Abstract
Background: Posterior interosseous nerve neurectomies (PINN) are an option in the treatment of chronic dorsal wrist pain. However, the literature describing PINN consists primarily of small case series, and the procedure is typically done as an adjunct treatment; therefore, the outcomes of the PINN itself are not well known. We performed a systematic review of the literature to provide characteristics of patients following a PINN. Methods: A systematic review of the literature was performed. Papers published in the PubMed database in English on isolated PINN were included. Articles in which a PINN was performed as an adjunct were excluded. Primary outcomes were return to work, patient satisfaction, pain/function scores, wrist range of motion, complications, and pain recurrence. Weighted averages were used to calculate continuous data, whereas categorical data were noted in percentages. Results: The search yielded 427 articles including 6 studies and 135 patients (136 cases). The average age was 43.6 years (range, 17-75), and most patients were female (54.1%). At an average final follow-up of 51 months, 88.9% of patients were able to return to work. After initial improvement, a recurrence of pain occurred in 25.5% of patients at an average of 12.3 months. Excluding recurrence of pain, the complication rate was 0.9%, including 1 reflex sympathetic dystrophy. Overall, 88.4% of patients experienced a subjective improvement and were satisfied with the procedure. Conclusions: Isolated PINN have shown excellent clinical outcomes, with few patients experiencing recurrent pain at long-term follow-up. PINN can provide relief in patient’s chronic wrist pain.
Keywords: wrist denervation, posterior interosseous nerve neurectomy, chronic wrist pain, PINN, hand and wrist surgery
Introduction
The posterior interosseous nerve neurectomy (PINN) was first described in 1966 by Wilhelm who performed dorsal wrist denervation in patients presenting with pain due to trauma, necrosis of the lunate, arthritis, and scaphoid nonunions recalcitrant to conservative measures.17 These findings were reinforced by a second German report 11 years later in which a combination of wrist denervations were performed, yielding good pain relief in 80% of patients after a follow-up of more than 2 years.3
Subsequently, PINN has been used as both an isolated5,6,8,9,11,12 and adjunct procedure1,4,13,18 treating patients with chronic dorsal wrist pain that is unresponsive to nonoperative treatments. Although several techniques for wrist denervation exist,7,10 the PINN is the simplest technically to achieve, requires the least soft tissue handling, and the PIN innervates the central two-thirds of the wrist including to the wrist capsule, scaphoid, lunate, and dorsal distal radius.15
However, the PINN literature is comprised of short case series without controls. In addition, because the procedure is typically in addition to other treatments to include carpal excision,13 wrist fracture,1 nonunion,18 or Kienbock disease,4 the quality of and length of effect of wrist denervation alone are not well known. The goal of this study is to produce a large conglomeration of patients who have undergone an isolated PINN to give a better understanding of the advantages and disadvantages of the technique. A systematic review of the published literature was performed to show patients’ demographics and elucidate outcomes, complications, and length of effect following an isolated PINN. We hypothesize that in the treatment of wrist pain, PINN as a palliative procedure will provide moderate pain relief with few complications.
Materials and Methods
Literature Search
We identified all publications regarding isolated PINN. A comprehensive literature search was performed beginning with queries into the PubMed, MEDLINE, Cochrane, and EMBASE databases for all articles between January 1, 1980, and June 1, 2016. A total of 3 search terms—(1) “PIN neurectomy,” (2) “wrist denervation,” and (3) “posterior interosseous nerve neurectomy”—were entered into the keyword search field. This initial search yielded a total of 427 original articles that were then isolated for further screening.
Study Selection
The abstracts of all the articles were initially analyzed to determine relevance to our review and were excluded if they were clearly irrelevant, published in a non-English language, involving PINN procedures combined with concomitant procedures (such as fracture fixation or other soft tissue procedures), literature reviews or expert opinion, basic science/anatomical studies, or published prior to 1980. Full articles of the remaining studies were then obtained and reviewed for the following inclusion criteria: peer-reviewed clinical studies of level I to IV evidence; involving at least 6 patients; evaluating the outcomes following isolated PINN, with at least 1 year and 80% follow-up; and reporting at least 1 outcome measure of interest including postoperative pain, function, or complications. One article included 8 patients, of which 3 had an additional procedure.5 To ensure that only isolated PINN were included, all 8 of these patients were excluded. The references of these articles were additionally reviewed by the authors to isolate any additional publications not included based on the initial searches.
