Abstract
Objective:
Little is known regarding patterns of alcohol use and alcohol-related care among transgender adults. This study examined alcohol use and alcohol-related care across transgender status in a probability sample of U.S. adults.
Method:
We conducted secondary analyses of the 2014 Behavioral Risk Factor Surveillance System survey, focusing on adults in eight states that administered both an Alcohol Screening and Brief Intervention module and a Gender Identity module (n = 58,381). Measurements included transgender status, sociodemographic characteristics, alcohol consumption (any alcohol use, risky drinking, heavy episodic drinking, and any unhealthy alcohol use), and alcohol-related care (alcohol screening during healthcare visits and advice about unhealthy alcohol use). We tested the association between transgender status and alcohol consumption and alcohol-related care using multivariable logistic regression models adjusted for sociodemographic characteristics.
Results:
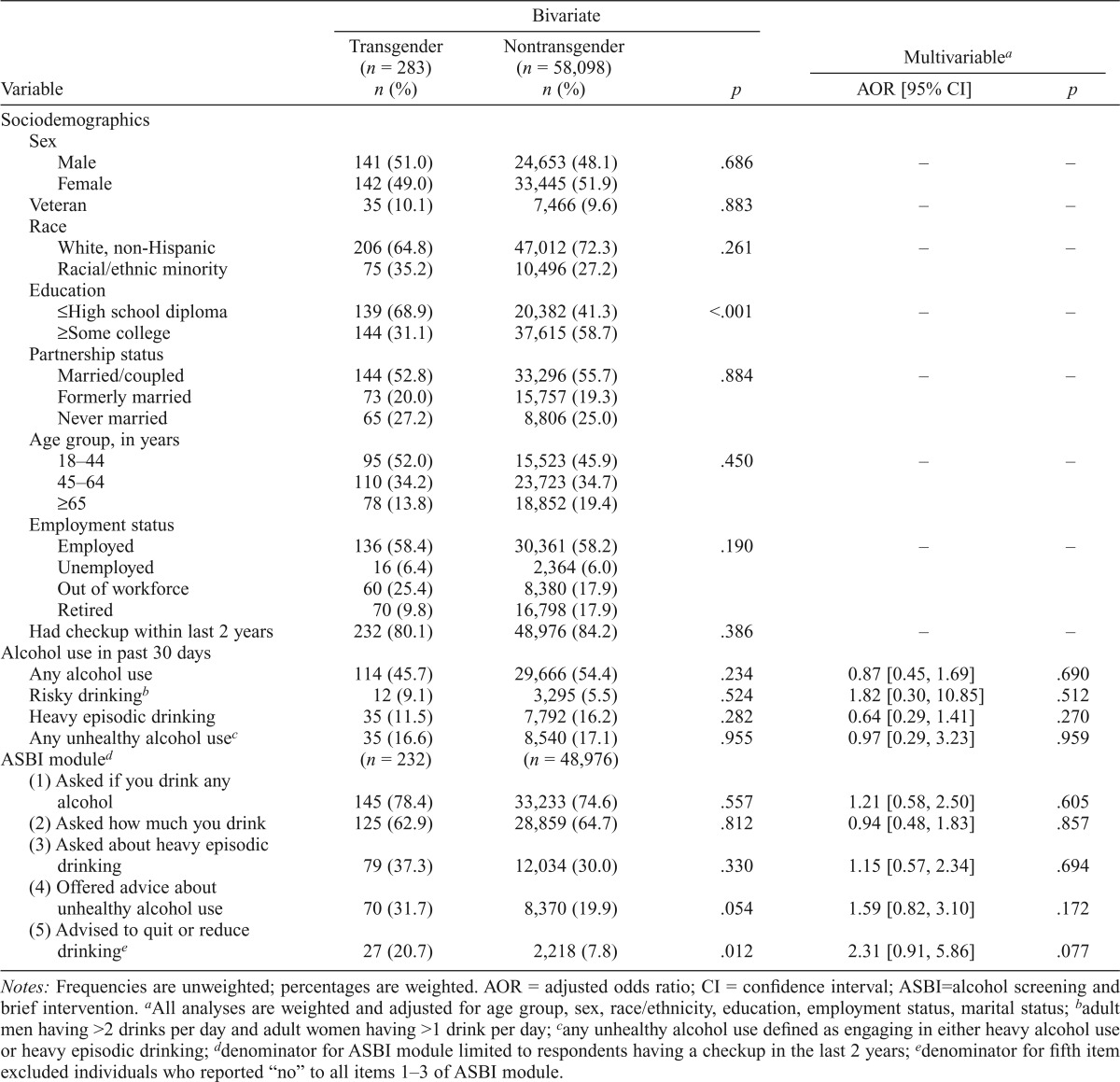
Approximately 0.6% of respondents (n = 283) self-identified as transgender. Overall, there were no significant differences in alcohol consumption or screening between transgender and nontransgender adults. A greater proportion of transgender than nontransgender adults reported being advised to reduce alcohol use (20.7% vs. 7.8%, p = .012). However, this difference was not significant after adjusting for other sociodemographic characteristics (adjusted odds ratio = 2.31, 95% CI [0.91, 5.86], p = .077).
