Abstract
Rural African American cocaine users experience high rates of STIs/HIV. This NIDA-funded trial tested an adapted evidence-based risk reduction program versus an active control condition. Participants were 251 African American cocaine users in rural Arkansas recruited from 2009–2011. Outcomes included condom use skills and self-efficacy, sexual negotiation skills, peer norms, and self-reported risk behavior. The intervention group experienced greater increases in condom use skills and overall effectiveness in sexual negotiation skills. Both groups reported reductions in trading sex, improvements in condom use self-efficacy, and increased use of specific negotiation skills. Implications and limitations are discussed.
Keywords: Sexual risk, respondent-driven sampling, cocaine use, condom use, active control condition, self-efficacy
Human immunodeficiency virus (HIV) and sexually transmitted infection (STI) rates are disproportionately high among African Americans, particularly in the rural South, with 68% of all rural HIV infections in the United States occurring in Southern states, and African Americans representing 50% of rural AIDS cases.1,2 Poverty and limited economic opportunities; decreased access to social services and health care; close social and sexual networks; HIV-related stigma; and educational, historical, and structural challenges are all contextual forces that shape sexual risk among rural African Americans in the South.3–5
Stimulant use confers additional HIV and STI risk as it leads to more risky sexual behavior such as unsafe sex.6 Multiple high risk sexual behaviors have been reported among rural and urban cocaine users, including Southern African American cocaine users.7,8 However, the perceived stigma of participation in HIV education programs, low perceived risk, and limited community resources are barriers to reducing risk in this under-served and vulnerable population.9,10
Although effective sexual risk reduction interventions have been designed for drug-using populations and for African Americans,11 none has demonstrated efficacy in rural African American drug users. Most research focuses on drug users in large urban centers12 and there is little research on modifications of evidence-based interventions to rural settings.11 However, adaptation of efficacious interventions to be more culturally relevant is crucial for maintaining or even enhancing the efficacy of risk reduction programs as they are transferred to new settings or new populations. It is particularly important that community needs are well-incorporated through dialogue and collaboration with community partners and that the core elements of the program are retained.13 Core elements are often identified by means of behavioral theories that frame or guide the content and process of the intervention programs.
Social Cognitive Theory (SCT) is a frequently used theoretical framework for sexual risk reduction interventions due to its effectiveness among vulnerable populations including drug users12 and African American heterosexuals.14 Specifically, SCT posits that sustained behavioral change is most likely to occur when individuals develop specific behavioral skills, perceive social support among their peers for engaging in those skills, and have an opportunity both to practice those skills and receive social or tangible reinforcement for performing them.15,16 As individuals practice their new skills in increasingly challenging situations and receive reinforcement for doing so, they develop increased confidence in their abilities, known as self-efficacy.17 Thus, SCT-based interventions often emphasize skill-building as a crucial first step, and provide opportunities for practice and feedback in the context of supportive peer groups. Extensive research in diverse populations has validated the links between lower sexual risk and SCT-based constructs, including acquisition of sexual risk negotiation and condom use skills, self-efficacy for condom use, and healthier peer norms.12,14,18
Safety Counts19–21 is a theory- and evidence-based intervention with proven efficacy among urban drug users and included in the Centers for Disease Control and Prevention’s Compendium of Evidence-Based HIV Prevention Interventions.22 It is grounded in SCT and the readiness to change constructs described in the Transtheoretical Model (TTM).23 Because it addresses sex and drug-related risks, Safety Counts may be particularly amenable to modification so that it addresses the multi-level barriers to safer sex that face African American cocaine users in the rural South and, as a result, fills an important gap in sexual risk reduction interventions. This manuscript describes the initial results of a randomized trial of an adapted version of Safety Counts in two rural Arkansas counties. An active control condition was included to address ethical concerns regarding the use of attention-control and usual care control groups24 and to assure appropriate equivalence of the two conditions.25
Methods
Participants
Participants were from two under-served, predominantly African American, rural counties in the Arkansas Delta region with HIV and STI rates that are higher than the rest of the state. These counties are nearly 50 miles from a large city, and the two small towns that serve as their respective county seats are approximately 18 miles apart from each other, taking an estimated 30 minutes to drive between them. There is profound lack of educational and economic opportunities and few medical and social services in these counties due to the loss of manufacturing and agricultural industries throughout the rural South.26 As a result, high school graduation rates are low, unemployment rates are high, and poverty rates are nearly twice the nationwide and statewide poverty rates.27,28 In this vulnerable environment with limited infrastructure, violent crime, prostitution, and drug use have flourished and concomitantly, rates of sexually transmitted diseases have escalated.26,28,29
Eligibility criteria for participation were: (a) age 18 or older, (b) self-identified as African American, Black, or mixed race of African American ancestry, (c) self-reported cocaine use at least once in the past 30 days, (d) self-reported oral, vaginal, or anal sex at least once in the past 30 days, (e) not participating in a drug treatment program at study entry and (f) residing in a study county. Exclusion criteria were: (a) incarceration, or (b) inability to provide contact information. The study was approved by the University of Arkansas for Medical Sciences Institutional Review Board.
Participants were recruited using a rolling cohort design across both counties, so that recruitment occurred sequentially and counties were alternated (see Table 1). At the beginning of the study, randomization among the two conditions determined that the control condition would be the condition implemented in the first county. Thus a cohort of African-American cocaine users was recruited in that county, all of whom would participate in the control condition. Subsequently, a cohort for the risk reduction condition (adapted Safety Counts) was recruited from the second county. Furthermore, within each county, the condition that was assigned to each cohort alternated as well, with the result that the delivery of each condition was separated by at least ten months in a given county. At least 22 and no more than 31 participants were recruited per cohort.
Table 1.
ROLLING COHORT PLAN FOR RECRUITMENT, INTERVENTION, ASSESSMENT ACROSS TWO COUNTIESa
| Months (during intervention/assessment phase) | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
||||||||||||||||||||
| County | 1–2 | 3–4 | 5–6 | 7–8 | 9–10 | 11–12 | 13–14 | 15–16 | 17–18 | 19–20 | 21–22 | 23–24 | 25–26 | 27–28 | 29–30 | 31–32 | 33–34 | 35–36 | 37–38 | 39–40 |
| 1 | ||||||||||||||||||||
|
| ||||||||||||||||||||
| C1: (SSA) | C3: (SRR) | C5: (SSA) | C7: (SRR) | C9: (SSA) | ||||||||||||||||
| 6m f/ub C1 | 6m f/ub C3 | 6m f/ub C5 | 6m f/ub C7 | 6m f/ub C9 | ||||||||||||||||
|
| ||||||||||||||||||||
| 12m f/u C1 | 12m f/u C3 | 12m f/u C5 | 12m f/u C7 | 12m f/u C9 | ||||||||||||||||
|
| ||||||||||||||||||||
| 2 | ||||||||||||||||||||
|
| ||||||||||||||||||||
| C2: (SRR) | C4: (SSA) | C6: (SRR) | C8: (SSA) | C10: (SSR) | ||||||||||||||||
| 6m f/ub C2 | 6m f/ub C4 | 6m f/ub C6 | 6m f/ub C8 | 6m f/ub C10 | ||||||||||||||||
|
| ||||||||||||||||||||
| 12m f/u C2 | 12m f/u C4 | 12m f/u C6 | 12m f/u C8 | 12m f/u C10 | ||||||||||||||||
Each cohort (C) included 4 gender-specific groups of 6–8 participants each; each cohort ranged from 22 to 31 participants total.
