Abstract
Objective:
The aim of the study was to assess undernutrition and factors associated with, among people living with human immunodeficiency virus (HIV) and on antiretroviral therapy (ART).
Methods:
Facility-based cross-sectional study design was implemented. Data were collected using pretested structured questionnaire at ART service site. Basic descriptive statistics were computed. Bivariate and multivariate logistic regression analyses were used to assess the association between outcome variable and explanatory variables.
Results:
The prevalence of undernutrition (body mass index [BMI] ≤18.5 kg/m2) among patients on ART was 30%. The mean BMI was 20.3 with standard deviation ± 2.9 kg/m2. Undernutrition was significantly associated with CD4 (200-500) (adjusted odds ratio [AOR] = 0.576, 95% confidence interval [CI]: 0.338, 0.979) and CD4 >500 (AOR = 0.431, 95% CI: 0.239-0.778), duration on ART >12 months (AOR = 0.466, 95% CI: 0.224, 0.966), unable to get nutritional care and support (AOR = 2.188, 95% CI: 1.349, 3.549), diarrhea (AOR = 1.641, 95% CI: 1.036, 2.6), khat chewing (AOR = 0.589, 95% CI: 0.377, 0.92), and severe food insecurity (AOR = 1.594, 95% CI: 1.008, 2.521).
Conclusions:
Our study provides a unique insight into prevalence and associated factors of undernutrition which greatly affect ART outcomes. The study revealed that the undernutrition was found to be high and its problem in HIV-positive patients are interworsen. Diarrhea, severe food insecurity, nutritional care and support, khat chewing, CD4 >200/µl, and duration on ART >12 months were independently associated with undernutrition. Comprehensive nutritional assessment during follow-up and routine nutritional supplement therapy for undernutrition in conjunction with early start on ART need to be initiated.
Keywords: Acquired immune deficiency syndrome, antiretroviral therapy, body mass index, nutritional status, undernutrition
Introduction
Human immunodeficiency virus/acquired immunodeficiency syndrome (HIV/AIDS) is chronic epidemic highly challenging to the world, particularly to Africa. According to global HIV/AIDS report 2013, globally, about 35.0 million people were living with HIV at the end of 2013, and the number of newly infection cases had declined by 33% from 2001. An estimated 0.8% of adults from 15 to 49 years worldwide are living with HIV. Sub-Saharan Africa was the most severely affected region in the world and accounts about 71% of the peoples living with HIV worldwide.1
In Ethiopia, there are several interventions taken to prevent further spread of the disease and care for peoples living with HIV. According to single-point estimate and projections, the national prevalence rate of HIV was 1.14%.2 The 2011 Ethiopia Demographic Health Survey (EDHS) data show that the national prevalence was 1.5% with women proportionately infected 1.95 compared to 1% in men, and the urban prevalence is 4.2% which is 7 times higher than that of rural (0.6%). Furthermore, the regional variation shows ranges from 0.9% in Southern Nation Nationalities and people and 6.5% in Gambela. According to the EDHS 2011, the prevalence of Oromia regional state was 1.0%.3 Around 542,121 adults and 178,500 children under 15 years of age need antiretroviral therapy (ART) service and the coverage reached 76% for adult (age 15+) but remain low (23.5%) for children <15 years living with HIV.2
Antiretroviral (ARV) drugs improve the immune function of an individual’s living with HIV by suppressing the viral load of the patients. The word malnutrition refers for both overnutrition and undernutrition, and in this study, malnutrition is used for undernutrition which is more prevalent all over the world. One of the long-term causes of malnutrition is poverty, especially in Sub-Saharan Africa including Ethiopia. Undernutrition occurs when peoples take insufficient food which do not met their calorie need for growth and energy.4
Sub-Saharan Africa is the home of most nutritionally unsecured communities in the world. Poor infrastructure, limited resource with conflict, HIV, and lack of access to health service coverage are the main factors contribute to malnutrition challenging in the continents.5 Globally, over 805 million people are undernourished, and majority of the number are from developing countries, which was most of the time influenced by seasonal variation.6 Poor nutrition and HIV disease progression are a part of a vicious cycle that contributes to further deterioration of the health of patients and that ultimately leads to death. Adequate nutrition is necessary to manage opportunistic infections, maintain the immune system, optimize response to medical treatment, and support optimal quality of life for people living with HIV (PLWHA).7,8
Both malnutrition and HIV are major public health problems which contribute to high morbidity and mortality particularly in Sub-Saharan Africa. Malnutrition advances the progression of HIV by decreasing dietary intake and affecting physiologic metabolism.1,9 HIV affects nutritional status of individuals by increasing energy requirement and in another way affecting nutrient metabolism and absorptions.10-12 Food insecurity and malnutrition enforce the community to the risk of developing HIV infection when they accomplish different activities to acquire their daily food.13 The objective of this study was to assess undernutrition and factors associated with among PLWHA and on ART.