Conclusions:
In this representative sample from eight U.S. states, we did not find differences related to transgender status in rates of alcohol use or of alcohol-related care.
Lesbian, gay, bisexual, and transgender (LGBT) populations experience many health and health care disparities, and transgender individuals may be particularly vulnerable to disparities (Institute of Medicine, 2011). The term transgender refers broadly to individuals whose sex assigned at birth is inconsistent with their core gender identity. Because transgender identities transcend the social construction of gender as a culturally strict and biologically static binary of either masculine or feminine, transgender individuals often endure prejudice and discrimination (Blosnich et al., 2016; Grant et al., 2010; Stotzer, 2009), which may elevate stress and other negative emotions (e.g., anxiety) and the potential for maladaptive coping behaviors, such as unhealthy alcohol use (Kuntsche et al., 2006).
It is unclear whether transgender individuals have different patterns of alcohol use than their nontransgender peers. Previous research suggests high rates of alcohol use among transgender populations (Benotsch et al., 2016; Brown and Jones, 2016; Coulter et al., 2015; Garofalo et al., 2006; Melendez et al., 2006; Santos et al., 2014), but these studies either used non-probability-based sampling methods that limit generalizability or often did not compare transgender with nontransgender individuals.
Among populations receiving primary care, alcohol screening and brief intervention for unhealthy alcohol use are recommended (Jonas et al., 2012; Kaner et al., 2007; National Institute on Alcohol Abuse and Alcoholism [NIAAA], 2007), but no population-level study has described alcohol-related care for transgender populations. However, in a convenience-based sample of transgender women, nearly 60% reported alcohol use in the past 6 months, but less than 20% reported access to alcohol treatment (Santos et al., 2014). Because transgender persons may have medically complicated, competing health care needs (Brown & Jones, 2016), transgender patients with unhealthy alcohol use may be less likely than nontransgender patients to receive alcohol-related care. On the other hand, because transgender persons have high rates of suicide risk (Blosnich et al., 2013, 2014), screening and intervention for unhealthy alcohol use may be more routine due to associations between alcohol use and suicide (Borges & Loera, 2010; Wilcox et al., 2004).
This brief report sought to examine patterns of alcohol use and alcohol-related care by transgender status in a probability-based sample of adults. Specifically, differences between transgender and nontransgender adults were examined on alcohol use measures, alcohol screening during routine checkup, and advice about recommended drinking limits or to reduce use (i.e., brief intervention).