6m f/u: 6 month follow-up assessments
SSA = Social Services Access; SRR = Sexual Risk Reduction.
Power calculations for cluster randomization were conducted to determine the required sample size needed to detect the intervention effect on the outcomes of interest.30 After evaluation of various effect sizes based on the previous literature31,32 and adjusting intraclass correlation coefficient estimates based on data from the Rural Stimulant Study29 we proposed a final sample size of at least 240 after attrition.
Sampling and study sites
Respondent Driven Sampling (RDS)33 was used to recruit 324 African American cocaine users from the study counties. Community liaisons and members of the study’s Community Advisory Board (CAB), composed of ten African American cocaine-using county residents, identified five individuals who served as the initial study participants or “seeds” and began the RDS recruitment process. Identified seeds provided informed consent and completed a screening form and, if eligible, were invited to participate. Local staff members obtained consent, conducted baseline assessments, and assigned participants to the intervention cohort currently forming in their county. Each participant was given referral coupons to pass on to other individuals and reimbursed for referring up to five eligible individuals to the study.33 In addition to reimbursement for recruitment, participants were compensated $15 for time and $5 for travel for each assessment interview, and $5 for time and $5 for travel for each attended intervention session. Participants also received incentives such as condoms, personal care items (such as hand lotion, small durable zip-top cases with the study logo, etc., and valued at no more than $2 each), and t-shirts at the completion of each assessment and intervention session.
Intervention sessions and most assessments took place at conveniently—yet discreetly-located local offices in each county to provide easy access while avoiding potential disclosure of participants’ drug-using status. Community events were held in local public meeting venues.
Hypothesis
It was hypothesized that participants in the sexual risk condition would demonstrate significantly greater post-intervention improvements in condom use skills, sexual negotiation skills, condom use self-efficacy, risky peer norms, and risky sexual behaviors when compared with participants in the control condition.
Intervention conditions
Common elements
Both conditions followed the basic structure of the Safety Counts intervention. Core elements of Safety Counts were retained but session content was tailored to meet the study aims and the needs of the local cocaine-using population based on previous research in the area,8,10 input from the CAB and community liaisons,34 and focus groups conducted with members of the study population.35 For example, we adapted content of Safety Counts to address primarily the risks of HIV and STI for non-injectors because of the project’s focus on cocaine users and prior research8 documenting rarity of injection use amongst cocaine users in these rural counties. Other key changes made to the Safety Counts protocol included revising intervention scripts to reflect the rural, rather than urban, drug setting; conducting same-gender group sessions; restricting attendance to participants only at the community events rather than allowing invited guests; and conducting follow-up sessions in study offices rather than on the street. Community engagement was emphasized throughout to build social capital and trust and to create a more culturally-relevant intervention.
Both conditions included two two-hour group sessions, two 60-minute individual sessions, two two-to-three-hour community events, and two 40-minute follow-up individual sessions. The entire program for a given cohort occurs over four months. Group sessions included six to eight same-gender participants from the recruitment cohort. Participants completed the two groups sessions together before separating for individual sessions. All members of a cohort, both male and female, attended the community events together.
Group sessions and community events were co-led by a local health educator and a peer leader. The health educator conducted all individual sessions. The same health educator conducted all sessions for a cohort so that he or she could reinforce session activities and provide personalized guidance and referrals. Peer leaders were all African American residents of study counties who had histories of cocaine use and reported abstinence from use for at least one year. The health educators and peer leaders were selected based on recommendations from community liaisons and received extensive training on session content and procedures using active learning, modeling, and behavioral rehearsal with feedback.
Both conditions focused on enhancing healthy behaviors relevant to that condition using theory-based methods including goal setting, skills-building, and problem-solving. Since both conditions involved the application of a complex, multi-dimensional protocol, it was important to control for any factors that might compromise the integrity of the experimental design. Procedures were implemented to enhance intervention quality control across both conditions including the development of detailed intervention protocols, ensuring adequate qualifications and training of health educators and peer leaders, pilot testing of intervention materials and methods, bi-weekly meetings with health educators to monitor treatment delivery, and interim analyses of process and manipulation check measures to ensure fidelity to the treatment protocols. Health educators and peer leaders for both conditions were blind to study hypotheses, so that interventionists’ expectations would not contaminate the delivery of intervention protocols. To avoid potential contamination effects, peer leaders and health educators were hired and trained separately for each condition. During training, interventions were presented as containing necessary information for supporting health and quality of life among rural African-American cocaine users. All assessment and intervention staff were blind to study hypotheses and treatment outcomes. Assessment staff were hired and trained separately from intervention staff and not allowed to witness or assist with any intervention activities except transportation to and from the study office for intervention activities. Session audiotapes were reviewed by investigative team members to document participant involvement and protocol fidelity.
The Sexual Risk Reduction Condition
The content of this condition was adapted from Safety Counts and emphasized multiple aspects of sexual risk reduction. Group session 1 helped participants identify their personal risk for acquiring STIs or HIV, practice condom use skills, and identify their stage of readiness to change for specific sexual risk behaviors. Discussion of stories of successful behavior change by drug-using peers provided opportunities for modeling and motivation and helped participants identify sources of social support for their risk reduction efforts. Group session 2 focused on helping participants choose a personally-relevant and measurable goal for reducing their sexual risk, identify first steps to take towards their goal, identify barriers to the goal, brainstorm possible solutions to the barriers, and identify sources of social support and reinforcement. Individual sessions reviewed and refined each participant’s risk reduction goal and progress towards that goal, identified encountered barriers, reinforced the pursuit of social support for reducing sexual risk, provided problem-solving for overcoming barriers and augmented social support as needed. Community events were designed to strengthen participation in the program, provide opportunities for reinforcement of program norms and messages, and provide social support for risk reduction efforts. Event activities included a humorous skit that reinforced messages from the group sessions, brainstorming about addressing barriers to risk-reduction goals, and a drawing for gender-specific gift baskets filled with personal care items valued at $15.00. The follow-up individual sessions provided opportunities for goal review and reinforcement for progress toward goal attainment, identification of new barriers along with strategies for overcoming those barriers, and identification of next steps for achieving or maintaining goals. Free condoms were available at all sessions.
