Abstract
Objective
Statin use over the age of 80 years is weakly evidence-based. This study aimed to estimate rates of statin inception and deprescribing by frailty level in people aged 80 years or older.
Methods
A cohort of 212,566 participants aged ≥80 years was sampled from the UK Clinical Practice Research Datalink. Statin inception was defined as a first-ever prescription in a non-statin user; deprescribing was defined as a last ever statin prescription more than 6 months before the end of participant records. Rates were estimated in a time-to-event framework allowing for mortality as a competing risk. Covariates were age, gender, frailty category and prevention type.
Results
Prevalent statin use increased from 2001-5 (9.9%) to 2011-15 (49.3%). Inception of statins in never-users was low overall at 2.4% per year (95% confidence interval (CI) 2.2% to 2.6%) and declined with age. Deprescribing of statins in current users occurred at a rate of 5.6% (95% CI 5.4% to 5.9%) per year overall and increased with age, reaching 17.8% per year (95% CI 6.7% to 28.9%) among centenarians. Deprescribing was slightly higher for primary prevention (6.5% per year) than secondary prevention (5.2% per year) indications (P<0.001). Deprescribing increased with frailty level being 5.0% per year in ‘fit’ participants and 7.1% in ‘severe’ frailty (P<0.001).
Conclusions
Statin use has increased in the over-80s but deprescribing is common and increases with age and frailty level. These paradoxical findings highlight a need for better evidence to inform statin use and discontinuation for people aged ≥80 years.
Keywords: cardiovascular disease, statin therapy, primary care, 80 and over, frailty
Background
CVD prevention is of increasing importance in people aged 80 years and over. [1,2] The use of statins has become more widespread [3] and this trend extends to people over 80 years.[4, 5] However, prescribing of statins in this age-group, especially for primary prevention of CVD, remains controversial and poorly evidence-based.[6, 7] Current guidelines encourage individualised decisions for older people.[8–10] This may require consideration of level of frailty because frailty is often associated with clinical indications for prescribing but the risks of harms may increase with frailty level.[10] This study aimed to evaluate statin prescribing in people aged 80 years and older.
Methods
Study Design and Participants
A population-based cohort study was conducted in the UK Clinical Practice Research Datalink (CPRD). [11, 12] Eligible participants were selected from patients aged at least 80 years old and registered with the CPRD between 1st January 2001 and the 31st December 2015. For each calendar year from 2001 to 2015, and for each single year of age from 80 to 105 years, 1,000 patients were sampled from the population of patients registered during that year. The final cohort was 212,566 participants because there were fewer eligible at the maximum at older ages and, because sampling was performed with replacement, some participants were sampled in multiple years. The sample size was sufficient to estimate a proportion with precision (confidence interval width) of less than +/- 1%. Person-time was analysed for each participant from the later of start of their record in CPRD or the 1st January in the year in which they were sampled, to the earlier of the date of death or end of CPRD record.
Study Measures
Statin drugs were considered as a single group based on all statins available for prescription between 2001 and 2015. Covariates were gender, five-year age group, co-morbidity and frailty category. Co-morbidity was determined from analysis of Read medical codes, and drug product codes, for diabetes mellitus,[13] coronary heart disease[14] and stroke[15] as reported previously. Participants with one or more of these conditions were classified as having a secondary prevention indication from the date of the earliest diagnosis. Diabetes mellitus confers a similar level of CVD-risk as a previous cardiovascular event.[16] Frailty status was assessed using a previously published 36-item electronic Frailty Index (eFI)[17] based on a cumulative deficit model.[18] Categories of fit, mild, moderate and severe frailty were defined.[17] The 36 items included in the eFI encompass common cardiovascular diseases and diabetes.
