Abstract
Malignant peripheral nerve sheath tumor (MPNST) in the thorax is an extremely rare disease, and half of all cases of MPNST are associated with neurofibromatosis type I. Sporadic intrathoracic MPNST is difficult to diagnose and treat. Because of the rarity of intrathoracic MPNST, the optimal method of diagnosis and the efficacy of chemotherapy are unknown. Herein, we present a case of inoperable mediastinal MPNST, in which the diagnosis was immunohistochemically made by the loss of H3K27me3 expression in a transbronchial needle biopsy specimen. The patient showed a good response to doxorubicin plus ifosfamide chemotherapy. The present case highlights that MPNST should be included in the differential diagnosis of non‐posterior mediastinum thoracic lesions, and that appropriate diagnosis and treatment for intrathoracic MPNST should be considered in patients with a thoracic mass.
Keywords: Chemotherapy, doxorubicin, ifosfamide, mediastinal tumor
Introduction
Malignant peripheral nerve sheath tumors (MPNST), also called malignant schwannomas or neurofibrosarcomas, account for approximately 5–10% of all soft tissue sarcomas, and 50% of MPNST cases are associated with neurofibromatosis type I (NF‐1).1, 2, 3 Although MPNST commonly develops in the extremities, head, and neck, intrathoracic MPNST is extremely rare.2, 3, 4, 5, 6, 7 Most benign neurogenic tumors in the thorax develop in the posterior mediastinum, but MPNST has been reported to arise in various thoracic spaces, including the non‐posterior mediastinum and chest wall, as well as the posterior mediastinum.4, 5, 6, 7, 8 Because of the rarity of intrathoracic MPNST, the optimal method of diagnosis and the efficacy of chemotherapy for advanced intrathoracic MPNST are unknown.9, 10, 11, 12
We encountered a case of locally advanced inoperable MPNST mainly involving the middle mediastinum. The patient was treated with doxorubicin plus ifosfamide chemotherapy, and a partial response was obtained. Herein, we describe a rare case of intrathoracic MPNST focusing on the diagnosis and chemotherapy, along with a review of the relevant literature.
Case report
A 64‐year‐old woman was referred to our hospital because of a gradually progressing cough and abnormality on chest radiography. Chest radiography (Fig 1a) and computed tomography (CT) (Fig 2a) revealed a large middle mediastinal mass measuring 100 mm on the right side, compressing the trachea. Bronchoscopic examination was performed, and histological findings by endobronchial ultrasound‐guided transbronchial needle aspiration revealed oval to spindle‐shaped cells with hyperchromatic and pleomorphic nuclei arranged in dense cellular fascicles (Fig 3). Immunohistochemical analysis showed that the tumor cells were negative for AE1/AE3, S‐100 protein, α‐smooth muscle actin, desmin, vimentin, myogenin, STAT6, p40, and TTF‐1. In addition, Ki‐67 showed 30–40% positivity and loss of H3K27me3 (rabbit monoclonal C36B11, Cell Signaling Technology, Ltd., Danvers, MA, USA) expression. These findings confirmed a diagnosis of MPNST, although S‐100 immunostaining was negative.13 Positron emission tomography with fluorodeoxyglucose‐computed tomography (FDG‐PET/CT) revealed positive accumulation of FDG in the mediastinal mass (maximum standardized uptake value 16.1), but other organs were negative. As the mediastinal tumor was considered to be locally advanced and unresectable, the patient was treated with chemotherapy containing doxorubicin and ifosfamide (AI therapy: a total of 5 mg/m2 of ifosfamide and 60 mg/m2 doxorubicin were administered intravenously on days 1–2, and 40 mg of dexamethasone on days 1–3). A partial response was achieved after four cycles of AI therapy and in total six cycles of AI therapy were performed. Chest radiograph and CT results after chemotherapy are shown in Figures 1b and 2b, respectively. The tumor size was remarkably reduced. The major adverse effect of the chemotherapy was grade 4 neutropenia. Although febrile neutropenia was observed during the first cycle of AI chemotherapy, it was well controlled by the administration of G‐CSF and antibiotics. However, the patient presented with progressive disease two months after the cessation of chemotherapy. A total of 60 Gy of thoracic radiotherapy was performed and the disease remained stable for three months after the radiotherapy.
Figure 1.
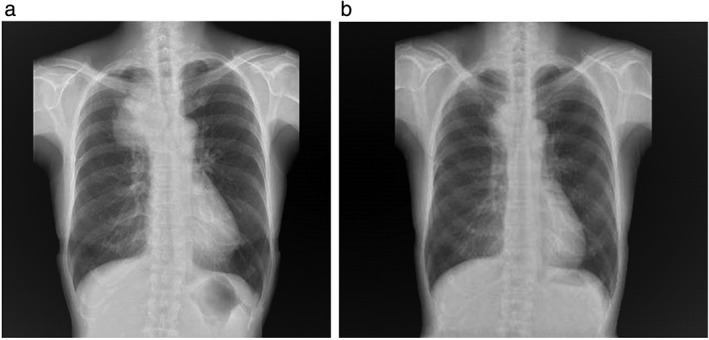
Chest radiography (a) before and (b) after six cycles of doxorubicin and ifosfamide chemotherapy.