The Social Services Access Condition
The control condition was an active, culturally-relevant intervention, which included SCT-based strategies that have been demonstrated to influence behavior change. This condition was designed to be identical to the sexual risk reduction condition in structure and time, so that participants received an equivalent amount of contact with concerned professionals and with other African American cocaine users. The content focused on increasing access to and use of social and community services such as educational or legal support, medical or dental care, or financial assistance.
Data collection
Participants were assessed at baseline, post-intervention (within four weeks of the last intervention session), and 6 and 12-month follow-up. Post-intervention assessments were the same as the baseline assessment. This manuscript reports only on analyses of baseline and post-intervention data to examine preliminary study effects, since several study outcomes (i.e., behavioral skills, self-efficacy) would be expected, based on SCT, to change more quickly than others (e.g., overall risk behaviors in sexual relationships).15
The first baseline assessment was conducted on February 4, 2009, and the last post-intervention assessment occurred on August 5, 2011. Three types of sexual risk outcomes were used to test the efficacy of the intervention: (1) self-reported sexual risk behaviors (unprotected sex and trading sex), (2) observable behavioral skills (condom use and sexual risk negotiation skills), and (3) theory-based constructs (self-efficacy for condom use and perceived peer norms for safe sexual behavior). The assessment was arranged so that the most emotionally-challenging scales were in the middle of the assessment and less challenging items were at the beginning and end. Pretests of the complete battery were conducted with members of the CAB and the interviewers to identify and revise survey items that were confusing, unclear, or repetitive. Steps taken to reduce error due to bias included employing two local interviewers to conduct the assessment; using Computer-Assisted Personal Interviewing (CAPI) technology; and extensive interviewer training using guided practice and rehearsal in encouraging episodic memory recall, responding to questions or emotional demands, and promoting a supportive and non-judgmental atmosphere. The assessment protocol took approximately 2.5 hours to complete with a 15-minute break.
Measures
Measure of Observed Condom Use Skills (MOCUS)
The MOCUS36 uses scripted wording to instruct respondents to place a condom on a penile model. The presence or absence of seven observable skills, including properly opening the condom package, pinching the tip and correctly removing the condom, is coded by the observer. The MOCUS has a possible range of 0–7, with higher scores indicating more skilled behaviors.
Sexual risk negotiation skills
Adapting the protocol of Kelly et al.,37,38 participants were sequentially presented with two scripted scenarios (main partner and recently met partner), which included increasingly coercive requests for unprotected sex. Participants’ role-played responses to each scenario were audio-recorded and independently coded by two members of the research team for the presence or absence (1 or 0) of five specific verbal behaviors: acknowledgement of the coercive request, refusing unprotected sex, giving a reason for refusal, stating a need to be safer, and stating a preference for a safer sex alternative. These items were summed with a range of 0 to 5, with higher scores representing the presence of more risk-reducing responses. Each role play was also scored with a global rating of 1–7 to indicate overall effectiveness in reducing sexual risk.
We calculated inter-rater reliability for the summed score of risk reducing behaviors and the global rating of effectiveness for both the main and recently met partner scenarios using the weighted kappa, κ, statistic for ordered scale data39 using the guidelines introduced by Landis and Koch (1977).40 For analysis, we averaged the raters’ responses across main and recently met partner scenarios, resulting in a single summed score of risk reducing behaviors observed in the role plays and a single global rating of effectiveness in the role plays for each participant at each assessment time point.
Transtheoretical Model (TTM) of Change for Condom Use Self-Efficacy
Condom use self-efficacy questions were adapted from the TTM of Condom Use questionnaire.41 Respondents rated how sure they were that they could use condoms every time they had sex with a given partner type (main, other) in five situations. Self-efficacy for each situation was rated on a scale from 1 (“not at all sure”) to 5 (“extremely sure”). The ratings for the five questions were averaged within partner type, and the mean score across partner type was calculated.
Peer norms
A measure of peer norms that has been significantly associated with sexual risk42 was adapted for this study. Respondents were asked 13 items about the prevalence of sexual risk or protective behaviors, including condom use, trading sex, STIs, and substance use in isolation or in combination with sexual behavior, among their same-gender friends. A 5-point scale was used to report whether none, a few, about half, most or all of their friends engaged in each behavior. Some of the items asked about risk behaviors in the past three months, while others were phrased generically in the past or present tense. Items about protective behaviors were reverse-coded and the item scores summed, so that higher scores indicated riskier peer norms. Given that this measure had not been used in a similar population prior to this investigation, we calculated internal reliability (Cronbach’s alpha) for the measure using baseline data. Reliability was .91 for both male and female peer norms scales.
Risk Behavior Assessment (RBA)
Demographic and self-reported sexual risk behavior data were collected using items from the RBA,43 a structured interview that has been well-validated among men and women in diverse samples of current drug users.44,45 Age was analyzed as a continuous variable. Gender, marital status, education, and employment status were examined as dichotomous variables (% married or cohabiting, % high school graduate or GED, % employed or self-employed). Income was summarized as a three category ordinal variable (<$5,000, $5,000–$9,999, ≥$10,000). Self-reported sexual risk behaviors included number and gender of sex partners, condom use, and trading sex (exchanging sex for food, money, or drugs; and giving food, money, or drugs in exchange for sex). Respondents reported the number of times they had vaginal, oral, and/or anal sex (within partner gender) during the past 30 days and the number of times they used a condom or other barrier in those encounters. An absolute count of the number of reported unprotected sex acts in the past 30 days was then calculated by type of sex and overall.
Addiction Severity Index (ASI)
Self-reported substance use was measured using the alcohol and drug use items from the ASI,46 a widely used semi-structured instrument with demonstrated validity and reliability among substance-abusing populations. Respondents were asked if they have ever used a particular substance and if so, on how many of the past 30 days. Respondents were also asked how many days they had used multiple substances, including alcohol. These analyses include the number of days (truncated at 30) respondents used alcohol, marijuana, cocaine (powder or crack), and multiple substances.