Patient demographics (age, sex, dominant extremity), preoperative symptoms (pain/functional scores, chronicity of symptoms), and primary outcomes of interest (pain and functional outcome scores, patient satisfaction, range of motion [ROM], return to work) were extracted. We additionally analyzed the reported complications and reoperations.
Statistical Analysis
Continuous data were calculated using weighted averages with respective standard deviations. Categorical data were noted in percentages. A 2-tailed student’s t test was performed to compare the M-SACRAH (modified score for the assessment and quantification of chronic rheumatoid affections of the hand) scores, a questionnaire that assesses the rheumatoid hand in hand function, rated 0 (possible without difficulty) to 800 (impossible); stiffness, rated 0 (no stiffness) to 200 (unbearable stiffness); and pain, rated 0 (no pain) to 200 (unbearable pain), and a P value less than .05 was considered statistically significant. All calculations were performed using SAS version 9.3 (SAS Institute Inc, Cary, North Carolina).
Results
Study Selection
Of the 427 original articles, 90 were immediately eliminated due to clear irrelevance and the exclusion criteria set forth. Of the remaining 337, the full manuscripts and respective references were reviewed by the 3 primary investigators (D.J.V.B., J.C.D., N.A.K.). Following review, 92 were discarded for being of non-English origin, 22 because PINN was used as an adjunct with another procedure, 153 because they were anesthesia/blockade studies, 4 because they were literature reviews or expert opinions, 26 because they were anatomical studies, 3 discarded for being nonsurgical procedures, 30 because they were other upper extremity denervations (not involving PIN), and 1 study because it contained the same subset of patients already included in the systematic review (Figure 1). The final compilation comprised 6 publications (all level IV studies), and 4 reported procedures performed by a single surgeon.5,8,9,12 The most frequent journal included was the Journal of Hand Surgery (4), and publication dates ranged from 1985 to 2016.
Figure 1.
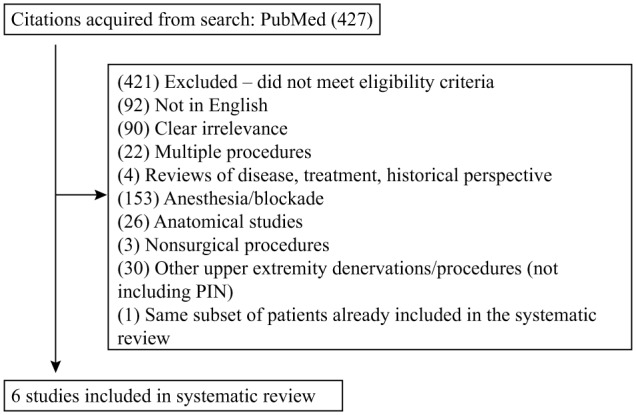
Study selection.
Note. PIN = posterior interosseous nerve.
Patient Demographics and Injury Characteristics
The 6 studies included in this systematic review contained 135 patients (136 wrists). The weighted average age of the cohort was 43.6 years (range of study means, 17-75), and just over one-half of the patients were female (54.1%). Of those studies that reported hand dominance,11,12 the dominant hand was involved in 74.3% of cases. Patient demographics are included in Table 1.
Table 1.
Demographics (135 Patients).
| Patients | Number of studies (patients for which was recorded) | |
|---|---|---|
| Average age | 43.6 (range, 17-75) | 6 (135) |
| Average follow-up, mo | 51 (range, 16.3-138.1) | 4 (106) |
| Male | 62 (45.9%) | 6 (135) |
| Dominant extremity | 26 (73.4%) | 3 (35) |
| Average symptom duration, mo | 47.5 | 1 (6) |
| Preoperative pain score (M-SACRAH criteria; 0-800) | 167 (range, NR; SD, 41) | 1 (12) |
| Preoperative functional score (M-SACRAH criteria; 0-200) | 632 (range, NR; SD, 86) | 1 (12) |
| Preoperative stiffness score (M-SACRAH criteria; 0-200) | 90 (range, NR; SD, 30) | 1 (12) |
Note. M-SACRAH = modified score for the assessment and quantification of chronic rheumatoid affections of the hand; NR = not reported; SD = standard deviation.
