Abstract
Background:
Neeri is a well-established polyherbal formulation prescribed for renal stones by the physicians but has not been experimentally evaluated for its antiurolithiatic potential using cell-lines.
Objective:
This study is aimed to scientifically substantiate the antiurolithiatic effect of Neeri extract (NRE) through calcium oxalate (CaOx) crystallization inhibition, scavenging of free radicals, and protection of renal tubular epithelial NRK-52E cells from oxalate-induced injury.
Materials and Methods:
The crystallization inhibition was studied by turbidimetric assay while the free radical scavenging potential was determined for superoxide and nitric oxide (NO) radicals. The cytoprotective effect against oxalate-induced injury was assessed by estimating lactate dehydrogenase (LDH) leakage and determining cell viability using 3-(4,5-Dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide assay.
Results:
NRE significantly inhibited the CaOx crystallization in a concentration-dependent manner and also scavenged superoxide (IC50 302.88 μg/ml) and NO (IC50 300.45 μg/ml) free radicals. It did not show any significant cytotoxicity for NRK-52E cells till the highest dose (500 μg/ml) and found to be safe. When NRK-52E cells, injured by exposing to oxalate crystals for 24 h, were treated with NRE, it appreciably prevented the cell injury in a dose-dependent manner. It significantly decreased the elevated LDH leakage toward normal range and improved renal cell viability (82.37% ± 0.87%), hence, prevented growth and retention of crystals.
Conclusion:
The experimental findings concluded that Neeri is a potent antiurolithiatic formulation that inhibited CaOx crystallization and prevented tubular retention of crystals by protecting the renal cells against oxalate-induced injury as well as reducing the oxidative stress by scavenging free radicals.
SUMMARY
Neeri extract significantly (P < 0.001) inhibited the in vitro crystallization (88.11% ± 7.70%) of calcium oxalate
It reduced oxidative stress by scavenging superoxide and nitric oxide free radicals
It significantly (P < 0.001) improved the cell viability by inhibiting the leakage of lactate dehydrogenase in a dose-dependent manner.

Abbreviations used: Ac: Absorbance of control, At: Absorbance of test, ANOVA: Analysis of variance, CaOx: Calcium oxalate, DMEM: Dulbecco's Modified Eagle's Medium, DMSO: Dimethyl sulfoxide, EDTA: Ethylenediaminetetraacetic acid, FBS: Fetal bovine serum, INT: Iodonitrotetrazolium, LDH: Lactate dehydrogenase, M: Molar, ml: Milliliter, mM: Millimolar, MTT: 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide, NAD: Nicotinamide adenine dinucleotide, NADPH: Nicotinamide adenine dinucleotide phosphate, NBT: Nitro blue tetrazolium, nm: Nanometer, NO: Nitric oxide, NRE: Neeri extract, PMS: Phenazine methosulfate, ROS: Reactive oxygen species, Sc: Slope of the graph of control, SEM: Standard error of mean, Si: Slope of the graph with inhibitor, U/I: International unit, mg: Microgram, ml: Microliter.
Keywords: Antiurolithiatic effect, calcium oxalate, free radicals, NRK-52E cells, renal cell-injury
INTRODUCTION
Urolithiasis or urinary stone, the presence of one or more calculi in the urinary tract, is a serious, debilitating problem worldwide, affecting approximately 12% of the population. It is the third most prevalent disease of the urinary system that affects about 11% population in India.[1,2,3] The highest risks of developing urolithiasis have been reported in Asian countries with lifetime recurrence rates of up to 50%.[4] Due to the very high incidences of recurrence and detrimental effects on renal functions, kidney stones have seriously jeopardized the public health and affected the quality of life.[5] Further, it increased the risk of developing chronic kidney disorders and is also associated with different cardiovascular diseases.[6,7,8,9,10] Among several types of renal stones such as oxalate, phosphate, struvite, cysteine, etc., the most common (80%) stones are composed of calcium oxalate (CaOx).[11,12] The CaOx stone occurs in two forms, i.e., monohydrate and dihydrate. The monohydrate form is more stable, having a greater affinity for renal tubular cells and clinically observed more frequently.[13,14]
The formation of urinary oxalate stones is a complex process which requires the supersaturation of urine followed by nucleation, growth, aggregation, and retention of crystals in renal tubules or tubular epithelial cells.[15,16] The crystal retention involves interaction between the crystals and renal tubular epithelial cells, including the adhesion or endocytosis of crystals. A significant role of crystal-induced renal cell injury has been suggested in the development of stones. The cell injury promotes the retention of CaOx crystals within the kidney by providing sites for attachment of crystals.[16] The exposure of tubular epithelial cells to oxalate, leads to the disruption of normal renal cell activities and mitochondrial dysfunctions. This enhances the production of reactive oxygen species (ROS) leading to oxidative stress, which in turn decreases the cell viability and leads to cell death by promoting apoptosis as well as necrosis.[17,18]
The present manuscript is mainly focused to elucidate the antiurolithiatic aspects of Neeri, a polyherbal formulation, especially prescribed for renal stones and restoring the altered renal functions. Neeri consists of extracts of several herbs, some classical Ayurvedic preparations, lixiviated herbal ash, exudates, etc., as described in Table 1. Further, this manuscript is the first report of experimental findings of such scientific investigations, in which Neeri was explored for its effects on CaOx crystallization, free radical scavenging, and oxalate-induced injury in renal tubular epithelial NRK-52E cells.
