Abstract
Dislodged intrabiliary drainage devices, including catheters, endoprostheses, and stents, may further impair drainage and cause various local reactions, vascular and gastrointestinal tract complications. Endoscopic approaches for management of plastic biliary endoprostheses have been extensively discussed. However, in rare cases of fracture of percutaneous transhepatic biliary drainage (PTBD) catheters, only a percutaneous transhepatic technique for retrieving should be applied to avoid further damage by its rigid fragment. We present the adjusted techniques using either a goose neck snare, over-the-wire balloon catheter, or biopsy forceps with image demonstration and reviews. We encountered two patients with PTBD tube fracture and intrahepatic dislodgment. In both patients, percutaneous approaches were used for successfully retrieving and removing the fractured catheter through transhepatic tract: one with the use of a biopsy forceps, another with an inflatable balloon catheter.
Intrabiliary devices, including percutaneous transhepatic biliary drainage (PTBD) catheter, plastic biliary endoprostheses (PBE), and metallic stents are widely used for relieving biliary occlusion in patients with inoperable tumors and benign, postinflammatory, or iatrogenic strictures. These devices are placed at the stricture site using minimally invasive procedures via endoscopic retrograde cholangiopancreatography (ERCP) or ultrasound- and fluoroscopy-guided percutaneous transhepatic route.
Dysfunction of the implanted devices from occlusion, migration, or malposition is occasionally encountered, and various complications can occur if the dysfunctional device is not retrieved. These include impaired biliary drainage, local inflammation and stricture, recurrent cholangitis, perforation of hepatic capsule causing biloma or abscess formation, erosion of the adjacent vasculature causing bleeding or pseudoaneurysm, and bowel obstruction or perforation if the fragment freely migrates through gastrointestinal tract (1).
Intervention with minimally invasive ERCP or percutaneous approach are the initial options, while open surgery is performed only when these procedures fail. Compared with plastic PTBD drainage catheters, PBEs have a soft tip and a flexible body. Therefore, variable forms of either ERCP or percutaneous techniques are suitable options, with the reported success rate of 80%–90% (1, 2). However, in extremely rare cases of fracture of rigid PTBD catheters, the percutaneous method may be the optimal solution for retrieving the fragment and avoiding further complications.
Technique
In our institute, PTBD is performed routinely under combined ultrasound and fluoroscopic guidance. A plastic ring biliary drainage catheter (Cook Medical) with the appropriate length and number of side holes is placed through stricture site. The rigid ring catheter is retained for at least 14 days and subsequently replaced with a more flexible silicon (Cliny) or pigtail (Cook Medical) catheter.
The patient database was retrospectively reviewed from 2012 to 2014, and two cases of catheter fracture and intrahepatic dislodgment out of 689 procedures of PTBD were found during this time period, the incidence being 0.3%. Informed consent for image-guided invasive PTBD is routinely acquired; and the retrospective review of patient information is approved by the Institutional Review Board of our hospital.
Case 1
A 71-year-old man with history of hepatitis B-related hepatocellular carcinoma underwent deceased donor liver transplant after local control of tumor. The procedure was complicated with choledocho-jejunostomy stenosis and recurrent biliary tract infection, resulting in right lobe atrophy. Therefore, PTBD was performed through the left lobe.
The catheter size was gradually increased over a period of one year, and a 14 and 8.5 French (F) dual pigtail catheters were used for sufficient dilation of the stricture site. During a routine catheter change, an accidental intrahepatic withdrawal of the dual catheter occurred after cutting the external end.
For catheter retrieval, we threaded a 0.035-inch hydrophilic stiff guidewire (Merit Medical Systems) through the tract and along-side the catheter, then a 14 F angiosheath (Merit Medical Systems) was used to further secure the tract. A 7 F biopsy forceps (Cordis Corporation) was inserted through the angiosheath, to grab the end of the fractured catheter and successfully retrieve it (Fig. 1).
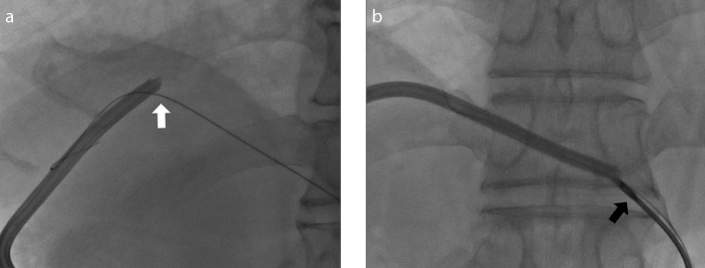
Figure 1. a, b.
