Abstract
Background: Volar plate fixation of distal radius fractures can result in soft tissue injuries. Abnormal contour of the dorsal cortex of the distal radius provides difficulties in discerning screw penetration on standard radiographs. The skyline and carpal shoot-through views are additional views to improve dorsal cortex visibility. We report on the sensitivity and specificity of determining screw protrusion with these views. Methods: Seven fresh frozen cadavers were instrumented with a distal radius volar locking plate. Initial screw length was determined by depth gauge measurement. A dorsal dissection of the wrist was performed to detect screw penetration. Protruding screws were documented and replaced with screws of the appropriate length and deemed as baseline. Screws were then sequentially lengthened by 2 and 4 mm. Skyline and carpal shoot-through views were obtained at baseline, 2 mm, and 4 mm. The images were randomized and compiled into an untimed survey asking orthopedic surgeons to determine whether screws were penetrating through the dorsal cortex. Results: Based on depth gauge measurements, 4 out of 44 (9.1%) volar plate locking screws penetrated the dorsal cortex, as confirmed with dorsal dissection. Sensitivities for the skyline and carpal shoot-through views were 75% and 86% (P ≤ .001), respectively, for 2-mm protrusions, and 76% and 89% (P ≤ .001), respectively, for 4-mm screw protrusions. Specificities were 85% and 84% for the skyline and shoot-through views, respectively. Conclusions: We believe that the carpal shoot-through view has utility and can be implemented to augment standard intraoperative views, and may decrease the incidence of screw protrusion resulting in soft tissue injuries.
Keywords: skyline view, carpal shoot-through view, volar plate fixation, distal radius fracture
Introduction
Operative fixation of distal radius fractures is performed more frequently in today’s practice, with the incidence of open reduction internal fixation (ORIF) increasing significantly since the advent of volar locking plates.3 Volar locking plates can achieve an anatomic reduction even in the setting of comminution and the most dorsally displaced distal radius fractures.9 Dorsal plate fixation is another option for surgical management of distal radius fractures. This technique has fallen out of favor secondary to increased complications arising from plate contact with the extensor tendons, resulting in tendonitis and tendon rupture.2,12,13
Although volar plate fixation is the preferred surgical treatment, extensor tendon complications still occur. Extensor tendon complications from volar plating most commonly result from technical errors, such as screw penetration through the dorsal cortex or drill plunging, with a reported incidence of 2% to 7%.1,14,15 These technical mishaps may be attributed to a variety of factors. Increased comminution may impede the ability of the depth gauge to accurately determine screw length, therefore increasing the need for intraoperative fluoroscopy for better visualization of the dorsal cortex. Even with fluoroscopy, bony irregularities of the dorsal cortex often make it difficult to discern penetrating screws. Lister’s tubercle has been reported to further hinder detection of screw protrusion through distal locking plate holes where the extensor pollicis longus (EPL) tendon is most vulnerable to injury and often goes undetected with standard lateral views.4,5,7,10,11,16
A number of fluoroscopic views have been described to increase the ability to detect dorsal cortex screw penetration.4-6,8,10,11 The skyline view and carpal shoot-through views have been developed to increase visibility of the dorsal cortex. These views place the arm in supination with elbow flexion of approximately 70° to 75° (15°-20° inclination from vertical). Views differ from each other by the position of the wrist. The skyline view palmar flexes at the wrist, whereas the carpal shoot-through view dorsiflexes at the wrist, providing visibility of the dorsal cortex.6,11
In this cadaveric study, we attempt to achieve 2 goals: (1) determination of the accuracy of using the depth gauge independently to measure the appropriate screw length; and (2) determination of the specificity and sensitivity of using the skyline and carpal shoot-through views intraoperatively to detect screw penetration through the dorsal cortex.
Materials and Methods
Seven fresh frozen human cadaver specimens from 6 different donors without gross evidence of wrist or forearm abnormalities were used. Upon receipt, the specimens were stored at −20°C and thawed at room temperature for 24 hours prior to instrumentation.
Surgical Technique
Volar plate fixation of the wrist was performed through the Henry approach to the distal radius using the Acu-Loc 2 Volar Distal Radius (VDR) plating system (Acumed, Hillsboro, OR) per manufacturer-recommended surgical guidelines. Specimens were instrumented with a standard (6 distal holes) or wide (7 distal holes) locking plate using 2.3-mm-diameter screws. Plate size was chosen based on the size and contour of each specimen’s distal radius. Appropriate screw length was determined by the depth gauge provided in the manufacturer’s surgical instrumentation tray. Each screw length was measured twice, and the shortest measured screw length was chosen.
Following instrumentation, a dorsal dissection (Figure 1) of the wrist to expose the dorsal surface of the distal radius was performed. Screws penetrating through the dorsal cortex were documented and changed to the appropriate screw length to ensure that the screw was flush and not protruding through the dorsal cortex. Proper screw length confirmed by dorsal dissection was deemed as baseline. Thereafter, screws in hole positions 3 and 4 (Figure 2) were sequentially lengthened by 2 and 4 mm above baseline.
Figure 1.

Gross dorsal dissection of the distal radius showing baseline screw lengths.
Figure 2.

Acu-Loc 2 volar distal radius plate screw positions 3 and 4 (arrows) that were sequentially lengthened by 2 and 4 mm.
Screw hole positions 3 and 4 were determined to place the EPL tendon at greatest risk for injury based on our pilot investigation, where we placed Kirschner wires (K-wires) in the distal hole positions of an Acu-Loc 2 VDR plate instrumented in a cadaver radius. A dorsal dissection of the distal radius provided direct visualization of where proud screws would come in contact with the tendon (Figure 3).
Figure 3.
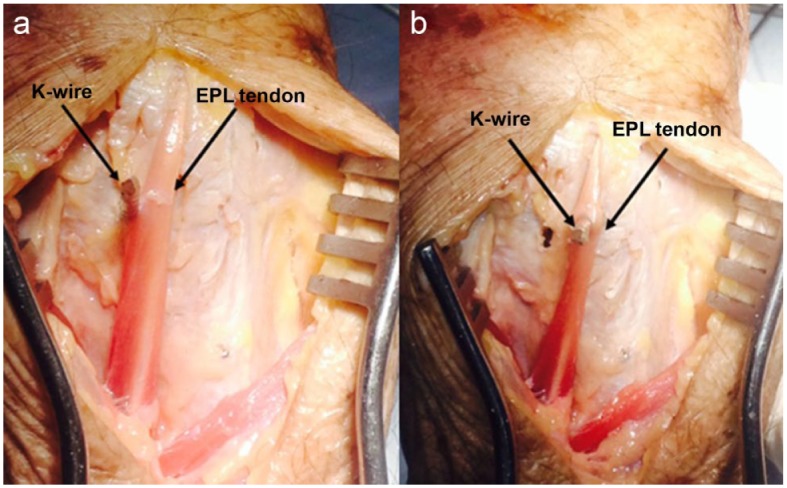
a, Gross dorsal dissection showing a K-wire placed through hole position 4 of the VDR plate coming in contact with the EPL tendon. b, Gross dorsal dissection showing K-wire placed through hole position 3 of the VDR plate penetrating the EPL tendon.
Note. K-wire = Kirschner wire; VDR = volar distal radius; EPL = extensor pollicis longus.
Radiographic Assessment
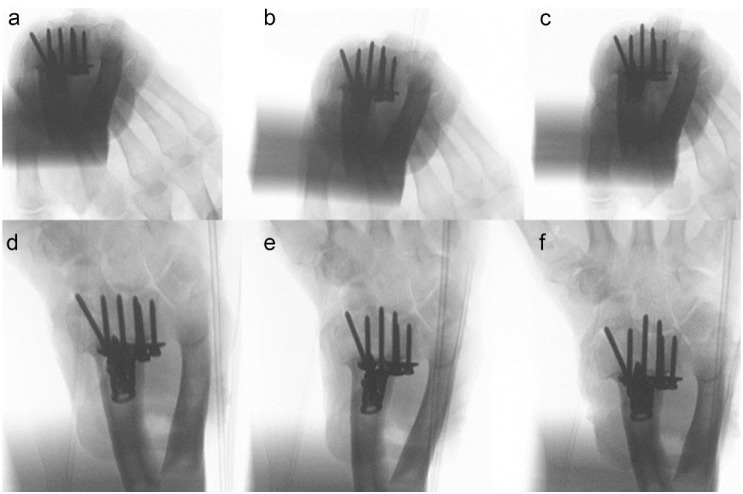
Skyline and carpal shoot-through fluoroscopic views were taken at baseline, 2 mm, and 4 mm screw length increments (Figure 4). To obtain the skyline view of the distal radius, the arm was supinated with elbow flexion at 70° (20° inclination from vertical), with the wrist palmar flexed at 75° (Figure 5a).11 The carpal shoot-through view placed the arm in supination and elbow flexion of approximately 70° (20° inclination from vertical), with the wrist in 70° of dorsiflexion (Figure 5b).6 To ensure consistency and accuracy of arm placement, a radiolucent support base was utilized.
Figure 4.
a, Skyline view of baseline screw lengths. b, Skyline view of 2-mm screw protrusions. c, Skyline view of 4-mm screw protrusion. d, Carpal Shoot-through view of baseline screw lengths. e, Carpal shoot-through view of 2-mm screw protrusions. f, Carpal shoot-through view of 4-mm screw protrusion.
Figure 5.
a, Intraoperative illustration of skyline view. b, Intraoperative illustration of carpal shoot-through view.
Survey Analysis
Fluoroscopic images were compiled in random order and formatted into a commercially available survey (SurveyMonkey Inc, Palo Alto, California). Emails were sent to orthopedic surgeons inviting them to participate in the survey. This untimed survey included a brief orientation describing each view. The radiographs were labeled with arrows identifying the screw positions that we had changed and asked participants to determine whether the screws were penetrating through the dorsal cortex of the distal radius. Surveys were collected and analyzed.
Statistical Analysis
Sensitivities for each view were determined for screws protruding 2 and 4 mm through the dorsal cortex. Specificity was determined using the baseline screw lengths for each view. A contingency matrix was created using survey data to calculate the sensitivities and specificities along with their 95% confidence intervals (CIs) for the skyline and carpal shoot-through views. A chi-square analysis was used to compare differences between the skyline and carpal shoot-through views, using a significance level of α = 0.05.
Results
Depth Gauge Measurements
The distal radius of 7 (4 left and 3 right) fresh frozen cadaver arms was instrumented. Five specimens were instrumented with a standard locking plate, and 2 specimens were instrumented with wide locking plates. Using a depth gauge to determine screw length, a total of 44 locking screws were placed in the distal hole positions of the volar plates. Four out of 44 (9.1%) screws were found to be protruding through the dorsal cortex upon gross dorsal dissection. Protruding screws required on average 2 mm of shortening to achieve baseline lengths.
Survey Results
Sixty-four orthopedic surgeons participated in the survey. Surgeon experience ranged from residents/fellows (26.5%), general orthopedic surgeons (35.9%), to fellowship-trained hand surgeons (37.5%). Sensitivities for detecting 2-mm protrusions were 75% (95% CI, 0.70-0.80) and 86% (95% CI, 0.82-0.90), P ≤ .001, for skyline and carpal shoot-through views, respectively. Sensitivities for detecting 4-mm protrusions were 76% (95% CI, 0.71-0.81) and 89% (95% CI, 0.85-0.92), P ≤ .001, for skyline and carpal shoot views, respectively. The specificities for skyline and carpal shoot-through views were 85% (95% CI, 0.80-0.88) and 84% (95% CI, 0.80-0.88), P = .84, respectively.
Discussion
Irregularities of the dorsal cortex of the distal radius can make it difficult to detect screw prominence into the adjacent soft tissues when using volar plate fixation for distal radius fractures. Surgeons often use depth gauge measuring devices and various fluoroscopic views to prevent excessive screw lengths as a means to lessen the incidence of soft tissue injury. We investigated the accuracy of the depth gauge as well as the utility of the skyline and carpal shoot-through fluoroscopic views. We found that, when relying only on the depth gauge to determine proper screw length, approximately 9.1% of locking screws placed in the volar plate were too long and protruded into soft tissues. Dolce et al4 reported similar results in their study with 9.4% of screws penetrating through the dorsal cortex after initial measurement and placement. Extensive comminution may further decrease the accuracy of the depth gauge. As the cadaveric specimens used in our study did not have distal radius fractures, our results may overestimate the accuracy of the depth gauge in the setting of comminution. These findings further support the need for better visualization of the dorsal cortex to confirm that the screws are in a safe position.
The clinical challenge to date has been obtaining fluoroscopic views that adequately show the dorsal cortex of the distal radius. Standard lateral views have been reported to be less accurate at detecting screw penetration.4 Therefore, the skyline and carpal shoot-through views have been described to provide additional visualization of the dorsal cortex. Several studies have looked at the utility of using the skyline view. Riddick et al11 compared the skyline view with the lateral and pronated oblique views and found that the skyline view had an overall sensitivity of 83% compared with 77% and 51% for the pronated oblique and lateral views, respectively.
The one shortcoming of the skyline view is the potential for overexposure of the image, as the image intensifier has difficulty regulating radiation dose based on perceived density.6 This is thought to be attributed to the palmar flexion at the wrist. We also found this to be a challenge, and noted that more images were needed to obtain an acceptable skyline view compared with the carpal shoot-through view. The carpal shoot-through view attempts to eliminate this by dorsiflexing at the wrist. We found the carpal shoot-through view to be more sensitive at detecting 2- and 4-mm screw penetration through the dorsal cortex compared with the skyline view.
Our study had some limitations. We found that there is a learning curve with interpreting the skyline and carpal shoot-through radiographs. Many of the surgeons participating in this survey may not have had extensive experience with these views. We attempted to address this limitation with a brief orientation at the beginning of the survey. However, we believe this study captures the broad range of orthopedic surgeons who treat distal radius fractures in the orthopedic community.