Operative indications include chronic dorsal wrist pain (83.3%), followed by rheumatoid arthritis (8.3%), Kienbock disease (3.5%), osteoarthritis (2.8%), scaphoid nonunion (1.4%), and wrist instability (0.7%). Two articles reported previous procedures on the affected carpus including open reductions with internal fixation (n = 8), closed reduction (n = 6), and nonunion treated with volar bone grafting (n = 5).5,11
Operative Technique
Two authors included a discussion of their operative technique and postoperative rehabilitation protocol.5,8 Dellon et al5 resected a 2-cm section of the PIN proximal to the extensor retinaculum through a standard dorsal approach. Patients were subsequently splinted postoperatively for 1 week followed by an active ROM with protective splinting for an additional 2 weeks. Lluch and Beasley8 reported a similar procedure but noted some variability in that in earlier cases within the series, the posterior interosseous artery was resected with the nerve, whereas the artery was left intact in 25 later cases.
Outcomes
At an average final follow-up of 51 months (range of study means, 16.3-138.1), 88.9% of patients were able to return to work at their full capacity. In addition, 3 patients were able to return to partial work, requiring the use of a splint. Of those studies reporting ROM, 96.4% of patients had increased wrist ROM postoperatively.5,9 Outcomes are displayed in Table 2.
Table 2.
Outcomes.
| Patients | Number of studies (number of cases) | |
|---|---|---|
| Return to work | 24 (88.9%) | 2 (27) |
| Increase in wrist ROM | 27 (96.4%) | 2 (28) |
| Subjective improvement and good patient satisfaction | 99 (88.4%) | 5 (112) |
| Postoperative pain score (M-SACRAH; 0-800) | 14 (range, NR; SD, 19) | 1 (12) |
| Postoperative functional score (M-SACRAH; 0-200) | 98 (range, NR; SD, 94) | 1 (12) |
| Postoperative stiffness score (M-SACRAH; 0-200) | 79 (range, NR; SD, 27) | 1 (12) |
| Would recommend the surgery | 12 (100%) | 1 (12) |
Note. ROM = range of motion; M-SACRAH = modified score for the assessment and quantification of chronic rheumatoid affections of the hand; NR = not reported; SD = standard deviation.
One study utilized validated functional outcome measures. Riches et al12 utilized an M-SACRAH questionnaire preoperatively and postoperatively and found that pain improved substantially from 167 to 14, the functional score from 632 to 98, and stiffness score less dramatically, from 90 to 79. All patients noted a significant improvement in pain and function (P < .001) but not a significant improvement in stiffness.12
Two series mentioned an initial improvement of symptoms postoperatively, with the recurrence of pain occurring in 25.5% of patients at an average follow-up of 12.3 months.5,6
Patterson and colleagues11 evaluated proprioception following PINN evaluating the patients’ sense of wrist position at neutral (0°) as well as varying degrees of flexion (20°, 40°, 60°), extension (20°, 40°, 60°), and radial (10°) and ulnar (10°) deviation. The most imprecise estimations of wrist positions occurred at 40° and 60° of flexion (both a 14°-16° underestimation). Patients also tended to overestimate amount of ulnar (4°-9°) versus radial deviation (−4° to +2° deviation). Second, authors compared proprioception of patient’s surgical wrist versus a control (wrists of healthy volunteers) which showed a statistically significant, more accurate measurement at 40° extension in the postoperative patients (measurement of 46°) compared with control (measurement of 52°; P = .032). Finally, proprioception was measured between patient’s surgical wrist and the same patient’s nonsurgical wrist which showed no statistically significant differences.11
Overall, 88.4% of patients experienced a subjective improvement and were satisfied with the procedure. In addition, one study reported that all of the patients in the series would recommend the surgery to someone experiencing similar symptoms.12
Complications
All studies discussed complications. Overall, only 1 complication (excluding recurrence of pain) was reported among 113 cases5,6,8,9,12 (0.9%), including 1 case of reflex sympathetic dystrophy, which was treated with 2 stellate ganglion blocks.5 Four studies reported no complications (0%) among their respective cohorts.6,8,9 Of 3 patients experiencing recurrence of pain due to progressive carpal collapse, all went onto fusion after returning to work.5 Complication and secondary surgery rates are shown in Table 3.
