Abstract
Background: Microsurgery is a specialized surgical technique with wide clinical application. The purpose of this study was to analyze case logs of graduating orthopedic surgery residents to assess trends in case volume for microsurgery procedures. Methods: Accreditation Council for Graduate Medical Education case log reports were analyzed for microsurgery experience from 2007 to 2013. The mean number of adult, pediatric, and total microsurgery cases was noted. In addition, the median number of microsurgery procedures performed by the 90th, 50th, and 10th percentiles of residents (by case volume) was recorded. Temporal changes in case volume were calculated utilizing linear regression analyses. Results: The proportion of microsurgery procedures increased significantly (1.3% to 2%; P = .024). The mean number of adult (24.5 to 41.9; P = .01), pediatric (1.9 to 3.4; P = .011), and total (26.3 to 45.3; P = .01) microsurgery procedures also increased significantly. Similarly, residents in both the 90th (63 to 109; P = .01) and 50th (10 to 21; P = .036) percentiles sustained significant increases in the median number of microsurgery procedures. No change was noted for residents in 10th percentile (0 to 0; P > .999). Graduating residents in the 90th percentile performed over 6 times more microsurgery procedures than residents in the 50th percentile. Conclusions: Microsurgical caseload is increasing among graduating orthopedic residents. However, there is substantial variability in resident microsurgery case volume. Future investigations are needed to explore the educational implications of these findings and should seek to correlate microsurgical caseload with competency.
Keywords: caseload, education, microsurgery, resident, variation
Introduction
Microsurgery is a specialized technique utilized in many areas of modern surgery with wide clinical application.11 It involves manipulation of very small caliber structures, requiring precise surgical technique and refined operative principles.13 Among orthopedic surgeons, microsurgery is often used when performing nerve grafting and repair, free tissue transfers, and replantation of digits or extremities.7 Although typically utilized by hand surgeons, adeptness in microsurgery is of use to the orthopedic resident. In addition to improving macrosurgical skill and technique, microsurgical exposure during residency training may also impact career choices among residents.4,8
Reports in the orthopedic literature have identified procedural case volume as being a key component in the training of orthopedic residents.14 Case volume is also thought to be representative of resident competency.10 However, an assessment of microsurgical caseload during orthopedic residency training has not been performed. The purpose of this study was to assess trends in resident case volume for microsurgery procedures and to assess caseload variation among residents. We hypothesized that considerable discrepancies subsist among residents regarding microsurgery case volume.
Methods
Accreditation Council for Graduate Medical Education (ACGME) case log reports were analyzed for microsurgery experience from 2007 to 2013 for graduating orthopedic surgery residents.2 All cases designated as microsurgery procedures utilized a microscope for nerve or vessel repair. Primary or supervising resident surgeon cases as well as assisting resident surgeon cases were included in the case log reports.1 ACGME case log reports for orthopedic surgery residency programs are presented annually and include data from graduating orthopedic surgery residents, representing procedural caseload from their entire residency experience. Only resident cases of ACGME accredited orthopedic surgery residencies are featured in the annual reports. ACGME accreditation of orthopedic surgery residencies necessitates the meeting of a standardized set of ACGME requirements. These include, but are not limited to, having at least 3 American Board of Orthopaedic Surgery (ABOS) certified faculty members devoting a minimum of 20 hours per week to the program as well as at least 1 full-time ABOS certified faculty member devoting a minimum of 45 hours per week to the program.3
The mean number of adult, pediatric, and total microsurgery cases as well as the total number of orthopedic cases was reviewed. The mean number of graduating orthopedic residents and orthopedic residencies was also noted. In addition, the median number of microsurgery procedures performed by the 90th, 50th, and 10th percentiles of graduating residents (by case volume) was recorded. Changes in case volume and the proportion of microsurgery cases over time were calculated utilizing linear regression analyses. A P value less than .05 indicated the level of significance.
Results
From 2007 to 2013, there was a significant increase in the number of graduating orthopedic residents (616 to 678; P < .001). During this 7-year period, the number of orthopedic residencies increased slightly (149 to 150; P = .38). The mean number of all orthopedic cases performed by graduating orthopedic residents increased significantly (1952.7 to 2291.4; P = .001). The proportion of microsurgery procedures among all cases performed by graduating orthopedic residents also increased significantly (1.3% to 2%; P = .024). The mean number of adult (24.5 to 41.9; P = .01) and pediatric (1.9 to 3.4; P = .011) microsurgery procedures performed by graduating residents increased significantly. Similarly, the mean number of all microsurgery procedures performed by graduating residents increased significantly (26.3 to 45.3; P = .01) (Table 1).
Table 1.
