Abstract
Objective
To evaluate whether knee contact force and knee pain are different between continuous and interval walking exercise in patients with knee osteoarthritis (OA).
Methods
Twenty seven patients with unilateral symptomatic knee OA completed two separate walking exercise sessions on a treadmill at 1.3 m/s on two different days: 1) a continuous 45-minute walking exercise session, and 2) three 15-minute bouts of walking exercise separated by 1-hour rest periods for a total of 45 minutes of exercise in an interval format. Estimated knee contact forces using the OpenSim software and knee pain were evaluated at baseline (1st minute of walking) and after every 15 minutes between the continuous and interval walking conditions.
Results
A significant increase from baseline was observed in peak knee contact force during the weight-acceptance phase of gait after 30 and 45 minutes of walking, irrespective of the walking exercise condition. Additionally, whereas continuous walking resulted in an increase in knee pain, interval walking did not lead to increased knee pain.
Conclusion
Walking exercise durations of 30 minutes or greater may lead to undesirable knee joint loading in patients with knee OA, while performing the same volume of exercise in multiple bouts as opposed to one continuous bout may be beneficial for limiting knee pain.
Keywords: knee osteoarthritis, walking, exercise, joint loading, pain
Introduction
General aerobic exercise is advocated by most international clinical guidelines as an effective treatment for management of patients with knee osteoarthritis (OA) [1-3]. Randomized clinical trials of aerobic walking exercise, in particular, have shown significant short-term improvements in pain, functional status and quality of life in patients with knee OA [4, 5]. However, high exercise attrition and low long-term compliance rates with walking exercise programs are major barriers for achieving sustained clinical improvements in patients with knee OA. For instance, a recent systematic review reported significant dropout rates of 20-30% in as many as 12 randomized controlled trials of walking exercise in patients with knee OA, indicating patients' reluctance to adopt walking as a form of exercise [3]. Additionally, sustained compliance with maintaining a regular walking exercise program has been reported to be as low as 50% in patients with knee OA, resulting in loss of therapeutic benefits observed immediately after completing a walking exercise program [5, 6]. To this end, evidence suggests that exercise-induced increases in symptoms, beliefs that exercise could be damaging to the knee, and reduced physical capacity to perform exercises at intensities and durations recommended for cardiovascular fitness gains appear to influence why patients with knee OA stop exercising [6, 7].
The current recommendations for walking exercise by the Ottawa Panel suggest that aerobic walking for obtaining cardiovascular fitness in patients with knee OA should be performed for at least 30 minutes, at a level of exercise intensity above normal daily activities and at a minimal frequency of 3 to 4 times a week [3]. This recommendation is similar to that of the American Geriatric Society which advocates 20-30 minutes of aerobic exercise for patients with knee OA at low to moderate intensity (40–60% of heart rate reserve), two to five times per week [8]. According to the recommendations from the American College of Sports Medicine and the American Heart Association, further participation in aerobic activities above the minimum recommended amounts can provide additional health benefits [9]. However, prolonged aerobic exercise may also increase symptoms and lead to non-compliance in patients with knee OA. Evidence from a randomized clinical trial comparing aerobic and resistance exercise with a health education program suggests that the benefits gained from a walking program may be negated by exercising for extended periods of greater than 35 minutes [6]. Similarly, findings from a clinical trial of combined effects of diet and exercise suggest that prolonged walking exercise appeared to lead to more knee symptoms and blunting of clinical benefits compared to a non-weightbearing exercise program [10]. As such, long duration walking in patients with knee OA has been hypothesized to lead to quadriceps muscle fatigue, loss of effective shock absorption, and higher rates of knee joint loading, which can lead to increased pain and greater cartilage damage [11]. As very few studies have evaluated the effects of increasing walking exercise duration on symptoms and other clinical benefits, the optimal walking exercise duration for patients with knee OA remains unknown.