Method
Data source and study sample
Data for this secondary analysis are from the 2014 Behavioral Risk Factor Surveillance System (BRFSS) conducted by the Centers for Disease Control and Prevention (CDC), which uses nationally representative samples of non-institutionalized adults in all U.S. states and territories. The BRFSS includes landline and mobile phone computer-assisted telephone interviews. All states and territories administer a standard core BRFSS questionnaire, and they can elect to use optional survey modules created by the CDC. Among the modules available with the 2014 BRFSS were the Alcohol Screening and Brief Intervention (ASBI) and the Sexual Orientation and Gender Identity (SOGI) modules. In 2014, 20 states/territories used the SOGI module and 19 states used the ASBI module. Eight states administered both optional modules: Hawaii, Indiana, Kansas, Kentucky, Minnesota, Montana, New York, and Wisconsin. Response rates ranged from 33.0% (New York) to 59.2% (Kentucky). Because we focused on unhealthy alcohol use among transgender individuals, our analytic sample included individuals in the eight states who answered both the gender identity item in the SOGI module and the ASBI module items (n = 58,381). Detailed information about BRFSS methodology and survey items is available from the CDC (2015a, 2015b).
Among states that administered the ASBI module, there were no differences in the four alcohol use measures based on whether those states did or did not use the SOGI module (p = .088–.771; data not shown). In addition, the prevalence of transgender respondents did not differ among SOGI states that did and did not administer the ASBI module (p = .665; data not shown).
Measures
Transgender status.
In the SOGI module, respondents were asked, “Do you consider yourself to be transgender?” If respondents said yes, they were asked if they considered themselves male-to-female (n = 138 [0.3% weighted percent]), female-to-male (n = 94 [0.2%]), or gender nonconforming (n = 51 [0.1%]). Because of small samples across the individual categories of transgender identities, we dichotomized the variable to be transgender (i.e., any transgender identity) versus nontransgender. Respondents who indicated “don’t know” (n = 363) or refused to answer (n = 520) were excluded from analyses.
Alcohol use.
Consistent with previous studies (Chavez et al., 2015; Chew et al., 2005), four measures of alcohol use were derived based on responses to the alcohol use measures included in the BRFSS core survey. Any alcohol use was measured based on report of more than one drink in the past 30 days on the following question: “During the past 30 days, how many days per week or per month did you have at least one drink of any alcoholic beverage such as beer, wine, a malt beverage or liquor?” Risky drinking was defined based on report of exceeding weekly recommended limits (14 drinks per week for men, 7 drinks per week for women) defined by the NIAAA based on report of drinking on average more than two drinks per day for men or more than one per day for women in the past 30 days (NIAAA, 2007). Heavy episodic drinking was measured based on report of five or more drinks for men or four or more drinks for women on a single occasion in the last 30 days. Finally, we created a summary measure of any unhealthy alcohol use defined as any respondent who met criteria for either heavy alcohol use or heavy episodic drinking in the last 30 days (Saitz, 2005).
Alcohol-related care.
The ASBI module included five measures of alcohol-related care in relation to their last checkup. Specifically, respondents were asked, “Were you asked in person or on a form if you drink alcohol,” “did the health care provider ask you in person or on a form how much you drink,” “did the healthcare provider specifically ask whether you drank [5 for men /4 for women] or more alcoholic drinks on an occasion,” and “were you offered advice about what level of drinking is harmful or risky for your health?” Only respondents who answered “yes” to any of the first three items were administered the fifth item, “Were you advised to reduce or quit your drinking?” The response options for each of the five questions were yes/no. The first three questions reflected receipt of alcohol screening, whereas the latter two items assessed components of brief intervention that were commonly offered as part of brief alcohol counseling interventions tested in randomized controlled trials (Kaner et al., 2007).
Sociodemographic characteristics.
Sociodemographic characteristics were race (coded as White vs. racial/ethnic minority because of the small sample size); education (high school diploma or less vs. some college or greater); partnership status (married/coupled, formerly married, or never married); age group (18–44, 45-64, ≥65); veteran status; and employment status (employed, unemployed, out of workforce [included student, homemaker, unable to work], or retired). Respondent’s sex was based on documentation by the interviewer and, because interviewers were given instructions to “ask only if necessary,” it could be determined without asking the respondent (Conron et al., 2012).
