Abstract
Background
Bystander cardiopulmonary resuscitation (CPR) more than doubles the chance of surviving an out‐of‐hospital cardiac arrest. Recent data have shown considerable regional variation in bystander CPR rates across the Australian state of Victoria. This study aims to determine whether there is associated regional variation in rates of CPR training and willingness to perform CPR in these communities.
Methods and Results
We categorized each Victorian postcode as either a low or high bystander CPR region using data on adult, bystander‐witnessed, out‐of‐hospital cardiac arrests of presumed cardiac etiology (n=7175) from the Victorian Ambulance Cardiac Arrest Registry. We then surveyed adult Victorians (n=404) and compared CPR training data of the respondents from low and high bystander CPR regions. Of the 404 adults surveyed, 223 (55%) resided in regions with low bystander CPR. Compared with respondents from high bystander CPR regions, respondents residing in regions with low bystander CPR had lower rates of CPR training (62% versus 75%, P=0.009) and lower self‐ratings for their overall knowledge of CPR (76% versus 84%, P=0.04). There were no differences between the regions in their reasons for not having undergone CPR training or in their willingness to perform CPR. Rates of survival for bystander‐witnessed, out‐of‐hospital cardiac arrests were significantly lower in low bystander CPR regions (15.7% versus 17.0%, P<0.001).
Conclusions
This study found lower rates of CPR training and lower survival in regions with lower rates of bystander CPR in Victoria, Australia. Targeting these regions with CPR training programs may improve bystander CPR rates and out‐of‐hospital cardiac arrest outcomes.
Keywords: cardiac arrest, cardiopulmonary resuscitation, heart arrest
Subject Categories: Cardiopulmonary Resuscitation and Emergency Cardiac Care, Cardiopulmonary Arrest
Clinical Perspective
What Is New?
Our study found that the regional variation seen in bystander CPR rates for adult, witnessed, out‐of‐hospital cardiac arrest is associated with similar variation in the CPR training rates of residents.
Importantly, there was no difference between regions in willingness to provide or learn CPR.
What Are the Clinical Implications?
Providing CPR training in these regions may improve bystander CPR rates and thus outcomes from out‐of‐hospital cardiac arrest.
Introduction
Bystander cardiopulmonary resuscitation (CPR) for patients with out‐of‐hospital cardiac arrest (OHCA) more than doubles survival.1, 2 Bystander CPR increases the likelihood of patients being found in a shockable cardiac rhythm and of emergency medical services attempting a resusitcation.3 In turn, shockable rhythms are treatable with defibrillation and CPR and are also associated with greater survival.3 However, bystander CPR is not provided in every instance, and recent reports have indicated the existence of significant regional variation in rates of bystander CPR.4, 5, 6
In our region, the Australian state of Victoria, only 42% of those with OHCA receive bystander CPR (≈75% in bystander‐witnessed OHCAs).7 This occurs despite relatively high recognition of OHCA by dispatchers during the emergency call (≈85%)7 and the availability of dispatcher CPR instructions.8 As has been reported internationally,4, 5 we have also found a significant variation in bystander CPR rates across our state and, in some instances, between neighboring areas.6
Recent evidence from 2 studies9, 10 suggests residents in regions of low CPR may have lower rates of CPR training. A study of major CPR providers in the United States found regional variation in attendance at CPR classes over the course of a year, with lower rates seen in regions with lower rates of bystander CPR.9 Another report from Korea found regional variation in self‐reported CPR training, and again, an association was found between low training rates in regions with lower bystander CPR.10 Given that CPR training is associated with higher willingness11 and likelihood to perform CPR,12 it is possible that a regional variation in CPR training rates exists in our region and may be contributing to the variation seen in bystander CPR rates. In this study, we aimed to determine whether regions of Victoria with lower CPR rates also have lower rates of CPR training, knowledge, and willingness to perform CPR.
Methods
This cross‐sectional study was conducted in the Australian state of Victoria (population 5.79 million). The study used data from 2 sources: (1) the Victorian Cardiac Arrest Registry (VACAR) and (2) survey data of adult Victorians in 2016. This study was approved by the Monash University human ethics committee.