While a single prolonged continuous bout of exercise could have unintended negative effects, completing the same volume of aerobic exercise through an interval training program of shorter daily bouts may be an effective alternative. Evidence suggests that an interval walking exercise program provides comparable and in some cases greater health and fitness benefits compared to a traditional continuous walking exercise program in middle aged men and women [12] as well as in post-menopausal women [13]. Interval walking exercise programs may also reduce attrition within the first 24 weeks of an exercise program [14] and increase compliance [15] compared to a continuous walking program. Evidence from a randomized clinical trial of aerobic and resistance exercise compared to a health education program in patients with knee OA also suggests that participants who either exceeded or worked at the upper end of their prescribed duration per session did not appear to benefit as much from their exercise program as those who elected to take brief timeouts approximately half-way through their exercise therapy [6]. Currently, whether an interval walking program could lead to greater joint protection and less symptoms compared to a continuous walking program has not been evaluated.
The purpose of this repeated-measures, cross-sectional, laboratory study was to compare the acute changes in knee joint contact loading and knee pain between a continuous 45-minute bout of walking exercise compared to performing the same volume of exercise as three shorter 15-minute bouts of walking, with a 1-hour rest break between each bout. We hypothesized that knee contact force (KCF) and knee pain will be higher during a continuous 45-minute bout of walking exercise compared to completing the same volume of exercise in an interval format.
Materials and Methods
Subjects
A total of 27 older adults who met the American College of Rheumatology (ACR) clinical criteria (sensitivity = 95% & specificity = 69%) were recruited from the local research registries and through community advertisements to participate in this study [16]. The ACR clinical criteria for knee OA include knee pain on most days plus 3 of the following 6 criteria: age > 50 years, morning stiffness of < 30 minutes, crepitus on active movement, tenderness of the bony margins of the joint, bony enlargement of the joint, and lack of palpable warmth of the synovium. For all participants, radiographic knee OA (grade II or greater) was confirmed according to the Kellgren and Lawrence rating scale [17] for their painful knee (Table 1). Participants were excluded if they had contralateral knee pain, had a past history of traumatic knee injury, total joint arthroplasty, hip or spine pain, cardiovascular disease or uncontrolled hypertension, were taking beta blockers, had a neurological disorder that affected their gait, required an assistive device for ambulation or had a history of two or more falls within the previous year.
Table 1.
Patient demographics and characteristics.
| Age (years) | 63.7 (7.7) |
|---|---|
| Female, n (%) | 20 (74.1%) |
|
| |
| Height (cm) | 168.0 (8.7) |
|
| |
| Weight (kg) | 77.4 (14.7) |
|
| |
| Body Mass Index (kg/m2) | 27.3 (3.7) |
|
| |
| Tibiofemoral Compartment Radiographic Severity, n (%)‡ | |
|
| |
| Grade 2 | 10 (37%) |
| Grade 3 | 8 (30%) |
| Grade 4 | 9 (33%) |
|
| |
| Patellofemoral Compartment Radiographic Severity, n (%) | |
|
| |
| Grade 0 | 4 (15%) |
| Grade 1 | 10 (37%) |
| Grade 2 | 7 (26%) |
| Grade 3 | 2 (7%) |
| Grade 4 | 4 (15%) |
|
| |
| Knee injury and Osteoarthritis Outcome Score (KOOS)* | |
| Pain (Range: 0 – 100) | 64.4 (17.7) |
| Symptoms (Range: 0 – 100) | 63.2 (17.3) |
| Function in Daily Living (Range: 0 – 100) | 72.5 (18.3) |
| Function in Sport and Recreation (Range: 0 – 100) | 46.2 (26.2) |
| Knee Related Quality of Life (Range: 0 – 100) | 53.6 (18.7) |
|
| |
| Heart Rate Response to Walking Exercise | |
| Baseline (Beats Per Minute) | 75.7 (10.3) |
| 15 Minutes of Walking (Beats Per Minute) | 100.8 (14.4) |
| 30 Minutes of Walking (Beats Per Minute) | 105.1 (15.6) |
| 45 Minutes of Walking (Beats Per Minute) | 105.5 (16.2) |
All patients had to have at least a grade 2 evidence of radiographic tibiofemoral joint OA to be included in the study.