Analyses
We used survey-adjusted Wald tests to compare sociodemographic characteristics and alcohol use and care patterns between transgender and nontransgender persons. We tested the association of transgender status with the alcohol use and ASBI measures using multiple logistic regression models, adjusted for sociodemographic characteristics. Because the ASBI module asked questions about alcohol screening and brief intervention in health care settings, only respondents who indicated having visited a doctor for a routine checkup in the last 2 years were asked the ASBI questions. Therefore, although all other analyses were conducted in the full analytic sample, analyses of alcohol-related care were conducted only among the 49,208 respondents who received the ASBI questions (84.2% of the sample from the eight states). All analyses were conducted in Stata/SE Version 13 (StataCorp LP, College Station, TX) and accounted for stratification, clustering, and weighting of the BRFSS complex survey design to generate population-representative estimates with accurate standard errors. The study was approved by the institutional review board of Veterans Affairs Pittsburgh Healthcare System.
Results
In this sample, 283 (approximately 0.60%, 95% CI [0.43, 0.75]) respondents self-identified as transgender. The only significant difference in sociodemographic characteristics was educational attainment, in which a significantly greater proportion of transgender individuals reported lower educational attainment than their nontransgender peers (Table 1). There were no differences between transgender and nontransgender groups on having a checkup in the last 2 years and thus no differences in whether each group received the ASBI module.
Table 1.
Sociodemographics and alcohol use and alcohol-related care prevalence, by transgender status
| Variable | Bivariate |
Multivariablea |
|||
| Transgender (n = 283) n (%) | Nontransgender (n = 58,098) n (%) | p | AOR [95% CI] | p | |
| Sociodemographics | |||||
| Sex | |||||
| Male | 141 (51.0) | 24,653 (48.1) | .686 | – | – |
| Female | 142 (49.0) | 33,445 (51.9) | |||
| Veteran | 35 (10.1) | 7,466 (9.6) | .883 | – | – |
| Race | |||||
| White, non-Hispanic | 206 (64.8) | 47,012 (72.3) | .261 | – | – |
| Racial/ethnic minority | 75 (35.2) | 10,496 (27.2) | |||
| Education | |||||
| ≤High school diploma | 139 (68.9) | 20,382 (41.3) | <.001 | – | – |
| ≥Some college | 144 (31.1) | 37,615 (58.7) | |||
| Partnership status | |||||
| Married/coupled | 144 (52.8) | 33,296 (55.7) | .884 | – | – |
| Formerly married | 73 (20.0) | 15,757 (19.3) | |||
| Never married | 65 (27.2) | 8,806 (25.0) | |||
| Age group, in years | |||||
| 18–44 | 95 (52.0) | 15,523 (45.9) | .450 | – | – |
| 45–64 | 110 (34.2) | 23,723 (34.7) | |||
| ≥65 | 78 (13.8) | 18,852 (19.4) | |||
| Employment status | |||||
| Employed | 136 (58.4) | 30,361 (58.2) | .190 | – | – |
| Unemployed | 16 (6.4) | 2,364 (6.0) | |||
| Out of workforce | 60 (25.4) | 8,380 (17.9) | |||
| Retired | 70 (9.8) | 16,798 (17.9) | |||
| Had checkup within last 2 years | 232 (80.1) | 48,976 (84.2) | .386 | – | – |
| Alcohol use in past 30 days | |||||
| Any alcohol use | 114(45.7) | 29,666 (54.4) | .234 | 0.87 [0.45, 1.69] | .690 |
| Risky drinkingb | 12 (9.1) | 3,295 (5.5) | .524 | 1.82 [0.30, 10.85] | .512 |
| Heavy episodic drinking | 35 (11.5) | 7,792 (16.2) | .282 | 0.64 [0.29, 1.41] | .270 |
| Any unhealthy alcohol usec | 35 (16.6) | 8,540 (17.1) | .955 | 0.97 [0.29, 3.23] | .959 |
| ASBI moduled | (n = 232) | (n = 48,976) | |||
| (1) Asked if you drink any alcohol | 145 (78.4) | 33,233 (74.6) | .557 | 1.21 [0.58, 2.50] | .605 |
| (2) Asked how much you drink | 125 (62.9) | 28,859 (64.7) | .812 | 0.94 [0.48, 1.83] | .857 |
| (3) Asked about heavy episodic drinking | 79 (37.3) | 12,034 (30.0) | .330 | 1.15 [0.57, 2.34] | .694 |
| (4) Offered advice about unhealthy alcohol use | 70 (31.7) | 8,370 (19.9) | .054 | 1.59 [0.82, 3.10] | .172 |
| (5) Advised to quit or reduce drinkinge | 27 (20.7) | 2,218 (7.8) | .012 | 2.31 [0.91, 5.86] | .077 |
Notes: Frequencies are unweighted; percentages are weighted. AOR = adjusted odds ratio; CI = confidence interval; ASBI = alcohol screening and brief intervention.