Methods
Study setting, design, and population
Facility-based cross-sectional study was conducted in four hospitals found in East Hararge zone of Oromia regional state from April to July 2016. East Hararge zone is found in Oromia regional state Eastern part of Ethiopia and has estimated total population of around 3.5 million according to the Central Statistical Agency in 2008. The zone has five hospitals, and of them, four are providing ART services. Patients on ART at ART clinic of Bisidimo, Deder, Haramaya, and Garamuleta Hospital were included in the study. The source population were all adult HIV-positive individuals who were currently on ART. The study population were all HIV-positive adults who were currently on ART in four selected hospitals providing ART service. Randomly selected adult HIV-positive individuals currently on ART in the selected hospitalswere taken as sample population.
Inclusion and exclusion criteria
All HIV-positive adults ≥18 years old who were on ART for at least 1 month were included in the study. Patients with difficulty to stand, pregnant mothers, mentally ill, and severely ill patients were excluded from the study.
Sample size determination and sampling technique/procedure
Sample size was calculated using single population proportion formulas with assumptions of: 95% confidence level (Zα/2) 1.96, prevalence of malnutrition (body mass index [BMI] <18.5%) 25.2%14 degree of precision (d) 3%, and total current on ART report of four hospitals (N) 868. The sample size (n) was then calculated using software Epi info version 3.3.2 and gave 459 with 10% nonresponsive rate consideration.
Four ART service providing hospitals in East Hararge zone were selected for the study. The proportion of subjects required from each health institutions was calculated according to their monthly case load. Systematic random sampling technique was used to select the study subjects from each facility. Health facility registration book serial number was taken during data collection, and the study subjects were selected by calculating K. Finally, the study subjects were selected every two patients from the registration book.
Data collection tool and procedure
The structured and pretested questionnaire which was adopted and modified from literature review was administered to gather all sociodemographic information, behavioral, patient-related factors, household assets, and food security. Data abstraction format was used to collect secondary data such as hemoglobin (Hgb) level, World Health Organization (WHO) clinical stage, adherence status, functional status of the patients, and CD4 counts from patient’s medical record (ART follow-up card) and registration book. Pretest was conducted at Babile Health Center which was not included in the study. A total of four supervisors and four trained data collectors carried out the total field work. ART nurse at ART sites supervised the data collection process to ensure completeness and consistency of the data.
Variables and measurement
The dependent variable wasundernutrition among adult HIV-positive patients, and the explanatory variables were age, sex, residence, religion, ethnic group, marital status, educational status, occupation, wealth, food security scales, nutritional care and support, nutritional counseling, adherence, functional status, duration of ART, CD4 counts, the WHO clinical stages, Hgb status, opportunistic infections like diarrhea, tuberculosis (TB), difficulty of eating, skin infection, and other problems, alcohol consumption, cigarette smoking, and khat chewing.
Anthropometric measurement (weight and height) of the patients was carried out by the data collectors using light cloths and bare foots calibrate to the nearest 0.5 kg and 0.5 cm, respectively. The height of the patient was measured on standing in Frankfurt position, and the weight was measured on standing scale. BMI was calculated as weight in kilogram divided by height in meter square (kg/m2). The wealth index questions were adopted from EDHS survey to collect common household assets, and wealth index was estimated by factor analyses. The food insecurity status was assessed by HFIAS of different nine standard questions adopted from the Food and Nutrition Technical Assistance.2 Level of food insecurity category was declared by the response of the participant to the questions. Undernutrition was measured by BMI and defined as BMI <18.5 kg/m2. ARTadherence level was measured by patient self-report. It was defined as good if ≥95% (the patients missed ≤2 dose of 30 doses), fair if the average adherence ≥85-94% (the patient missed 3-5 dose of 30 doses), and poor if the average adherence is ≤84% (the patient missed ≥6 doses from 30 doses). Food security is a condition access by all people at all the time to enough food for an active health life and categorized as food secure, mild food insecure, moderate food insecure, and severe food insecure.