KOOS scoring: 100 indicates no problems and 0 indicates extreme problems
All subjects were also screened prior to inclusion into the study to ensure that they are capable of maintaining a continuous 45-minute bout of walking exercise on a treadmill at a speed of 1.3 m/s. This walking speed was selected as the average self-selected walking speed previously reported in patients with knee OA [18] and to ensure that all participants completed similar volumes of exercise over a 45-minute bout of walking by covering the same distance, while minimizing the influence of variable gait speed on knee joint contact forces [19]. All participants wore a heart rate monitor (Polar Electro Inc.©, Lake Success, NY, USA) during the walking exercise screening to ensure that walking at the speed of 1.3 m/s coincides with 40-60% of their heart rate reserve (Table 1), which is the recommended intensity of aerobic exercise by the American Geriatric society for patients with knee OA [8]. All participants signed an informed consent form approved by the institutional review board of the University of Pittsburgh prior to any testing.
Data Collection
Participants meeting the inclusion criteria were invited to attend two separate testing sessions. For the continuous walking exercise session, participants completed a single 45-minute bout of walking exercise at a speed of 1.3m/s on an instrumented, split-belt treadmill (Bertec Corp., Columbus, OH, USA). For the interval walking exercise session, subjects performed three separate 15-minute bouts of walking exercise for a total of 45 minutes, with each bout separated by a 1-hour rest period. A 1-hour rest period was chosen to simulate performing multiple short bouts of exercise per day, which has been previously recommended in the literature for enhancing exercise adherence and weight loss, while producing similar changes in cardiorespiratory fitness when compared to a single long continuous bout of exercise [12-15]. During each rest period, subjects were asked to remain seated and refrain from standing or walking as much as possible. Testing days were not randomized but were scheduled at least 72 hours apart to allow for alleviation of potential joint flair-ups and to minimize any carry-over effects from the previous day of testing.
On both days of testing, participants were seated in a chair for 30 minutes and their baseline heart rate and blood pressure was checked. Participants' lower extremities were then outfitted with clusters of reflective markers (modified Cleveland Clinic Gait marker set) and virtual markers were calibrated at the hip, knee and ankle joint centers (The MotionMonitor, Chicago, IL, USA) for biomechanical data collection. Participants were then attached to a ceiling mounted safety harness system before the initiation of the treadmill walking exercise to avoid accidental falls and injury.
During the continuous walking exercise session, 30 seconds of passive marker trajectory data sampled at 100 Hz (Vicon motion Systems Ltd., Oxford, UK) along with ground reaction forces sampled at 1000 Hz were collected at baseline (i.e. 1st minute of walking) as well as during the 15th, 30th, and 45th minute of walking exercise. During the interval walking exercise session, 30 seconds of biomechanical data was collected during the 1st and 15th minute of each bout of walking exercise.
Knee Contact Force Prediction
A 3-dimensional, muscle-actuated, computational musculoskeletal model was adapted from the Lower Limb Model [20] in OpenSim [21] to simulate subject-specific KCFs. The adapted model contained 23 degrees of freedom (DOF) and 96 Hill-type muscles. Virtual markers and a marker representing the centroids of the Cleveland Clinic marker sets were used as the final marker set applied to the adjusted model. The knee in the model was represented as a 1 DOF hinge joint allowing anterior posterior translation of the tibiofemoral joint as a function of flexion/extension knee joint motion. Subject-specific models were anthropometrically scaled from the adapted model until the total root mean square (RMS) error between the predicted marker location and actual marker location was less than 0.01 meter.
Joint angles were calculated using an inverse kinematics tool which derived the angles by minimizing weighted square errors of the predicted marker location to the actual marker location. A computed muscle control algorithm [21] calculated muscle excitations and forces from inverse kinematic results by resolving the equations of motion for the unknown muscle forces. Finally, the KCFs were predicted as the sum of the muscle forces and the joint reaction forces calculated from inverse dynamics equations. The KCFs were subsequently decomposed into orthogonal components for each child segment in the parent frame (distal to proximal), with the vertical KCF component reported as the measure of knee joint loading during gait. The KCFs were predicted for 5 consecutive steps during the stance phase of gait and were averaged and normalized to the participant's body weight (BW) for reporting purposes.