Identification of Regions With Low CPR Rates
The VACAR is described in detail elsewhere.7, 13 In brief, the VACAR is maintained by Ambulance Victoria and is a statewide OHCA registry using the Utstein definitions.14, 15
The VACAR includes a variable for bystander CPR, defined as any attempt at chest compressions (with or without breaths). The VACAR data were used to calculate bystander CPR rates for each Victorian postcode. To do this, we extracted cases of adult, bystander‐witnessed (not a paramedic) arrests of presumed cardiac etiology for the period from 2008 to 2015 (n=7175). As described elsewhere,6 we calculated annual smoothed estimates of the bystander CPR and OHCA survival rates for each Victorian postcode using mixed‐effects regression. This method provides more conservative estimates of the rates where data are sparse (eg, postcodes with small numbers of OHCAs) and is clustered in uneven group sizes. We allowed for the average rate to vary over time by using year as a linear predictor and for regional variation by using a random effect on each postcode. As previously used,6 the smoothed estimate refers to the fitted value of the model and is an inverse variance weighted average of the fixed‐ and random‐effect components of the model. Because bystander CPR and survival rates varied annually, we used smoothed estimates from the year 2015—the year closest to the survey year (early 2016)—in the statistical analysis.
Collection of CPR Training Data
Over the month of April 2016, a telephone survey of 404 adults in Victoria was conducted. Following a brief introduction of the study, the respondent's consent was implied by continuation in the survey. The survey methods and the demographics of the respondents are described elsewhere.11 Briefly, a computer‐assisted telephone interviewing survey of Victorian, English‐speaking adults was conducted by a professional survey center. The survey (available from the corresponding author) gathered information about demographics, previous CPR training, self‐rated confidence and knowledge about CPR (5‐point Likert scale), awareness of hands‐only CPR, and willingness to perform CPR in 5 scenarios (from close relative to stranger). A sample of 400 was selected based on previous CPR training rates in our region (estimated at 52%16) and a confidence interval of 95% and a margin of error of 5%. The survey response rate was 45%. The survey sampling strategy used mobile (25%) and landline (75%) phone numbers and aimed to include 75% metropolitan and 25% regional/rural residents to reflect the population and cardiac arrest distribution in the state. The survey also ascertained reasons for not having CPR training and the respondents’ residential postcode.
Analysis
The residential postcodes of those surveyed were categorized as either high or low CPR regions using the median smoothed bystander CPR rate for bystander‐witnessed arrests. In 2015, the median estimate of bystander CPR for witnessed OHCAs of cardiac origin among postcodes was 75.6%; postcodes with estimated CPR rates below this rate were categorized as regions with low bystander CPR and those at or above this rate were categorized as regions with high bystander CPR. Respondents residing in postcodes with no OHCAs during the study period (n=18) were categorized using the average bystander CPR rates of all surrounding postcodes with which they shared a boundary.
The telephone survey data and OHCA survival from 2015 were then compared between regions with high and low bystander CPR rates. Because all data were categorical, we used the χ2 statistic to compare groups. We used logistic regression to examine the independent association between regions with high and low CPR (high versus low) and CPR training, adjusting for the demographics (female sex, age groups, regional/rural postcode, born in English‐speaking country, and level of education) of those surveyed (reported as an adjusted odds ratio and 95% confidence interval). We also conducted a sensitivity analysis removing respondents residing in postcodes with no OHCAs. P<0.05 was considered to be statistically significant.
Results
Of the 404 adults surveyed, 223 (55%) resided in regions with low CPR. There were no significant differences in the demographic characteristics of respondents between the high and low CPR regions (Table 1).
Table 1.
A Comparison of the Demographics of Respondents From Regions With Low and High Bystander CPR
| Characteristics | Regions With Low Bystander CPR (n=223) | Regions With High Bystander CPR (n=181) | Univariate P Value | Adjusted Odd Ratio (95% CI) | Multivariate P Value |
|---|---|---|---|---|---|
| Female, n (%) | 124 (56) | 113 (62) | 0.16 | 0.78 (0.52–1.18) | 0.24 |
| Age, n (%) | |||||
| 18–34 | 22 (10) | 25 (14) | 0.29 | Reference | |
| 35–54 | 73 (33) | 68 (38) | 1.25 (0.64–2.45) | 0.51 | |
| 55–74 | 93 (42) | 51 (34) | 1.83 (0.93–6.62) | 0.08 | |
| ≥75 | 35 (16) | 27 (15) | 1.47 (0.65–3.33) | 0.35 | |
| Born in Australia, n (%)a | 163 (73) | 122 (67) | 0.81 | … | … |
| Born in English‐speaking country, n (%) | 174 (78) | 143 (79) | 0.99 | 1.10 (0.66–1.83) | 0.71 |
| Resides in rural region, n (%) | 61 (27) | 49 (27) | 0.30 | 0.93 (0.58–1.48) | 0.76 |
| Level of education, n (%) | |||||
| Primary or some high school | 40 (18) | 38 (21) | 0.40 | Reference | |
| High school | 92 (41) | 63 (35) | 1.58 (0.88–2.83) | 0.12 | |
| Tertiary | 91 (41) | 80 (44) | 1.35 (0.75–2.43) | 0.31 | |
| Prior CPR training, n (%) | 139 (62) | 135 (75) | 0.009 | 0.55 (0.35–0.87) | 0.01 |
CI indicates confidence interval; CPR, cardiopulmonary resuscitation.