Analysis
Participants were classified as prevalent statin users if they received one or more statin prescriptions within 12 months of their entry to the study. Statin inception was defined as a first-ever statin prescription recorded more than 12 months after entry to the study. Statin deprescribing [19] among prevalent statin users was defined as a last ever statin prescription occurring more than six months before the end of the participant’s record. Previous research has shown that the average duration of prescriptions for long-term conditions in CPRD is about 90 days.[20] We estimated rates of inception and deprescribing as the cumulative incidence of each outcome allowing for competing risks.[21] Analyses were performed using the ‘cmprsk’, ‘ggplot2’ and ‘forestplot’ packages in the R program.[22]
Results
The cohort comprised 212,566 participants including 69,001 men and 143,565 women aged 80 years or older. In 2001-2005, 12% of men and 9% of women were prescribed statins (Table 1), increasing to 55% of men and 46% of women in 2011-2015. Statin prescribing generally decreased in frequency with increasing age group but by 2011-2015, 12% of centenarians were prescribed statins. Statin prescribing was considerably higher in participants with secondary prevention indications, in whom 80% were prescribed statins in 2011-2015 compared to 30% with primary prevention participants were prescribed statins (P<0.001). Statin prescribing also increased with frailty level from 26% of ‘fit’ patients to 69% of ‘severely frail’ patients in 2011-2015 (P<0.001). Data are presented for all person-time by year in Supplementary Figure 1 and Supplementary Table 1.
Table 1. Prevalent statin use at study entry. Figures are frequencies (column percent).
| Year of entry to study | P value (test for trend) | |||||||
|---|---|---|---|---|---|---|---|---|
| 2001-2005 | 2006-2010 | 2011-2015 | ||||||
| Freq. | % | Freq. | % | Freq. | % | |||
| Total | 8,091 / 81,353 | 9.9 | 23,293 / 66,817 | 34.9 | 31,747 / 64,396 | 49.3 | <0.001 | |
| Gender | Male | 3,013 / 24,251 | 12.4 | 8,780 / 22,004 | 39.9 | 12,492 / 22,746 | 54.9 | <0.001 |
| Female | 5,078 / 57,102 | 8.9 | 14,513 / 44,813 | 32.4 | 19,255 / 41,650 | 46.2 | <0.001 | |
| Age Group | 80-84 | 4,367 / 23,673 | 18.5 | 10,764 / 23,132 | 46.5 | 13,486 / 23,060 | 58.5 | <0.001 |
| 85-89 | 2,455 / 22,130 | 11.1 | 7,541 / 19,793 | 38.1 | 10,103 / 18,981 | 53.2 | <0.001 | |
| 90-94 | 1,060 / 20,412 | 5.2 | 3,863 / 15,327 | 25.2 | 6,233 / 14,724 | 42.3 | <0.001 | |
| 95-99 | 196 / 12,823 | 1.5 | 1,096 / 7,989 | 13.7 | 1,838 / 6,905 | 26.6 | <0.001 | |