Table 3.
Complications.
| Patients | Number of studies (number of cases) | |
|---|---|---|
| Pain recurrence | 13 (25.5%) | 2 (51) |
| Average time of pain recurrence, mo | 12.3 | 2 (13) |
| Complications (excluding pain recurrence) | 1 (0.9%) | 5 (113) |
| Required secondary surgery | 4 (3.5%) | 5 (113) |
Discussion
This investigation sought to characterize the demographics, outcomes, and complications of isolated PINN through a large systematic review of 135 patients. We hypothesized that PINN would provide moderate pain relief with few complications. There were 3 key findings in this study. First, 88.4% of patients achieved some degree of pain relief, 88.9% returned to full duty at work, and 100% would recommend surgery. Second, the pain recurrence rate was 25.5%, which recurred at an average of 12.3 months postoperatively. Finally, the complication rate (excluding pain recurrence) was exceptionally low at 0.9%, and only 3.5% required secondary surgery. The PINN is a simple procedure with excellent outcomes and few complications and should be considered in the treatment of chronic wrist pain.
Following isolated PINN for chronic wrist pain, excellent outcomes were achieved (Table 4). The results of an isolated PINN are generally comparable with that which has been reported from a combined anterior interosseous nerve (AIN) and PIN neurectomy2,7,16 or a total wrist denervation (TWD).10 Comparable with the present results of PINN, in a review of 23 patients undergoing AIN/PINN through a single dorsal incision after 2.5 years, 80% of patients reported a decrease in pain, 73% returned to work, and 90% would recommend the procedure.16 In a series of 48 wrists with chronic wrist pain treated with a 2-incision AIN/PINN after an average of 28 months, grip strength improved 16% (not statistically significant), there was a 51% improvement in pain, and the Disabilities of the Arm, Shoulder and Hand (DASH) score improved 15 points. There was no correlation with success of a preoperative injection and postoperative pain relief.7 There was not consistent reporting correlating preoperative injection to postoperative outcome in the present series. However, the patients receiving isolated PINN did overwhelming improve (88.4%), 89% returned to work, and 96% of patients experience an increase in ROM. Denervation of the wrist requires only a small dorsal incision and does not warrant postoperative splinting. In addition to postoperative local block, we encourage early active ROM, which likely contributes to the excellent functional outcomes.
Table 4.
Analyses Regarding Isolated Posterior Interosseous Nerve Neurectomies.
| Author, LOE | No. of patients (cases) | Mean age (y) | Follow-up (mo) | Subjective improvement/patient satisfaction | Reoperation rate | Complications (excluding pain recurrence) | Return to work | Pain recurrence | Average time to pain recurrence |
|---|---|---|---|---|---|---|---|---|---|
| Dellon et al,5 IV | 21 (22) | 38.5 | 15.8 | 21/21 (100%) | 4/22 (18.2%) | 1/22 (4.5%) | 18/21 (85.7%) | 3/21 (14.3%) | 14 |
| Ferreres et al,6 IV | 30 (30) | 34.4 | 56.4 | 19/30 (63.3%) | 0 | 0 | NR | 10/30 (33.3%) | 12 |
| Lluch and Beasley,8 IV | 43 (43) | 46 | 72 | 43/43 (100%) | 0 | 0 | NR | NR | NR |
| Loh et al,9 IV | 6 (6) | 37 | NR | 5/6 (83.3%) | 0 | 0 | 6/6 (100%) | NR | NR |
| Patterson et al,11 IV | 23 (23) | 47 | NR | NR | NR | NR | NR | NR | NR |
| Riches et al,12 IV | 12 (12) | 63.7 | 24 | 11/12 (91.7%) | 0 | 0 | NR | NR | NR |
| Weighted average | 135 (136) | 43.6 | 51 | 99/112 (88.4%) | 4/113 (3.5%) | 1/113 (0.9%) | 24/27 (88.9%) | 13/51 (25.5%) | 12.3 |
Note. LOE = level of evidence; NR = not reported.