Data analysis
Quantitative analyses were conducted on bivariate and multivariate levels. Initially, differences among participants’ demographic characteristics, baseline drug use, and baseline sexual risk behaviors between the two conditions were assessed using appropriate bivariate analyses. To test the overall effect of the intervention, we compared changes in outcome variables based on an intent-to-treat analysis between the two conditions from baseline to post-intervention. To account for the repeated measurements from each participant and the hierarchical structure of the data (i.e., individuals nested within cohorts), longitudinal generalized mixed models were used (SAS/STAT MIXED and GLIMMIX version 9.3, SAS Institute, Cary, NC, USA). The time and intervention-by-time interactions were included as fixed effects in the models to evaluate how the intervention means changed over time and how differences between intervention means changed over time. The cohort was included as a random effect in the intercept and slope for each of the outcome repeated measures models. The inclusion of the random component accounts for the hierarchical nature of the design. Different covariance structures were compared in the various repeated measures models based on graphical tools and information criteria such as the restricted maximum likelihood ratio test, the Akaike information criterion, and the Schwarz’s Bayesian information criterion. To obtain a parsimonious model, key demographic variables were included as fixed effects if they were statistically significant at the bivariate analysis level across the two treatment groups. All statistical tests were two-tailed with p < .05 considered statistically significant.
Results
Description of sample and baseline comparisons
Of the 324 individuals assessed for eligibility, 73 did not meet eligibility requirements, leaving a total sample of 251. Table 2 summarizes baseline demographics, drug use, and sexual behaviors of participants in each condition. Across conditions, approximately half of the participants were female and the majority were unemployed, with an average age of 38 years, an annual income of less than $5,000, and at least a high school education. Individuals in the social services condition were more likely than those in the sexual risk reduction condition to be married or cohabiting (p = .027).
Table 2.
BASELINE CHARACTERISTICS OF THE STUDY POPULATION GROUPED BY INTERVENTION CONDITION
| Variables | Social Services (N = 139) |
Risky Behavior (N = 112) |
|---|---|---|
| Demographics | ||
| Age (mean ± SD) | 38.5 ± 12.5 | 37.3 ± 13.0 |
| Female, N (%) | 67 (48%) | 55 (49%) |
| Married, N (%)* | 31 (22%) | 13 (12%) |
| High school graduate, N (%) | 71 (51%) | 54 (48%) |
| Employed, N (%) | 29 (21%) | 28 (25%) |
| Annual Income, N (%) | ||
| < $5,000 | 92 (71%) | 76 (76%) |
| $5,000 to $9,999 | 26 (20%) | 15 (15%) |
| ≥ $10,000 | 12 (9%) | 9 (9%) |
| In the 30 days prior to baseline (median, 1st and 3rd quartilea) | ||
| Times had sex | 10.0 [4.0–24.5] | 10.0 [3.0–24.0] |
| Number of sex partners | 1.0 [1.0–2.0] | 1.0 [1.0–2.0] |
| Times used alcohol | 15.0 [4.0–30.0] | 15.0 [5.0–30.0] |
| Times used marijuana | 7.0 [1.0–30.0] | 15.0 [2.0–30.0] |
| Times used cocaineb | 10.0 [3.0–20.0] | 10.0 [3.0–21.5] |
| Times used multiple substance | 12.0 [2.5–28.0] | 10.0 [5.0–30.0] |
| No. of sex partners > 1, N (%) | 40 (29.85%) | 40 (36.70%) |
p < .05
Interquartile range (Q3–Q1)
Sum of crack and powered cocaine truncated at 30 days.
Baseline sexual risk and drug use behaviors were similar across the two conditions. The median number of times participants had sex (vaginal, oral, and/or anal) and the number of partners 30 days prior to baseline were identical. The conditions were also identical with respect to the number of days of alcohol and cocaine use, and had similar median values for days of multi-drug use. While individuals in the sexual risk reduction condition reported more use of marijuana than those in the social services condition, the difference was not statistically significant.
Study outcomes
The mean number of sessions attended by participants in the sexual risk reduction condition (n = 112) was 4.12, the median number was 4.0 sessions. Among participants in the social services condition (n = 139), the mean for sessions attended was 4.98, while the median was 6.0 sessions. Table 3 displays the means, standard deviations, and outcomes for observed behavioral skills, theory-based constructs (self-efficacy and peer norms), and self-reported sexual risk behavior at baseline and post-intervention. To control for baseline differences in marital status across conditions, marital status was included in the longitudinal generalized mixed model as a fixed effect.
Table 3.
PRE/POST CHANGES IN BEHAVIORAL AND SELF-REPORTED OUTCOMES
| Outcomes | Social Servicesa |
Sexual Riska | p-values | ||
|---|---|---|---|---|---|
|
| |||||
| Interaction | Treatment | Time | |||
| Observed Behavioral Skills | |||||
| Condom skills (MOCUS) | 0.0013b | NA | NA | ||
| Pre | 3.24 ± 1.91 | 2.94 ± 1.59 | |||
| Post | 3.34 ± 1.76 | 4.01 ± 1.79 | |||
| Risk Reduction Role Plays | |||||
| —Sum of Specific Skills | |||||
| Pre | 2.20 ± 0.85 | 2.21 ± 0.81 | 0.3692 | .6176 | .0042 |
| Post | 2.33 ± 0.87 | 2.45 ± 0.83 | |||
| —Global rating of effectiveness | |||||
| Pre | 4.14 ± 1.59 | 4.07 ± 1.51 | 0.0416b | NA | NA |
| Post | 4.17 ± 1.66 | 4.58 ± 1.44 | |||
| Theoretically Based Constructs | |||||
| Perceived peer norms | 0.6738 | .9688 | .0669 | ||
| Pre | 33.50 ± 16.09 | 34.61 ± 14.68 | |||
| Post | 31.66 ± 17.33 | 31.33 ± 19.82 | |||
| Condom use self-efficacy total | |||||
| Pre | 3.04 ± 1.48 | 3.18 ± 1.46 | 0.2096 | .2248 | .0007 |
| Post | 3.30 ± 1.47 | 3.77 ± 1.32 | |||
| Condom use self-efficacy (Main partner) | |||||
| Pre | 2.40 ± 1.52 | 2.83 ± 1.53 | 0.5410 | .0513 | .0038 |
| Post | 2.82 ± 1.53 | 3.38 ± 1.42 | |||
| Condom use self-efficacy (Other partner) | |||||
| Pre | 4.01 ± 1.20 | 3.85 ± 1.30 | 0.0656 | .4581 | .0266 |
| Post | 4.04 ± 1.24 | 4.37 ± 0.90 | |||
| Self-Reported Risky Sex | |||||
| Total unprotected sex | 0.5287 | 09686 | .3260 | ||
| Pre | 12.57 ± 16.80 | 11.18 ±14.17 | |||
| Post | 10.90 ± 13.99 | 10.39 ± 16.13 | |||
| Total trading | |||||
| Pre | 39 (28%) | 28 (25%) | 0.9692 | .4558 | .0004 |
| Post | 20 (17%) | 12 (14%) | |||
Means, standard deviations, and percentages are reported based on unadjusted values.