| 100+ | 13 / 2,315 | 0.6 | 29 / 576 | 5.0 | 87 / 726 | 12.0 | <0.001 | |
| Frailty | Fit | 1,956 / 36,500 | 5.4 | 3,159 / 17,190 | 18.4 | 3,224 / 12,394 | 26.0 | <0.001 |
| Mild | 3,458 / 28,373 | 12.2 | 8,855 / 25,744 | 34.4 | 10,587 / 23,052 | 45.9 | <0.001 | |
| Moderate | 1,993 / 12,691 | 15.7 | 7,478 / 16,811 | 44.4 | 10,954 / 18,814 | 58.2 | <0.001 | |
| Severe | 684 / 3,789 | 18.0 | 3,801 / 7,072 | 53.7 | 6,982 / 10,136 | 68.9 | <0.001 | |
| Prevention Type | Primary | 2,251 / 57,155 | 3.9 | 7,815 / 43,397 | 18.0 | 12,146 / 39,892 | 30.4 | <0.001 |
| Secondary | 5,840 / 24,198 | 24.1 | 15,478 / 23,420 | 66.1 | 19,601 / 24,504 | 80.0 | <0.001 | |
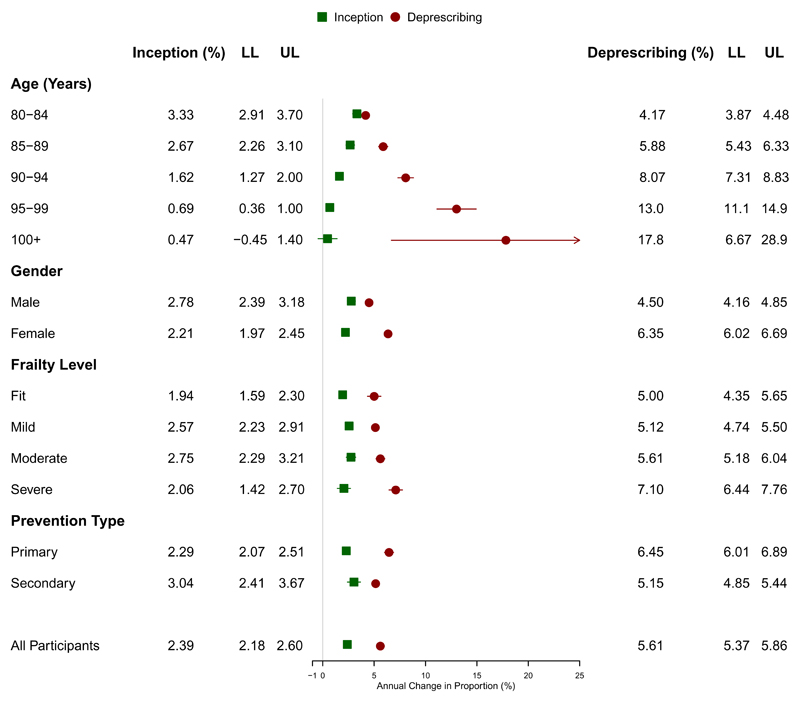
Figure 1 presents a forest plot showing rates of inception and deprescribing of statins during the period 2011-2015 according to levels of covariates of the whole sample. Among never-users of statins the rate of statin inception was 2.4% per year (95% confidence interval 2.2% to 2.60%). The rate of statin inception declined with age (P<0.001) being 3.3% per year (2.9% to 3.7%) at 80 to 84 years, but 1.6% (1.3% to 2.0%) at 90-94 years and 0.5% (-0.5% to 1.4%) among centenarians. Statin inception was only slightly higher in men than women (P<0.001) and was non-significantly higher for secondary prevention (3.0% per year) than primary prevention indications (2.3%) (P=0.177). Statin inception was but lowest among ‘fit’ participants but rates were generally similar among those with ‘mild’, ‘moderate’ or ‘severe’ frailty, though overall differences by frailty category were not significant (P=0.123).
Figure 1. Forest plot showing annual proportion (%) for inception of statins among never-users of statins, and deprescribing of statins among statin users. Upper (UL) and lower limits (LL) of 95% confidence intervals are shown.
The rate of statin deprescribing among statin users was 5.6% per year overall (95% confidence interval 5.4% to 5.9%). The rate of statin deprescribing increased substantially with age (P<0.001) being 4.2% per year (3.9% to 4.5%) at 80 to 84 years, 8.1% (7.3% to 8.8%) at 90 to 94 years and 17.8% (6.7% to 28.9%) among centenarians. Statin deprescribing was higher (P<0.001) among women (6.4%, 6.0% to 6.7%) than men (4.5%, 4.2% to 4.9%) and increased with frailty level (P<0.001), being 5.0% (4.4% to 5.7%) per year among ‘fit’ participants but 7.1% (6.4% to 7.8%) among participants with ‘severe’ frailty. Deprescribing was also slightly higher (P<0.001) among participants with primary prevention (6.5%) than secondary prevention (5.2%) indications.