Data processing and analysis
The data were entered to EPi data version 3.0, and then, it was exported to SPSS version 20 for analysis. Basic descriptive summaries of the patient characteristics and the outcome interest were computed. Frequency, ratio, and other measure of central tendency were computed accordingly. Bivariate and multivariate logistic regression analyses were used to assess the effect of explanatory variables on undernutrition. Finally, the explanatory variables significantly associated with undernutrition (P ≤ 0.05) in bivariate analyses were taken to multivariate logistic regression to declare independent predictors of undernutrition. Odds ratio along with 95% confidence interval (CI) was estimated to measure the strength of association.
Ethical considerations
Primarily, ethical clearance was obtained from the Institutional Health Research Ethical Review Committee of Haramaya University, College of Health and Medical Science. The participants were told that they have full right to participate or not. During the data collection period, name of the patient was not taken, and information obtained were not shared to any other third party.
Result
Sociodemographic characteristic of the study participant
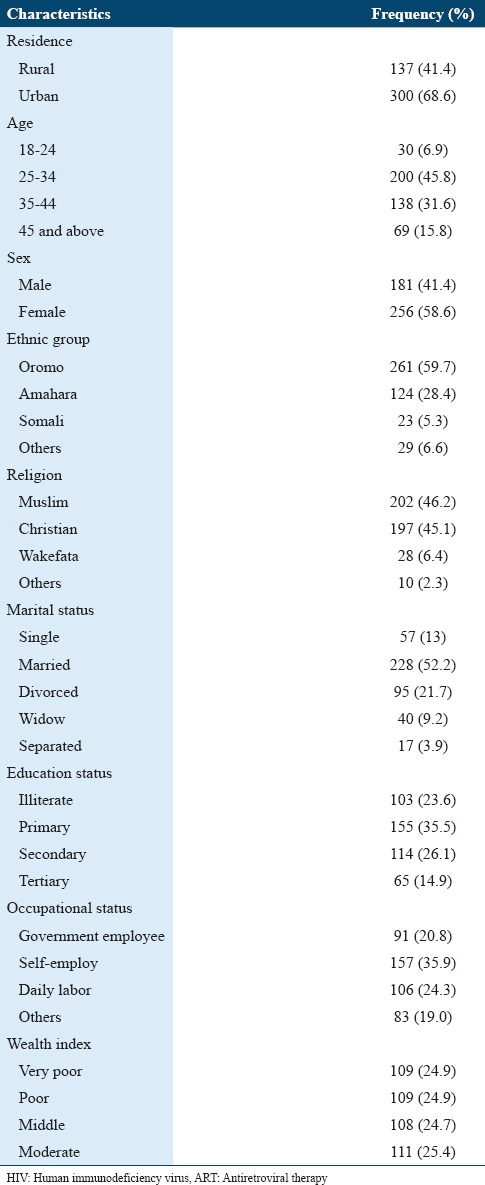
A total of 437 adult on ART participated in the study making a response rate of 95% and 256 (58.6%) of them were females. As portrayed in Table 1, most of the participants were from urban area 300 (68.6%), majority of the participant were in age group of 25-34 with mean age of 35.0 (standard deviation [SD]: ±8.307) years, and 202 (46.2%) were Muslim in religion. Greater parts of the respondents were married 228 (52%), and about 35.5% of them attended primary school. 261 (59.7%) were Oromo ethnic group, and the remaining were Amahara (28.4%), Somali (5.3%), and others (6.6%). Regarding occupation of the participants, about 35.9% were self-employed (Table 1).
Table 1.