At the conclusion of this study, we were able to determine sensitivity and specificity for the carpal shoot-through view, which, to our knowledge, has not been reported in the literature. Importantly, we were able to obtain these results based on screw positions that place the EPL tendon at risk for injury. Based on our findings, we believe that the carpal shoot-through can be used as an adjunct to standard intraoperative views to detect screw penetration through the dorsal cortex, and may decrease the incidence of EPL tendon injuries.
Acknowledgments
The authors would like to thank Jeremy Kalma for his graphic and technical contributions to this study.
Footnotes
Ethical Approval: Institutional review board (IRB) approval was not needed because living human subjects were not used in this study.
Statement of Human and Animal Rights: This article does not contain any studies with human or animal subjects.
Statement of Informed Consent: Informed consent was obtained when necessary.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Arora R, Lutz M, Hennerbichler A, et al. Complications following internal fixation of unstable distal radius fracture with a palmar locking-plate. J Orthop Trauma. 2007;21(5):316-322. [DOI] [PubMed] [Google Scholar]
- 2. Chiang PP, Roach S, Baratz ME. Failure of a retinacular flap to prevent dorsal wrist pain after titanium Pi plate fixation of distal radius fractures. J Hand Surg Am. 2002;27(4):724-728. [DOI] [PubMed] [Google Scholar]
- 3. Chung KC, Shauver MJ, Birkmeyer JD. Trends in the United States in the treatment of distal radial fractures in the elderly. J Bone Joint Surg Am. 2009;91(8):1868-1873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Dolce D, Goodwin D, Ludwig M, et al. Intraoperative evaluation of dorsal screw prominence after polyaxial volar plate fixation of distal radius fractures utilizing the Hoya view: a cadaveric study. Hand (N Y). 2014;9(4):511-515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Lee SK, Bae KW, Choy WS. Use of the radial groove view intra-operatively to prevent damage to the extensor pollicis longus tendon by protruding screws during volar plating of a distal radial fracture. Bone Joint J. 2013;95-B(10):1372-1376. [DOI] [PubMed] [Google Scholar]
- 6. Marsland D, Hobbs CM, Sauve PS. Volar locking plate fixation of distal radius fractures: use of an intra-operative “carpal shoot through” view to identify dorsal compartment and distal radioulnar joint screw penetration. Hand (N Y). 2014;9(4):516-521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Maschke SD, Evans PJ, Schub D, et al. Radiographic evaluation of dorsal screw penetration after volar fixed-angle plating of the distal radius: a cadaveric study. Hand (N Y). 2007;2(3):144-150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Matullo KS, Dennison DG. Lateral tilt wrist radiograph using the contralateral hand to position the wrist after volar plating of distal radius fractures. J Hand Surg Am. 2010;35(6):900-904. [DOI] [PubMed] [Google Scholar]
- 9. Orbay JL, Fernandez DL. Volar fixation for dorsally displaced fractures of the distal radius: a preliminary report. J Hand Surg Am. 2002;27(2):205-215. [DOI] [PubMed] [Google Scholar]
- 10. Ozer K, Wolf JM, Watkins B, et al. Comparison of 4 fluoroscopic views for dorsal cortex screw penetration after volar plating of the distal radius. J Hand Surg Am. 2012;37(5): 963-967. [DOI] [PubMed] [Google Scholar]
- 11. Riddick AP, Hickey B, White SP. Accuracy of the skyline view for detecting dorsal cortical penetration during volar distal radius fixation. J Hand Surg Eur Vol. 2012;37(5):407-411. [DOI] [PubMed] [Google Scholar]
- 12. Ring D, Jupiter JB, Brennwald J, et al. Prospective multicenter trial of a plate for dorsal fixation of distal radius fractures. J Hand Surg Am. 1997;22(5): 777-784. [DOI] [PubMed] [Google Scholar]
- 13. Rozental TD, Beredjiklian PK, Bozentka DJ. Functional outcome and complications following two types of dorsal plating for unstable fractures of the distal part of the radius. J Bone Joint Surg Am. 2003;85-A(10):1956-1960. [DOI] [PubMed] [Google Scholar]
- 14. Rozental TD, Blazar PE. Functional outcome and complications after volar plating for dorsally displaced, unstable fractures of the distal radius. J Hand Surg Am. 2006;31(3):359-365. [DOI] [PubMed] [Google Scholar]
- 15. Tarallo L, Mugnai R, Zambianchi F, et al. Volar plate fixation for the treatment of distal radius fractures: analysis of adverse events. J Orthop Trauma. 2013;27(12): 740-745. [DOI] [PubMed] [Google Scholar]
- 16. Thomas AD, Greenberg JA. Use of fluoroscopy in determining screw overshoot in the dorsal distal radius: a cadaveric study. J Hand Surg Am. 2009;34(2):258-261. [DOI] [PubMed] [Google Scholar]