Numeric Pain Rating
Pain intensity during walking exercise for the affected knee was recorded on an 11-point (0-10) numerical pain rating scale (NPRS). NPRS has been shown to have concurrent and predictive validity as a measure of pain intensity [22, 23]. The NPRS was anchored on the left with the phrase “No Pain” and on the right with the phrase “Worst Imaginable Pain.” NPRS was collected during the 1st, 15th, 30th, and 45th minute of continuous walking exercise. During the interval walking exercise session, NPRS was collected during the 1st and the 15th minute of each bout of walking exercise.
Statistical Analysis
Data were analyzed using SPSS (SPSS Inc., Chicago, IL, USA) and were first examined for normality and homogeneity of variance. To determine whether KCF varied between continuous and interval walking conditions or as a function of time, a 2×4 (walking condition × walking time) analysis of variance (ANOVA) with repeated measures was performed. For all factorial ANOVA tests, significant main effects were considered only if there were no significant interactions. For all significant main effects, individual differences were compared using independent sample t-tests with multiple comparison adjustments using Bonferroni corrections. The NPRS scores for each testing condition were compared using the Friedman test secondary to not meeting the assumption of normal distribution. Wilcoxon signed-rank tests were used to locate significant changes in NPRS scores over time using a Bonferroni correction.
Results
The KCF curves typically exhibited two peaks during the stance phase of gait which were consistent for all time points and for both walking conditions (Figure 1). The first and the often larger initial peak occurred during the weight-acceptance phase of gait, with the second peak occurring during the late stance phase of gait. The ANOVA results for the first peak in KCF revealed a significant walking time effect (F3,78= 5.13, P = 0.003) but no significant walking condition effect (F1,26= 2.53, P = 0.12) or a walking condition × walking time interaction (F3,78= 1.05, P = 0.38; Table 2). When averaged across the two walking conditions, post-hoc analysis revealed that the first peak in KCF was greater compared to baseline after 30 minutes (mean difference = 0.25 × body weight; P = 0.01) and after 45 minutes of walking (mean difference = 0.22 × body weight; P = 0.04; Table 1). No significant walking condition effect (F1,26= 0.29, P = 0.60), walking time effect (F3,78= 0.87, P = 0.46), or walking condition × walking time interaction (F3,78= 0.52, P = 0.66) was observed for the second peak in KCF (Table 2).
Figure 1.
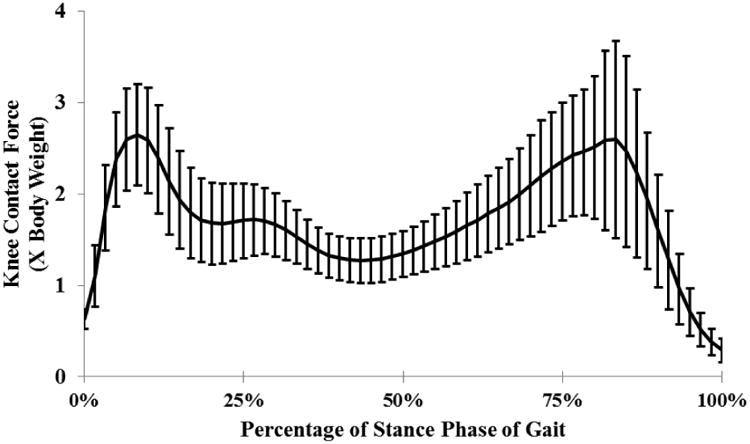
A representative mean knee contact force (KCF) profile during the stance phase of gait with two peaks during the weight acceptance and late stance phases of the gait cycle.
Table 2.
Comparison of the change in the first and the second peaks in the knee contact force between the continuous and interval walking exercise conditions.
| Knee Contact Force (1st Peak) | Baseline | 15 Minutes | 30 Minutes | 45 Minutes |
|---|---|---|---|---|
| Continuous (× body weight) | 2.73 (0.58) | 2.79 (0.60) | 3.03 (0.62) | 2.98 (0.65) |
| Interval (× body weight) | 2.92 (0.78) | 3.04 (0.84) | 3.12 (0.72) | 3.10 (0.76) |
| Combined (× body weight) | 2.82 (0.68) | 2.92 (0.72) | 3.08 (0.67)* | 3.04 (0.71)* |
| Knee Contact Force (2nd Peak) | ||||
| Continuous (× body weight) | 2.83 (1.05) | 2.78 (0.96) | 2.76 (0.96) | 2.72 (0.92) |
| Interval (× body weight) | 2.72 (1.02) | 2.73 (0.96) | 2.75 (0.94) | 2.59 (0.84) |
| Combined (× body weight) | 2.77 (1.04) | 2.75 (0.96) | 2.76 (0.95) | 2.66 (0.88) |
Statistically significant differences (p<0.05) compared to baseline.