Table 1.
Composition of Neeri: Each 10 ml of Neeri syrup containing

MATERIALS AND METHODS
Herbal formulation
The excipient free active constituents of polyherbal formulation Neeri Syrup, in the form of concentrates, i.e., Neeri extract (hereinafter designated as “NRE”), were obtained as a gift sample from Aimil Pharmaceutical India Ltd., New Delhi (India).
Chemicals
All the chemicals used in turbidimetric and free radicals scavenging assays were of analytical grade and purchased from Qualigens Fine Chemicals, Mumbai (India) while the chemicals and culture media used in cell-line study were of tissue culture grade and purchased from Hi-Media Laboratories, Mumbai (India). All other chemicals and reagents used were of at least analytical grade.
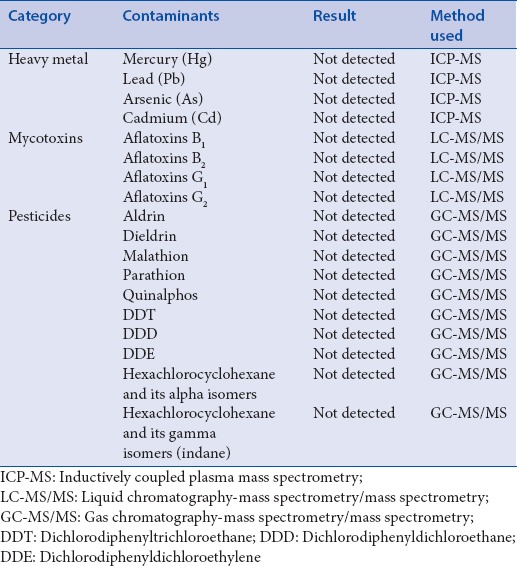
Estimation of contaminants
Following the standard guidelines, NRE was tested for the presence of various contaminants such as heavy metals, aflatoxins, pesticide residues, and their derivatives.[19,20] The various contaminants and different hyphenated techniques used for their estimation were depicted in Table 2.
Table 2.
Report of contaminants tested
Turbidimetric assay
The CaOx crystallization inhibition potential of NRE was estimated by time course measurement of turbidity changes due to crystallization of CaOx at 620 nm in the presence and absence of inhibitor, i.e., NRE.[21,22] For control (without inhibitor) study, 1.5 ml of calcium chloride solution (10 mM) was transferred into the cell, and blank reading was taken at 620 nm. Then, 1.5 ml of sodium oxalate solution (4 mM) was added, and measurement started immediately for 10 min. For study with inhibitors, a mixture of 1.0 ml calcium chloride solution (10 mM) and 1.0 ml NRE solutions (previously filtered through 0.45 μ syringe filter) at different concentrations 250, 500, 750, 1000, 1250, and 1500 μg/ml was versed in the cell, and a blank reading was taken. Then, a volume of 1.0 ml of sodium oxalate solution (4 mM) was added, and measurement was started immediately for 10 min. The percentage inhibition of CaOx crystallization was calculated using the formula:
% inhibition = [1 − (Si/Sc)] × 100
Where; Si: Slope of graph (turbidity changes vs. time) in the presence of inhibitor (NRE) and Sc: Slope of graph without inhibitor (control).
The photomicrograph of CaOx crystals, taken with a trinocular light microscope equipped with a digital camera, were visually analyzed for size, number, and aggregation of crystals.