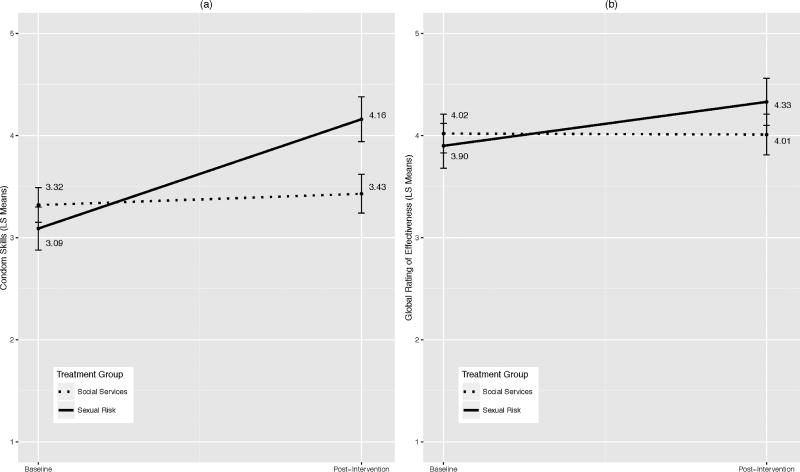
Given the significant interaction effect, the least square treatment means are presented as plots (see Figure 1a and 1b).
Observed behavioral skills
Significant treatment-by-time interactions were found for condom use skills (p = .0013) and for the global ratings of effectiveness in reducing sexual risk in the audiotaped role plays (p = .0416). At post-intervention, sexual risk reduction participants had significantly higher average condom use skill scores than the social services group (see Figure 1a). Similar changes occurred in the ratings of effectiveness in reducing sexual risk for the audiotaped role plays (see Figure 1b). At baseline, the two conditions had similar global ratings, but there were significant differences between the groups in these scores post-intervention with least squares mean difference of 0.32. Finally, for the summed scores of risk reduction behaviors observed in the role plays, there was a main time effect (p = .0042) with both conditions having increased scores from baseline to post-intervention.
Figure 1.
Time by treatment effects: Least squares mean for (a) condom skills and (b) global ratings of effectiveness in role plays.
Inter-rater reliability for the summed risk reduction behaviors observed in the role-play scenarios involving a main partner was κ = 0.52, indicating moderate agreement. Similar agreement was found for the global ratings of effectiveness at reducing risk with κ = 0.46. In contrast, inter-rater reliability for the summed risk negotiation scores and the global effectiveness ratings was lower for scenarios involving recently met partners, with κ = 0.37 and κ = 0.36, respectively.
Theory-based constructs
Participants in both conditions reported increased condom use self-efficacy at post-intervention. However, there were no statistically significant differences in condom use self-efficacy or perceived peer norms between the two conditions.
Self-reported sexual risk behavior
Participants in both conditions had a decline in total unprotected sex (vaginal, oral, and anal) post-intervention. However, there was no statistically significant difference between treatment conditions or in change over time (see Table 2). With regard to total trading sex, both conditions reported fewer incidences of having received or given drugs, money, or food in exchange for sex (i.e., a main time effect; p = .004).
Discussion
The results of this controlled trial of a culturally-adapted version of Safety Counts among rural African American cocaine users suggests that the intervention was effective in improving behavioral skills that are highly associated with reduced sexual risk. Specifically, participants in the sexual risk reduction condition demonstrated significantly greater improvement in condom use skills and in some sexual risk negotiation skills compared with participants in the control condition. Since acquisition of these skills is a pre-requisite for positive changes in sexual behavior,12,17 these results are encouraging.
We observed several significant changes in risk behavior from baseline to post-intervention in both conditions. Although neither group reported reductions in rates of unprotected sex, both groups had a sharp reduction in the proportion of individuals who engaged in transactional sex. Similarly, both groups improved in their condom use self-efficacy. Thus, both groups benefitted at least somewhat from participation in their respective conditions, but the participants in the sexual risk reduction condition improved their behavioral skills in both condom use and negotiation of safer sex to a greater degree. This finding is especially notable since the study population was composed of not-in-treatment drug users. Sexual risk tends to decrease among cocaine users during and after drug treatment,47 but the results of this study support the increasing evidence that individuals who are not pursuing drug treatment may nevertheless be able to benefit substantially from health promotion interventions.
The observed reductions in transactional sex and improvements in condom use self-efficacy in the control group were unanticipated. Some of the effects observed in this trial may be due to social desirability bias. We attempted to reduce this by including behavioral observation measures as study outcomes, and observed skills do show the strongest intervention effects. We also incorporated approaches that have been recommended to reduce social desirability and other reporting biases, including use of CAPI for all assessments, employing local interviewers familiar with the norms of the community, and adapting measures to reflect community experiences and language.48,49 The moderate inter-rater reliability estimates for the ratings of the recently met partner role-play scenarios may further limit the reliability of those findings.
The results also may have resulted from positive attention overall, or from our decision to employ an active control condition. The use of an active control condition is crucial for providing an appropriate test of the efficacy of a behavioral intervention but assuring that control conditions are sufficiently engaging and comparable yet simultaneously distinct from the intervention condition is a notable challenge in behavioral research.25,50 Our control condition was grounded in SCT, addressed issues of importance to the community, and may have provided social support or other indirect support for increasing participants’ general self-efficacy, which may have contributed to increased condom use self-efficacy for this group.51
Finally, in communities with extremely low social capital, such as in the communities in which we conducted this study, any intervention that helps develop social capital may result in improvements in health risk behaviors.52–54 Although this study did not include measures of social capital, the focus of both conditions on helping participants identify sources of interpersonal and community support for reaching their goals may have had a positive effect on risk reduction through these types of mechanisms.