Born in Australia was not included in multivariate model due to multicollinearity with born in English‐speaking country.
Respondents residing in regions with low CPR were less likely to have received CPR training (62% versus 75%, P=0.009; Figure 1) compared with residents of regions with high CPR rates, and this association remained significant after adjusting for the demographics of those surveyed (adjusted odds ratio: 0.55; 95% confidence interval, 0.35–0.87; P=0.01). The direction of effect and statistical significance did not change with removal of respondents with missing estimates for bystander CPR in the sensitivity analysis (data not shown).
Figure 1.
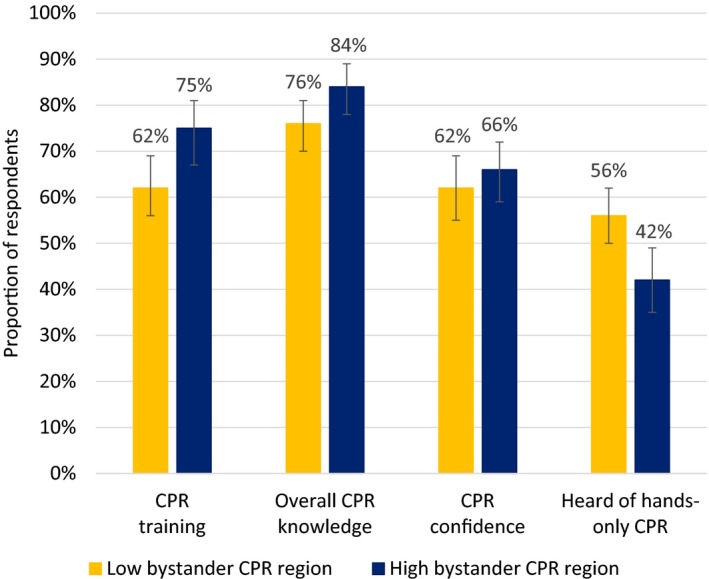
A comparison of rates of cardiopulmonary resuscitation (CPR) training, self‐reported knowledge, confidence to perform CPR, and awareness of hands‐only CPR between regions with low and high bystander CPR (error bars represent 95% confidence intervals).
For respondents who had received CPR training, there were no differences between the high and low regions in the time since CPR training (Table 2), although the majority had not received recent CPR training (71% were trained >12 months before the survey). Reasons for not receiving CPR training between the 2 regions were similar, with most stating they had “never thought about being trained” or citing “lack of time” as a factor. Approximately half of those who had never received CPR training stated that they would be willing to learn via a CPR training kit at home, and this proportion was similar between the 2 regions (50% versus 44% for high and low respectively, P=0.48).
Table 2.