Free radicals scavenging assays
Superoxide scavenging assay
The method is based on the fact that photooxidation of riboflavin generates superoxide radicals that reduce the nitro blue tetrazolium (NBT) to a blue-colored formazan which can be measured at 560 nm.[23,24] The antioxidant potential of NRE was calculated as the percentage of superoxide radicals scavenged and expressed in the form of IC50 values. The reaction mixture containing 200 μl ethylenediaminetetraacetic acid solution (0.1 M), 100 μl NBT (1.5 mM), 200 μl phosphate buffer (0.067 M), and 100 μl test samples (NRE solutions of varying concentrations, e.g., 100, 200, 300, 400, 500 and 600 μg/ml) was incubated for 5–8 min at 37°C. Then, 100 μl solutions of riboflavin (0.12 mM) were added, and the volume was made up to 3.0 ml using phosphate buffer. Now, the contents were illuminated for 12 min by incubating in a light box, and the absorbance was immediately measured at 560 nm against the blank.[25] Ascorbic acid was used as standard. The percentage inhibition of free radical generation was calculated using the formula:
% inhibition = ([Ac − At]/Ac) × 100
Where Ac is the absorbance of control (without NRE) and At is the absorbance of the test sample (with NRE).
Nitric-oxide scavenging assay
The procedure is based on the principle that the aqueous solution of sodium nitroprusside (at physiological pH 7.4) spontaneously generates nitric oxide (NO), which interacts with oxygen and produce nitrite ions. The nitrite ions diazotize with sulfanilic acid and couples with the Griess reagent to produce pink color which can be measured at 546 nm. NO scavengers compete with oxygen leading to decrease the production of nitrite ions. Briefly, the reaction mixture (3.0 ml) containing 2 ml of sodium nitroprusside (10 mM), 0.5 ml of standard phosphate buffered-(pH 7.4) solution and 0.5 ml of test sample (varying concentration of 100–600 μg/ml) or standard drug (ascorbic acid) was incubated at 25°C for 150 min. After incubation, 1.5 ml of reaction mixture and 1.5 ml of Griess reagent (1% sulfanilamide, 2% O-phosphoric acid and 0.1% of N-[1-naphthyl] ethylenediamine dihydrochloride) were mixed and allowed to stand for 30 min at 25°C. The absorbance of the chromophore formed was measured at 540 nm.[26,27] NO radical scavenging activity was calculated according to the following formula:
% inhibition = ([Ac − At]/Ac) × 100
Where Ac is the absorbance of control (without NRE) and At is the absorbance of test sample (with NRE).
Cell-line and culture
Normal rat epithelium-derived renal tubular epithelial cells, i.e., NRK-52E cells were procured from the National Centre of Cell Sciences, Pune (India). The cells were cultured and maintained in Dulbecco's Modified Eagle's Medium (DMEM) supplemented with 10% fetal bovine serum (FBS). At the confluence, the cell culture was trypsinized and seeded into a 96-multiwell plate at a seeding density of 1 × 104 cells per well. It was then incubated for 24 h to allow the attachment.
Cytotoxicity of Neeri extract
For determining the toxicity of NRE toward NRK-52E cells, various concentrations (500, 250, 125, 62.5, 31.25, 15.625, 7.812, and 3.906 μg/ml) of NRE were made by serial dilution and added to each well in triplicate. The plate was incubated for 24 h. Similarly, the control groups were also maintained, and the growth medium was aspirated from each well. Now, 3-(4,5-Dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT) assay was employed for determining cell viability.
Cytoprotective effect of Neeri extract against oxalate-induced injury
NRK-52E cells, cultured in DMEM supplemented with 10% FBS, were trypsinized and seeded in a 24-multiwell plate at a seeding density of 1 × 105 cells per well. Now, the plate was incubated overnight to allow cell attachment. To every well, 600 μg/ml oxalate solution was added and incubated for 24 h in the presence or absence of various concentrations (100, 200, 300, 400 and 500 μg/ml) of NRE. The cell control, i.e., growth and negative control groups, were also maintained similarly. The oxalate-induced cell injury and cytoprotection by NRE were assessed by determining the cell viability through MTT assay and monitoring the lactate dehydrogenase (LDH) leakage into the medium.[17]
3-(4,5-Dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide assay
At the end of the drug exposure period, the growth medium was aspirated from each well. The MTT solution (50 μl, 5 mg/ml) was added to each well and incubated in the dark for 4 h at 37°C to facilitate the formation of formazan crystals. After incubation, 200 μl acidified dimethyl sulfoxide (DMSO) was added to each well to dissolve the formazan crystals; and the purple color was obtained. The absorbance was measured at 570 nm using a plate reader, and the percentage viability of cells was calculated.