It is noteworthy that participants reported a relatively low number of sexual partners overall, with a median number of one sex partner in the last 30 days. However, nearly one-third of the sample reported more than one partner during that time frame. Although a lower number of sexual partners is associated with reduced STI risk for a given individual, close-knit sexual networks (especially those in impoverished or racially segregated communities) may be vulnerable to the spread of STIs when they include just a few high-risk members, including members who have only one partner at a time but who change partners frequently.55 Interventions that address contextual factors in such networks, including structural interventions that support access to housing and other critical social services and that address disparities in incarceration rates that affect sex ratios and thus sexual network risks, must be considered in addition to interventions that address individual risk factors, such as the one described in this study.55
This study focuses specifically on the efficacy of an adapted intervention among African American cocaine users living in the Delta region of Arkansas and thus, the generalizability of study findings to dissimilar populations may be limited. However, this focus is a crucial one given the epidemiology of the HIV and STI epidemics and the racial and geographic disparities in HIV and STI incidence among rural African Americans in the Southern U.S. Additionally, although RDS is not a random sampling approach, samples obtained through RDS can be quite representative,33 and this approach has the added benefit of reaching hidden and highly stigmatized populations quite effectively.56
Despite the proliferation of evidence-based interventions to reduce sexual risk, and thereby, reduce HIV and STI incidence, very few have been designed for rural communities, particularly rural, not-in-treatment drug users. By using a relatively conservative test of an existing intervention, this project resulted in significant changes in behavioral skills that are critical for reducing sexual risk, and demonstrates that interventions originally developed for urban drug users can be adapted successfully for rural populations. As such, these results represent an advance in sexual risk reduction science in this vulnerable and disproportionately affected community.
Acknowledgments
The research described in this manuscript was supported by a research grant (award number R01DA024575) to Dr. Katharine Stewart from the National Institute on Drug Abuse. It was also supported in part by the Arkansas Center for Minority Health Disparities (award number P20MD002329 from the National Institute on Minority Health and Health Disparities), the Arkansas Prevention Research Center (award number 1U48DP001943 from the Centers for Disease Control and Prevention) and by the UAMS Translational Research Institute (award number 1UL1RR029884 from the National Center for Advancing Translational Science). The content is solely the responsibility of the authors and does not necessarily represent the official views of the funding Institutes and Centers. The authors also wish to express their heartfelt thanks to the staff, Community Advisory Board members, and participants of the JES’ US Project, without whom this work would not have been possible.
Footnotes
For additional information about this article https://muse.jhu.edu/article/648776
Contributor Information
Katharine E. Stewart, Department of Psychology and Vice Provost for Faculty Affairs at North Carolina State University.
Patricia B. Wright, College of Nursing at the University of Arkansas for Medical Sciences.
Brooke E. E. Montgomery, Department of Health Behavior and Health Education at the Fay W. Boozman College of Public Health at the University of Arkansas for Medical Sciences.
Carol Cornell, Department of Health Behavior and Health Education at the Fay W. Boozman College of Public Health at the University of Arkansas for Medical Sciences.
Donna Gullette, College of Nursing at the University of Arkansas for Medical Sciences.
Leavonne Pulley, Department of Health Behavior and Health Education at the Fay W. Boozman College of Public Health at the University of Arkansas for Medical Sciences.
Songthip Ounpraseuth, Department of Biostatistics at the Fay W. Boozman College of Public Health at the University of Arkansas for Medical Sciences.
Jeff Thostenson, Department of Biostatistics at the Fay W. Boozman College of Public Health at the University of Arkansas for Medical Sciences.
Brenda Booth, Department of Psychiatry at the College of Medicine at the University of Arkansas for Medical Sciences and the Central Arkansas Veterans Healthcare System.
References
- 1.Centers for Disease Control and Prevention (CDC) Disparities in diagnoses of HIV infection between Blacks/African Americans and other racial/ethnic populations—37 states, 2005–2008. MMWR Morb Mortal Wkly Rep. 2011 Feb 4;60(4):93–8. [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention (CDC) HIV surveillance in urban and non-urban areas. Atlanta, GA: CDC; 2011. Available at: http://www.cdc.gov/hiv/topics/surveillance/resources/slides/urban-nonurban/index.htm. [Google Scholar]
- 3.Aral SO, Adimora AA, Fenton KA. Understanding and responding to disparities in HIV and other sexually transmitted infections in African Americans. Lancet. 2008 Jul 26;372(9635):337–40. doi: 10.1016/S0140-6736(08)61118-6. https://doi.org/10.1016/S0140-6736(08)61118-6. [DOI] [PubMed] [Google Scholar]
- 4.Chu C, Selwyn PA. Current health disparities in HIV/AIDS. AIDS Read. 2008 Mar;18(3):144–6. 152–8, C3. [PubMed] [Google Scholar]
- 5.Hogben M, Leichliter JS. Social determinants and sexually transmitted disease disparities. Sex Transm Dis. 2008 Dec;35(12Suppl):S13–8. doi: 10.1097/OLQ.0b013e31818d3cad. https://doi.org/10.1097/OLQ.0b013e31818d3cad. [DOI] [PubMed] [Google Scholar]
- 6.National Institute on Drug Abuse. Behavioral Therapies Development Program—effective drug abuse treatment approaches: The Matrix Model. Bethesda, MD: National Institute on Drug Abuse; 1995. Available at: https://archives.drugabuse.gov/BTDP/Effective/Rawson.html. [Google Scholar]
- 7.Fleming PL, Lansky A, Lee LM, et al. The epidemiology of HIV/AIDS in women in the southern United States. Sex Transm Dis. 2006 Jul;33(7 Suppl):S32–8. doi: 10.1097/01.olq.0000221020.13749.de. https://doi.org/10.1097/01.olq.0000221020.13749.de. [DOI] [PubMed] [Google Scholar]