The Friedman test results for NPRS scores revealed a significant difference in pain scores as a function of walking time during the continuous exercise condition (χ = 36.4, P < 0.001). As compared to baseline, NPRS scores were significantly increased after 15 minutes (Z = -2.94, P = 0.02), 30 minutes (Z = 3.32, P = 0.006), and 45 minutes (Z = -3.60, p = 0.001) of continuous walking (Figure 2). The NPRS scores were also significantly higher after 30 minutes (Z = -.2.69, P = 0.042) and 45 minutes (Z = -3.37, P = 0.006) of continuous walking as compared to after 15 minutes of walking. On the other hand, the results of the Friedman test for NPRS scores were not significant for the interval walking condition (χ = 4.87, P < 0.18).
Figure 2.
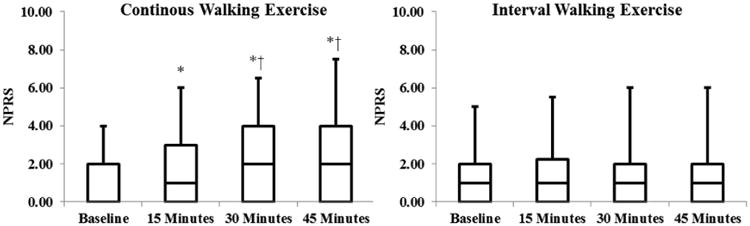
Box plots representing changes in numerical pain rating scale (NPRS) scores over time during the continuous and interval walking exercise conditions. Scores are presented as medians; the ends of the boxes define the 25th and 75th percentiles. * Denotes statistically significant difference from the baseline. † Denotes statistically significant difference from the 15-minute walking time point.
Discussion
Regular walking exercise has been proposed to have a beneficial effect on knee articular cartilage in healthy, community-based adults without history of knee injury or disease [24]. However, higher levels of joint loading through more intense physical activity have been associated with development of knee OA and greater risk of total knee replacement [25, 26]. Although walking exercise has been advocated as an effective treatment option for patients with knee OA, the magnitude of joint loading imposed on the knee joint during walking exercise remains unclear. The findings of the current study suggest that small (8-9%) but potentially meaningful (22-25% of body weight) increases in the first peak of the KCF were observed during the weight-acceptance phase of gait after 30 and 45 minutes of walking compared to baseline. This increase in early-stance KCF was irrespective of the continuous or interval format in which participants completed their exercise sessions. Additionally, our data suggests that increasing the volume of walking exercise from 30 to 45 minutes did not lead to additional increases in KCF beyond those observed at 30 minutes of walking.
Given that the current recommendations for aerobic exercise prescription for patients with knee OA advocate at least 30 minutes of walking at intensities similar to that of our study [3, 8], the observed increases in joint loading at and beyond 30 minutes of walking could have important clinical implications. For example, increased knee loading frequency and magnitude have previously been associated with increased pain in patients with knee OA [27]. Given that participants took an average of 870 steps during each 15-minute bout of walking in our study, the cumulative effects of a modest 22-25% of body weight increase in KCF at and beyond 30 minutes of walking for a 200 pound patient would lead to addition of approximately 36,540 to 43,500 pounds of compressive load to the total knee joint loading profile. Although there are no longitudinal studies indicating that prolonged walking with these levels of increase in KCF could lead to progression of knee OA, an increase of this magnitude would appear to be clinically relevant. The deleterious effects of increasing KCF as a function of time is further supported by the observation of increasing self-reports of pain with cumulative walking time in our study, which was especially apparent during the continuous walking condition.