All analyses are weighted and adjusted for age group, sex, race/ethnicity, education, employment status, marital status;
adult men having >2 drinks per day and adult women having >1 drink per day;
any unhealthy alcohol use defined as engaging in either heavy alcohol use or heavy episodic drinking;
denominator for ASBI module limited to respondents having a checkup in the last 2 years;
denominator for fifth item excluded individuals who reported “no” to all items 1–3 of ASBI module.
No bivariate differences by transgender and nontransgender status were observed in any of the four alcohol use measures (Table 1). With regard to alcohol-related care, there were no significant differences in receipt of alcohol screening. A significantly greater proportion of transgender individuals reported being advised to quit or reduce their alcohol use than their nontransgender peers (20.7% vs. 7.8%, respectively, p = .012) (Table 1). However, this difference was attenuated after adjusting for sociodemographic characteristics (adjusted odds ratio = 2.31, 95% CI [0.91, 5.86], p = .077).
Discussion
In this probability-based sample of U.S. adults, approximately 46% of transgender adults reported any alcohol use and approximately 16% met criteria for unhealthy alcohol use, proportions that were not statistically different from their nontransgender peers. Receipt of alcohol-related care also did not differ statistically by transgender status. However, regardless of transgender status, a minority of people in the United States are being asked about and/or receiving advice about their drinking, which is consistent with previous research (Glass et al., 2016).
The lack of statistical differences between transgender and nontransgender adults in alcohol use were somewhat surprising because previous research suggests that transgender populations report high levels of alcohol use (Benotsch et al., 2016; Brown & Jones, 2016; Coulter et al., 2015; Garofalo et al., 2006; Melendez et al., 2006; Santos et al., 2014). However, this prior work has focused on vulnerable groups of transgender people, including ethnic minority youth (Garofalo et al., 2006), people living with HIV (Melendez et al., 2006), and veterans using care through the Veterans Health Administration (Brown & Jones, 2016), and none used probability-based sampling methods. Thus, these studies may not be representative of the larger transgender population. However, participation in the BRFSS is predicated on having a phone and the time to complete the interview. Because transgender populations experience high rates of social environmental stresses that may preclude participation in a phone-based survey (e.g., homelessness, poverty; Grant et al., 2010), it is unclear whether the BRFSS achieves a representative sample of transgender adults. Until more and better probability-based data about transgender individuals become available, accurate estimates of alcohol use and screening among this minority population will remain unclear.
No previous study has assessed receipt of alcohol-related care among transgender individuals; thus, comparison of the study’s findings to others is limited. Our analyses suggest that transgender adults may be more likely to be advised to quit or reduce drinking than their nontransgender peers, but this finding was no longer statistically significant after accounting for other sociodemographic characteristics. Further research with a larger sample of transgender adults may help to clarify whether a significant difference exists. Moreover, it is unclear whether transgender individuals most in need of brief intervention (i.e., persons with unhealthy alcohol use) receive such services. Because in the present sample only 35 transgender individuals indicated any unhealthy alcohol use, we were unable to analyze this subsample as a result of its small size. Future studies with larger samples should address these questions.