A 71-year-old male post-liver transplant complicated with stenosis of choledocho-jejunosotmy. Percutaneous transhepatic biliary drainage (PTBD) with 14 and 8.5 F dual pigtail catheters was placed via left lobe. A stiff guidewire (a, white arrow) inserted through the transhepatic tract and placed alongside the dislodged catheter fragment. A 7 F biopsy forceps (b, black arrow) was advanced through an 8 F angiosheath firmly griping the end of the catheter fragment. The dislodged fragment was removed.
Case 2
An 88-year-old man with cholangiocarcinoma invading the caudate lobe and segments 7 and 8 of liver presented with elevated liver enzymes and jaundice. Abdominal computed tomography showed obstruction of the first-order bile ducts, and dilation of bilateral intrahepatic ducts. Palliative PTBD was performed, and 8.3 F ring catheters, with tips proximal to the stenotic segment, were placed in both lobes.
Drainage from ring catheter in the right lobe reduced 13 days after the initial placement. Fracture and intrahepatic withdrawal of catheter was found under fluoroscopy. After removing the extrahepatic fragment, we introduced a 0.035-inch hydrophilic stiff guidewire into the percutaneous tract and successfully threaded the end-hole of the fractured catheter. An 8 F angiosheath was used according to the diameter of the transhepatic tract. Finally, because the working space was relatively small for biopsy forceps manipulation, a balloon dilatation catheter (Wanda; Boston scientific) was partially introduced within the catheter and inflated. The entire unit (fractured catheter, guidewire, angiosheath, and balloon) was retrieved, and the guidewire was successfully reintroduced into the mature intrahepatic tract (Fig. 2).
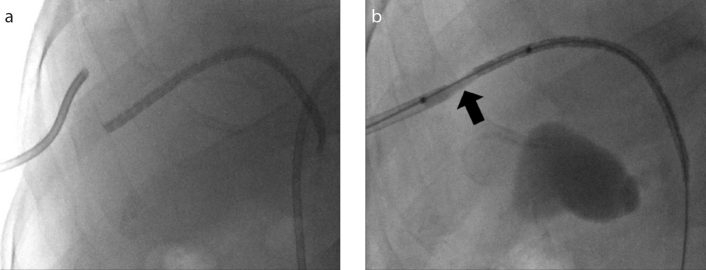
Figure 2. a, b.
An 88-year-old male with cholangiocarcinoma received palliative PTBD via right lobe. Follow-up cholangiogram on Day 13 (a) showed fracture of the rigid ring biliary catheter. The two fragments are not aligned. A 0.035-inch stiff guidewire was threaded through end-hole of the catheter fragment (b), then an inflatable balloon catheter was introduced in a partial-in-partial-out manner and inflated (the partially inflated balloon catheter indicated by black arrow). The catheter fragment was removed and finally a new drainage catheter was placed.
The dislodged catheters in both cases were successfully removed through the percutaneous tract under fluoroscopic guidance, and new catheters were placed. Bile was drained smoothly without visible hemobilia, indicating that there is no immediate bile duct or vessel injury during the retrieval procedure by using an angiosheath as protection. Moreover, hematologic examination of both patients revealed stable levels of bilirubin, hemoglobin, white cells, and liver enzymes. Follow-up X-ray and cholangiogram confirmed the appropriate position and function of catheters.
Discussion
PTBD is a highly efficient procedure for external and internal drainage in biliary obstruction and provides access for placement of metallic stents or plastic endoprostheses. But its clinical applications are slowly declining because of considerably high incidence of procedural and drainage-related complications. The onset of procedure-related complications, including pain, hemobilia, bleeding, cholangitis, fever, and sepsis, is generally observed immediately or within 48 hours of catheter placement and may result in death. Drainage-related complications including occlusion, migration, malposition and, rarely, catheter breakage usually occur later (3).
Breakage or fracture of percutaneous catheters, often results in intrahepatic retention of segments of the fractured catheter and requires immediate management. In these cases, ERCP techniques commonly used for dislodging PBEs are generally inapplicable because fragments of PTBD catheters are rigid, bulky, and with sharp edges, preventing its safe passage through the gastrointestinal tract. If a catheter fragment is pushed into bowel loops as with PBEs, rates of complications, such as bowel obstruction, perforation, or fistula formation (4), may be much higher. Whereas a percutaneous approach using the already established transhepatic tract is a safe alternative that also avoids the discomfort of endoscopy procedures.