Lactate dehydrogenase leakage assay
At the end of the drug exposure period, the growth medium was collected from each well. Now, 50 μl of each 200 mM TRIS (pH 8.0), 50 mM lithium lactate, and phenazine methosulfate (PMS)-iodo-nitrotetrazolium (INT)-nicotinamide adenine dinucleotide (NAD) solutions were added to each well of a 96-multiwell plate.(For preparing PMS-INT-NAD solutions, 100 μl INT solution (3.3 mg/100 μl in DMSO), 100 μl PMS solution (0.9 mg/100 μl in water), and 2.3 μl of NAD solutions (0.374 mg/100 μl in water) were mixed and stored in the dark). The 50 μl growth medium was added to each well and incubated at 37°C for 5 min. The absorbance was measured at 490 nm at 0 and 2 min. Now, the change in absorbance per minute was calculated and LDH activity (U/I) was determined.
Data analysis
All values were expressed as mean ± standard error of mean. The data were analyzed by employing one-way analysis of variance using GraphPad Prism Version 5.00 (Trial) Software (GraphPad Software, Inc, La Jolla, USA). The values of P < 0.05 were considered as statistically significant.
RESULTS
Estimation of contaminants
NRE sample was found to be free from various tested contaminants, i.e., heavy metals, namely, Mercury (Hg), Lead (Pb), Arsenic (As), and Cadmium (Cd); aflatoxins, namely, B1, B2, G1, and G2; pesticide residues and their derivatives. The various tested contaminants were reported in Table 2.
Turbidimetric assay
NRE, when compared with control, decreased the turbidity in a concentration-dependent manner and significantly inhibited the crystallization of CaOx. The percentage inhibitions of CaOx crystallization by different concentrations of NRE were shown in Table 3. When compared with control, the number, size, and aggregates of CaOx crystals, as visually observed in photomicrographs shown in Figure 1, were also found to be less in NRE-treated group. This also supported the crystallization inhibition effect of NRE.
Table 3.
Effect of Neeri extract on inhibition of calcium oxalate crystallization

Figure 1.
The photomicrograph showing effect of Neeri extract on calcium oxalate crystallization. (a and b) are control groups, (c-h) are Neeri extract treated (250, 500, 750, 1000, 1250, and 1500 µg/ml, respectively) groups
Free radicals scavenging potential
NRE significantly scavenged the NO and superoxide free radicals in a concentration-dependent manner and might reduce the oxidative stress which in turn prevented the cell damage. The percentages of free radical scavenging potential of NRE and standard ascorbic acid were described in Table 4.
Table 4.
Free radicals scavenging potential of Neeri extract

Cytotoxicity of Neeri extract
NRE did not show any significant toxicity even at the highest concentration, i.e., 500 μg/ml and found to be quite safe for cell-based assay. The effects of various concentrations of NRE on the viability of NRK-52E cells were shown in Table 5. Since the IC50 value (not shown) was also found to be very high (>500 μg/ml) so the proportional range of safe doses (100–500 μg/ml) was selected for the study.
Table 5.
Cytotoxicity of Neeri extract on NRK-52E cell-viability

Cytoprotective effects of Neeri extract against oxalate-induced injury
NRE showed a significant protective effect against oxalate-induced injury in NRK-52E cells when studied by MTT assay. The oxalates caused significant toxicity in renal tubular epithelial cells and decreased the cell viability to 46.0 ± 0.66 as depicted in Table 6. NRE inhibited the injury and significantly increased the percentage viability of renal epithelial tubular cells in a concentration-dependent manner.
Table 6.
Effect of Neeri extract on cell-viability in 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide assay and lactate dehydrogenase activity
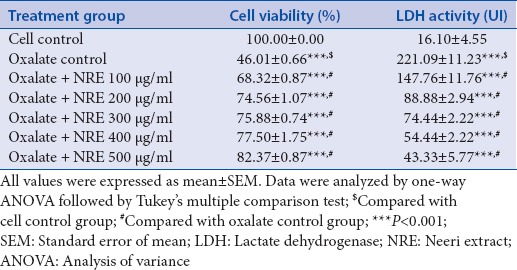
The oxalates caused significant injury in NRK-52E renal cells increased the LDH activity from 16.10 ± 4.55 − 221.09 ± 11.23 U/I and consequently decreased the cell viability. When renal epithelial cells were treated with different concentrations of NRE along with oxalates, a significant decrease in the elevation of LDH activity was observed as shown in Table 6. It clearly indicated that NRE protected the renal cells from oxalate-induced injury and improved the cell viability.