Although there is expert guidance on gathering data regarding transgender status in federal health research (Gender Identity in U.S. Surveillance [GenIUSS] Group, 2014), questions remain about other sex-specific measures such as heavy episodic drinking; this study met with the nexus of these issues. For instance, the number of drinks consumed on one occasion that increases health risks is gender specific (e.g., no more than four for men and three for women). This definition relies on biological definitions of male or female sex (Wechsler et al., 1995), but it remains unclear how and if those parameters apply to transgender individuals. For example, a person may have been assigned male sex at birth but identify as female and be taking feminizing hormones, which may influence how alcohol is metabolized and influences health. Further research is needed to investigate whether there are inadvertent biases to measuring alcohol use among transgender individuals with items that have sex-specific criteria.
Related, a significant limitation of this study is that in 2014 the BRFSS questionnaire suggested that interviewers did not systematically assess respondents’ sex. Interviewers may have determined the sex of the respondent, potentially inferring sex based on vocal timbre (Conron et al., 2012). No data are available on whether interviewers asked or interpreted respondents’ sex; thus, it is not possible to account for potential misclassification. Consequently, our aforementioned recommendations for future research come with the important qualification that respondents not only have autonomy in answering gender identity but also retain autonomy in identifying their sex.
Several additional limitations should be considered. First, although this was a probability-based sample of transgender adults, the data are from eight states and may not be representative of the U.S. population. Second, transgender groups were combined into one category, which precluded examining heterogeneity among the transgender population. Third, the survey assessed alcohol screening during the most recent health checkup in the past 2 years, but it is possible that respondents’ past-month drinking changed following the health checkup. Fourth, although measures of alcohol-related care in this report are included in two large U.S. population surveys, including the BRFSS and the National Survey on Drug Use and Health (Center for Behavioral Health Statistics and Quality, 2014; Glass et al., 2016), these measures have not been validated. Last, the survey instrument intended to assess alcohol screening but could not make distinctions between alcohol screenings with a validated tool versus other forms of assessment.
Despite these limitations, this study represents an initial step in investigating associations between transgender status and alcohol use and related care. It is unclear whether the lack of differences reflects accurate population patterns or is attributable to the small sample size, and only additional probability-based samples of transgender populations with representation from more states will clarify these preliminary findings. Consistent with multiple previous studies (Glass et al., 2016; Williams et al., 2011), findings suggest that receipt of recommended evidence-based care for unhealthy alcohol use—both screening and brief intervention—could be improved among transgender individuals and their nontransgender peers. However, despite similar needs for screening and brief intervention, future epidemiologic and intervention research must be attentive to the intense stigma and chronic sociopolitical challenges faced by transgender individuals (Institute of Medicine, 2011).
Footnotes
This work was supported by Health Services Research & Development Career Development Awards to John R. Blosnich (CDA-14-408) and Emily C. Williams (CDA-12-276) and a Clinical Sciences Research & Development Award to Keren Lehavot (CX000867) from the Department of Veterans Affairs. Josoph E. Glass is supported by the National Institutes of Health Extramural Loan Repayment program for Health Disparities Research (L60 MD009373). The opinions expressed in this work are those of the authors and do not necessarily reflect those of the funders, institutions, the Department of Veterans Affairs, or the United States Government.