Reports on percutaneous techniques have mainly focused on PBEs, describing several techniques for dislodging and pushing the fragment into bowel loops (1, 2, 5, 6). Here we focus on the management of fractured PTBD catheters, emphasizing on percutaneous retrieval techniques.
During percutaneous approach, an angiosheath is recommended for protecting the liver parenchyma against trauma from sharp edges of the fractured catheter. Furthermore, a mature tract is required for reestablishing biliary drainage after removal of fragment (1, 2). Devices such as a goose neck snare, an over-the-wire balloon catheter, or biopsy forceps, may be adapted and adjusted for catheter retrieval.
In case of goose neck snare, the peripheral free end of the catheter fragment is captured with the complete-circled-noose, securely grasped with continuous traction, and removed (1, 2).
When using over-the-wire balloon catheter, a guidewire is introduced into the percutaneous transhepatic tract and threaded through the catheter fragment using coaxial or monorail delivery systems. Then an over-the-wire balloon catheter can be completely or partially inflated within lumen of the catheter, and pulled through the tract. However, threading of the catheter is highly operator- and skill-dependent and time-consuming with high radiation exposure to both the operator and the patient.
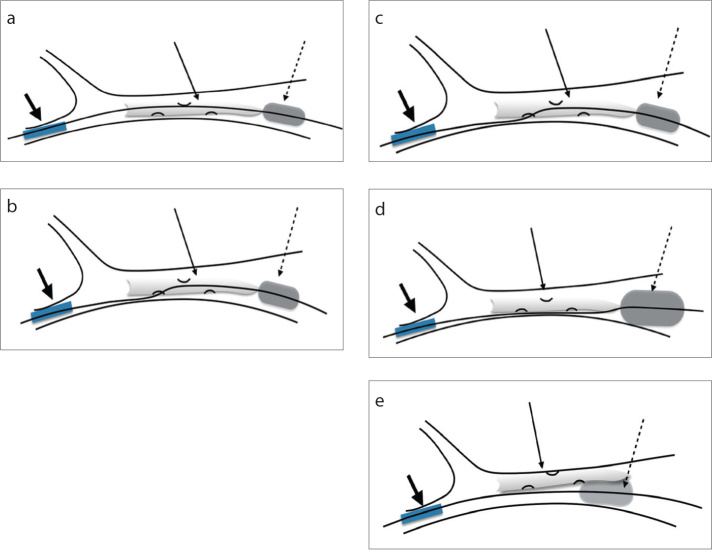
An alternative method of placing the guidewire and balloon catheter alongside the fragment can be used when threading is unsuccessful. In this case, the balloon is inflated and catheter fragment removed through friction. This procedure should be closely monitored during manipulation; if the balloon moves relative to the catheter, it is deflated, repositioned, and re-inflated to a higher degree (5). Techniques using the balloon catheter are summarized in Fig. 3.
Figure 3. a–e.
Techniques related to the use of an over-the-wire balloon catheter. Short black arrow indicates the angiosheath; long black arrow indicates the fractured catheter; and the dashed arrow indicates the balloon catheter. Panel (a) shows threading of the fractured catheter with balloon inflated at the distal end. Panel (b) shows threading of the fractured catheter through side-hole with balloon inflated at the distal end. Panel (c) shows threading and partially inflated balloon at proximal end of catheter. In panel (d), guidewire is passed alongside the catheter and inflated. Note that the balloon is inflated to a higher degree or a larger French is used to prevent sliding of the anchoring balloon relative to catheter. Panel (e) shows guidewire and inflated balloon alongside of the fractured catheter.
Finally, biopsy forceps are used by directly grabbing the distal free end of the catheter and retrieving it. However, this method may by unsuccessful if the forceps cannot be completely opened or if the grip is loosened during manipulation. A variation is the open-forceps method. It requires threading the targeted catheter with a guidewire, followed by advancing closed biopsy forceps into the catheter, and opening it within (acting as an anchor) or outside the distal end (7). Techniques using the biopsy forceps approach are summarized in Fig. 4.
Figure 4. a–c.