DISCUSSION
Despite of tremendous advances in the field of urology, there is no satisfactory antiurolithiatic drug in modern system of medicine which can be used in clinical therapy to dissolve stones or to prevent stone formation or recurrence; and the physicians have to depend on alternative systems of medicines.[11,28,29] Herbal drugs are the major constituents of different alternative systems of medicines such as Ayurveda, Unani, Siddha, etc. The present manuscript is also focused to a polyherbal formulation Neeri and aimed to elucidate its antiurolithiatic potential against CaOx urolithiasis.
Extracts of herbal drugs constitute the major part of NRE. The herbal drugs are easily accessible to many contaminants such as heavy metals, mycotoxins, pesticides, etc. These can easily absorb heavy metals such as Cd, Hg, As, Pb, etc., from contaminated air, water, and soil. The Cd causes kidney damage, lung cancer, bone disorders; Hg causes kidney damage, neurological disorders; As causes lung cancer, skin diseases; and Pb causes neurological disorders, affects the reproductive and hemopoietic systems.[30]
Mycotoxins such as aflatoxins also contaminate the medicinal herbs and foodstuffs. Aflatoxins are severely toxic secondary metabolites that are primarily produced by two fungal species, i.e., Aspergillus flavus and Aspergillus parasiticus. The World Health Organization classified the aflatoxins as carcinogenic. There are about 18 different types of aflatoxins, out of which four are considered important and designated as B1, B2, G1, and G2.[31]
Some pesticides may also reach to the herbal drugs during agricultural practices such as spraying, handling of soils during farming, etc., and also during fumigation for storage purposes. Many pesticides such as organophosphates, for example, malathion, parathion, etc., organochlorides, for example, hexachlorocyclohexanes, dichlorodiphenylethanes, etc., are toxic to human beings and have long residual action.[20,32,33]
Any of such contaminants can be highly toxic to human beings if present in the formulation and consumed, hence, needs to be determined. No such types of contaminants were detected in NRE.
The hyperoxaluria is considered as the major risk factor for CaOx stones. It is usually associated with renal cell injury and causes a variety of changes in the normal architecture of tubular epithelial cells that facilitate the renal adherence and retention of CaOx crystals. It also alters the cell membrane integrity, increases the free radical production, and decreases the antioxidant levels that enhance the cell death.
The renal tubular epithelial NRK-52E cells were significantly injured when exposed to oxalate ions in culture media. The interactions between injured tubular epithelial cells and CaOx crystals and/or oxalate ions are considered to have a significant role in urolithiasis.[34,35,36] The exposure of renal tubular cells to high levels of oxalate crystals leads to oxidative stress by (a) generation of free radicals and overproduction of ROS, (b) increasing lipid peroxidation, and (c) decreasing cellular antioxidant status. The mitochondria and nicotinamide adenine dinucleotide phosphate (NADPH) oxidase are the major source of ROS in renal cells.[37,38,39,40] There are also the evidence that hyperoxaluria causes the activation of the renin-angiotensin system and generates angiotensin-2 which in turn activates the membrane-associated NADPH oxidase. The NADPH oxidase leads to the overproduction of ROS and hence oxidative stress.[39,41,42] The oxidative stress, mitochondrial dysfunctions, and altered surface properties of the cell membrane that disrupt the membrane integrity, facilitates the retention and growth of CaOx stones in renal tubules. The ROS-induced renal epithelial cell injury, determined by the imbalance between defense mechanisms of antioxidants and generation of ROS, is also considered as the prerequisite step in the pathogenesis of urolithiasis.[43,44]
The NRE significantly inhibited the in vitro CaOx crystallization in a concentration-dependent manner and therefore altered the conditions of hyperoxaluria. Further, NRE also significantly protected the NRK-52E cells from oxalate-induced injury. The nephroprotective effect of NRE against oxalate-induced injury may also be potentiated by the antioxidant effect as it significantly scavenged NO and superoxide free radicals. It hampered the production of ROS, reduced the oxidative stress, and protected the renal cells. Further, it also showed significant nephroprotective potential against the heavy metal Pb-induced nephrotoxicity in rats. It also prevented oxidative stress by preventing the elevation in thiobarbituric acid reactive substances levels and decreasing the lipid peroxidation.[45]
LDH, a stable cytosolic enzyme, is considered as the marker of cell injury. It is released when any injury to cell or cell membrane, which leads to cell death, occurs.[17] Oxalates significantly enhanced the NRK-52E cellular damage and increased the LDH release. NRE protected the renal tubular epithelial cells from oxalate-induced injury, decreased the LDH release, and improved the cell viability. Further, NRE is a plant product, and plant products are usually considered as more natural, less expensive, and having least side effects.[46]
CONCLUSION
The polyherbal formulation Neeri was confirmed to have significant antiurolithiatic potential against CaOx stones. It inhibited the in vitro CaOx crystallization which is the critical step in calculi formation. Further, it also protected the renal tubular epithelial NRK-52E cells from oxalate-induced injury and increased the cell viability that hampered the growth and retention of CaOx stones in renal tubules.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
The authors are thankful to Aimil Pharmaceutical India Limited for providing a gift sample of NRE. The authors are also thankful to IKGPTU, Jalandhar (Punjab), India, for providing a platform to carry out this research work.