A Comparison of CPR Training and Willingness to Perform CPR Between Low and High Bystander CPR Regions
| Characteristics | Regions With Low Bystander CPR (n=223) | Regions With High Bystander CPR (n=181) | P Value |
|---|---|---|---|
| Prior CPR training, n (%) | 139 (62) | 135 (75) | 0.009 |
| Time since training, n (%) | |||
| <1 y | 40 (29) | 38 (28) | |
| 1–5 y | 29 (21) | 22 (16) | |
| 5 y | 68 (49) | 73 (54) | 0.77 |
| Can recall | 9 (1) | 2 (1) | |
| Reasons for not receiving training, n (%) | |||
| Never thought about it | 49 (58) | 28 (61) | 0.78 |
| Time | 23 (27) | 9 (20) | 0.32 |
| Did not know where to learn | 13 (15) | 6 (13) | 0.71 |
| Cost | 6 (7) | 6 (13) | 0.27 |
| Other | 6 (7) | 6 (13) | 0.27 |
| Previously performed CPR in an emergency, n (%) | 28 (13) | 24 (13) | 0.65 |
| Heard of hands‐only CPR, n (%) | 124 (56) | 77 (43) | 0.03 |
| Source of hands‐only CPR awareness, n (%) | |||
| First aid course | 48 (39) | 38 (49) | 0.28 |
| Social media | 19 (15) | 10 (13) | |
| Other media | 25 (20) | 8 (10) | |
| Word of mouth | 24 (19) | 15 (19) | |
| DVD kit | 1 (1) | 0 (0) | |
| Other (online) | 2 (1) | 1 (3) | |
| Cannot recall | 3 (2) | 1 (1) | |
| Willingness to perform conventional CPR, n (%) | |||
| Close family member | 204 (91) | 160 (88) | 0.62 |
| Distant family member | 193 (86) | 152 (84) | 0.64 |
| Friend | 196 (88) | 152 (84) | 0.58 |
| Unrelated child | 189 (85) | 153 (85) | 0.31 |
| Stranger | 151 (67) | 121 (67) | 0.69 |
| Willingness to perform hands‐only CPR, n (%) | |||
| Close family member | 203 (91) | 158 (87) | 0.47 |
| Distant family member | 202 (91) | 157 (87) | 0.40 |
| Friend | 202 (91) | 159 (88) | 0.56 |
| Unrelated child | 190 (85) | 155 (86) | 0.46 |
| Stranger | 196 (88) | 150 (83) | 0.38 |
CPR indicates cardiopulmonary resuscitation.
Respondents in regions with lower CPR rates also had lower self‐ratings for their overall knowledge of CPR (good to excellent: 76% versus 84%; P=0.04; Figure 1), but they reported levels of confidence similar to those in high CPR regions. There was also no significant difference between the 2 regions in the willingness to perform either standard or hands‐only CPR on family members, children, friends, or strangers.
Residents in regions with low rates of CPR were more likely to have heard of hands‐only CPR; however, they were more likely to have heard about it through the media rather than in CPR classes.
In the postcodes in which respondents resided, rates of survival for bystander‐witnessed OHCAs in 2015 were significantly lower in regions with low bystander CPR (15.7% versus 17.0%, P<0.001; Figure 2).
Figure 2.
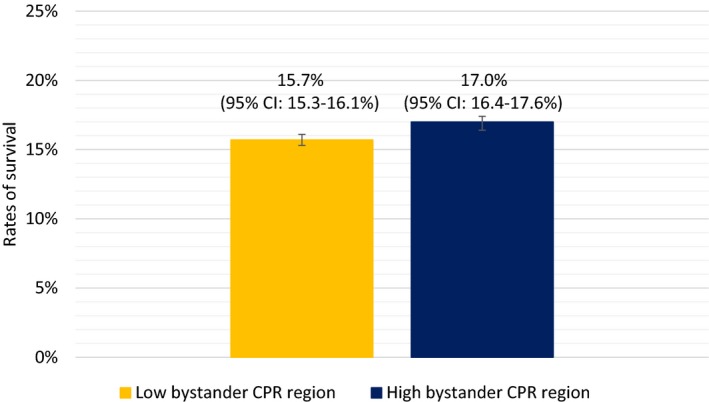
A comparison of rates of survival for bystander witnessed out‐of‐hospital cardiac arrests in 2015 between regions with low and high bystander cardiopulmonary resuscitation (CPR; error bars represent 95% confidence intervals [CI]).
Discussion
Across the Australian state of Victoria, we found that regions with low bystander CPR rates also had lower rates of CPR training, self‐rated CPR knowledge, and OHCA survival when compared with regions with high rates of CPR. However, there were no differences in confidence or willingness to perform CPR in hypothetical situations.
Our results confirm and add to those recently reported from Korea, in which regional variation in CPR rates was also associated with differences in CPR training rates.10 Given that people without CPR training are less likely to provide bystander CPR,17 this finding is important—particularly in our region, as we had not previously identified any unique characteristics of the population in these regions.18 We are currently listening to the emergency calls in regions with low bystander CPR to better understand the reasons for not providing CPR. However, it is possible that in some cases, untrained bystanders experience difficulty in identifying a person in cardiac arrest or lack confidence to follow dispatcher instructions. Importantly, our findings also suggest that untrained persons in regions of low CPR would be willing to perform and learn CPR, particularly using self‐instructional methods.