Our study also found that continuous walking led to a significant increase in pain, whereas the change in pain was negligible during the interval walking condition, which is a key consideration for both patients and clinicians. It has been previously suggested that presence of pain and other symptoms during exercise is a strong predictor of moods experienced post-exercise, which can discourage habitual health actions such as the potential for long-term compliance with walking exercise [28]. To this end, the findings of negligible pain increase in completing a similar volume of exercise in an interval compared to continuous format could potentially lead to more successful adoption and sustained compliance with maintaining a regular walking exercise program which should be formally tested in future studies.
The findings of this study should be evaluated in the context of a number of limitations. We evaluated walking exercise on a treadmill as opposed to walking overground. While treadmill and overground walking are biomechanically similar, the metabolic cost of treadmill walking has shown to be higher in older adults, which may lead to premature fatigue [29]. Use of a treadmill also limits the ability of participants to modify their gait in response to changes in pain, which is a compensatory strategy often observed during overground walking. Therefore, further validation of our findings during an overground walking exercise condition is warranted. Additionally, ligaments were not included in our modeling approach, which assumes that external KCFs are generated entirely by the muscle-tendon structures. In future efforts, contributions from passive structures will be considered along with the impact of muscle activity and ground reaction forces. It is also important to note that the intensity of pain during walking exercise in our cohort of patients with knee OA was on average on the lower end of the NPRS scale. Given that our inclusion criteria required our participants to be able to walk continuously on the treadmill for at least 45 minutes at the speed of 1.3m/s, our cohort of patients with knee OA could be representative of a more functionally capable subgroup of patients with knee OA. Finally, testing days were not randomized. To this end, a post-hoc analysis of walking knee joint kinematics and kinetics (data not reported) revealed no significant between day differences, suggesting that the 72-hour (or greater) washout period between sessions was sufficient to minimize any carry-over effects. Therefore, it is unlikely that the order of testing affected the clinical interpretation of the data but this assertion cannot be fully verified.
In conclusion, cumulative increases in walking exercise volume of greater than 30 minutes (irrespective of walking condition) were associated with a 22-25% of body weight increase in the first peak in KCF, suggesting a significant increase in articular cartilage loading profile that may be undesirable. Additionally, the continuous walking regimen appeared to potentiate an increase in knee pain, while an interval walking regimen of similar walking volume did not lead to increased pain. Together our preliminary findings suggest that prescription of walking exercise of greater than 30 minutes may lead to undesirable joint loading and increased reports of pain, while performing the same volume of exercise in multiple bouts as opposed to one continuous bout may be beneficial for limiting knee pain.
Highlights.
We compared continuous and interval exercise in patients with knee osteoarthritis.
Knee loads and pain were evaluated every 15 minutes for a total of 45 minutes.
Knee loads increased after 30 minutes of walking for both exercise conditions.
Knee pain increased with time during continuous but not interval walking.
Acknowledgments
The project described was supported by the University of Pittsburgh Medical Center Rehabilitation Institute, Pittsburgh Claude D. Pepper Older Americans Independence Center through (Grant number P30 AG024827) and the National Institutes of Health (Grant numbers UL1 RR024153, UL1 TR000005 and K12 HD055931).