REFERENCES
- 1.Leye A, Jaeger P, Robertson W, Unwin R. Renal stone disease. Medicine. 2007;35:415–9. [Google Scholar]
- 2.Worcester EM, Coe FL. Nephrolithiasis. Prim Care. 2008;35:369–91. doi: 10.1016/j.pop.2008.01.005. vii. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lulat SI, Yadav YC, Balaraman R, Maheshwari R. Antiurolithiatic effect of lithocare against ethylene glycol-induced urolithiasis in Wistar rats. Indian J Pharmacol. 2016;48:78–82. doi: 10.4103/0253-7613.174564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.López M, Hoppe B. History, epidemiology and regional diversities of urolithiasis. Pediatr Nephrol. 2010;25:49–59. doi: 10.1007/s00467-008-0960-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gao S, Chen W, Peng Z, Li N, Su L, Lv D, et al. Urinary metabonomics elucidate the therapeutic mechanism of Orthosiphon stamineus in mouse crystal-induced kidney injury. J Ethnopharmacol. 2015;166:323–32. doi: 10.1016/j.jep.2015.03.025. [DOI] [PubMed] [Google Scholar]
- 6.Ando R, Nagaya T, Suzuki S, Takahashi H, Kawai M, Okada A, et al. Kidney stone formation is positively associated with conventional risk factors for coronary heart disease in Japanese men. J Urol. 2013;189:1340–6. doi: 10.1016/j.juro.2012.11.045. [DOI] [PubMed] [Google Scholar]
- 7.Domingos F, Serra A. Nephrolithiasis is associated with an increased prevalence of cardiovascular disease. Nephrol Dial Transplant. 2011;26:864–8. doi: 10.1093/ndt/gfq501. [DOI] [PubMed] [Google Scholar]
- 8.Rule AD, Bergstralh EJ, Melton LJ, 3rd, Li X, Weaver AL, Lieske JC. Kidney stones and the risk for chronic kidney disease. Clin J Am Soc Nephrol. 2009;4:804–11. doi: 10.2215/CJN.05811108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rule AD, Roger VL, Melton LJ, 3rd, Bergstralh EJ, Li X, Peyser PA, et al. Kidney stones associate with increased risk for myocardial infarction. J Am Soc Nephrol. 2010;21:1641–4. doi: 10.1681/ASN.2010030253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rule AD, Krambeck AE, Lieske JC. Chronic kidney disease in kidney stone formers. Clin J Am Soc Nephrol. 2011;6:2069–75. doi: 10.2215/CJN.10651110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ghelani H, Chapala M, Jadav P. Diuretic and antiurolithiatic activities of an ethanolic extract of Acorus calamus L. rhizome in experimental animal models. J Tradit Complement Med. 2016;6:431–6. doi: 10.1016/j.jtcme.2015.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bhagavathula AS, Mahmoud Al-Khatib AJ, Elnour AA, Al Kalbani NM, Shehab A. Ammi visnaga in treatment of urolithiasis and hypertriglyceridemia. Pharmacognosy Res. 2014;7:397–400. doi: 10.4103/0974-8490.167894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Butterweck V, Khan SR. Herbal medicines in the management of urolithiasis: Alternative or complementary? Planta Med. 2009;75:1095–103. doi: 10.1055/s-0029-1185719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Saha S, Verma RJ. Evaluation of hydro-alcoholic extract of Dolichos biflorus seeds on inhibition of calcium oxalate crystallization. J Herb Med. 2015;5:41–7. [Google Scholar]
- 15.Srinivas S, Venkanna B, Madan-Mohan E, Krishna-Mohan C. Urolithiasis: Overview. Int J Pharm Res Biomed Anal. 2012;1:20–31. [Google Scholar]
- 16.Tsujihata M. Mechanism of calcium oxalate renal stone formation and renal tubular cell injury. Int J Urol. 2008;15:115–20. doi: 10.1111/j.1442-2042.2007.01953.x. [DOI] [PubMed] [Google Scholar]