Sociodemographic and economic characteristic of HIV-positive adults on ART in hospitals, Eastern Ethiopia, 2016
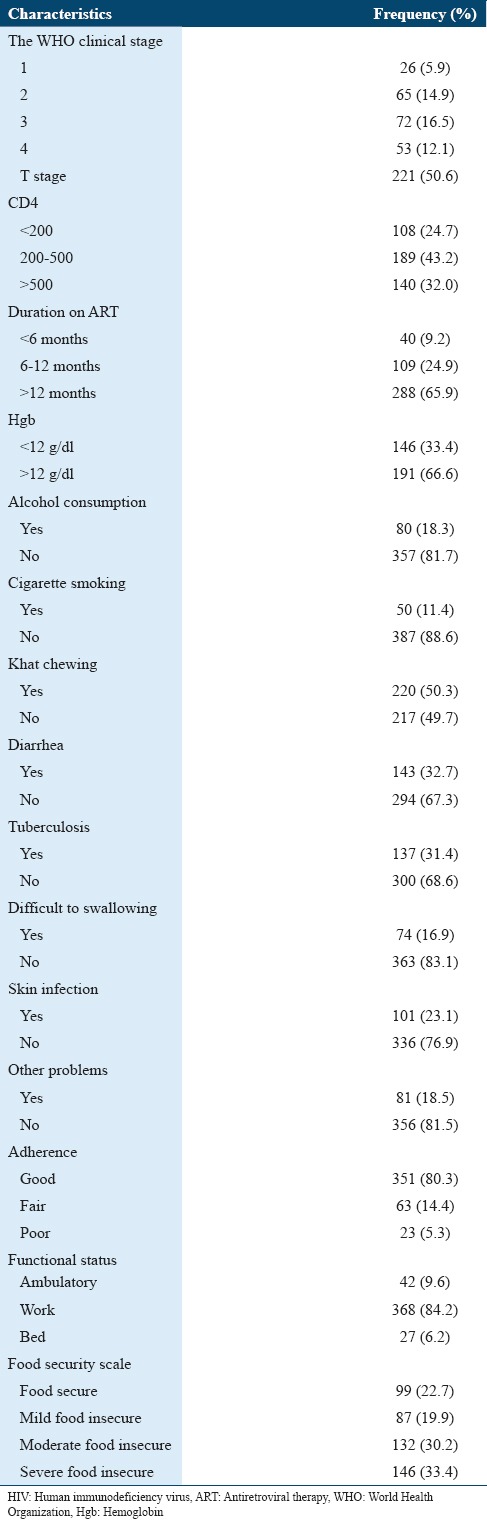
Treatment related, behavioral, and food security characteristic of study participants
Large number of the respondents had good adherence 351 (80.3%), higher percent of them were on the WHO T stage 50.6%, and greater part of the respondents (84.2%) were in working functional status. Most of the respondents involved in the study (70%) were on ART for >12 months. From the study participants, half (50%) of them chew khat, and 18.3% and 11.4% drink alcohol and smoke cigarette, respectively. 146 (33.4%) of the study participants developed anemia. Diarrhea and TB were the two leading opportunistic infections that caused morbidity in HIV-positive patients. The study identified that 32.7% and 31.4% of the study subjects developed diarrhea and TB, respectively. Large number of the respondents (33.4%) were living under severe food insecurity, whereas 30.2% were under moderate food insecurity, 19.9% under mild foods insecurity, and 22.7% were food secured. Greater part (75.5%) of the respondents did not get nutritional care and support, and more of them (84.2%) got nutritional counseling from the health worker (Table 2).
Table 2.
Clinical, behavioral, and food security characteristics of HIV-positive adults on ART in hospitals, Eastern Ethiopia, 2016
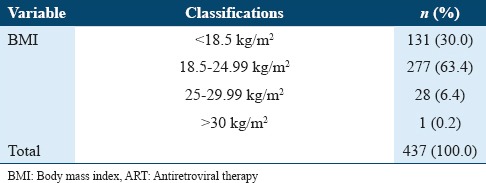
Nutritional status of study participant
The prevalence of undernutrition (BMI ≤18.5 kg/m2) was 30%, whereas 63.4% and 6.4% of the study subjects were normal BMI (18.5-24.99 kg/m2) and overweight (BMI 25-29.99 kg/m2), respectively. The mean BMI was 20.3 SD ± 2.9 kg/m2. Undernutrition was more common in female which was 33.2% and 25.4% among male participants. Prevalence of undernutrition varies by age group of the study subjects. From 131 (30%), undernourished study subjects (40.7%) were in 18-24 years age range while 33.5% of study subjects were in 25-34 years age range (Table 3).
Table 3.