While the results of AIN/PINN and isolated PINN are analogous in many cases,7,14,16 one direct comparison of TWD with PINN was performed with 52 patients. Although the study was retrospective, not randomized, and the indications for the procedures in all cases are not known, the authors demonstrated a larger percentage of patients in the TWD group achieving improvement as compared with the PINN cohort. Furthermore, the authors believe that the PINN cohort would have had a higher recurrence rate if studied for a longer period of time.6
In the current analysis, pain recurrence occurred in 13 patients, 10 (77%) of whom were included in the aforementioned TWD-PINN comparison, which had the second longest follow-up (56.4 months) included presently6 (Table 4). It is possible that a longer follow-up enables the patients to be studied when they return to work and therefore may explain pain recurrence. In addition, the underlying disease process, which may include rheumatoid arthritis, may progress postoperatively, causing additional pain and thereby accounting for the 25.5% recurrence rate. Despite this, the pain recurrence in this review was not until an average of 12.3 months postoperatively. Even in the minority of patients with pain recurrence (25.5%), these patients still had a year of pain relief. For a procedure as simple as a small 3-cm incision over the fourth dorsal compartment,7 we believe the PINN is worth the risk of pain recurrence.
One article included accounted for all of the reoperations, other complications, and 3 of 13 cases of pain recurrence. It is worth noting that in this cohort, 16 of 29 (55.2%) were involved in either workmen’s compensation cases or ligation after motor vehicle accidents. The other complications noted in this report included 4 patients with progressive carpal collapse, 3 of which went onto fusion after returning to work.5 There were no cases of development of a neuropathic Charcot wrist.3,11,17 With resection of the sensory portion of the PIN, the denervated wrist joint could hypothetically lose wrist proprioception, precipitating a neuropathic joint. However, in a laboratory analysis of proprioceptive function following PINN, there was no difference between PINN and control in terms of wrist proprioception.
There were 3 limitations to the present analysis. First, the study was retrospective and the data were heterogeneous, making it impossible to draw overly specific conclusions about the results. In addition, the heterogeneous nature of the data limits the external validity of our findings to specific patient populations. Second, because of the nature of a systematic review, the quality of the data presented is limited by the quality of the data recorded in the included studies. Third, the complication rate is likely underreported. Pain recurrence was only recorded in 2 of 6 studies, and the 4 studies did not report any complications. It is likely that after a 3-cm dorsal incision with limited dissection, complications would be low; however, the authors would anticipate a prospective analysis with strict follow-up would yield a higher complication rate.
Despite these shortcomings, the present analysis is the largest review of isolated PINN in the literature. Although the PINN is most typically performed as an adjunct, in conjunction with an additional procedure, the present analysis of isolated PINN demonstrates that the PINN may be completed as a stand-alone procedure in the setting of recalcitrant wrist pain. At almost 4-year follow-up, PINN has proven to achieve excellent clinical outcomes, few complications, and a low recurrence rate. When wrist pain is recalcitrant to conservative measures, PINN is a simple treatment option offering the prospect of pain relief with few risks to the patient.
Footnotes
Ethical Approval: This study was approved by our institutional review board.
Statement of Human and Animal Rights: This article does not contain any studies with human or animal subjects.