Figure 2.
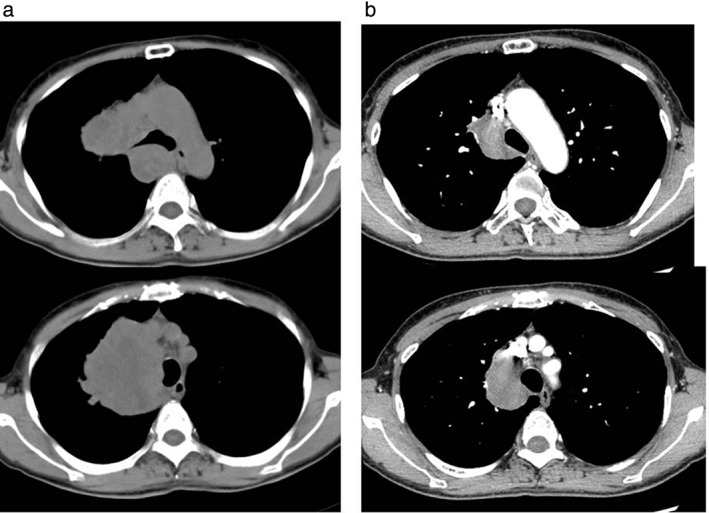
Chest computed tomography (a) before and (b) after six cycles of doxorubicin and ifosfamide chemotherapy.
Figure 3.
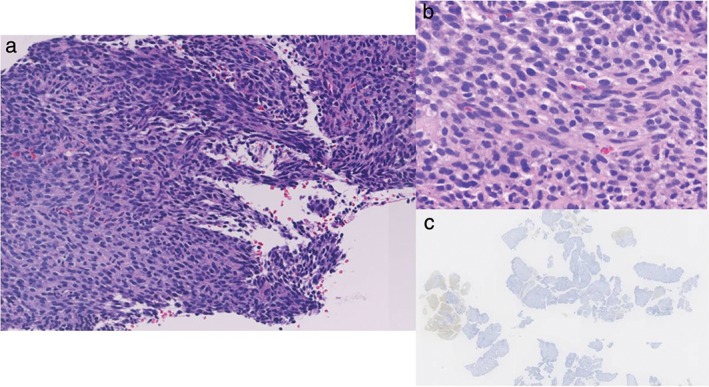
Histological findings by endobronchial ultrasound‐guided transbronchial needle aspiration revealed oval to spindle‐shaped cells with hyperchromatic and pleomorphic nuclei arranged in dense cellular fascicles (a ×40, b ×100). (c) There was a loss of H3K27me3 (rabbit monoclonal C36B11) expression.
Discussion
We present a case of advanced intrathoracic MPNST located in the non‐posterior mediastinum. In general, neurogenic tumors develop mainly in the posterior mediastinum.4 However, MPNST primarily located in the pulmonary parenchyma may be pleural‐based, hilar, or closely associated with large bronchovascular bundles. Thus, intrathoracic MPNST can involve various sites, including the anterior or middle mediastinum and chest wall.4, 5, 6, 7, 8 As such, intrathoracic MPNST should be included as a differential diagnosis of aggressive masses in the mediastinum, especially in a sporadic setting.
Sporadic intrathoracic MPNST may be quite difficult to diagnosis because of its rarity and diverse morphologic features. Loss of H3K27me3 expression is considered an important diagnostic marker for MPNST, especially in differential diagnosis with neurofibroma. Loss of H3K27me3 expression is not always a specific marker for MPNST, but is related to poorer survival in patients with MPNST.13 A combination of S‐100 and cytokeratin staining with smooth muscle antigen is also useful for differential diagnosis for MPNST.1, 2, 3, 4, 5, 6 However, examination of H3K27me3 immunohistochemistry can help with the diagnosis and prognosis of MPNST.13
The patient in our case was treated with AI chemotherapy and showed a partial response. Kroep et al. summarized the data of 12 pooled clinical trials of first‐line chemotherapy for soft tissue sarcoma and reported that MPNST showed similar response (21%) and progression‐free survival (17 weeks) rates to chemotherapy compared to other soft tissue sarcomas (22% and 16 weeks, respectively).9 Although not statistically significant, AI therapy tended to show the best response and progression‐free survival rates in these studies. Indeed, our patient exhibited a good response to AI therapy. Thus, AI therapy is one of the active chemotherapy regimens available to treat this disease at present.