Targeting low CPR regions with CPR educational programs may have considerable potential to improve bystander CPR rates and survival, specifically if focused on regions with accompanying high OHCA incidence.19 The Community CPR Take 10 Program conducted in the United States, for example, targeted CPR education in high‐risk regions and saw a subsequent increase in CPR rates.20 More recent programs are now using different training strategies, (eg, classes, self‐instruction, online)21 to overcome the barriers of time and cost, and the promotion of hands‐only (or compression‐only) CPR is now encouraged internationally, especially for bystanders who are not trained in CPR.22, 23
Despite a lack of promotion in our region, there was reasonable awareness of hands‐only CPR in our population (50%), including regions with low bystander CPR; however, we did note a difference in the source of this information, with respondents from low CPR regions more likely to hear of hands‐only CPR via media or word of mouth rather than through formalized training, where they could practice. Future efforts to train residents in these regions may need to consider providing opportunities to receive hands‐on practice and to target groups within these regions known to have no prior CPR training. As reported previously, in our region, this includes young adults, those with lower levels of education, and residents born outside of Australia.11
Our study also has implications for regions considering implementing mobile device activation of lay rescuers to attend OHCA patients.24 An identified issue with such systems is a lack of trained rescuers.25 Emergency medical services planning to use these systems may need to consider identifying and training willing rescuers in regions with existing low bystander and community CPR training.
This study has several potential limitations. The survey data are subject to recall and potential responder bias. The OHCA bystander CPR rates are reported for witnessed OHCA of presumed cardiac etiology only and do not represent rates for all OHCA cases. We restricted the data to witnessed arrests in this study because there was regional variation in rates of witnessed arrest and because we wanted to remove cases that were obviously deceased by the time they were found by bystanders.
In summary, our study found that the regional variation seen in bystander CPR rates for adult witnessed OHCA is associated with a similar variation in the CPR training rates of residents. Importantly, there was no difference between regions in willingness to provide or learn CPR. Providing CPR training in these regions may improve bystander CPR rates and thus outcomes for those with OHCA.
Sources of Funding
This study is supported by a National Heart Foundation (NHF) Vanguard grant (no. 101048). Dr Bray is supported by a National Health and Medical Research Council/NHF Fellowship (no. 1069985). Dr Straney, Ms Cartledge, Dr Case and Professor Finn receive salary support from the NHMRC Centre of Research Excellence: the Australian Resuscitation Outcomes Consortium (Aus‐ROC; no. 1029983).
Disclosures
None.
Acknowledgments
We would like to thank staff at the Edith Cowan University Survey Research Center (ECU‐SRC) for assistance with the data collection.
(J Am Heart Assoc. 2017;6:e005972 DOI: 10.1161/JAHA.117.005972.)28584073
References
- 1. Sasson C, Rogers MA, Dahl J, Kellermann AL. Predictors of survival from out‐of‐hospital cardiac arrest: a systematic review and meta‐analysis. Circ Cardiovasc Qual Outcomes. 2010;3:63–81. [DOI] [PubMed] [Google Scholar]
- 2. Hasselqvist‐Ax I, Herlitz J, Svensson L. Early CPR in out‐of‐hospital cardiac arrest. N Engl J Med. 2015;373:1573–1574. [DOI] [PubMed] [Google Scholar]
- 3. Fridman M, Barnes V, Whyman A, Currell A, Bernard S, Walker T, Smith KL. A model of survival following pre‐hospital cardiac arrest based on the Victorian Ambulance Cardiac Arrest Register. Resuscitation. 2007;75:311–322. [DOI] [PubMed] [Google Scholar]
- 4. Fosbol EL, Dupre ME, Strauss B, Swanson DR, Myers B, McNally BF, Anderson ML, Bagai A, Monk L, Garvey JL, Bitner M, Jollis JG, Granger CB. Association of neighborhood characteristics with incidence of out‐of‐hospital cardiac arrest and rates of bystander‐initiated CPR: implications for community‐based education intervention. Resuscitation. 2014;85:1512–1517. [DOI] [PubMed] [Google Scholar]
- 5. Sasson C, Keirns CC, Smith D, Sayre M, Macy M, Meurer W, McNally BF, Kellermann AL, Iwashyna TJ; Group CS . Small area variations in out‐of‐hospital cardiac arrest: does the neighborhood matter? Ann Intern Med. 2010;153:19–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Straney LD, Bray JE, Beck B, Finn J, Bernard S, Dyson K, Lijovic M, Smith K. Regions of high out‐of‐hospital cardiac arrest incidence and low bystander CPR rates in Victoria, Australia. PLoS One. 2015;10:e0139776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ambulance Victoria . The Victorian Cardiac Arrest Registry Annual Report 2014/15. 2015. Available at: http://s3-ap-southeast-2.amazonaws.com/prod.assets.ambulance.vic.gov.au/wp-content/uploads/2016/03/vacar-annual-report-2014-2015.pdf. Accessed 8/2/2016.