Mean Number of Adult, Pediatric, and Total Microsurgery Procedures as well as the Proportion of Microsurgery Procedures Performed Among All Orthopaedic Procedures per Graduating Resident From 2007 to 2013.
| Graduating year | Adult microsurgeries | Pediatric microsurgeries | Total microsurgeries | Proportion of microsurgeries per graduating resident |
|---|---|---|---|---|
| 2007 | 24.5 | 1.9 | 26.3 | 1.3% |
| 2008 | 24.2 | 1.9 | 26 | 1.4% |
| 2009 | 23.8 | 2.1 | 25.8 | 1.3% |
| 2010 | 25.4 | 2 | 27.4 | 1.3% |
| 2011 | 29 | 2.3 | 31.4 | 1.5% |
| 2012 | 33.4 | 2.6 | 36 | 1.6% |
| 2013 | 41.9 | 3.4 | 45.3 | 2% |
| P Value | .01 | .011 | .01 | .024 |
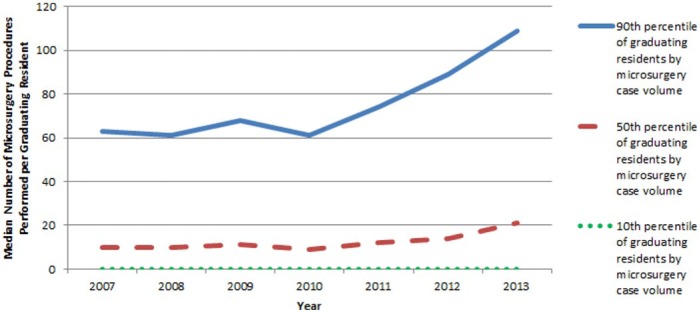
Subgroup analysis revealed that residents in the 90th percentile of case volume experienced a significant increase in the median number of microsurgery procedures performed from 2007 to 2013 (63 to 109; P = .01). Similarly, graduating residents in the 50th percentile of case volume sustained a significant increase in the median number of microsurgery procedures (10 to 21; P = .036). However, microsurgery caseload for graduating residents in the 10th percentile of case volume remained unchanged during the study period (0 to 0; P > .999) (Figure 1). On average, graduating residents in the 90th percentile performed 75 microsurgery cases, residents in the 50th percentile performed 12.4 microsurgery cases, and residents in the 10th percentile performed no microsurgery cases.
Figure 1.
Chart demonstrating the median number of microsurgery procedures performed per graduating resident in the 90th, 50th, and 10th percentiles of case volume from 2007 to 2013.
Discussion
The results of this study indicate that microsurgical case volume is increasing among graduating orthopedic residents. The mean number of microsurgery cases per graduating resident increased 72% over the 7-year period with the proportion of microsurgery cases among all orthopedic cases increasing as well. Similarly, adult and pediatric microsurgery cases were found to have increased by 71% and 79%, respectively. Increased microsurgery caseload among orthopedic residents may be due to an increase in the amount of hand call orthopedic hand surgeons take versus plastic surgery hand surgeons. However, a direct comparison of attending hand call and caseload between orthopedic hand surgeons and plastic surgery hand surgeons would be needed to verify this association.
Our findings of increasing microsurgery caseload among residents were in contrast to decreasing case volume trends reported by hand surgeons in the community. Payatakes et al surveyed members of American Society for Surgery of the Hand regarding current microsurgery practices with respondents reporting a decline in caseload over the past decade.12 It is likely that microsurgery has shifted toward being performed at academic centers where resident training takes place, and both resources and staff are better geared for support.
Caseload growth in the current study was concentrated among graduating orthopedic residents in the 90th and 50th percentiles of case volume with microsurgery caseload increases of 73% and 110%, respectively. There was no change in case volume among graduating orthopedic residents in the 10th percentile of case volume. However, microsurgery case volume was found to be highly variable among residents. Graduating residents in the 90th percentile of case volume performed over 500% more microsurgery cases than graduating residents in the 50th percentile. This case volume variability is likely due to several factors. Resident microsurgery case volume may be affected by the number of orthopedic residents in a given program and the duration of the rotation wherein microsurgery training takes place (eg, hand surgery rotation). Moreover, work hour restrictions may limit the number of cases available to trainees.16 The clinical interests of residents may also impact microsurgery caseload, particularly during the senior resident years when there may be more independence in selecting cases. In addition, each attending surgeon’s microsurgery caseload will expectedly impact the number of cases seen by residents during training.
Microsurgery has achieved widespread utilization across surgical specialties and has emerged as an important component of clinical care.15 Despite this importance, education in the required skills and techniques has proven to be complex. Clinical assessment of microsurgical technique necessitates objective scores of skills, skill acquisition, and skill maintenance.5 The equipoise of maintaining quality patient care while simultaneously facilitating resident education is a notably frequent challenge and likely influences resident caseload. In addition, financial constraints have pressured surgeons to reduce operative durations, resulting in further truncated resident learning opportunities.13
Although the educational impact of microsurgery caseload variability is unknown, one potential area for future educational focus to reduce potential negative effects of comparatively low microsurgery caseload includes the use of microsurgery simulators. Gould described the benefit of microsurgery laboratory simulations in improving teaching, research, and clinical support in orthopedic residency programs.6 A recent study confirmed these sentiments by reporting improved orthopedic resident microsurgical skills after institution of a microvascular surgery training curriculum consisting of regular one-on-one laboratory teaching sessions.7 Loh et al also described a do-it-yourself home microsurgery simulator to combat financial and temporal pressures which may prohibit clinical experience.9 Although microsurgery simulation cannot replace operative caseload, the literature indicates that it may serve as a valuable compliment to clinical experience.