Techniques related to the use of a biopsy forceps. Short black arrow indicates the angiosheath; long black arrow indicates the fractured catheter; and the dashed arrow indicates the biopsy forceps. In panel (a), the guidewire is threaded through catheter and forceps opened at the distal end of the fractured catheter. Panel (b) shows directly grasping the fracture end of the catheter. In panel (c), the guidewire is threaded through catheter and opened within the lumen, acting as an anchor while steadily pulling out the fragment.
In conclusion, fracture and intrahepatic migration of plastic percutaneous biliary catheters are rare. It occurs with rigid catheters, short purchase within the biliary tract, and exaggerated respiratory motion causing shearing forces between the liver surface and thoracic cage (8). Because the fractured catheter is rigid and generally located upstream to the stricture site, endoscopic approaches used for PBEs are inapplicable. Although no consensus exists on a single method appropriate in all clinical situations, an understanding of the different percutaneous options is helpful. These include using a goose-neck snare, an over-the-wire balloon catheter, or biopsy forceps manipulation within a large-bore angiosheath in mature transhepatic tract.
Main points.
Fracture of rigid percutaneous transhepatic biliary drainage (PTBD) catheters requires immediate management. Percutaneous approach should be preferred for retrieval, while the endoscopic retrograde cholangiopancreatography approach for dislodging plastic biliary endoprostheses should not be used for rigid PTBD catheters.
Percutaneous retrieval should be performed within a mature percutaneous tract and with use of a large-bore angiosheath for protection of the bile duct and liver parenchyma.
Devices such as goose neck snare, an over-the-wire balloon catheter, or biopsy forceps, may be employed in techniques for catheter retrieval.
Footnotes
Conflict of interest disclosure
The authors declared no conflicts of interest.
References
- 1.Gumus B. Percutaneous intervention strategies for the management of dysfunctioning biliary plastic endoprostheses in patients with malignant biliary obstruction. Diagn Interv Radiol. 2012;18:503–507. doi: 10.4261/1305-3825.DIR.5219-11.2. [DOI] [PubMed] [Google Scholar]
- 2.Saad WE. Percutaneous transhepatic techniques for removal of endoscopically placed biliary plastic endoprostheses. Tech Vasc Interv Radiol. 2008;11:120–132. doi: 10.1053/j.tvir.2008.07.006. https://doi.org/10.1053/j.tvir.2008.07.006. [DOI] [PubMed] [Google Scholar]
- 3.Mueller PR, Van Sonnenberg E, Ferrucci JT., Jr Percutaneous biliary drainage: Technical and catheter-related problems in 200 procedures. AJR Am J Roentgenol. 1982;138:17–23. doi: 10.2214/ajr.138.1.17. https://doi.org/10.2214/ajr.138.1.17. [DOI] [PubMed] [Google Scholar]
- 4.Namdar T, Raffel AM, Topp SA, et al. Complications and treatment of migrated biliary endoprostheses: A review of the literature. World J Gastroenterol. 2007;13:5397–5399. doi: 10.3748/wjg.v13.i40.5397. https://doi.org/10.3748/wjg.v13.i40.5397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fotheringham T, Abbass S, Varghese JC, et al. Displacement of occluded plastic endoprostheses into the duodenum during percutaneous biliary drainage: Description of an under-reported technique. Clin Radiol. 2002;57:1113–1117. doi: 10.1053/crad.2002.1115. https://doi.org/10.1053/crad.2002.1115. [DOI] [PubMed] [Google Scholar]
- 6.Brown KT, Schubert J, Covey AM, et al. Displacement of endoscopically placed plastic biliary endoprostheses into the duodenum with a simple transhepatic technique. J Vasc Interv Radiol. 2004;15:1139–1143. doi: 10.1097/01.RVI.0000136292.23500.0A. https://doi.org/10.1097/01.RVI.0000136292.23500.0A. [DOI] [PubMed] [Google Scholar]
- 7.Matsushita M, Takakuwa H, Nishio A, et al. Open-biopsy-forceps technique for endoscopic removal of distally migrated and impacted biliary metallic stents. Gastrointest Endosc. 2003;58:924–927. doi: 10.1016/s0016-5107(03)02335-6. https://doi.org/10.1016/S0016-5107(03)02335-6. [DOI] [PubMed] [Google Scholar]
- 8.Nghiem DD. Bile leakage after fracture of a percutaneous transhepatic biliary drainage catheter. JAMA. 1984;251:892. https://doi.org/10.1001/jama.1984.03340310014010. [PubMed] [Google Scholar]