- 8. Bray JE, Deasy C, Walsh J, Bacon A, Currell A, Smith K. Changing EMS dispatcher CPR instructions to 400 compressions before mouth‐to‐mouth improved bystander CPR rates. Resuscitation. 2011;82:1393–1398. [DOI] [PubMed] [Google Scholar]
- 9. Anderson ML, Cox M, Al‐Khatib SM, Nichol G, Thomas KL, Chan PS, Saha‐Chaudhuri P, Fosbol EL, Eigel B, Clendenen B, Peterson ED. Rates of cardiopulmonary resuscitation training in the United States. JAMA Intern Med. 2014;174:194–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ro YS, Shin SD, Song KJ, Hong SO, Kim YT, Lee DW, Cho SI. Public awareness and self‐efficacy of cardiopulmonary resuscitation in communities and outcomes of out‐of‐hospital cardiac arrest: a multi‐level analysis. Resuscitation. 2016;102:17–24. [DOI] [PubMed] [Google Scholar]
- 11. Bray JE, Smith K, Case R, Cartledge S, Straney L, Finn J. Public cardiopulmonary resuscitation training rates and awareness of hands‐only cardiopulmonary resuscitation: a cross‐sectional survey of Victorians. Emerg Med Australas. 2017;29:157–164. [DOI] [PubMed] [Google Scholar]
- 12. Tanigawa K, Iwami T, Nishiyama C, Nonogi H, Kawamura T. Are trained individuals more likely to perform bystander CPR? An observational study. Resuscitation. 2011;82:523–528. [DOI] [PubMed] [Google Scholar]
- 13. Nehme Z, Bernard S, Cameron P, Bray JE, Meredith IT, Lijovic M, Smith K. Using a cardiac arrest registry to measure the quality of emergency medical service care: decade of findings from the Victorian Ambulance Cardiac Arrest Registry. Circ Cardiovasc Qual Outcomes. 2015;8:56–66. [DOI] [PubMed] [Google Scholar]
- 14. Perkins GD, Jacobs IG, Nadkarni VM, Berg RA, Bhanji F, Biarent D, Bossaert LL, Brett SJ, Chamberlain D, de Caen AR, Deakin CD, Finn JC, Grasner JT, Hazinski MF, Iwami T, Koster RW, Lim SH, Ma MH, McNally BF, Morley PT, Morrison LJ, Monsieurs KG, Montgomery W, Nichol G, Okada K, Ong ME, Travers AH, Nolan JP, Utstein C. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update of the Utstein resuscitation registry templates for out‐of‐hospital cardiac arrest: a statement for healthcare professionals from a Task Force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian and New Zealand Council on Resuscitation, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Council of Southern Africa, Resuscitation Council of Asia); and the American Heart Association Emergency Cardiovascular Care Committee and the Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation. Resuscitation. 2015;96:328–340. [DOI] [PubMed] [Google Scholar]
- 15. Jacobs I, Nadkarni V, Bahr J, Berg RA, Billi JE, Bossaert L, Cassan P, Coovadia A, D'Este K, Finn J, Halperin H, Handley A, Herlitz J, Hickey R, Idris A, Kloeck W, Larkin GL, Mancini ME, Mason P, Mears G, Monsieurs K, Montgomery W, Morley P, Nichol G, Nolan J, Okada K, Perlman J, Shuster M, Steen PA, Sterz F, Tibballs J, Timerman S, Truitt T, Zideman D; International Liason Committee on Resusitation . Cardiac arrest and cardiopulmonary resuscitation outcome reports: update and simplification of the Utstein templates for resuscitation registries. A statement for healthcare professionals from a Task Force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian Resuscitation Council, New Zealand Resuscitation Council, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Council of Southern Africa). Resuscitation. 2004;63:233–249. [DOI] [PubMed] [Google Scholar]