- 8.Wright PB, Stewart KE, Fischer EP, et al. HIV risk behaviors among rural stimulant users: variation by gender and race/ethnicity. AIDS Educ Prev. 2007 Apr;19(2):137–50. doi: 10.1521/aeap.2007.19.2.137. https://doi.org/10.1521/aeap.2007.19.2.137. [DOI] [PubMed] [Google Scholar]
- 9.Brown EJ, Hill MA. Perceptions of HIV risks and prevention strategies by rural and small city African Americans who use cocaine: views from the inside. Issues Ment Health Nurs. 2005 May;26(4):359–77. doi: 10.1080/01612840590922416. https://doi.org/10.1080/01612840590922416. [DOI] [PubMed] [Google Scholar]
- 10.Wright PB, McSweeney JC, Frith SE, et al. Losing all the pieces: a qualitative study of HIV risk perception and risk reduction among rural African American women who use cocaine. Journal of Drug Issues. 2009 Jul;39(3):577–605. https://doi.org/10.1177/002204260903900306. [Google Scholar]
- 11.Lyles CM, Kay LS, Crepaz N, et al. Best-evidence interventions: findings from a systematic review of HIV behavioral interventions for US populations at high risk, 2000–2004. Am J Public Health. 2007 Jan;97(1):133–43. doi: 10.2105/AJPH.2005.076182. Epub 2006 Nov 30. https://doi.org/10.2105/AJPH.2005.076182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Van Empelen P, Kok G, van Kesteren NM, et al. Effective methods to change sex-risk among drug users: a review of psychosocial interventions. Soc Sci Med. 2003 Nov;57(9):1593–608. doi: 10.1016/s0277-9536(02)00557-9. https://doi.org/10.1016/S0277-9536(02)00557-9. [DOI] [PubMed] [Google Scholar]
- 13.Solomon J, Card JJ, Malow R. Adapting efficacious interventions: advancing translational research in HIV prevention. Eval Health Prof. 2006 Jun;29(2):162–94. doi: 10.1177/0163278706287344. https://doi.org/10.1177/0163278706287344. [DOI] [PubMed] [Google Scholar]
- 14.Darbes L, Crepaz N, Lyles C, et al. The efficacy of behavioral interventions in reducing HIV risk behaviors and incident sexually transmitted diseases in heterosexual African Americans. AIDS. 2008 Jun 19;22(10):1177–94. doi: 10.1097/QAD.0b013e3282ff624e. https://doi.org/10.1097/QAD.0b013e3282ff624e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bandura A. Social foundations of thought and action: a social cognitive theory. Englewood Cliffs, NH: Prentice Hall; 1985. [Google Scholar]
- 16.Bandura A. Social cognitive theory of moral thought and action. In: Kurtines WM, Gewirtz JL, editors. Handbook of moral behavior and development (vol 1) Hillsdale, NJ: Lawrence Erlbaum; 1991. pp. 45–103. [Google Scholar]
- 17.Bandura A. Perceived self-efficacy in the exercise of control over AIDS infection. Evaluation and Program Planning. 1990 Feb;13(1):9–17. https://doi.org/10.1016/0149-7189(90)90004-G. [Google Scholar]
- 18.Albarracin D, Gillette JC, Earl AN, et al. A test of major assumptions about behavior change: a comprehensive look at the effects of passive and active HIV-prevention interventions since the beginning of the epidemic. Psychol Bull. 2005 Nov;131(6):856–97. doi: 10.1037/0033-2909.131.6.856. https://doi.org/10.1037/0033-2909.131.6.856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rotheram-Borus MJ, Rhodes F, Desmond K, et al. Reducing HIV risks among active injection drug and crack users: the safety counts program. AIDS Behav. 2010 Jun;14(3):658–68. doi: 10.1007/s10461-009-9606-2. Epub 2009 Sep 11. https://doi.org/10.1007/s10461-009-9606-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rhodes F, Humfleet GL. Using goal-oriented counseling and peer support to reduce HIV/AIDS risk among drug users not in treatment. Drugs & Society. 1993;7(3–4):185–204. https://doi.org/10.1300/J023v07n03_13. [Google Scholar]
- 21.Hershberger SL, Wood MM, Fisher DG. A cognitive-behavioral intervention to reduce HIV risk behaviors in crack and injection drug users. AIDS Behav. 2003 Sep;7(3):229–43. doi: 10.1023/a:1025487501743. https://doi.org/10.1023/A:1025487501743. [DOI] [PubMed] [Google Scholar]
- 22.CDC’s Prevention Research Synthesis Project (PRS) Compendium of evidence-based HIV behavioral interventions and best practies for HIV prevention. Atlanta, GA: Centers for Disease Control and Prevention; 2016. Available at: http://www.cdc.gov/hiv/research/interventionresearch/compendium/index.html. [Google Scholar]
- 23.Prochaska JO, DiClemente CC. Transtheoretical therapy: toward a more integrative model of change. Psychotherapy: Theory, Research, and Practice. 1982 Fall;19(3):276–88. https://doi.org/10.1037/h0088437. [Google Scholar]
- 24.Duan N, Fox SA, Derose KP, et al. Maintaining mammography adherence through telephone counseling in a church-based trial. Am J Public Health. 2000 Sep;90(9):1468–71. doi: 10.2105/ajph.90.9.1468. https://doi.org/10.2105/AJPH.90.9.1468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lindquist R, Wyman JF, Talley KM, et al. Design of control-group conditions in clinical trials of behavioral interventions. J Nurs Scholarsh. 2007;39(3):214–21. doi: 10.1111/j.1547-5069.2007.00171.x. https://doi.org/10.1111/j.1547-5069.2007.00171.x. [DOI] [PubMed] [Google Scholar]
- 26.Gamm LD. Mental health and substance abuse services among rural minorities. J Rural Health. 2004 Summer;20(3):206–9. doi: 10.1111/j.1748-0361.2004.tb00030.x. https://doi.org/10.1111/j.1748-0361.2004.tb00030.x. [DOI] [PubMed] [Google Scholar]
- 27.U.S. Census Bureau. American Fact Finder. Washington, DC: US Census Bureau; 2016. Available at: http://www.factfinder.census.gov. [Google Scholar]
- 28.Arkansas Department of Health. County health profile data. Little Rock, AR: 2011. Available at: Retrieved 10/01/2010: Available at: http://www.healthy.arkansas.gov/programsServices/healthStatistics/Pages/Statistics.aspx. [Google Scholar]
- 29.Booth BM, Leukefeld C, Falck R, et al. Correlates of rural methamphetamine and cocaine users: results from a multi-state community study. J Stud Alcohol. 2006 Jul;67(4):493–501. doi: 10.15288/jsa.2006.67.493. https://doi.org/10.15288/jsa.2006.67.493. [DOI] [PubMed] [Google Scholar]
- 30.Simpson JM, Klar N, Donner A. Accounting for cluster randomization: a review of primary prevention trials, 1990 through 1993. Am J Public Health. 1995 Oct;85(10):1378–83. doi: 10.2105/ajph.85.10.1378. https://doi.org/10.2105/AJPH.85.10.1378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lindemann DF, Brigham TA, Harbke CR, et al. Toward errorless condom use: a comparison of two courses to improve condom use skills. AIDS Behav. 2005 Dec;9(4):451–7. doi: 10.1007/s10461-005-9017-y. https://doi.org/10.1007/s10461-005-9017-y. [DOI] [PubMed] [Google Scholar]