Discussion
Main findings
These data reveal a substantial increase in the use of statins between 2001 and 2015. Statin prescribing has increased in the general population following publication of several studies that demonstrated reduced mortality and new CVD events from statin therapy in people at high risk.[23, 24] Much of the increase in statin use in the over-80s may be accounted for by a ‘cohort effect’, with individuals who started statins in their 60s and 70s now reaching older ages still taking statins. We find that inception of statins in people aged more than 80 is not a frequent event, we also provide estimates of statin deprescribing for relevant population sub-groups.
Individuals classified as ‘frail’ according to a deficit accumulation model that includes CVD conditions [17, 25] are also frequently prescribed statins. Nearly one in four ‘fit’ individuals who do not have cardiovascular disease or diabetes are now statin users. Our results show that statin inception among never-users of statins in their 80s and 90s only occurs at low rates [3] and generally become less frequent with age. The results show that statin deprescribing among prevalent statin users occurs at twice the rate of statin inception at 80 to 84 years. Among 90 to 94 year olds, statin deprescribing is observed at more than four times the rate of statin inception.
Strengths and limitations
We classified patients’ frailty level according to an established measure of frailty but this relied on medical diagnoses coded into electronic health records.[17, 26] This approach may not always be consistent with assessment of frailty using physical measures.[25] We observed evidence for discontinuation of statin prescriptions but lack of information on the reasons for discontinuation is a limitation of this study. We were not able to assess the appropriateness of statin prescribing or deprescribing, our results might be compatible either with over- or under-use of statins in this age group. One of the main conclusions of the study is that clearer recommendations for appropriate use of statins in the over-80s are needed.
Comparison with other studies
Trends reported in this paper are consistent with those reported from Europe[4] and the U.S. [5] Clinical recommendations for the use of statins have been informed by meta-analyses of randomised controlled trials but these provide limited evidence for people aged over-80. The 2013 Cochrane review on statins for the primary prevention of cardiovascular disease included 18 trials,[27] nine of these excluded participants aged over 80 and in the remaining trials, the mean age of participants was no higher than 66 years. A systematic review of clinical trials of statin treatment suggested that statins may reduce mortality in people aged over 65 with coronary heart disease.[28] In participants without established CVD, there was evidence of reduced incidence of myocardial infarction and stroke but no evidence for reduction in mortality.[29] In a review of clinical trial evidence for people aged over 80 years, Petersen et al. [30] concluded that there was no evidence from clinical trials that cholesterol-lowering treatment was associated with lower mortality. UK recommendations suggest that statin use should be based on clinical judgement informed by assessment of patient preference, comorbidities, polypharmacy, general frailty and life expectancy.’ [9]
Conclusions
Widespread statin use is consistent with the elevated risk of CVD in the over-80s but an age-related increase in deprescribing implies recognition of the limitations of preventive medical intervention, and a changing balance of benefits and harms in this age-group. Further research may be required to inform deprescribing decisions and promote deprescribing strategies where appropriate.
Supplementary Material
Key Points.
The frequency of statin use in people aged 80 to 105 years was evaluated
Statin prescription increased rapidly from 2001 to 2015 in men and women
Inception of statins was infrequent and decreased with age
Deprescribing was more frequent and increased with age and frailty level
Statin prescribing and deprescribing have both increased in the over 80’s. More evidence is needed concerning appropriate use of statins in this age group
Acknowledgements
This work was supported by the Dunhill Medical Trust [grant number: R392/1114]. MG was supported by the National Institute for Health Research (NIHR) Biomedical Research Centre at Guy’s and St Thomas’ NHS Foundation Trust and King’s College London.
