Abstract
Background: The development of Complex Regional Pain Syndrome (CRPS) represents a potentially devastating complication following carpal tunnel release. In the presence of a suspected incomplete release of the transverse carpal ligament or direct injury to the median nerve, neurolysis as well as nerve coverage to prevent recurrent scar has been shown to be effective. Methods: Retrospective chart review and telephone interview was conducted for patients who underwent abductor digiti minimi flap coverage and neurolysis of the median nerve for CRPS following carpal tunnel release. Results: Fourteen wrists in 12 patients were reviewed. Mean patient age was 64 years (range, 49-83 years), and the mean follow-up was 44 months. Carpal tunnel outcome instrument scores were 47.4 ± 6.8 preoperatively and 27.1 ± 10.6 at follow-up (P < .001). Quick Disabilities of the Arm, Shoulder, and Hand (QuickDASH) scores at follow-up were 29.4 ± 26. No significant postoperative complications were identified. Conclusions: The abductor digiti minimi flap is a reliable option with minimal donor site morbidity. It provides predictable coverage when treating CRPS following carpal tunnel syndrome.
Keywords: carpal tunnel syndrome, abductor digiti minimi flap, complex regional pain syndrome, median nerve, revision carpal tunnel surgery
Introduction
Carpal tunnel release (CTR) is one of the most common procedures performed in the upper limb. A small subset of patients, however, may have persistent symptoms or develop complex regional pain syndrome (CRPS), a known complication of CTR.1,12
Complete rerelease of the transverse carpal ligament and neurolysis for recurrent carpal tunnel syndrome associated with CRPS may not be sufficient to prevent new scar formation or to relieve the complications of allodynia and hyperesthesia.11,20 In a blinded study comparing successful CTR and patients with recurrence of symptoms, significantly more fibrosis and nerve enhancement was seen on magnetic resonance imaging (MRI) in the latter group.2 Interposition of well-vascularized soft tissue may be beneficial in cases of recurrent carpal tunnel syndrome.
Several techniques have been described to provide increased soft tissue coverage in repeat CTR. These include hypothenar fat flap, abductor digiti minimi (ADM) flap, sublimis turn down flap, pronator quadratus muscle flap, fascial or fasciocutaneous flaps, synovial tissue transposition, vein wrapping, or free flap including omentum.3,5-9,14,15,17,18,21 Each technique has unique advantages and disadvantages that guide the surgeon’s decision.
The ADM flap has several advantages over other soft tissue coverage options in treating recurrent carpal tunnel syndrome including the length of the flap, the proximity to the median nerve, the ability to provide coverage distal to the wrist crease, predictable anatomy, and minimal donor site morbidity. We describe the use of the ADM flap to provide soft tissue coverage around the median nerve in cases of recurrent carpal tunnel syndrome and in the setting of CRPS.
Methods
From 1996 to 2014, 16 patients (18 cases) with CRPS following CTR were treated with repeat open CTR and ADM flap by the senior author (J.B.J.). Retrospective chart review was performed for patient demographics, comorbidities, electrodiagnostic investigations, operative findings, and postoperative complications. Patients were contacted by telephone for follow-up evaluation including administration of the Carpal Tunnel Outcomes Instrument (CTOI)13 and the Quick Disabilities of the Arm, Shoulder, and Hand score (QuickDASH).4 Patients were asked to rate improvement following surgery: if they would have the surgery again and to assign themselves postoperative grades. These 4 grades consisted of: (1) “severe pain with hand function resulting in inability to perform daily activities;” (2) “moderate pain significantly limiting work and limiting activities;” (3) “mild or occasional pain with hand function but able to work and to perform all daily activities;” and (4) “no pain with wrist flexion or extension or palpation of the wrist and able to work without pain.” Pain was also assessed on an ordinal scale from 1 to 10.
Statistical analysis was performed using a 2-tailed Student t test for continuous variables. P < .05 was considered statistically significant.