- 16. Smith KL, Cameron PA, Meyer AD, McNeil JJ. Is the public equipped to act in out of hospital cardiac emergencies? Emerg Med J. 2003;20:85–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Swor R, Khan I, Domeier R, Honeycutt L, Chu K, Compton S. CPR training and CPR performance: do CPR‐trained bystanders perform CPR? Acad Emerg Med. 2006;13:596–601. [DOI] [PubMed] [Google Scholar]
- 18. Straney LD, Bray JE, Beck B, Bernard S, Lijovic M, Smith K. Are sociodemographic characteristics associated with spatial variation in the incidence of OHCA and bystander CPR rates? A population‐based observational study in Victoria, Australia. BMJ Open. 2016;6:e012434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Sasson C, Meischke H, Abella BS, Berg RA, Bobrow BJ, Chan PS, Root ED, Heisler M, Levy JH, Link M, Masoudi F, Ong M, Sayre MR, Rumsfeld JS, Rea TD; American Heart Association Council on Quality of Care and Outcomes Research, Emergency Cardiovascular Care Committee, Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation, Council on Clinical Cardiology, and Council on Cardiovascular Surgery and Anesthesia . Increasing cardiopulmonary resuscitation provision in communities with low bystander cardiopulmonary resuscitation rates: a science advisory from the American Heart Association for healthcare providers, policymakers, public health departments, and community leaders. Circulation. 2013;127:1342–1350. [DOI] [PubMed] [Google Scholar]
- 20. Bergamo C, Bui QM, Gonzales L, Hinchey P, Sasson C, Cabanas JG. TAKE10: a community approach to teaching compression‐only CPR to high‐risk zip codes. Resuscitation. 2016;102:75–79. [DOI] [PubMed] [Google Scholar]
- 21. Blewer AL, Putt ME, Becker LB, Riegel BJ, Li J, Leary M, Shea JA, Kirkpatrick JN, Berg RA, Nadkarni VM, Groeneveld PW, Abella BS; Group CS . Video‐only cardiopulmonary resuscitation education for high‐risk families before hospital discharge: a multicenter pragmatic trial. Circ Cardiovasc Qual Outcomes. 2016;9:740–748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Sayre MR, Berg RA, Cave DM, Page RL, Potts J, White RD; American Heart Association Emergency Cardiovascular Care C . Hands‐only (compression‐only) cardiopulmonary resuscitation: a call to action for bystander response to adults who experience out‐of‐hospital sudden cardiac arrest: a science advisory for the public from the American Heart Association Emergency Cardiovascular Care Committee. Circulation. 2008;117:2162–2167. [DOI] [PubMed] [Google Scholar]
- 23. Abella BS, Aufderheide TP, Eigel B, Hickey RW, Longstreth WT Jr, Nadkarni V, Nichol G, Sayre MR, Sommargren CE, Hazinski MF; American Heart A . Reducing barriers for implementation of bystander‐initiated cardiopulmonary resuscitation: a scientific statement from the American Heart Association for healthcare providers, policymakers, and community leaders regarding the effectiveness of cardiopulmonary resuscitation. Circulation. 2008;117:704–709. [DOI] [PubMed] [Google Scholar]
- 24. Rumsfeld JS, Brooks SC, Aufderheide TP, Leary M, Bradley SM, Nkonde‐Price C, Schwamm LH, Jessup M, Ferrer JM, Merchant RM. Use of mobile devices, social media, and crowdsourcing as digital strategies to improve emergency cardiovascular care: a scientific statement from the American Heart Association. Circulation. 2016;134:e87–e108. [DOI] [PubMed] [Google Scholar]
- 25. Ringh M, Rosenqvist M, Hollenberg J, Jonsson M, Fredman D, Nordberg P, Jarnbert‐Pettersson H, Hasselqvist‐Ax I, Riva G, Svensson L. Mobile‐phone dispatch of laypersons for CPR in out‐of‐hospital cardiac arrest. N Engl J Med. 2015;372:2316–2325. [DOI] [PubMed] [Google Scholar]