Nutritional status of patients on ART in hospitals, Eastern Ethiopia, 2016
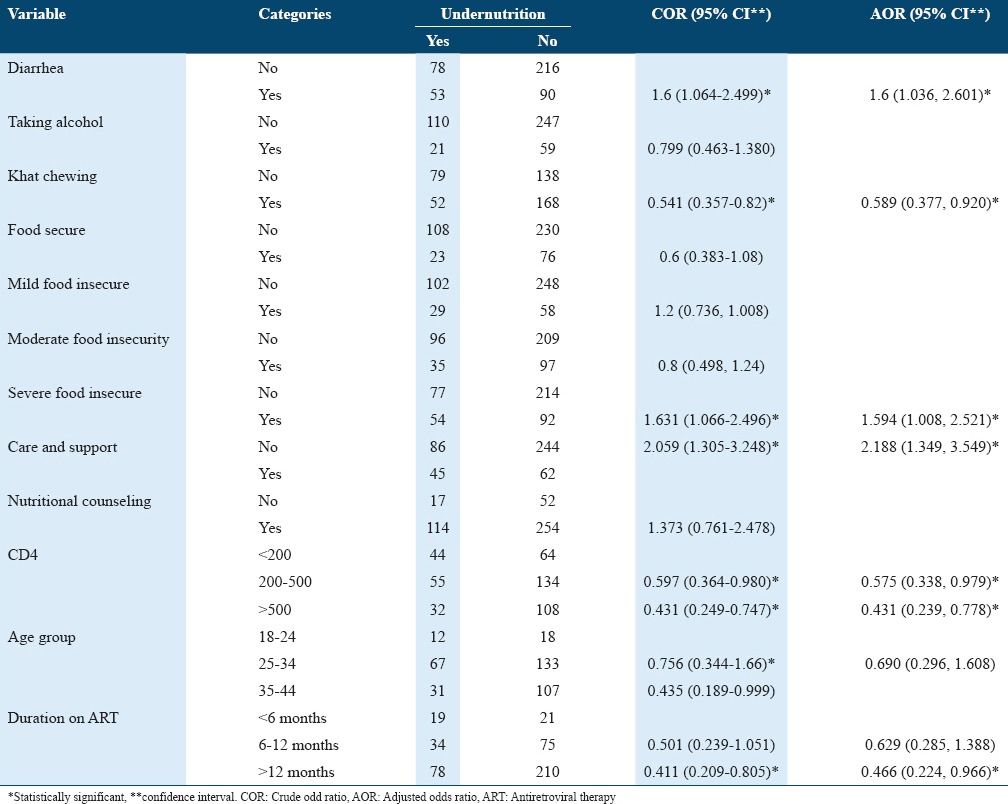
Factors associated with undernutrition
Multivariate logistic regression was used to identify predictors of the outcome variable. Variables associated with the outcome variable in bivariate logistic regression analysis were directly taken to multivariate logistic regression analysis. After controlling possible confounding effects of other covariates, those who were in 25-34 age group were 0.69 times less likely undernourished as compared to those in 18-24 age group (adjusted odds ratio [AOR] = 0.69, 95% CI: 0.296, 1.608). Concerning clinical factors, CD4 count 200-500, and >500 were less likely undernourished as compared to those with CD4 <200, and they were statistically associated with undernutrition at (AOR = 0.6, 95% CI: 0.338-0.979) and (AOR = 0.4, 95% CI: 0.239-0.778), respectively. Those survived on ART for greater than a year were 0.46 less likely undernourished as compared to those survived <6 months on ART (AOR = 0.466, 95% CI: 0.224, 0.966). Regarding behavioral factors, those who chew khat were 0.589 less likely undernourished as compared to their counterparts (AOR = 0.589, 95% CI: 0.377-0.92). Adults who developed diarrhea were 1.64 times more likely undernourished as compared to their counterparts (AOR = 1.64, 95% CI: 1.306-2.6). As food security scale is concerned, those severely food insecure were 1.59 times more likely undernourished as compared to food secured (AOR = 1.59, 95% CI: 1.008, 2.5). Adult PLWHA who did not got nutritional care and support were 2.188 times more likely undernourished (AOR = 2.188, 95% CI: 1.35, 3.55) as compared to their counterparts (Table 4).
Table 4.
Factors associated with undernutrition among the patients on ART in hospitals, Eastern Ethiopia, 2016
Discussion
Undernutrition and HIV independently cause immune suppression, and one exacerbates the other by vicious cycle and increases susceptibility to infection. Since the initiation of ART could not resolve undernutrition, nutritional status depends on the duration of ART. This study was designed to assess the undernutrition among HIV-positive adults on ART and associated factors in four selected East Hararge zone hospitals.
The number of female population in this study exceeds that of male which shows high HIV infection among female (58.6%). There was high prevalence of HIV infection among female as mentioned in EDHS 2011 report. According to this study, undernutrition mostly affected females (33.2%) and it was a bit higher than the prevalence of malnutrition among HIV-infected women in Ethiopia (13.2%), as indicated by meta-analysis in 11 Sub-Saharan African countries.15 It is also similar with different pocket studies in Ethiopia.16-18
Large number of subjects following ART in this study were in age group of 25-34 years (45.8%) because of high prevalence of HIV infection in this group has also seen in AID in the Ethiopia sixth report 2013 and EDHS 2011 report. Age-specific undernutrition was also highly prevalent in this age group next to 18-24 years.