- 17.Aggarwal A, Tandon S, Singla SK, Tandon C. Diminution of oxalate induced renal tubular epithelial cell injury and inhibition of calcium oxalate crystallization in vitro by aqueous extract of Tribulus terrestris. Int Braz J Urol. 2010;36:480–8. doi: 10.1590/s1677-55382010000400011. [DOI] [PubMed] [Google Scholar]
- 18.Zager RA, Johnson AC, Becker K. Renal cortical lactate dehydrogenase: A useful, accurate, quantitative marker of in vivo tubular injury and acute renal failure. PLoS One. 2013;8:e66776. doi: 10.1371/journal.pone.0066776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lehotay SJ, de Kok A, Hiemstra M, Van Bodegraven P. Validation of a fast and easy method for the determination of residues from 229 pesticides in fruits and vegetables using gas and liquid chromatography and mass spectrometric detection. J AOAC Int. 2005;88:595–614. [PubMed] [Google Scholar]
- 20.World Health Organization (WHO) WHO Guidelines for Assessing Quality of Herbal Medicines with Reference to Contaminants and Residue. Geneva: World Health Organization; 2007. [Last accessed on 2016 Nov 06]. Available from: http://www.apps.who.int/medicinedocs/index/assoc/s14878e/s14878e.pdf . [Google Scholar]
- 21.Bensatal A, Ouahrani MR. Inhibition of crystallization of calcium oxalate by the extraction of Tamarix gallica L. Urol Res. 2008;36:283–7. doi: 10.1007/s00240-008-0157-1. [DOI] [PubMed] [Google Scholar]
- 22.Khare P, Mishra VK, Kakkar A, Bais N, Singh R. Study on in-vitro anti-lithiatic activity of Phyllanthus niruri Linn. leaves by homogenous precipitation and turbiditory method. Int J Pharm Pharm Sci. 2014;6:124–7. [Google Scholar]
- 23.Beauchamp C, Fridovich I. Superoxide dismutase: Improved assays and an assay applicable to acrylamide gels. Anal Biochem. 1971;44:276–87. doi: 10.1016/0003-2697(71)90370-8. [DOI] [PubMed] [Google Scholar]
- 24.Zhishen J, Mengcheng T, Jianming W. The determination of flavonoid contents on mulberry and their scavenging effects on superoxide radical. Food Chem. 1999;64:555–9. [Google Scholar]
- 25.Mandade R, Sreenivas SA, Sakarkar DM, Choudhury A. Radical scavenging and antioxidant activity of Hibiscus rosasinensis extract. Afr J Pharm Pharmacol. 2011;5:2027–34. [Google Scholar]
- 26.Sreejayan, Rao MN. Nitric oxide scavenging by curcuminoids. J Pharm Pharmacol. 1997;49:105–7. doi: 10.1111/j.2042-7158.1997.tb06761.x. [DOI] [PubMed] [Google Scholar]
- 27.Marcocci L, Maguire JJ, Droy-Lefaix MT, Packer L. The nitric oxide-scavenging properties of Ginkgo biloba extract EGb 761. Biochem Biophys Res Commun. 1994;201:748–55. doi: 10.1006/bbrc.1994.1764. [DOI] [PubMed] [Google Scholar]
- 28.Evan AP. Physiopathology and etiology of stone formation in the kidney and the urinary tract. Pediatr Nephrol. 2010;25:831–41. doi: 10.1007/s00467-009-1116-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Prasad KV, Sujatha D, Bharti K. Herbal drugs in urolithiasis: A review. Pharmacogn Rev. 2007;1:175–9. [Google Scholar]
- 30.Singh R, Gautam N, Mishra A, Gupta R. Heavy metals and living systems: An overview. Indian J Pharmacol. 2011;43:246–53. doi: 10.4103/0253-7613.81505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wacoo AP, Wendiro D, Vuzi PC, Hawumba JF. Methods for detection of aflatoxins in agricultural food crops. J Appl Chem. 2014;2014:1–15. (Article ID 706291) http://dx.doi.org/10.1155/2014/706291 . [Google Scholar]
- 32.Kunle OF, Egharevba HO, Ahmadu PO. Standardization of herbal medicines – A review. Int J Biodivers Conserv. 2012;4:101–12. [Google Scholar]