Footnotes
Conflicts of Interest: None
References
- 1.Office for National Statistics. Estimates of the very old (including centenarians) London; Office for National Statistics: 2016. [Google Scholar]
- 2.Olshansky SJ, Ault AB. The fourth stage of the epidemiologic transition: the age of delayed degenerative diseases. Milbank Q. 1986;64:355–91. [PubMed] [Google Scholar]
- 3.O'Keeffe AG, Nazareth I, Petersen I. Time trends in the prescription of statins for the primary prevention of cardiovascular disease in the United Kingdom: a cohort study using The Health Improvement Network primary care data. Clinical epidemiology. 2016;8:123–32. doi: 10.2147/CLEP.S104258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Walley T, Folino-Gallo P, Stephens P, Van Ganse E, the EuroMedStat Group Trends in prescribing and utilization of statins and other lipid lowering drugs across Europe 1997–2003. British Journal of Clinical Pharmacology. 2005;60:543–51. doi: 10.1111/j.1365-2125.2005.02478.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Johansen ME, Green LA. Statin use in very elderly individuals, 1999-2012. JAMA Internal Medicine. 2015;175:1715–6. doi: 10.1001/jamainternmed.2015.4302. [DOI] [PubMed] [Google Scholar]
- 6.Shepherd J, Cobbe SM, Ford I, et al. Prevention of coronary heart disease with pravastatin in men with hypercholesterolemia. West of Scotland Coronary Prevention Study Group. The New England Journal of Medicine. 1995;333:1301–7. doi: 10.1056/NEJM199511163332001. [DOI] [PubMed] [Google Scholar]
- 7.Chokshi NP, Messerli FH, Sutin D, Supariwala AA, Shah NR. Appropriateness of Statins in Patients Aged ≥80 Years and Comparison to Other Age Groups. The American Journal of Cardiology. 2012;110:1477–81. doi: 10.1016/j.amjcard.2012.06.058. [DOI] [PubMed] [Google Scholar]
- 8.U.S. Preventive Services Task Force. Statin use for the primary prevention of cardiovascular disease in adults: US preventive services task force recommendation statement. JAMA. 2016;316:1997–2007. doi: 10.1001/jama.2016.15450. [DOI] [PubMed] [Google Scholar]
- 9.National Institute for Health and Care Excellence (NICE) Lipid modification. Cardiovascular risk assessment and the modification of blood lipids for the primary and secondary prevention of cardiovascular disease. London: NICE; 2014. Available from: http://www.nice.org.uk/nicemedia/live/13637/66552/66552.pdf. [PubMed] [Google Scholar]
- 10.Strandberg TE, Kolehmainen L, Vuorio A. Evaluation and treatment of older patients with hypercholesterolaemia. JAMA. 2014;312:1136–1144. doi: 10.1001/jama.2014.10924. [DOI] [PubMed] [Google Scholar]
- 11.Williams T, van Staa T, Puri S, Eaton S. Recent advances in the utility and use of the General Practice Research Database as an example of a UK Primary Care Data resource. Therapeutic Advances in Drug Safety. 2012;3:89–99. doi: 10.1177/2042098611435911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Herrett E, Gallagher AM, Bhaskaran K, et al. Data Resource Profile: Clinical Practice Research Datalink (CPRD) Int J Epidemiol. 2015;44:827–36. doi: 10.1093/ije/dyv098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Charlton J, Latinovic R, Gulliford MC. Explaining the decline in early mortality in men and women with type 2 diabetes - A population-based cohort study. Diabetes Care. 2008;31:1761–6. doi: 10.2337/dc08-0137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bhattarai N, Charlton J, Rudisill C, Gulliford MC. Coding, recording and incidence of different forms of coronary heart disease in primary care. PLoS One. 2012;7:e29776. doi: 10.1371/journal.pone.0029776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gulliford MCJ, Ashworth M, Rudd AG, et al. for the eCRT Research Team Selection of medical diagnostic codes for analysis of electronic patient records. Application to stroke in a primary care database. PLoS One. 2009;4(9) doi: 10.1371/journal.pone.0007168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Juutilainen A, Lehto S, Rönnemaa T, Pyörälä K, Laakso M. Type 2 Diabetes as a “Coronary Heart Disease Equivalent”. An 18-year prospective population-based study in Finnish subjects. 2005;28:2901–7. doi: 10.2337/diacare.28.12.2901. [DOI] [PubMed] [Google Scholar]