Healthy nutrition plays a central role in the management of HIV/AIDS, especially those symptoms such as diarrhea, anorexia, sore mouth, fever, and muscle wasting - directly associated with the disease. Adequate dietary intake enhances the therapeutic effect of medicines, boosts the immune system (thus helping to fight against the disease and to maintain body weight), prolongs the progression of HIV infection to AIDS, increases longevity, and promotes healthy living. The overall prevalence of undernutrition (BMI <18.5 kg/m2) was 30% which is relatively lower than the cross-sectional study conducted in china on adult LWHIV (37.2%) and Bahirdar northwest Ethiopia on current on ART (63.5%).19,20 The prevalence of undernutrition was reported different in different parts of Ethiopia. In Jima University referral hospital, the prevalence of malnutrition among adults on ART was 46.8%17 which was high as compared to this finding and 12.3% in Dilla University referral hospital south part of Ethiopia which was lower as compared to this study. On the other hand, the prevalence of malnutrition among adults living with HIV in Kenya was 9.8% and Gonder northwest of Ethiopia was 27.8%.21,22 This different result of malnutrition among different parts of the country shows that there is existence of different socioeconomic and other factors that predispose the community to the problem, probably different feeding styles of different ethnic groups in the country.
According to the finding of this research, there was statistically significant association between nutritional care and support and undernutrition. Patients who did not get care and support were two times more likely undernourished as compared to their counterparts. This might be due to protein diet encouragement through nutritional care and support to build the muscle, organ, and strong immune system, which increase the nutritional status of the patient. Since morbidity of HIV increases the energy requirement and advancing undernutrition, low dietary intake leads to improper metabolism. This was in contradiction with the studies conducted in East Wollega, Oromia regional state, and Gonder referral hospital northwest Ethiopia which shows that there is no statistically significant association between nutritional care and support with undernourished.18,22 Diarrhea was the most common from opportunistic infection occurs on people LHIV. This study found significant association between diarrhea and undernutrition. From the respondents who develop diarrhea were 1.6 times more likely undernourished as compared to their counterparts.
HIV-related infection such as TB and diarrhea has severe nutritional consequences.23 This finding is in line with the idea of the WHO that diarrhea has significant effect on undernutrition of the respondents. This may be due to reducing dietary intake and nutrient absorption. On the other hand, the research conducted at Butajira Hospital shows that diarrhea has no effect on undernutrition.16
Severe food insecurity was found to have significant association with undernutrition. Adult people HIV positive on ART who have severe food insecurity were 1.6 times more likely undernourished as compares to those foods secure. Similarly, the study conducted in Nepal shows household with food insecure have highest odds of being undernourished while this result was in opposite with research conducted in Butajira Hospital south Ethiopia.16,24 This was obviously due to lack access to sufficient food to meet dietary needs for productive and health life, and it leads to deficiency of macro and micronutrient.
Regarding CD4, there was significant association between CD4 200-500 and >500 with undernutrition. Patients who have high CD4 count >200 cell/mm3 were approximately half times less likely undernourished as compared to those with CD4 <200 cell/mm3. This is due to immune (resistance) against infection. Similarly, the study conducted in Senegal shows that CD4 was significantly associated with less CD4 count.25 Furthermore, the finding from Jima Specialized Hospital indicates that CD4 has significant effect on undernutrition; patients having baseline CD4 count <200 cell/µl was 5.7 times more malnourished.17 In other side, the finding of the research conducted in Dilla University Hospital southern part of Ethiopia shows that CD4 has no significant effect on undernutrition.26 This was in opposite to our finding, and probably the difference may be due to variation in study population and period.
The study revealed that khat chewing has significant effect on undernutrition. Adults HIV positive on ART were half times less likely undernourished. In other side, behavioral factors such as alcohol and smoking were found to have no significant association with undernutrition.24 Ever khat chewing while on ART has no significant effect on undernutrition.27 Since the study did not collect the amount and dose of khat consumption in time period, it may not induce the complication with khat chewing such as poor appetite, constipation, and other gastrointestinal problems.
After controlling the effect of confounding variables, patients who survived on ART for >12 months were 0.5 less likely undernourished as compared to those on ART for <6 months. Similarly, the study conducted in north central Nigeria and University of Gondar Northwest Ethiopia supports this study.22,28 This may be due to ARV drug improvement of immune status of the patient against opportunistic infection promoting healthy life.