- 33.Shaban NS, Abdou KA, Hassan NE. Impact of toxic heavy metals and pesticide residues in herbal products. Beni-Suef Univ J Basic Appl Sci. 2016;5:102–6. [Google Scholar]
- 34.Khan SR, Thamilselvan S. Nephrolithiasis: A consequence of renal epithelial cell exposure to oxalate and calcium oxalate crystals. Mol Urol. 2000;4:305–12. [PubMed] [Google Scholar]
- 35.Khan SR. Role of renal epithelial cells in the initiation of calcium oxalate stones. Nephron Exp Nephrol. 2004;98:e55–60. doi: 10.1159/000080257. [DOI] [PubMed] [Google Scholar]
- 36.Zuo J, Khan A, Glenton PA, Khan SR. Effect of NADPH oxidase inhibition on the expression of kidney injury molecule and calcium oxalate crystal deposition in hydroxy-L-proline-induced hyperoxaluria in the male Sprague-Dawley rats. Nephrol Dial Transplant. 2011;26:1785–96. doi: 10.1093/ndt/gfr035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kohjimoto Y, Kennington L, Scheid CR, Honeyman TW. Role of phospholipase A2 in the cytotoxic effects of oxalate in cultured renal epithelial cells. Kidney Int. 1999;56:1432–41. doi: 10.1046/j.1523-1755.1999.00683.x. [DOI] [PubMed] [Google Scholar]
- 38.Thamilselvan S, Byer KJ, Hackett RL, Khan SR. Free radical scavengers, catalase and superoxide dismutase provide protection from oxalate-associated injury to LLC-PK1 and MDCK cells. J Urol. 2000;164:224–9. [PubMed] [Google Scholar]
- 39.Umekawa T, Byer K, Uemura H, Khan SR. Diphenyleneiodium (DPI) reduces oxalate ion- and calcium oxalate monohydrate and brushite crystal-induced upregulation of MCP-1 in NRK 52E cells. Nephrol Dial Transplant. 2005;20:870–8. doi: 10.1093/ndt/gfh750. [DOI] [PubMed] [Google Scholar]
- 40.Olugbami JO, Gbadegesin MA, Odunola OA. In vitro free radical scavenging and antioxidant properties of ethanol extract of Terminalia glaucescens. Pharmacognosy Res. 2015;7:49–56. doi: 10.4103/0974-8490.147200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Umekawa T, Hatanaka Y, Kurita T, Khan SR. Effect of angiotensin II receptor blockage on osteopontin expression and calcium oxalate crystal deposition in rat kidneys. J Am Soc Nephrol. 2004;15:635–44. doi: 10.1097/01.asn.0000113321.49771.2d. [DOI] [PubMed] [Google Scholar]
- 42.Aggarwal D, Sharma M, Singla SK. The role of natural antioxidants as potential therapeutic agent in nephrolithiasis. Asian J Pharm Clin Res. 2013;6:48–53. [Google Scholar]
- 43.Ghodasara J, Pawar A, Deshmukh C, Kuchekar B. Inhibitory effect of rutin and curcumin on experimentally-induced calcium oxalate urolithiasis in rats. Pharmacognosy Res. 2010;2:388–92. doi: 10.4103/0974-8490.75462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Patel P, Patel M, Saralai M, Gandhi T. Antiurolithiatic effects of Solanum xanthocarpum fruit extract on ethylene-glycol-induced nephrolithiasis in rats. J Young Pharm. 2012;4:164–70. doi: 10.4103/0975-1483.100022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Barwal A, Kumari S, Verma SK, Goyal PK, Sharma I, Sharma S, et al. Evaluation of herbal formulation Neeri (NS-RF) for protective effect against heavy metal induced nephrotoxicity in rats. Indo Am J Pharm Res. 2015;5:2790–8. [Google Scholar]
- 46.Kumar BP, Kannan MM, Quine DS. Litsea deccanensis ameliorates myocardial infarction in wistar rats: Evidence from biochemical and histological studies. J Young Pharm. 2011;3:287–96. doi: 10.4103/0975-1483.90239. [DOI] [PMC free article] [PubMed] [Google Scholar]