Statement of Informed Consent: Informed consent is not necessary in this study.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Backowski B, Dzwonkowska J, Lorczynski A, et al. Posterior interosseous nerve neuropathy in distal radius fracture. Ortop Traumatol Rehabil. 2006;8(3):350-355. [PubMed] [Google Scholar]
- 2. Berger RA. Partial denervation of the wrist: a new approach. Tech Hand Up Extrem Surg. 1998;2:25-35. [DOI] [PubMed] [Google Scholar]
- 3. Buck-Gramcko D. Denervation of the wrist joint. J Hand Surg Am. 1977;2:54-61. [DOI] [PubMed] [Google Scholar]
- 4. Buck-Gramcko D. Wrist denervation procedures in the treatment of Kienbock’s disease. Hand Clin. 1993;9(3):517-520. [PubMed] [Google Scholar]
- 5. Dellon AL, Mackinnon SE, Daneshvar A. Terminal branch of anterior interosseous nerve as source of wrist pain. J Hand Surg Br. 1985;9:613-620. [DOI] [PubMed] [Google Scholar]
- 6. Ferreres A, Suso S, Foucher G, et al. Wrist denervation: surgical considerations. J Hand Surg Br. 1995;20(6):769-772. [DOI] [PubMed] [Google Scholar]
- 7. Hofmeister EP, Moran SL, Shin AY. Anterior and posterior interosseous neurectomy for the treatment of chronic dynamic instability of the wrist. Hand (N Y). 2006;1(2):63-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Lluch A, Beasley R. Treatment of dysesthesia of the sensory branch of the radial nerve by distal posterior interosseous neurectomy. J Hand Surg Am. 1989;14(1):121-124. [DOI] [PubMed] [Google Scholar]
- 9. Loh YC, Stanley JK, Jari S, et al. Neuroma of the distal posterior interosseous nerve. J Bone Joint Surg Br. 1997;80(4):629-630. [DOI] [PubMed] [Google Scholar]
- 10. Patil V, Arenas-Prat J. Radical wrist denervation and preliminary results [published online ahead of print September 20, 2016]. Tech Hand Up Extrem Surg. 2016. doi: 10.1097/BTH.0000000000000124. [DOI] [PubMed] [Google Scholar]
- 11. Patterson R, Van Niel M, Shimko P, et al. Proprioception of the wrist following posterior interosseous sensory neurectomy. J Hand Surg Am. 2010;35(1):52-56. [DOI] [PubMed] [Google Scholar]
- 12. Riches P, Elherik F, Dolan S, et al. Patient rated outcomes study into the surgical interventions available for the rheumatoid hand and wrist. Arch Orthop Trauma Surg. 2016;136(4):563-570. [DOI] [PubMed] [Google Scholar]
- 13. Roberts D, Power DM. Acute scaphoidectomy and four-corner fusion for the surgical treatment of trans-scaphoid perilunate fracture dislocation with pre-existing scaphoid non-union [published online ahead of print July 16, 2015]. BMJ Case Rep. doi: 10.1136/bcr-2015-209520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Schweizer A, von Kanel O, Kammer E, et al. Long-term follow-up evaluation of denervation of the wrist. Nerve. 2006;31(4):559-564. [DOI] [PubMed] [Google Scholar]
- 15. Van de Pol GJ, Koudstaal MJ, Schuurman AH, et al. Innervation of the wrist joint and surgical perspectives of denervation. J Hand Surg Am. 2006;31(1):28-34. [DOI] [PubMed] [Google Scholar]
- 16. Weinstein LP, Berger RA. Analgesic benefit, functional outcome, and patient satisfaction after partial wrist denervation. J Hand Surg Am. 2002;27:833-839. [DOI] [PubMed] [Google Scholar]
- 17. Wilhelm A. Die Gelenkdenervation und ihre anatomischen Grundlagen. Hefte zur Unfallheilkunde. 1966;86:1-109. [PubMed] [Google Scholar]
- 18. Xiong L, Harhaus L, Heffinger C, et al. A comparative study on autologous bone grafting combined with or without posterior interosseous nerve neurectomy for scaphoid nonunion treatment. J Plast Reconstr Aesthet Surg. 2015;68(8):1138-1144. [DOI] [PubMed] [Google Scholar]