As a limitation, using cross-sectional study design could not represent the whole time of undernutrition effects which limits the cause-and-effect relationship. Recall bias was the limitation of this study when measuring household food insecurity scales and household asset. Moreover, in using anthropometric measurement (BMI) to assess, the nutritional status of participant do not show the fat distribution of participant. The study did not include patients on ART who were taking ART in private health facilities.
Conclusion and Recommendations
In summary, our study provides a unique insight into prevalence and associated factors of undernutrition which greatly affect ART outcomes. The study revealed that the undernutrition was found to be high and its problem in HIV-positive patients is interworsen. Diarrhea, severe food insecurity, nutritional care and support, khat chewing, CD4 >200/µl, and duration on ART >12 months were independently associated with undernutrition. Comprehensive nutritional assessment during follow-up and routine nutritional supplement therapy for undernutrition in conjunction with early start on ART need to be initiated.
Acknowledgment
The authors would like to thank Haramaya University Health and Medical Science College staff for their support through the research work. We also acknowledge East Hararge zone health department, supervisors, and data collectors for their support and active cooperation during the study period.
References
- 1.WHO. Global Report UNAIDS Report on the Global AIDS Epidemic Joint United Nations Programme on HIV/AIDS (UNAIDS) Global Report. 2013. [[Last accessed on 2016 Mar 20]]. Available from: http://www.unaids.org/sites/default/files/media_asset/UNAIDS_Global_Report_2013_en_1.pdf .
- 2.Fmoh E. National Guideline for Comprehensive HIV Prevention, Care and Treatment, Guidleine. 3rd ed. Federal Democratic Republic of Ethiopia; 2014. [Google Scholar]
- 3.CSA. Ethiopia Demographic and Health Survey Survey. 2011. [[Last accessed on 2016 Mar 20]]. p. 3. Available from: https://www.dhsprogram.com/pubs/pdf/FR255/FR255.pdf .
- 4.Koeth R, John HC. Nutritional aspects of HIV-associated wasting in sub-Saharan Africa. Am J Clin Nutr. 2010;91:1–7. doi: 10.3945/ajcn.2010.28608D. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jeica F. UNDP Report on the Nutrition Challenge in Sub-Saharan Africa, Rome. 2012. [[Last accessed on 2016 Mar 10]]. pp. 1–70. Available from: http://www.undp.org/content/dam/rba/docs/Working%20Papers/Nutrition%20Challenge.pdf .
- 6.FAOI WFP. The State of Food Insecurity in the World, Strengthening the Enabling Environment for Food Security and Nutrition. 2014. [[Last accessed on 2016 Mar 20]]. pp. 1–57. Available from: http://www.fao.org/3/a-i4030e.pdf .
- 7.Ivers LC, Cullen KA, Freedberg KA, Block S, Coates J, Webb P. HIV/AIDS, undernutrition, and food insecurity. Clin Infect Dis. 2009;49:1096–102. doi: 10.1086/605573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fanta. Food and Nutrition Implications of Antiretroviral Therapy in Resource Limited Settings. 2016. [[Last accessed on 2016 Mar 23]]. pp. 1–2. Available from: http//www.pdf.usaid.gov/pdf_docs/Pnacw463.pdf .