References
- Benotsch E. G., Zimmerman R. S., Cathers L., Pierce J., McNulty S., Heck T., Snipes D. J. Non-medical use of prescription drugs and HIV risk behaviour in transgender women in the Mid-Atlantic region of the United States. International Journal of STD & AIDS. 2016;27:776–782. doi: 10.1177/0956462415595319. doi:10.1177/0956462415595319. [DOI] [PubMed] [Google Scholar]
- Blosnich J. R., Brown G. R., Shipherd J. C., Kauth M., Piegari R. I., Bossarte R. M. Prevalence of gender identity disorder and suicide risk among transgender veterans utilizing Veterans Health Administration care. American Journal of Public Health. 2013;103:e27–e32. doi: 10.2105/AJPH.2013.301507. doi:10.2105/AJPH.2013.301507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blosnich J. R., Brown G. R., Wojcio S., Jones K. T., Bossarte R. M. Mortality among veterans with transgender-related diagnoses in the Veterans Health Administration, FY2000-2009. LGBTHealth. 2014;1:269–276. doi: 10.1089/lgbt.2014.0050. doi:10.1089/lgbt.2014.0050. [DOI] [PubMed] [Google Scholar]
- Blosnich J. R., Marsiglio M. C., Gao S., Gordon A. J., Shipherd J. C., Kauth M., Fine M. J. Mental health of transgender veterans in US states with and without discrimination and hate crime legal protection. American Journal of Public Health. 2016;106:534–540. doi: 10.2105/AJPH.2015.302981. doi:10.2105/AJPH.2015.302981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borges G., Loera C. R. Alcohol and drug use in suicidal behaviour. Current Opinion in Psychiatry. 2010;23:195–204. doi: 10.1097/YCO.0b013e3283386322. doi:10.1097/YCO.0b013e3283386322. [DOI] [PubMed] [Google Scholar]
- Brown G. R., Jones K. T. Mental health and medical health disparities in 5135 transgender veterans receiving healthcare in the Veterans Health Administration: A case-control study. LGBT Health. 2016;3:122–131. doi: 10.1089/lgbt.2015.0058. doi:10.1089/lgbt.2015.0058. [DOI] [PubMed] [Google Scholar]
- Center for Behavioral Health Statistics and Quality. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2014. National Survey on Drug Use and Health (NSDUH): Summary of methodological studies, 1971–2014. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System: 2014 summary data quality report. 2015a Retrieved from http://www.cdc.gov/brfss/annual_data/2014/pdf/2014_dqr.pdf.
- Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System: Comparability of data BRFSS 2014. 2015b Retrieved from http://www.cdc.gov/brfss/annual_data/2014/pdf/compare_2014.pdf.
- Chavez L. J., Ornelas I. J., Lyles C. R., Williams E. C. Racial/ethnic workplace discrimination: Association with tobacco and alcohol use. American Journal of Preventive Medicine. 2015;48:42–49. doi: 10.1016/j.amepre.2014.08.013. doi:10.1016/j.amepre.2014.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chew L. D., Nelson K. M., Young B. A., Bradley K. A. Association between alcohol consumption and diabetes preventive practices. Family Medicine. 2005;37:589–594. [PubMed] [Google Scholar]
- Conron K. J., Scott G., Stowell G. S., Landers S. J. Transgender health in Massachusetts: Results from a household probability sample of adults. American Journal of Public Health. 2012;102:118–122. doi: 10.2105/AJPH.2011.300315. doi:10.2105/AJPH.2011.300315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coulter R. W., Blosnich J. R., Bukowski L. A., Herrick A. L., Siconolfi D. E., Stall R. D. Differences in alcohol use and alcohol-related problems between transgender- and nontransgender-identified young adults. Drug and Alcohol Dependence. 2015;154:251–259. doi: 10.1016/j.drugalcdep.2015.07.006. doi:10.1016/j.drugalcdep.2015.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garofalo R., Deleon J., Osmer E., Doll M., Harper G. W. Overlooked, misunderstood and at-risk: Exploring the lives and HIV risk of ethnic minority male-to-female transgender youth. Journal of Adolescent Health. 2006;38:230–236. doi: 10.1016/j.jadohealth.2005.03.023. doi:10.1016/j.jadohealth.2005.03.023. [DOI] [PubMed] [Google Scholar]
- Gender Identity in U.S. Surveillance (GenIUSS) Group. Best practices for asking questions to identify transgender and other gender minority respondents on population-based surveys. In: Herman J. L., editor. Los Angeles, CA: The Williams Institute; 2014. Retrieved from http://williamsinstitute.law.ucla.edu/wp-content/uploads/geniuss-report-sep-2014.pdf. [Google Scholar]