Surgical Technique
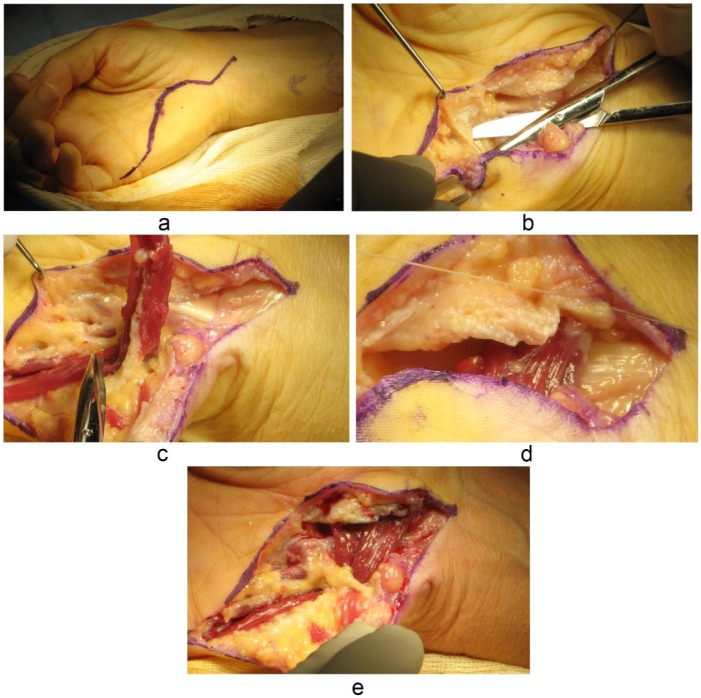
The surgical technique is similar to the approach originally described in 1921 by Huber.10 A volar incision is made through the previous surgical scar with extension on to the volar forearm, proximal to the transverse carpal ligament (Figure 1a). The median nerve is identified outside the zone of previous scar, and neurolysis is performed under high-powered loupe or microscope magnification. The incision is then extended distally to the ulnar aspect of the small finger to expose the hypothenar musculature (Figure 1b). The ADM is identified, disinserted from its insertion at the ulnar base of the proximal phalanx, and elevated from distal to proximal, preserving the proximal pedicle (Figure 1c). The ADM is then transposed to provide soft tissue coverage over the median nerve. Once in place, the muscle is sutured to the radial aspect of the transverse carpal ligament (Figures 1d and 1e). The skin and subcutaneous tissues are closed in layers in the normal fashion.
Figure 1.
a, An incision is made starting along the distal forearm over the median nerve and includes the prior incision. b, Following neurolysis of the median nerve, the ADM is identified, c, ADM is elevated while maintaining its proximal pedicle, d, ADM is transposed over the median nerve and sutured to the radial aspect of the transverse carpal ligament, and e, final position of the ADM providing soft tissue coverage over the median nerve.
Note. ADM = abductor digiti minimi.
Results
Of the 16 patients (18 cases) who underwent revision CTR and ADM flap reconstruction, 12 patients (14 cases) agreed to participate in telephone follow-up. Three patients were unreachable for follow-up, and 1 patient declined to participate. Patient demographics are summarized in Table 1. Mean age at the time of surgery was 64.5 ± 11.7 years, and 58% (7 patients) were female. Mean follow-up from the time of surgery was 44 months. All patients had at least 1 previous CTR; 4 patients had 2 prior surgeries. Diabetes was present in 33% of patients. Three patients were Worker’s compensation cases.
Table 1.