Footnotes
Conflict of interest: None of the authors of this manuscript “The Influence of Continuous Versus Interval Walking Exercise on Joint Loading and Self-Reported Pain in Patients with Knee Osteoarthritis” have any conflicts of interest. In addition, the study sponsors had no role in the study design, data collection, analysis or writing of this manuscript.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Zhang W, Nuki G, Moskowitz RW, Abramson S, Altman RD, Arden NK, et al. OARSI recommendations for the management of hip and knee osteoarthritis: part III: Changes in evidence following systematic cumulative update of research published through January 2009. Osteoarthritis Cartilage. 2010;18:476–99. doi: 10.1016/j.joca.2010.01.013. [DOI] [PubMed] [Google Scholar]
- 2.Hochberg MC, Altman RD, April KT, Benkhalti M, Guyatt G, McGowan J, et al. American College of Rheumatology 2012 recommendations for the use of nonpharmacologic and pharmacologic therapies in osteoarthritis of the hand, hip, and knee. Arthritis Care Res. 2012;64:465–74. doi: 10.1002/acr.21596. [DOI] [PubMed] [Google Scholar]
- 3.Loew L, Brosseau L, Wells GA, Tugwell P, Kenny GP, Reid R, et al. Ottawa panel evidence-based clinical practice guidelines for aerobic walking programs in the management of osteoarthritis. Arch Phys Med Rehabil. 2012;93:1269–85. doi: 10.1016/j.apmr.2012.01.024. [DOI] [PubMed] [Google Scholar]
- 4.Bautch JC, Malone DG, Vailas AC. Effects of exercise on knee joints with osteoarthritis: a pilot study of biologic markers. Arthritis Care Res. 1997;10:48–55. doi: 10.1002/art.1790100108. [DOI] [PubMed] [Google Scholar]
- 5.Ettinger WH, Jr, Burns R, Messier SP, Applegate W, Rejeski WJ, Morgan T, et al. A randomized trial comparing aerobic exercise and resistance exercise with a health education program in older adults with knee osteoarthritis. The Fitness Arthritis and Seniors Trial (FAST) Jama. 1997;277:25–31. [PubMed] [Google Scholar]
- 6.Rejeski WJ, Brawley LR, Ettinger W, Morgan T, Thompson C. Compliance to exercise therapy in older participants with knee osteoarthritis: implications for treating disability. Med Sci Sports Exerc. 1997;29:977–85. doi: 10.1097/00005768-199708000-00001. [DOI] [PubMed] [Google Scholar]
- 7.Hendry M, Williams NH, Markland D, Wilkinson C, Maddison P. Why should we exercise when our knees hurt? A qualitative study of primary care patients with osteoarthritis of the knee. Fam pract. 2006;23:558–67. doi: 10.1093/fampra/cml022. [DOI] [PubMed] [Google Scholar]
- 8.Exercise prescription for older adults with osteoarthritis pain: consensus practice recommendations. A supplement to the AGS Clinical Practice Guidelines on the management of chronic pain in older adults. J Am Geriatr Soc. 2001;49:808–23. doi: 10.1046/j.1532-5415.2001.00496.x. [DOI] [PubMed] [Google Scholar]
- 9.Nelson ME, Rejeski WJ, Blair SN, Duncan PW, Judge JO, King AC, et al. Physical activity and public health in older adults: recommendation from the American College of Sports Medicine and the American Heart Association. Med Sci Sports Exerc. 2007;39:1435–45. doi: 10.1249/mss.0b013e3180616aa2. [DOI] [PubMed] [Google Scholar]
- 10.Toda Y. The effect of energy restriction, walking, and exercise on lower extremity lean body mass in obese women with osteoarthritis of the knee. J Orthop Sci. 2001;6:148–54. doi: 10.1007/s007760100063. [DOI] [PubMed] [Google Scholar]
- 11.Syed IY, Davis BL. Obesity and osteoarthritis of the knee: hypotheses concerning the relationship between ground reaction forces and quadriceps fatigue in long-duration walking. Med Hypotheses. 2000;54:182–5. doi: 10.1054/mehy.1999.0013. [DOI] [PubMed] [Google Scholar]
- 12.Quinn TJ, Klooster JR, Kenefick RW. Two short, daily activity bouts vs. one long bout: are health and fitness improvements similar over twelve and twenty-four weeks? J Strength Cond Res. 2006;20:130–5. doi: 10.1519/R-16394.1. [DOI] [PubMed] [Google Scholar]
- 13.Asikainen TM, Miilunpalo S, Oja P, Rinne M, Pasanen M, Vuori I. Walking trials in postmenopausal women: effect of one vs two daily bouts on aerobic fitness. Scand J Med Sci Sports. 2002;12:99–105. doi: 10.1034/j.1600-0838.2002.120206.x. [DOI] [PubMed] [Google Scholar]
- 14.Jacobsen DJ, Donnelly JE, Snyder-Heelan K, Livingston K. Adherence and attrition with intermittent and continuous exercise in overweight women. Int J Sports Med. 2003;24:459–64. doi: 10.1055/s-2003-41177. [DOI] [PubMed] [Google Scholar]
- 15.Jakicic JM, Wing RR, Butler BA, Robertson RJ. Prescribing exercise in multiple short bouts versus one continuous bout: effects on adherence, cardiorespiratory fitness, and weight loss in overweight women. