheria B, Narula J, Sengupta PP. Assessment of myocardial mechanics using speckle tracking echocardiography: fundamentals and clinical applications. J Am Soc Echocardiogr 23: 351–369, 2010. doi: 10.1016/j.echo.2010.02.015. [DOI] [PubMed] [Google Scholar]
- 48.Gill R, Jones B, Corbly A, Ohad D, Smith G. Exhaustion of the Frank–Starling mechanism in conscious dogs with heart failure induced by chronic coronary microembolization. Life Sci 79: 536–544, 2006. 10.1016/j.lfs.2006.01.045. [DOI] [PubMed] [Google Scholar]
- 49.Gjesdal O, Helle-Valle T, Hopp E, Lunde K, Vartdal T, Aakhus S, Smith H-J, Ihlen H, Edvardsen T. Noninvasive separation of large, medium, and small myocardial infarcts in survivors of reperfused ST-elevation myocardial infarction: a comprehensive tissue Doppler and speckle-tracking echocardiography study. Circ Cardiovasc Imaging 1: 189–196, 2008. doi: 10.1161/CIRCIMAGING.108.784900. [DOI] [PubMed] [Google Scholar]
- 50.Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Blaha MJ, Dai S, Ford ES, Fox CS, Franco S, Fullerton HJ, Gillespie C, Hailpern SM, Heit JA, Howard VJ, Huffman MD, Judd SE, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Mackey RH, Magid DJ, Marcus GM, Marelli A, Matchar DB, McGuire DK, Mohler ER III, Moy CS, Mussolino ME, Neumar RW, Nichol G, Pandey DK, Paynter NP, Reeves MJ, Sorlie PD, Stein J, Towfighi A, Turan TN, Virani SS, Wong ND, Woo D, Turner MB; American Heart Association Statistics Committee and Stroke Statistics Subcommittee . Heart disease and stroke statistics—2014 update: a report from the American Heart Association. Circulation 129: e28–e292, 2014. doi: 10.1161/01.cir.0000441139.02102.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Borden WB, Bravata DM, Dai S, Ford ES, Fox CS, Franco S, Fullerton HJ, Gillespie C, Hailpern SM, Heit JA, Howard VJ, Huffman MD, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Magid D, Marcus GM, Marelli A, Matchar DB, McGuire DK, Mohler ER, Moy CS, Mussolino ME, Nichol G, Paynter NP, Schreiner PJ, Sorlie PD, Stein J, Turan TN, Virani SS, Wong ND, Woo D, Turner MB; American Heart Association Statistics Committee and Stroke Statistics Subcommittee . Heart disease and stroke statistics—2013 update: a report from the American Heart Association. Circulation 127: e6–e245, 2013. doi: 10.1161/CIR.0b013e31828124ad. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Göktepe S, Acharya SNS, Wong J, Kuhl E. Computational modeling of passive myocardium. Int J Numer Methods Biomed Eng 27: 1–12, 2011. doi: 10.1002/cnm.1402. [DOI] [Google Scholar]
- 53.Gorcsan J III, Tanaka H. Echocardiographic assessment of myocardial strain. J Am Coll Cardiol 58: 1401–1413, 2011. doi: 10.1016/j.jacc.2011.06.038. [DOI] [PubMed] [Google Scholar]
- 54.Gupta KB, Ratcliffe MB, Fallert MA, Edmunds LH Jr, Bogen DK. Changes in passive mechanical stiffness of myocardial tissue with aneurysm formation. Circulation 89: 2315–2326, 1994. doi: 10.1161/01.CIR.89.5.2315. [DOI] [PubMed] [Google Scholar]
- 55.Hayashida W, Van Eyll C, Rousseau MF, Pouleur H; The SOLVD Investigators . Regional remodeling and nonuniform changes in diastolic function in patients with left ventricular dysfunction: modification by long-term enalapril treatment. J Am Coll Cardiol 22: 1403–1410, 1993. [DOI] [PubMed] [Google Scholar]
- 56.Helle-valle T, Remme EW, Lyseggen E, Pettersen E, Vartdal T, Opdahl A, Smith H, Osman NF, Ihlen H, Edvardsen T, Smiseth OA. Clinical assessment of left ventricular rotation and strain: a novel approach for quantification of function in infarcted myocardium and its border zones. Am J Physiol Heart Circ Physiol 297: H257–H267, 2009. doi: 10.1152/ajpheart.01116.2008. [DOI] [PubMed] [Google Scholar]
- 57.Hochman JS, Bulkley BH. Expansion of acute myocardial infarction: an experimental study. Circulation 65: 1446–1450, 1982. doi: 10.1161/01.CIR.65.7.1446. [DOI] [PubMed] [Google Scholar]
- 58.Holmes JW, Nunez JA, Covell JW. Functional implications of myocardial scar structure. Am J Physiol Heart Circ Physiol 272: H2123–H2130, 1997. [DOI] [PubMed] [Google Scholar]
- 59.Holmes JW, Yamashita H, Waldman LK, Covell JW. Scar remodeling and transmural deformation after infarction in the pig. Circulation 90: 411–420, 1994. doi: 10.1161/01.CIR.90.1.411. [DOI] [PubMed] [Google Scholar]
- 60.Holzapfel GA, Ogden RW. Constitutive modelling of passive myocardium: a structurally based framework for material characterization. Philos Trans A Math Phys Eng Sci 367: 3445–3475, 2009. doi: 10.1098/rsta.2009.0091. [DOI] [PubMed] [Google Scholar]
- 61.Hunter PJ, McCulloch AD, ter Keurs HE. Modelling the mechanical properties of cardiac muscle. Prog Biophys Mol Biol 69: 289–331, 1998. doi: 10.1016/S0079-6107(98)00013-3. [DOI] [PubMed] [Google Scholar]
- 62.Ifkovits JL, Tous E, Minakawa M, Morita M, Robb JD, Koomalsingh KJ. Injec hydrogel properties influence infarct expansion and extent of postinfarction left ventricular remodeling in an ovine model. Proc Natl Acad Sci USA 107: 11,507–11,512, 2010. doi: 10.1073/pnas.1004097107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Jackson BM, Gorman JH III, Moainie SL, Guy TS, Narula N, Narula J, St. John-Sutton MG, Edmunds LH Jr, Gorman RC. Extension of borderzone myocardium in postinfarction dilated cardiomyopathy. J Am Coll Cardiol 40: 1160–1167, 2002. doi: 10.1016/S0735-1097(02)02121-6. [DOI] [PubMed] [Google Scholar]
- 64.Jaeschke H, Smith CW. Mechanisms of neutrophil-induced parenchymal cell injury. J Leukoc Biol 61: 647–653, 1997. [DOI] [PubMed] [Google Scholar]
- 65.Jugdutt BI, Amy RWM. Healing after myocardial infarction in the dog: changes in infarct hydroxyproline and topography. J Am Coll Cardiol 7: 91–102, 1986. doi: 10.1016/S0735-1097(86)80265-0. [DOI] [PubMed] [Google Scholar]
- 66.Jugdutt BI, Joljart MJ, Khan MI. Rate of collagen deposition during healing and ventricular remodeling after myocardial infarction in rat and dog models. Circulation 94: 94–101, 1996. doi: 10.1161/01.CIR.94.1.94. [DOI] [PubMed] [Google Scholar]
- 67.Jugdutt BI. Prevention of ventricular remodelling post myocardial infarction: timing and duration of therapy. Can J Cardiol 9: 103–114, 1993. [PubMed] [Google Scholar]
- 68.Jugdutt BI. Cyclooxygenase inhibition and adverse remodeling during healing after myocardial infarction. Circulation 115: 288–291, 2007. doi: 10.1161/CIRCULATIONAHA.106.675306. [DOI] [PubMed] [Google Scholar]
- 69.Kang T, Humphrey JD, Yin FC. Comparison of biaxial mechanical properties of excised endocardium and epicardium. Am J Physiol Heart Circ Physiol 270: H2169–H2176, 1996. [DOI] [PubMed] [Google Scholar]
- 70.Kellar RS, Shepherd BR, Larson DF, Naughton GK, Williams SK. Cardiac patch constructed from human fibroblasts attenuates reduction in cardiac function after acute infarct. Tissue Eng 11: 1678–1687, 2005. doi: 10.1089/ten.2005.11.1678. [DOI] [PubMed] [Google Scholar]
- 71.Kelley ST, Malekan R, Gorman JH III, Jackson BM, Gorman RC, Suzuki Y, Plappert T, Bogen DK, St. John Sutton MG, Edmunds LH. Restraining infarct expansion preserves left ventricular geometry and function after acute anteroapical infarction. Circulation 99: 135–142, 1999. doi: 10.1161/01.CIR.99.1.135. [DOI] [PubMed] [Google Scholar]
- 73.Kichula ET, Wang H, Dorsey SM, Szczesny SE, Elliott DM, Burdick JA, Wenk JF. Experimental and computational investigation of altered mechanical properties in myocardium after hydrogel injection. Ann Biomed Eng 42: 1546–1556, 2014. doi: 10.1007/s10439-013-0937-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Kilic A, Li T, Nolan TDC, Nash JR, Li S, Prastein DJ, Schwartzbauer G, Moainie SL, Yankey GK, DeFilippi C, Wu Z, Griffith BP. Strain-related regional alterations of calcium-handling proteins in myocardial remodeling. J Thorac Cardiovasc Surg 132: 900–908, 2006. doi: 10.1016/j.jtcvs.2006.07.016. [DOI] [PubMed] [Google Scholar]
- 75.Klepach D, Lee LC, Wenk JF, Ratcliffe MB, Zohdi TI, Navia JA, Kassab GS, Kuhl E, Guccione JM. Growth and remodeling of the left ventricle: A case study of myocardial infarction and surgical ventricular restoration. Mech Res Commun 42: 134–141, 2012. doi: 10.1016/j.mechrescom.2012.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Komamura K, Shannon RP, Ihara T, Shen YT, Mirsky I, Bishop SP, Vatner SF. Exhaustion of Frank-Starling mechanism in conscious dogs with heart failure. Am J Physiol Heart Circ Physiol 265: H1119–H1131, 1993. [DOI] [PubMed] [Google Scholar]
- 77.Kraitchman DL, Young AA, Bloomgarden DC, Fayad ZA, Dougherty L, Ferrari VA, Boston RC, Axel L. Integrated MRI assessment of regional function and perfusion in canine myocardial infarction. Magn Reson Med 40: 311–326, 1998. doi: 10.1002/mrm.1910400217. [DOI] [PubMed] [Google Scholar]
- 78.Kukielka GL, Smith CW, LaRosa GJ, Manning AM, Mendoza LH, Daly TJ, Hughes BJ, Youker KA, Hawkins HK, Michael LH. Interleukin-8 gene induction in the myocardium after ischemia and reperfusion in vivo. J Clin Invest 95: 89–103, 1995. doi: 10.1172/JCI117680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Leask A. TGFbeta, cardiac fibroblasts, and the fibrotic response. Cardiovasc Res 74: 207–212, 2007. doi: 10.1016/j.cardiores.2006.07.012. [DOI] [PubMed] [Google Scholar]
- 80.Lee AA, Delhaas T, McCulloch AD, Villarreal FJ. Differential responses of adult cardiac fibroblasts to in vitro biaxial strain patterns. J Mol Cell Cardiol 31: 1833–1843, 1999. doi: 10.1006/jmcc.1999.1017. [DOI] [PubMed] [Google Scholar]
- 81.Lerman RH, Apstein CS, Kagan HM, Osmers EL, Chichester CO, Vogel WM, Connelly CM, Steffee WP. Myocardial healing and repair after experimental infarction in the rabbit. Circ Res 53: 378–388, 1983. doi: 10.1161/01.RES.53.3.378. [DOI] [PubMed] [Google Scholar]
- 82.Liao SS, Ruan QY, Lin MY, Yan L. Value of segmental myocardial strain by 2-dimensional strain echocardiography for assessment of scar area induced in a rat model of myocardial infarction. Cardiovasc Ultrasound 10: 17, 2012. doi: 10.1186/1476-7120-10-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Lijnen PJ, Petrov VV, Fagard RH. Induction of cardiac fibrosis by transforming growth factor-β1. Mol Genet Metab 71: 418–435, 2000. doi: 10.1006/mgme.2000.3032. [DOI] [PubMed] [Google Scholar]
- 84.Liu W, Chen J, Ji S, Allen JS, Bayly PV, Wickline SA, Yu X. Harmonic phase MR tagging for direct quantification of Lagrangian strain in rat hearts after myocardial infarction. Magn Reson Med 52: 1282–1290, 2004. doi: 10.1002/mrm.20276. [DOI] [PubMed] [Google Scholar]
- 86.López B, González A, Hermida N, Valencia F, de Teresa E, Díez J. Role of lysyl oxidase in myocardial fibrosis: from basic science to clinical aspects. Am J Physiol Heart Circ Physiol 299: H1–H9, 2010. doi: 10.1152/ajpheart.00335.2010. [DOI] [PubMed] [Google Scholar]
- 87.MacKenna D, Summerour SR, Villarreal FJ. Role of mechanical factors in modulating cardiac fibroblast function and extracellular matrix synthesis. Cardiovasc Res 46: 257–263, 2000. doi: 10.1016/S0008-6363(00)00030-4. [DOI] [PubMed] [Google Scholar]
- 87a.Mallory GK, White PD, Salcedo-Salgar J. The speed of healing of myocardial infarction. Am Heart J 18: 647–671, 1939. doi: 10.1016/S0002-8703(39)90845-8. [DOI] [Google Scholar]
- 88.McKay RG, Pfeffer MA, Pasternak RC, Markis JE, Come PC, Nakao S, Alderman JD, Ferguson JJ, Safian RD, Grossman W. Left ventricular remodeling after myocardial infarction: a corollary to infarct expansion. Circulation 74: 693–702, 1986. doi: 10.1161/01.CIR.74.4.693. [DOI] [PubMed] [Google Scholar]
- 89.Mirsky I, Rankin JS. The effects of geometry, elasticity, and external pressures on the diastolic pressure-volume and stiffness-stress relations. How important is the pericardium? Circ Res 44: 601–611, 1979. doi: 10.1161/01.RES.44.5.601. [DOI] [PubMed] [Google Scholar]
- 90.Mirsky I, Tajimi T, Peterson KL. The development of the entire end-systolic pressure-volume and ejection fraction-afterload relations: a new concept of systolic myocardial stiffness. Circulation 76: 343–356, 1987. doi: 10.1161/01.CIR.76.2.343. [DOI] [PubMed] [Google Scholar]
- 91.Mitchell GF, Lamas GA, Vaughan DE, Pfeffer MA. Left ventricular remodeling in the year after first anterior myocardial infarction: a quantitative analysis of contractile segment lengths and ventricular shape. J Am Coll Cardiol 19: 1136–1144, 1992. doi: 10.1016/0735-1097(92)90314-D. [DOI] [PubMed] [Google Scholar]
- 92.Moreno R, López-Sendón J, García E, Pérez de Isla L, López de Sá E, Ortega A, Moreno M, Rubio R, Soriano J, Abeytua M, García-Fernández M-A. Primary angioplasty reduces the risk of left ventricular free wall rupture compared with thrombolysis in patients with acute myocardial infarction. J Am Coll Cardiol 39: 598–603, 2002. doi: 10.1016/S0735-1097(01)01796-X. [DOI] [PubMed] [Google Scholar]
- 92a.Moreno R, López de Sá E, López-Sendón JL, García E, Soriano J, Abeytua M, Elízaga J, Botas J, Rubio R, Moreno M, García-Fernández MA, Delcán JL. Frequency of left ventricular free-wall rupture in patients with acute myocardial infarction treated with primary angioplasty. Am J Cardiol 85: 757–760, 2000. doi: 10.1016/S0002-9149(99)00855-3. [DOI] [PubMed] [Google Scholar]
- 93.Morita M, Eckert CE, Matsuzaki K, Noma M, Ryan LP, Burdick JA, Jackson BM, Gorman JH III, Sacks MS, Gorman RC. Modification of infarct material properties limits adverse ventricular remodeling. Ann Thorac Surg 92: 617–624, 2011. doi: 10.1016/j.athoracsur.2011.04.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Okamoto RJ, Moulton MJ, Peterson SJ, Li D, Pasque MK, Guccione JM. Epicardial suction: a new approach to mechanical testing of the passive ventricular wall. J Biomech Eng 122: 479–487, 2000. doi: 10.1115/1.1289625. [DOI] [PubMed] [Google Scholar]
- 95.Omens JH, Miller TR, Covell JW. Relationship between passive tissue strain and collagen uncoiling during healing of infarcted myocardium. Cardiovasc Res 33: 351–358, 1997. doi: 10.1016/S0008-6363(96)00206-4. [DOI] [PubMed] [Google Scholar]
- 96.Osman NF, Kerwin WS, McVeigh ER, Prince JL. Cardiac motion tracking using CINE harmonic phase (HARP) magnetic resonance imaging. Magn Reson Med 42: 1048–1060, 1999. doi:. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Park TH, Nagueh SF, Khoury DS, Kopelen HA, Akrivakis S, Nasser K, Ren G, Frangogiannis NG. Impact of myocardial structure and function postinfarction on diastolic strain measurements: implications for assessment of myocardial viability. Am J Physiol Heart Circ Physiol 290: H724–H731, 2006. doi: 10.1152/ajpheart.00714.2005. [DOI] [PubMed] [Google Scholar]
- 98.Partington SL, Kwong RY, Dorbala S. Multimodality imaging in the assessment of myocardial viability. Heart Fail Rev 16: 381–395, 2011. doi: 10.1007/s10741-010-9201-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Patel SR, Piña IL. From acute decompensated to chronic heart failure. Am J Cardiol 114: 1923–1929, 2014. doi: 10.1016/j.amjcard.2014.09.033. [DOI] [PubMed] [Google Scholar]
- 100.Pauschinger M, Knopf D, Petschauer S, Doerner A, Poller W, Schwimmbeck PL, Kühl U, Schultheiss H-P. Dilated cardiomyopathy is associated with significant changes in collagen type I/III ratio. Circulation 99: 2750–2756, 1999. doi: 10.1161/01.CIR.99.21.2750. [DOI] [PubMed] [Google Scholar]
- 101.Pfeffer JM, Pfeffer MA, Fletcher PJ, Braunwald E. Progressive ventricular remodeling in rat with myocardial infarction. Am J Physiol Heart Circ Physiol 260: H1406–H1414, 1991. [DOI] [PubMed] [Google Scholar]
- 102.Pfeffer MA, Braunwald E, Moyé LA, Basta L, Brown EJ Jr, Cuddy TE, Davis BR, Geltman EM, Goldman S, Flaker GC, Klein M, Lamas GA, Packer M, Rouleau J, Rouleau JL, Rutherford J, Wertheimer JH, Hawkins CM; The SAVE Investigators . Effect of captopril on mortality and morbidity in patients with left ventricular dysfunction after myocardial infarction. Results of the survival and ventricular enlargement trial. N Engl J Med 327: 669–677, 1992. doi: 10.1056/NEJM199209033271001. [DOI] [PubMed] [Google Scholar]
- 103.Pfeffer MA, Braunwald E. Ventricular remodeling after myocardial infarction. Experimental observations and clinical implications. Circulation 81: 1161–1172, 1990. doi: 10.1161/01.CIR.81.4.1161. [DOI] [PubMed] [Google Scholar]
- 103a.Popović ZB, Benejam C, Bian J, Mal N, Drinko J, Lee K, Forudi F, Reeg R, Greenberg NL, Thomas JD, Penn MS. Speckle-tracking echocardiography correctly identifies segmental left ventricular dysfunction induced by scarring in a rat model of myocardial infarction. Am J Physiol Heart Circ Physiol 292: H2809–H2816, 2007. doi: 10.1152/ajpheart.01176.2006. [DOI] [PubMed] [Google Scholar]
- 104.Raghupathy R, Witzenburg C, Lake SP, Sander EA, Barocas VH. Identification of regional mechanical anisotropy in soft tissue analogs. J Biomech Eng 133: 091011, 2011. doi: 10.1115/1.4005170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Raya TE, Gay RG, Lancaster L, Aguirre M, Moffett C, Goldman S. Serial changes in left ventricular relaxation and chamber stiffness after large myocardial infarction in rats. Circulation 77: 1424–1431, 1988. doi: 10.1161/01.CIR.77.6.1424. [DOI] [PubMed] [Google Scholar]
- 106.Reimer KA, Lowe JE, Rasmussen MM, Jennings RB. The wavefront phenomenon of ischemic cell death. 1. Myocardial infarct size vs duration of coronary occlusion in dogs. Circulation 56: 786–794, 1977. doi: 10.1161/01.CIR.56.5.786. [DOI] [PubMed] [Google Scholar]
- 107.Romson JL, Hook BG, Kunkel SL, Abrams GD, Schork MA, Lucchesi BR. Reduction of the extent of ischemic myocardial injury by neutrophil depletion in the dog. Circulation 67: 1016–1023, 1983. doi: 10.1161/01.CIR.67.5.1016. [DOI] [PubMed] [Google Scholar]
- 108.Ross AJ, Yang Z, Berr SS, Gilson WD, Petersen WC, Oshinski JN, French BA. Serial MRI evaluation of cardiac structure and function in mice after reperfused myocardial infarction. Magn Reson Med 47: 1158–1168, 2002. doi: 10.1002/mrm.10166. [DOI] [PubMed] [Google Scholar]
- 109.Rouillard AD, Holmes JW. Mechanical regulation of fibroblast migration and collagen remodelling in healing myocardial infarcts. J Physiol 590: 4585–4602, 2012. doi: 10.1113/jphysiol.2012.229484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Rouillard AD, Holmes JW. Coupled agent-based and finite-element models for predicting scar structure following myocardial infarction. Prog Biophys Mol Biol 115: 235–243, 2014. doi: 10.1016/j.pbiomolbio.2014.06.010. [DOI] [PubMed] [Google Scholar]
- 111.Saeed M, Martin AJ, Saloner D, Do L, Wilson M. Noninvasive MR characterization of structural and functional components of reperfused infarct. Acta Radiol 51: 1093–1102, 2010. doi: 10.3109/02841851.2010.520025. [DOI] [PubMed] [Google Scholar]
- 112.Sakamoto H, Parish LM, Hamamoto H, Ryan LP, Eperjesi TJ, Plappert TJ, Jackson BM, St John-Sutton MG, Gorman JH III, Gorman RC. Effect of reperfusion on left ventricular regional remodeling strains after myocardial infarction. Ann Thorac Surg 84: 1528–1536, 2007. doi: 10.1016/j.athoracsur.2007.05.060. [DOI] [PubMed] [Google Scholar]
- 113.Schuleri KH, Centola M, Evers KS, Zviman A, Evers R, Lima JA, Lardo AC. Cardiovascular magnetic resonance characterization of peri-infarct zone remodeling following myocardial infarction. J Cardiovasc Magn Reson 14: 24, 2012. doi: 10.1186/1532-429X-14-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Sequeira V, Nijenkamp L, Regan J. The physiological role of cardiac cytoskeleton and its alterations in heart failure. Biochim Biophys Acta 1838: 700–722, 2014. 10.1016/j.bbamem.2013.07.011. [DOI] [PubMed] [Google Scholar]
- 115.Smith WB, Noack L, Khew-goodall Y, Isenmann S, Vadasr MA, Gamblep JR. Transforming growth factor-βl inhibits the production of IL–8 and the transmigration of neutrophils through activated endothelium. J Immunol 157: 360–368, 1996. [PubMed] [Google Scholar]
- 116.Soleimanifard S, Abd-Elmoniem KZ, Sasano T, Agarwal HK, Abraham MR, Abraham TP, Prince JL. Three-dimensional regional strain analysis in porcine myocardial infarction: a 3T magnetic resonance tagging study. J Cardiovasc Magn Reson 14: 85, 2012. doi: 10.1186/1532-429X-14-85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Stewart S, MacIntyre K, Hole DJ, Capewell S, McMurray JJV. More ‘malignant’ than cancer? Five-year survival following a first admission for heart failure. Eur J Heart Fail 3: 315–322, 2001. doi: 10.1016/S1388-9842(00)00141-0. [DOI] [PubMed] [Google Scholar]
- 118.Sun M, Dawood F, Wen W-H, Chen M, Dixon I, Kirshenbaum LA, Liu PP. Excessive tumor necrosis factor activation after infarction contributes to susceptibility of myocardial rupture and left ventricular dysfunction. Circulation 110: 3221–3228, 2004. doi: 10.1161/01.CIR.0000147233.10318.23. [DOI] [PubMed] [Google Scholar]
- 119.Sun Y, Weber KT. Infarct scar: a dynamic tissue. Cardiovasc Res 46: 250–256, 2000. doi: 10.1016/S0008-6363(00)00032-8. [DOI] [PubMed] [Google Scholar]
- 120.Sutton MGSJ, Sharpe N. Left ventricular remodeling after myocardial infarction: pathophysiology and therapy. Circulation 101: 2981–2988, 2000. doi: 10.1161/01.CIR.101.25.2981. [DOI] [PubMed] [Google Scholar]
- 121.Takahashi T, Levine MJ, Grossman W. Regional diastolic mechanics of ischemic and nonischemic myocardium in the pig heart. J Am Coll Cardiol 17: 1203–1212, 1991. doi: 10.1016/0735-1097(91)90855-4. [DOI] [PubMed] [Google Scholar]
- 122.Tao Z-Y, Cavasin MA, Yang F, Liu Y-H, Yang X-P. Temporal changes in matrix metalloproteinase expression and inflammatory response associated with cardiac rupture after myocardial infarction in mice. Life Sci 74: 1561–1572, 2004. doi: 10.1016/j.lfs.2003.09.042. [DOI] [PubMed] [Google Scholar]
- 123.Theroux P, Ross J Jr, Franklin D, Covell JW, Bloor CM, Sasayama S. Regional myocardial function and dimensions early and late after myocardial infarction in the unanesthetized dog. Circ Res 40: 158–165, 1977. doi: 10.1161/01.RES.40.2.158. [DOI] [PubMed] [Google Scholar]
- 124.Thorstensen A, Amundsen BH, Dalen H, Hala P, Kiss G, Aase SA, Torp H, Støylen A. Strain rate imaging combined with wall motion analysis gives incremental value in direct quantification of myocardial infarct size. Eur Heart J Cardiovasc Imaging 13: 914–921, 2012. doi: 10.1093/ehjci/jes070. [DOI] [PubMed] [Google Scholar]
- 125.Thorstensen A, Dalen H, Hala P, Kiss G, D’hooge J, Torp H, Støylen A, Amundsen B. Three-dimensional echocardiography in the evaluation of global and regional function in patients with recent myocardial infarction: a comparison with magnetic resonance imaging. Echocardiography 30: 682–692, 2013. doi: 10.1111/echo.12115. [DOI] [PubMed] [Google Scholar]
- 126.Thygesen K, Alpert JS, Jaffe AS, Simoons ML, Chaitman BR, White HD, Thygesen K, Alpert JS, White HD, Jaffe AS, Katus HA, Apple FS, Lindahl B, Morrow DA, Chaitman BR, Clemmensen PM, Johanson P, Hod H, Underwood R, Bax JJ, Bonow JJ, Pinto F, Gibbons RJ, Fox KA, Atar D, Newby LK, Galvani M, Hamm CW, Uretsky BF, Steg PG, Wijns W, Bassand JP, Menasche P, Ravkilde J, Ohman EM, Antman EM, Wallentin LC, Armstrong PW, Simoons ML, Januzzi JL, Nieminen MS, Gheorghiade M, Filippatos G, Luepker RV, Fortmann SP, Rosamond WD, Levy D, Wood D, Smith SC, Hu D, Lopez-Sendon JL, Robertson RM, Weaver D, Tendera M, Bove AA, Parkhomenko AN, Vasilieva EJ, Mendis S, Bax JJ, Baumgartner H, Ceconi C, Dean V, Deaton C, Fagard R, Funck-Brentano C, Hasdai D, Hoes A, Kirchhof P, Knuuti J, Kolh P, McDonagh T, Moulin C, Popescu BA, Reiner Z, Sechtem U, Sirnes PA, Tendera M, Torbicki A, Vahanian A, Windecker S, Morais J, Aguiar C, Almahmeed W, Arnar DO, Barili F, Bloch KD, Bolger AF, Botker HE, Bozkurt B, Bugiardini R, Cannon C, de Lemos J, Eberli FR, Escobar E, Hlatky M, James S, Kern KB, Moliterno DJ, Mueller C, Neskovic AN, Pieske BM, Schulman SP, Storey RF, Taubert KA, Vranckx P, Wagner DR; Joint ESC/ACCF/AHA/WHF Task Force for Universal Definition of Myocardial Infarction; Authors/Task Force Members Chairpersons; Biomarker Subcommittee; ECG Subcommittee; Imaging Subcommittee; Classification Subcommittee; Intervention Subcommittee; Trials & Registries Subcommittee; Trials & Registries Subcommittee; Trials & Registries Subcommittee; Trials & Registries Subcommittee; ESC Committee for Practice Guidelines (CPG); Document Reviewers . Third universal definition of myocardial infarction. J Am Coll Cardiol 60: 1581–1598, 2012. doi: 10.1016/j.jacc.2012.08.001. [DOI] [PubMed] [Google Scholar]
- 127.Urheim S, Edvardsen T, Torp H, Angelsen B, Smiseth OA. Myocardial strain by Doppler echocardiography. Validation of a new method to quantify regional myocardial function. Circulation 102: 1158–1164, 2000. doi: 10.1161/01.CIR.102.10.1158. [DOI] [PubMed] [Google Scholar]
- 128.Walker JC, Ratcliffe MB, Zhang P, Wallace AW, Fata B, Hsu EW, Saloner D, Guccione JM. MRI-based finite-element analysis of left ventricular aneurysm. Am J Physiol Heart Circ Physiol 289: H692–H700, 2005. doi: 10.1152/ajpheart.01226.2004. [DOI] [PubMed] [Google Scholar]
- 129.Wall ST, Walker JC, Healy KE, Ratcliffe MB, Guccione JM. Theoretical impact of the injection of material into the myocardium: a finite element model simulation. Circulation 114: 2627–2635, 2006. doi: 10.1161/CIRCULATIONAHA.106.657270. [DOI] [PubMed] [Google Scholar]
- 130.Wang VY, Lam HI, Ennis DB, Cowan BR, Young AA, Nash MP. Modelling passive diastolic mechanics with quantitative MRI of cardiac structure and function. Med Image Anal 13: 773–784, 2009. doi: 10.1016/j.media.2009.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Weber KT, Sun Y, Katwa LC. Wound healing following myocardial infarction [Online]. Clin Cardiol 19: 447–455, 1996. doi: 10.1002/clc.4960190602. [DOI] [PubMed] [Google Scholar]
- 132.Weisman HF, Bush DE, Mannisi JA, Bulkley BH. Global cardiac remodeling after acute myocardial infarction: a study in the rat model. J Am Coll Cardiol 5: 1355–1362, 1985. doi: 10.1016/S0735-1097(85)80348-X. [DOI] [PubMed] [Google Scholar]
- 133.Weisman HF, Bush DE, Mannisi JA, Weisfeldt ML, Healy B. Cellular mechanisms of myocardial infarct expansion. Circulation 78: 186–201, 1988. doi: 10.1161/01.CIR.78.1.186. [DOI] [PubMed] [Google Scholar]
- 134.Whittaker P, Boughner DR, Kloner RA. Role of collagen in acute myocardial infarct expansion. Circulation 84: 2123–2134, 1991. doi: 10.1161/01.CIR.84.5.2123. [DOI] [PubMed] [Google Scholar]
- 135.Wong EY, O’Donnell M, Thiele K, Compas CB, Huang X, Sampath S, Lin B, Pal P, Papademetris X, Dione D, Staib L, Sinusas AJ, Duncan JS. 4-D echocardiography assessment of local myocardial strain using 3-D speckle tracking combined with shape tracking. IEEE Int Ultrason Symp July 2013. doi: 10.1109/ULTSYM.2013.0026. [DOI] [Google Scholar]
- 136.Yang Z, Zingarelli B, Szabó C. Crucial role of endogenous interleukin-10 production in myocardial ischemia/reperfusion injury. Circulation 101: 1019–1026, 2000. doi: 10.1161/01.CIR.101.9.1019. [DOI] [PubMed] [Google Scholar]
- 137.Yankey GK, Li T, Kilic A, Cheng G, Satpute A, Savai K, Li S, Moainie SL, Prastein D, DeFillipi C, Wu ZJ, Griffith BP. Regional remodeling strain and its association with myocardial apoptosis after myocardial infarction in an ovine model. J Thorac Cardiovasc Surg 135: 991–998, 2008. doi: 10.1016/j.jtcvs.2007.12.021. [DOI] [PubMed] [Google Scholar]
- 138.Yeon SB, Reichek N, Tallant BA, Lima JA, Calhoun LP, Clark NR, Hoffman EA, Ho KK, Axel L. Validation of in vivo myocardial strain measurement by magnetic resonance tagging with sonomicrometry. J Am Coll Cardiol 38: 555–561, 2001. doi: 10.1016/S0735-1097(01)01397-3. [DOI] [PubMed] [Google Scholar]
- 139.Yin FC, Strumpf RK, Chew PH, Zeger SL. Quantification of the mechanical properties of noncontracting canine myocardium under simultaneous biaxial loading. J Biomech 20: 577–589, 1987. doi: 10.1016/0021-9290(87)90279-X. [DOI] [PubMed] [Google Scholar]
- 140.Young AA, French BA, Yang Z, Cowan BR, Gilson WD, Berr SS, Kramer CM, Epstein FH. Reperfused myocardial infarction in mice: 3D mapping of late gadolinium enhancement and strain. J Cardiovasc Magn Reson 8: 685–692, 2006. doi: 10.1080/10976640600721767. [DOI] [PubMed] [Google Scholar]
- 141.Zhang Y, Chan AKY, Yu C-M, Yip GWK, Fung JWH, Lam WWM, So NMC, Wang M, Wu EB, Wong JT, Sanderson JE. Strain rate imaging differentiates transmural from non-transmural myocardial infarction: a validation study using delayed-enhancement magnetic resonance imaging. J Am Coll Cardiol 46: 864–871, 2005. doi: 10.1016/j.jacc.2005.05.054. [DOI] [PubMed] [Google Scholar]
- 142.Zimmerman SD, Criscione J, Covell JW. Remodeling in myocardium adjacent to an infarction in the pig left ventricle. Am J Physiol Heart Circ Physiol 287: H2697–H2704, 2004. doi: 10.1152/ajpheart.00160.2004. [DOI] [PubMed] [Google Scholar]