Patient Demographics.
| Patient | Age at surgery | Gender | Side | Hand dominance | Previous surgery | Comorbidity | WCB | Occupation | Duration of follow-up (months) |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 50 | M | R | RHD | Bilateral CTR | Asthma | y | Sheet metal worker, unemployed | 4 |
| 50 | M | L | RHD | Bilateral CTR | Asthma | y | Sheet metal worker, unemployed | 11 | |
| 2 | 73 | F | R | RHD | 2 prior: endoscopic and open CTR | T2DM, HTN | Self-employed driver | 60 | |
| 3 | 58 | M | L | RHD | CTR ×2 | CAD, ulnar brachial plexopathy | y | Financial officer | 58 |
| 4 | 83 | F | R | RHD | CTR | T2DM, HTN, Afib | n | Retired | 26 |
| 5 | 67 | M | R | RHD | CTR | n | Director of education | 17 | |
| 6 | 52 | F | L | RHD | CTR ×2 | GERD | n | On disability for other issue | 12 |
| 7 | 63 | M | R | RHD | CTR | T2DM, OA | n | Self-employed plumber | 10 |
| 8 | 57 | F | R | RHD | CTR | T2DM | n | Nurse | 170 |
| 9 | 73 | M | L | CTR | CAD, gout, Afib, OSA | n | Retired | 22 | |
| 10 | 82 | F | L | RHD | Endoscopic CTR | HTN | n | 20 | |
| 11 | 49 | M | R | LHD | Bilateral CTR | y | Autotechnician, on disability | 72 | |
| 49 | M | L | LHD | Bilateral CTR | y | Autotechnician, on disability | 80 | ||
| 12 | 67 | F | R | RHD | CTR | n | Homemaker | 60 |
Note. WCB = Worker’s Compensation Board; RHD = right hand dominant; CTR = carpal tunnel release; T2DM = type 2 diabetes; HTN = hypertension; CAD = coronary artery disease; Afib = atrial fibrillation; GERD = gastric reflux; OA = osteoarthritis; OSA = obstructive sleep apnea; LHD = left hand dominant.
One postoperative complication of contact dermatitis was observed. This was treated with topical steroids and resolved. All patients reported that they would have surgery again. When asked specifically about the function of the small finger, no patients reported any complaints. Improvement was “good” or “excellent” in 6 cases, “fair” in 6 cases, and “no improvement” in 2 cases. No patients felt worse than prior to surgery. Mean carpal tunnel outcome instrument scores were 47.4 ± 6.8 preoperatively and 27.1 ± 10.6 at follow-up (P < .001). QuickDASH scores at follow-up were 29.4 ± 26. Most patients reported improvement in pain but no patient had return of normal sensation. In 11 patients, pain was graded preoperatively as “severe pain with hand function resulting in inability to perform daily activities” or “moderate pain significantly limiting work and limiting activities.” Eight patients (75%) improved to “mild or occasional pain with hand function but able to work and to perform all daily activities” or “no pain with wrist flexion or extension or palpation of the wrist and able to work without pain.” Of the 3 patients who continued to have severe or moderate pain limiting their activities, 2 patients were Worker’s Compensation cases. Mean postoperative pain scores on a 1 to 10 scale was 2.9 ± 1.5. No patient has undergone further surgery on their carpal tunnel; 1 patient underwent an intrinsic release and another underwent bilateral trigger thumb release.
Discussion
The ADM flap was first described by Huber as a transfer for thumb opposition.10 Milward et al16 originally described the application of an ADM flap for use in 1 patient with recurrent median and ulnar nerve compression after failed decompression and neurolysis. Leslie and Ruby13 also applied the ADM flap for coverage of an infected wound dehiscence following CTR in a 41-year-old man taking prednisone for dermatomyositis. Other uses of the ADM flap have been described, including the treatment of metacarpal osteomyelitis.4
In our study, patients with recurrent carpal tunnel syndrome complicated with CRPS underwent ADM flap coverage of the median nerve at the carpal tunnel. Seventy-five percent of patients reported improvement allowing them to perform activities with mild to no pain. Improvements in CTOI scores were observed (Figure 2). Patients reported no difficulties related to the donor muscle site, and no significant complications have arisen related to the palmar incision.
Figure 2.