This study has certain limitations. First, poor resident recall and varying levels of resident participation in cases may result in underreporting or overreporting of caseload. Second, the ACGME case logs of summarized data may not be representative of microsurgery case volume for individual residency programs or residents. Third, ACGME case log reports do not differentiate between the types of microsurgery performed which may be prohibitive in drawing definitive conclusions regarding specific microsurgery procedures. Last, the findings of our study may be affected by changes in the way residents report caseload. Some residents may pursue and document cases with the goal of achieving high caseload status and may comprise their academic enrichment in the process.
On the basis of our findings, we conclude that microsurgical case volume is increasing among graduating orthopedic residents with growth concentrated among residents in the 90th and 50th percentiles of case volume. However, substantial variability in resident microsurgery case volume was noted. Additional investigations are needed to explore the educational implications of these findings and should include quantitative correlation of resident microsurgical case volume with clinical competency.
Footnotes
Ethical Approval: This study was approved by our institutional review board.
Statement of Human and Animal Rights: This article does not contain any studies with human or animal subjects.
Statement of Informed Consent: Informed consent was not applicable to this study design as case log data is made publicly available by the Accreditation Council for Graduate Medical Education.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Accreditation Council for Graduate Medical Education. ACGME orthopaedic surgery case logs guidelines. http://www.acgme.org/acgmeweb/portals/0/pfassets/programresources/260_case_log_guidelines.pdf. Published 2014. Accessed March 12, 2015.
- 2. Accreditation Council for Graduate Medical Education. ACGME orthopaedic surgery case logs national data report. https://www.acgme.org/acgmeweb/Portals/0/ORSNatData1213.pdf. Published 2013. Accessed March 12, 2015.
- 3. Accreditation Council for Graduate Medical Education. ACGME program requirements for graduate medical education in orthopaedic surgery. https://www.acgme.org/Portals/0/PFAssets/ProgramRequirements/260_orthopaedic_surgery_2016.pdf. Published 2016. Accessed August 28, 2016.
- 4. Di Cataldo A, Li Destri G, Trombatore G, et al. Usefulness of microsurgery in the training of the general surgeon. Microsurgery. 1998;18(8):446-448. [DOI] [PubMed] [Google Scholar]
- 5. Ghanem AM, Hachach-Haram N, Leung CC, et al. A systematic review of evidence for education and training interventions in microsurgery. Arch Plast Surg. 2013;40(4):312-319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Gould SH. The role of the microsurgical laboratory in orthopedic training programs. Orthopedics. 1986;9(6):881-882. [DOI] [PubMed] [Google Scholar]
- 7. Ko JW, Lorzano A, Mirarchi AJ. Effectiveness of a microvascular surgery training curriculum for orthopaedic surgery residents. J Bone Joint Surg Am. 2015;97(11):950-955. [DOI] [PubMed] [Google Scholar]
- 8. Lin TS, Chiang YC. Correlation between microsurgical course performance and future surgical training selection by intern and junior residents. Microsurgery. 2008;28(3):171-172. [DOI] [PubMed] [Google Scholar]
- 9. Loh CY, Tiong VT, Loh AY, et al. Microsurgery training—a home do-it-yourself model. Microsurgery. 2014;34(5):417-418. [DOI] [PubMed] [Google Scholar]
- 10. Malangoni MA, Biester TW, Jones AT, et al. Operative experience of surgery residents: trends and challenges. J Surg Educ. 2013;70(6):783-788. [DOI] [PubMed] [Google Scholar]
- 11. Myers SR, Froschauer S, Akelina Y, et al. Microsurgery training for the twenty-first century. Arch Plast Surg. 2013;40(4):302-303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Payatakes AH, Zagoreos NP, Fedorcik GG, et al. Current practice of microsurgery by members of the American Society for Surgery of the Hand. J Hand Surg Am. 2007;32(4):541-547. [DOI] [PubMed] [Google Scholar]
- 13. Ramachandran S, Ghanem AM, Myers SR. Assessment of microsurgery competency-where are we now? Microsurgery. 2013;33(5):406-415. [DOI] [PubMed] [Google Scholar]
- 14. Robbins L, Bostrom M, Craig E, et al. Proposals for change in orthopaedic education: recommendations from an orthopaedic residency directors’ peer forum. J Bone Joint Surg Am. 2010;92(1):245-249. [DOI] [PubMed] [Google Scholar]
- 15. Tsai TM, Breyer JM, Panattoni JB. History of microsurgery: curiosities from the sixties and seventies. Microsurgery. 2013;33(2):85-89. [DOI] [PubMed] [Google Scholar]
- 16. Watson DR, Flesher TD, Ruiz O, et al. Impact of the 80-hour workweek on surgical case exposure within a general surgery residency program. J Surg Educ. 2010;67(5):283-289. [DOI] [PubMed] [Google Scholar]