- 17.Clegg A, Bates C, Young J, et al. Development and validation of an electronic frailty index using routine primary care electronic health record data. Age and Ageing. 2016;45:353–60. doi: 10.1093/ageing/afw039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rockwood K, Song X, MacKnight C, et al. A global clinical measure of fitness and frailty in elderly people. Canadian Medical Association Journal. 2005;173:489–95. doi: 10.1503/cmaj.050051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Reeve E, Gnjidic D, Long J, Hilmer S. A systematic review of the emerging definition of ‘deprescribing’ with network analysis: implications for future research and clinical practice. British Journal of Clinical Pharmacology. 2015;80:1254–68. doi: 10.1111/bcp.12732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nicholas JM, Ridsdale L, Richardson MP, Grieve AP, Gulliford MC. Fracture risk with use of liver enzyme inducing antiepileptic drugs in people with active epilepsy: cohort study using the general practice research database. Seizure. 2013;22:37–42. doi: 10.1016/j.seizure.2012.10.002. [DOI] [PubMed] [Google Scholar]
- 21.Austin PC, Lee DS, Fine JP. Introduction to the Analysis of Survival Data in the Presence of Competing Risks. Circulation. 2016;133:601–9. doi: 10.1161/CIRCULATIONAHA.115.017719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.R Core Team. R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2016. [Google Scholar]
- 23.MRC/BHF Heart Protection Study of cholesterol lowering with simvastatin in 20536 high-risk individuals: a randomised placebo-controlled trial. The Lancet. 2002;360:7–22. doi: 10.1016/S0140-6736(02)09327-3. [DOI] [PubMed] [Google Scholar]
- 24.Scandinavian Simvastatin Survival Study G. Randomised trial of cholesterol lowering in 4444 patients with coronary heart disease: the Scandinavian Simvastatin Survival Study (4S) The Lancet. 1994;344:1383–9. [PubMed] [Google Scholar]
- 25.Rockwood K, Andrew M, Mitnitski A. A Comparison of Two Approaches to Measuring Frailty in Elderly People. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences. 2007;62:738–43. doi: 10.1093/gerona/62.7.738. [DOI] [PubMed] [Google Scholar]
- 26.Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K. Frailty in elderly people. The Lancet. 2013;381:752–62. doi: 10.1016/S0140-6736(12)62167-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Taylor F, Huffman MD, Macedo AF, et al. Statins for the primary prevention of cardiovascular disease. Cochrane Database Syst Rev. 2013;(1):CD004816. doi: 10.1002/14651858.CD004816.pub5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Afilalo J, Duque G, Steele R, Jukema JW, de Craen AJM, Eisenberg MJ. Statins for Secondary Prevention in Elderly PatientsA Hierarchical Bayesian Meta-Analysis. Journal of the American College of Cardiology. 2008;51:37–45. doi: 10.1016/j.jacc.2007.06.063. [DOI] [PubMed] [Google Scholar]
- 29.Savarese G, Gotto AM, Paolillo S, et al. Benefits of Statins in Elderly Subjects Without Established Cardiovascular DiseaseA Meta-Analysis. Journal of the American College of Cardiology. 2013;62:2090–9. doi: 10.1016/j.jacc.2013.07.069. [DOI] [PubMed] [Google Scholar]
- 30.Petersen LK, Christensen K, Kragstrup J. Lipid-lowering treatment to the end? A review of observational studies and RCTs on cholesterol and mortality in 80+-year olds. Age and Ageing. 2010;39:674–80. doi: 10.1093/ageing/afq129. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.