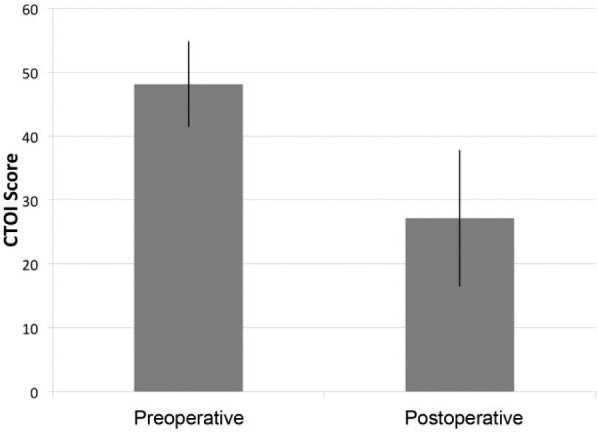
Preoperative and postoperative Carpal Tunnel Outcome Instrument (CTOI) scores.
Note. Error bars indicate standard deviation, P < .001.
The ADM has a number of advantages that make it a good choice to provide soft tissue coverage of the median nerve. It provides reliable vascularized tissue in an attempt to minimize recurrent fibrosis. Indeed, vascularized hypothenar fat flap coverage of the median nerve was superior to synovial tissue with respect to clinical results of treatment of recurrent carpal tunnel syndrome.21 Anatomy is predictable, and the flap easily covers the median nerve distal to the wrist crease.19 Tang et al studied 10 fresh cadavers to detail the anatomy of the intrinsic muscles of the hand. They found the ADM to be the longest intrinsic muscle with an average length of 6.3 cm. They found 1 dominant pedicle that was a direct branch of the muscular branch of the ulnar artery and 2 minor vascular pedicles consistent with a type II flap by the Mathes and Nahai classification.22 Potential disadvantages to use of this technique include risk of taking donor muscle and issues stemming from the palmar incision.
This study is limited by the patient selection, small sample size, and incomplete preoperative data collection. Validated patient report outcome measures were used to assess clinical outcomes. Objective measurements of patient strength, range of motion, and sensation were not assessed.
The ADM flap is a readily available, reliable, and well-vascularized source of soft tissue coverage of the median nerve in recurrent carpal tunnel syndrome and CRPS. It may offer some of these patients improvement in symptoms and function.
Footnotes
Ethical Approval: This study was approved by our institutional review board.
Statement of Human and Animal Rights: All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008 (5).
Statement of Informed Consent: Informed consent was obtained from all patients for being included in the study.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Ackerman WE, Ahmad M. Recurrent postoperative CRPS I in patients with abnormal preoperative sympathetic function. J Hand Surg Am. 2008;33:217-222. [DOI] [PubMed] [Google Scholar]
- 2. Campagna R, Pessis E, Feydy A, et al. MRI assessment of recurrent carpal tunnel syndrome after open surgical release of the median nerve. AJR Am J Roentgenol. 2009;193:644-650. [DOI] [PubMed] [Google Scholar]
- 3. Chrysopoulo MT, Greenberg JA, Kleinman WB. The hypothenar fat pad transposition flap: a modified surgical technique. Tech Hand Up Extrem Surg. 2006;10:150-156. [DOI] [PubMed] [Google Scholar]
- 4. Cirrincione C, Stern PJ. The abductor digiti minimi muscle flap: an adjunct in the treatment of metacarpal osteomyelitis. J Hand Surg Am. 1991;16:824-827. [DOI] [PubMed] [Google Scholar]
- 5. Dahlin LB, Lekholm C, Kardum P, et al. Coverage of the median nerve with free and pedicled flaps for the treatment of recurrent severe carpal tunnel syndrome. Scand J Plast Reconstr Surg Hand Surg. 2002;36:172-176. [DOI] [PubMed] [Google Scholar]
- 6. Dellon AL, Mackinnon SE. The pronator quadratus muscle flap. J Hand Surg Am. 1984;9:423-427. [DOI] [PubMed] [Google Scholar]