- Glass J. E., Bohnert K. M., Brown R. L. Alcohol screening and intervention among United States adults who attend ambulatory healthcare. Journal of General Internal Medicine. 2016;31:739–745. doi: 10.1007/s11606-016-3614-5. doi:10.1007/s11606-016-3614-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant J. M., Mottet L. A., Tanis J., Herman J. L., Harrison J., Keisling M. Washington, DC: National Center for Transgender Equality and the National Gay and Lesbian Task Force; 2010. National transgender discrimination survey report on health and health care. [Google Scholar]
- Institute of Medicine. Washington DC: Author; 2011. The health of lesbian, gay, bisexual, and transgender people: Building a foundation for better understanding. [PubMed] [Google Scholar]
- Jonas D. E., Garbutt J. C., Amick H. R., Brown J. M., Brownley K. A., Council C. L., Harris R. P. Behavioral counseling after screening for alcohol misuse in primary care: A systematic review and meta-analysis for the U.S. Preventive Services Task Force. Annals of Internal Medicine. 2012;157:645–654. doi: 10.7326/0003-4819-157-9-201211060-00544. doi:10.7326/0003-4819-157-9-201211060-00544. [DOI] [PubMed] [Google Scholar]
- Kaner E. F., Beyer F., Dickinson H. O., Pienaar E., Campbell F., Schlesinger C., Burnand B. Effectiveness of brief alcohol interventions in primary care populations. Cochrane Database of Systematic Reviews, Issue 2. 2007 doi: 10.1002/14651858.CD004148.pub3. Article No. CD004148. doi:10.1002/14651858.CD004148.pub3. [DOI] [PubMed] [Google Scholar]
- Kuntsche E., Knibbe R., Gmel G., Engels R. Who drinks and why? A review of socio-demographic, personality, and contextual issues behind the drinking motives in young people. Addictive Behaviors. 2006;31:1844–1857. doi: 10.1016/j.addbeh.2005.12.028. doi:10.1016/j.addbeh.2005.12.028. [DOI] [PubMed] [Google Scholar]
- Melendez R. M., Exner T. A., Ehrhardt A. A., Dodge B., Remien R. H., Rotheram-Borus M.-J., Hong D. Health and health care among male-to-female transgender persons who are HIV positive. American Journal of Public Health. 2006;96:1034–1037. doi: 10.2105/AJPH.2004.042010. doi:10.2105/AJPH.2004.042010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism. Washington, D.C.: National Institutes of Health, U.S. Department of Health and Human Services; 2007. Helping patients who drink too much: A clinician's guide (updated 2005 edition) (pp. 1–34) [Google Scholar]
- Saitz R. Clinical practice. Unhealthy alcohol use. The New England Journal of Medicine. 2005;352:596–607. doi: 10.1056/NEJMcp042262. doi:10.1056/NEJMcp042262. [DOI] [PubMed] [Google Scholar]
- Santos G.-M., Rapues J., Wilson E. C., Macias O., Packer T., Colfax G., Raymond H. F. Alcohol and substance use among transgender women in San Francisco: Prevalence and association with human immunodeficiency virus infection. Drug and Alcohol Review. 2014;33:287–295. doi: 10.1111/dar.12116. doi:10.1111/dar.12116. [DOI] [PubMed] [Google Scholar]
- Stotzer R. Violence against transgender people: A review of United States data. Aggression and Violent Behavior. 2009;14:170–179. doi:10.1016/j.avb.2009.01.006. [Google Scholar]
- Wechsler H., Dowdall G. W., Davenport A., Rimm E. B. A gender-specific measure of binge drinking among college students. American Journal of Public Health. 1995;85:982–985. doi: 10.2105/ajph.85.7.982. doi:10.2105/AJPH.85.7.982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilcox H. C., Conner K. R., Caine E. D. Association of alcohol and drug use disorders and completed suicide: An empirical review of cohort studies. Drug and Alcohol Dependence, 76, Supplement. 2004:S11–S19. doi: 10.1016/j.drugalcdep.2004.08.003. doi:10.1016/j.drugalcdep.2004.08.003. [DOI] [PubMed] [Google Scholar]
- Williams E. C., Johnson M. L., Lapham G. T., Caldeiro R. M., Chew L., Fletcher G. S., Bradley K. A. Strategies to implement alcohol screening and brief intervention in primary care settings: A structured literature review. Psychology of Addictive Behaviors. 2011;25:206–214. doi: 10.1037/a0022102. doi:10.1037/a0022102. [DOI] [PubMed] [Google Scholar]