- 32.Kinsler J, Sneed CD, Morisky DE, et al. Evaluation of a school-based intervention for HIV/AIDS prevention among Belizean adolescents. Health Educ Res. 2004 Dec;19(6):730–8. doi: 10.1093/her/cyg091. Epub 2004 Jun 15. https://doi.org/10.1093/her/cyg091. [DOI] [PubMed] [Google Scholar]
- 33.Heckathorn DD, Semaan S, Broadhead RS, et al. Extension of respondent-driven sampling: a new approach to the study of injection drug users aged 18–25. AIDS Behav. 2002 Mar;6(1):55–67. https://doi.org/10.1023/A:1014528612685. [Google Scholar]
- 34.Stewart KE, Wright PB, Sims D, et al. The “translators”: engaging former drug users as key research staff to design and implement a risk reduction program for rural cocaine users. Subst Use Misuse. 2012 Apr;47(5):547–54. doi: 10.3109/10826084.2011.644379. https://doi.org/10.3109/10826084.2011.644379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Montgomery BE, Stewart KE, Wright PB, et al. “We as drug addicts need that program”: insight from rural African American cocaine users on designing a sexual risk reduction intervention for their community. Subst Use Misuse. 2012 Jan;47(1):44–55. doi: 10.3109/10826084.2011.628734. https://doi.org/10.3109/10826084.2011.628734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lindemann DF, Brigham TA. A Guttman scale for assessing condom use skills among college students. AIDS Behav. 2003 Mar;7(1):23–7. doi: 10.1023/a:1022505205852. https://doi.org/10.1023/A:1022505205852. [DOI] [PubMed] [Google Scholar]
- 37.Kelly JA, St Lawrence JS, Hood HV, et al. Behavioral intervention to reduce AIDS risk activities. J Consult Clin Psychol. 1989 Feb;57(1):60–7. doi: 10.1037//0022-006x.57.1.60. https://doi.org/10.1037/0022-006X.57.1.60. [DOI] [PubMed] [Google Scholar]
- 38.Somlai AM, Kelly JA, McAuliffe TL, et al. Role play assessments of sexual assertiveness skills: relationships with HIV/AIDS sexual risk behavior practices. AIDS Behav. 1998 Dec;2(4):319–28. https://doi.org/10.1023/A:1022622108917. [Google Scholar]
- 39.Cohen J. Statistical power analysis for the behavioral sciences. 2. New York, NY: Routledge; 1988. [Google Scholar]
- 40.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977 Mar;33(1):159–74. https://doi.org/10.2307/2529310. [PubMed] [Google Scholar]
- 41.Grimley DM, Prochaska GE, Prochaska JO. Condom use adoption and continuation: a transtheoretical approach. Health Educ Res. 1997;12(1):61–75. https://doi.org/10.1093/her/12.1.61. [Google Scholar]
- 42.Crosby RA, DiClemente RJ, Wingood GM, et al. Identification of strategies for promoting condom use: a prospective analysis of high-risk African American female teens. Prev Sci. 2003 Dec;4(4):263–70. doi: 10.1023/a:1026020332309. https://doi.org/10.1023/A:1026020332309. [DOI] [PubMed] [Google Scholar]
- 43.Needle R, Fisher DG, Weatherby N, et al. Reliability of self-reported HIV risk behaviors of drug users. Psychol Addict Behav. 1995 Dec;9(4):242–50. https://doi.org/10.1037/0893-164X.9.4.242. [Google Scholar]
- 44.Fisher DG, Reynolds GL, Jaffe A, et al. Reliability, sensitivity and specificity of self-report of HIV test results. AIDS Care. 2007 May;19(5):692–6. doi: 10.1080/09540120601087004. https://doi.org/10.1080/09540120601087004. [DOI] [PubMed] [Google Scholar]
- 45.Johnson ME, Fisher DG. Reliability of drug users’ self-report of economic variables. Addiction Research. 1999;7(3):227–38. https://doi.org/10.3109/16066359909004385. [Google Scholar]
- 46.McLellan AT, Cacciola JC, Alterman AI, et al. The Addiction Severity Index at 25: origins, contributions and transitions. Am J Addict. 2006 Mar-Apr;15(2):113–24. doi: 10.1080/10550490500528316. https://doi.org/10.1080/10550490500528316. [DOI] [PubMed] [Google Scholar]
- 47.Schroeder JR, Epstein DH, Umbricht A, et al. Changes in HIV risk behaviors among patients receiving combined pharmacological and behavioral interventions for heorin and cocaine dependece. Addict Behav. 2006 May;31(5):868–79. doi: 10.1016/j.addbeh.2005.07.009. Epub 2005 Aug 8. https://doi.org/10.1016/j.addbeh.2005.07.009. [DOI] [PubMed] [Google Scholar]
- 48.Schroder KE, Carey MP, Vanable PA. Methodological challenges in research on sexual risk behavior: I. Item content, scaling, and data analytical options. Ann Behav Med. 2003 Oct;26(2):76–103. doi: 10.1207/s15324796abm2602_02. https://doi.org/10.1207/S15324796ABM2602_02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Weinhardt LS, Forsyth AD, Carey MP, et al. Reliability and validity of self-report measures of HIV-related sexual behavior: progress since 1990 and recommendations for research and practice. Arch Sex Behav. 1998 Apr;27(2):155–80. doi: 10.1023/a:1018682530519. https://doi.org/10.1023/A:1018682530519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Campbell DT, Stanley J. Experimental and quasi-experimental designs for research. Chicago, IL: Rand-McNally; 1963. [Google Scholar]
- 51.Strecher VJ, DeVellis BM, Becker MH, et al. The role of self-efficacy in acheiving health behavior change. Health Educ Q. 1986 Spring;13(1):73–92. doi: 10.1177/109019818601300108. https://doi.org/10.1177/109019818601300108. [DOI] [PubMed] [Google Scholar]
- 52.Murayama H, Fujiwara Y, Kawachi I. Social capital and health: a review of prospective multilevel studies. J Epidemiol. 2012;22(3):179–87. doi: 10.2188/jea.JE20110128. Epub 2012 Mar 17. https://doi.org/10.2188/jea.JE20110128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Davies SL, Thind HR, Chandler SD, et al. Enhancing resilience among young people: the role of communities and asset-building approaches to intervention. Adolesc Med State Art Rev. 2011 Dec;22(3):402–40. [PubMed] [Google Scholar]
- 54.Webel A, Phillips JC, Rose CD, et al. A cross-sectional description of social capital in an international sample of persons living with HIV/AIDS (PLWH) BMC Public Health. 2012 Mar 13;12:188. doi: 10.1186/1471-2458-12-188. https://doi.org/10.1186/1471-2458-12-188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Adimora AA, Schoenbach VJ. Social context, sexual networks, and racial disparities in rates of sexually transmitted infections. J Infect Dis. 2005 Feb 1;191(Suppl 1):S115–22. doi: 10.1086/425280. https://doi.org/10.1086/425280. [DOI] [PubMed] [Google Scholar]
- 56.Wang J, Carlson RG, Falck RS, et al. Respondent-driven sampling to recruit MDMA users: a methodological assessment. Drug Alcohol Depend. 2005 May 9;78(2):147–57. doi: 10.1016/j.drugalcdep.2004.10.011. Epub 2004 Dec 22. https://doi.org/10.1016/j.drugalcdep.2004.10.011. [DOI] [PubMed] [Google Scholar]