- 7. Frank U, Giunta R, Krimmer H, et al. Relocation of the median nerve after scarring along the carpal tunnel with hypothenar fatty tissue flap-plasty. Handchir Mikrochir Plast Chir. 1999;31:317-322. [DOI] [PubMed] [Google Scholar]
- 8. Giunta R, Frank U, Lanz U. The hypothenar fat-pad flap for reconstructive repair after scarring of the median nerve at the wrist joint. Chir Main. 1998;17:107-112. [DOI] [PubMed] [Google Scholar]
- 9. Goitz Rj, Steichen JB. Microvascular omental transfer for the treatment of severe recurrent median neuritis of the wrist: a long-term follow up. Plast Reconstr Surg. 2005;115:163-171. [PubMed] [Google Scholar]
- 10. Huber E. Relief operation in the case of paralysis of the median nerve. J Hand Surg Eur Vol. 2004;29:35-37. [DOI] [PubMed] [Google Scholar]
- 11. Jones NF, Ahn HC, Eo S. Revision surgery for persistent and recurrent carpal tunnel syndrome and for failed carpal tunnel release. Plast Reconstr Surg. 2012;129:683-692. [DOI] [PubMed] [Google Scholar]
- 12. Jupiter JB, Seiler JG, Zienowicz R. Sympathetic maintained pain (causalgia) associated with a demonstrable peripheral-nerve lesion. Operative treatment. J Bone Joint Surg Am. 1994;76:1376-1384. [DOI] [PubMed] [Google Scholar]
- 13. Leslie BM, Ruby LK. Coverage of a carpal tunnel wound dehiscence with the abductor digiti minimi muscle flap. J Hand Surg Am. 1988;13:36-39. [DOI] [PubMed] [Google Scholar]
- 14. Luchetti R, Riccio M, Papini Zorli I, et al. Protective coverage of the median nerve using fascial, fasciocutaneous or island flaps. Handchir Mikrochir Plast Chir. 2006;38:317-330. [DOI] [PubMed] [Google Scholar]
- 15. Mathoulin C, Bahm J, Roukoz S. Pedicled hypothenar fat flap for median nerve coverage in recalcitrant carpal tunnel syndrome. Hand Surg. 2000;5:33-40. [DOI] [PubMed] [Google Scholar]
- 16. Milward TM, Stott WG, Kleinert HE. The abductor digiti minimi muscle flap. Hand. 1977;9:82-85. [DOI] [PubMed] [Google Scholar]
- 17. Plancher KD, Idler RS, Lourie GM, et al. Recalcitrant carpal tunnel. The hypothenar fat pad flap. Hand Clin. 1996;12:337-349. [PubMed] [Google Scholar]
- 18. Sotereanos DG, Giannakopoulos PN, Mitsionis GI, et al. Vein-graft wrapping for the treatment of recurrent compression of the median nerve. Microsurgery. 1995;16:752-756. [DOI] [PubMed] [Google Scholar]
- 19. Spokevicius S, Kleinert HE. The abductor digiti minimi flap: its use in revision carpal tunnel surgery. Hand Clin. 1996;12:351-355. [PubMed] [Google Scholar]
- 20. Stütz N, Gohritz J, Van Shoonhoven J, et al. Revision surgery after carpal tunnel release—analysis of the pathology in 200 cases during a 2 year period. J Hand Surg-Brit Eur. 2006;31:68-71. [DOI] [PubMed] [Google Scholar]
- 21. Stutz NM, Gohritz A, Novotny A, et al. Clinical and electrophysiological comparison of different methods of soft tissue coverage of the median nerve in recurrent carpal tunnel syndrome. Neurosurgery. 2008;62:194-199. [DOI] [PubMed] [Google Scholar]
- 22. Tang M, Thomas BP, Geddes CR, et al. Vascular basis of intrinsic muscle flaps in the hand. Plast Reconstr Surg. 2008;122;206-215. [DOI] [PubMed] [Google Scholar]