Surgery with wide margins is considered the only procedure to improve the prognosis of MPNSTs; however, previous studies have reported that intrathoracic MPNSTs are larger than when they occur at other sites, and spread with invasion or encasement into adjacent mediastinal structures.4, 5, 6, 7, 8 Thus, it is speculated that non‐surgically treated or inoperable subjects may be included among cases of intrathoracic MPNST, as in the present case.
Several case reports have demonstrated the efficacy of neoadjuvant chemotherapy followed by surgery for advanced MPNST.10, 11, 12 However, no information is available regarding the efficacy of neoadjuvant chemotherapy for advanced intrathoracic MPNST. The resectability of the remaining tumor after chemotherapy may be an important issue in patients with locally advanced intrathoracic MPNST. Unfortunately, the residual tumor after chemotherapy in the present case remained inoperable because of the involvement of large vessels. Further clinical experience and data regarding therapeutic outcomes of intrathoracic MPNST are required.
In conclusion, we describe a case of sporadic intrathoracic MPNST mainly involving the middle mediastinum that responded to ifosfamide plus doxorubicin chemotherapy. Sporadic intrathoracic MPNSTs are extremely rare in clinical practice. MPNSTs should be considered in the differential diagnosis of a large, elongated intrathoracic mass. Clinicians should be aware of this disease entity, and the accumulation of additional therapeutic experience is necessary.
Disclosure
No authors report any conflict of interest.
References
- 1. Ducatman BS, Scheithauer BW, Piepgras DG, Reiman HM, Ilstrup DM. Malignant peripheral nerve sheath tumors. A clinicopathologic study of 120 cases. Cancer 1986; 57: 2006–21. [DOI] [PubMed] [Google Scholar]
- 2. King AA, Debaun MR, Riccardi VM, Gutmann DH. Malignant peripheral nerve sheath tumors in neurofibromatosis 1. Am J Med Genet 2000; 93: 388–92. [PubMed] [Google Scholar]
- 3. Zou C, Smith KD, Liu J et al Clinical, pathological, and molecular variables predictive of malignant peripheral nerve sheath tumor outcome. Ann Surg 2009; 249: 1014–22. [DOI] [PubMed] [Google Scholar]
- 4. Boland JM, Colby TV, Folpe AL. Intrathoracic peripheral nerve sheath tumors‐a clinicopathological study of 75 cases. Hum Pathol 2015; 46: 419–25. [DOI] [PubMed] [Google Scholar]
- 5. Chao BH, Stogner‐Underwood KA, Kiev J, Smith TJ. Intrathoracic malignant peripheral nerve sheath tumor in neurofibromatosis 1. J Clin Oncol 2008; 26: 2216–8. [DOI] [PubMed] [Google Scholar]
- 6. Ralli M, Singh S, Hasija S, Verma R. Intrathoracic malignant peripheral nerve sheath tumor: Histopathological and immunohistochemical features. Iran J Pathol 2015; 10: 74–8. [PMC free article] [PubMed] [Google Scholar]
- 7. Kalra B, Kingsley PA, Bedi HS, Kwatra KS, Negi P. Malignant peripheral nerve sheath tumor of the anterior mediastinum: A rare presentation. Rare Tumors 2014; 6: 5528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Kamran SC, Shinagare AB, Howard SA et al Intrathoracic malignant peripheral nerve sheath tumors: Imaging features and implications for management. Radiol Oncol 2013; 47: 230–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Kroep JR, Ouali M, Gelderblom H et al First‐line chemotherapy for malignant peripheral nerve sheath tumor (MPNST) versus other histological soft tissue sarcoma subtypes and as a prognostic factor for MPNST: An EORTC soft tissue and bone sarcoma group study. Ann Oncol 2011; 22: 207–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Moretti VM, Crawford EA, Staddon AP, Lackman RD, Ogilvie CM. Early outcomes for malignant peripheral nerve sheath tumor treated with chemotherapy. Am J Clin Oncol 2011; 34: 417–21. [DOI] [PubMed] [Google Scholar]
- 11. Minagawa T, Shioya R, Sato C et al Advanced epithelioid malignant peripheral nerve sheath tumor showing complete response to combined surgery and chemotherapy: A case report. Case Rep Oncol Med 2011; 2011: 705345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Masui F, Yokoyama R, Soshi S, Beppu Y, Asanuma K, Fujii K. A malignant peripheral nerve‐sheath tumour responding to chemotherapy. J Bone Joint Surg Br 2004; 86: 113–5. [PubMed] [Google Scholar]
- 13. Cleven AH, Sannaa GA, Briaire‐de Bruijn I et al Loss of H3K27 tri‐methylation is a diagnostic marker for malignant peripheral nerve sheath tumors and an indicator for an inferior survival. Mod Pathol 2016; 29: 582–90. [DOI] [PMC free article] [PubMed] [Google Scholar]