- 9.Stephen D. World AIDS day the role of nutrition in living with HIV/AIDS. J Trop Med Int Health. 2008;12:48–56. [Google Scholar]
- 10.Bonnard TC, Bruce C, Leslie E, Sandra R. Caroline Nutrition and HIV/AIDS: Evidence, Gaps, and Priority Actions Academy for Educational Development (AED) Prepared by Ellen Piwoz of the Support for Analysis and Research in Africa (SARA) Project with Inputs from Patricia Journal. 2006:1–6. [Google Scholar]
- 11.WHO. Nutrient Requirements for People Living with HIV/AIDS, Report of Technical Consultation. Geneva: WHO; 2003. [[Last accessed on 2016 Mar 20]]. p. 5032. Available from: http//www.who.int/nutrition/publications/Content_nutrient_requirements.pdf . [Google Scholar]
- 12.FMOH-E. National Guideline for Comprehensive HIV Prevention, Care and Treatment, Guidline. 2nd ed. FMOH-E; 2008. [Google Scholar]
- 13.Tiyou A, Belachew T, Alemseged F, Biadgilign S. Food insecurity and associated factors among HIV-infected individuals receiving highly active antiretroviral therapy in Jimma zone Southwest Ethiopia. BMC Nutr J. 2012;11:1–9. doi: 10.1186/1475-2891-11-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gedle D, Gelaw B, Mesele DM. Prevalence of malnutrition and its associated factors among adult people living with HIV/AIDS receiving anti-retroviral therapy at Butajira Hospital, southern Ethiopia. BMC Nutr. 2015;5:8–14. [Google Scholar]
- 15.Uthman OA. Prevalence and pattern of HIV-related malnutrition among women in sub-Saharan Africa: A meta-analysis of demographic health surveys. BMC Public Health. 2008;8:1471–83. doi: 10.1186/1471-2458-8-226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gedle D, Mekuria G, Kumera G, Eshete T, Fayera F, Kumera G, et al. Food insecurity and its associated factors among adult people living with HIV/AIDS receiving anti-retroviral therapy at Butajira Hospital, southern. Ethiop J Nutr Food Sci. 2015;5:1–7. [Google Scholar]
- 17.Mulu H, Hamza L, Alemseged F. Prevalence of malnutrition and associated factors among hospitalized patients with acquired immunodeficiency syndrome in Jimma University Specialized Hospital, Ethiopia. Ethiop J Health Sci. 2016;26:217–26. doi: 10.4314/ejhs.v26i3.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Alemayehu K, Garoma S, Gemede HF. Assessment of adult nutritional status and associated factors among ART users in Nekemte Referral Hospital and Health Center, East Wollega Zone. Ethiop J Nutr Food Sci. 2013;3:67–73. [Google Scholar]
- 19.Hu W, Jiang H, Chen W, He SH, Deng B, Wang WY, et al. Malnutrition in hospitalized people living with HIV/AIDS: Evidence from a cross-sectional study from Chengdu, China. Asia Pac J Clin Nutr. 2011;20:544–50. [PubMed] [Google Scholar]
- 20.Daniel M, Mazengia F, Birhanu D. Nutritional status and associated factors among adult HIV/AIDS clients in Felege Hiwot Referral Hospital Bahir Dar. Ethiop Sci J Public Health. 2013;1:1–8. [Google Scholar]
- 21.Jayne J, Scrimgeour AG, Polhemus ME, Otieno L, Bovill ME. Dietary and socio-economic correlates of nutritional status in a rural adult Kenyan population. Afr J Food Agric Nutr Dev. 2011;11:1–7. [Google Scholar]
- 22.Wasie B, Kebede Y, Yibrie A. Nutritional status of adults living with HIV/AIDS at the university of Gondar Referral Hospital, northwest Ethiopia. J Health Biomed Sci. 2010;3:14–27. [Google Scholar]
- 23.WHO. Nutrient Requirements for People Living with HIV/AIDS. Report of Technical Consultation. Geneva: WHO; 2003. [[Last accessed on 2016 Mar 12]]. pp. 1–5. Available from: https://www.amazon.com/State-Food-Insecurity-World-Strengthening/dp/9251085420 . [Google Scholar]
- 24.Thapa R, Amatya A, Pahari DP, Bam K, Newman MS. Nutritional status and its association with quality of life among people living with HIV attending public anti-retroviral therapy sites of Kathmandu Valley, Nepal. AIDS Res Ther. 2015;12:14. doi: 10.1186/s12981-015-0056-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Benzekri NA, Sambou J, Diaw B, Sall EH, Sall F, Niang A, et al. High prevalence of severe food insecurity and malnutrition among HIV-infected adults in Senegal, West Africa. PLoS One. 2015;10:67–77. doi: 10.1371/journal.pone.0141819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hailemariam S, Girma T, Henok T. Malnutrition: Prevalence and its associated factors in people living with HIV/AIDS, in Dilla University Referral Hospital. BMC Public Health. 2013;13:1–8. doi: 10.1186/0778-7367-71-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Berhe N, Tegabu D, Alemayehu M. Effect of nutritional factors on adherence to antiretroviral therapy among HIV-infected adults: A case control study in Northern Ethiopia. BMC Infect Dis. 2013;4:1–8. doi: 10.1186/1471-2334-13-233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Banwat ME, Yakubu NW, Olalude EO, Ogunsakin JA. An assessment of the nutritional knowledge, practice and status of adult HIV/AIDS patients attending an ART centre in Jos, north central Nigeria. J Health Care Curr Rev. 2013;1:10–9. [Google Scholar]


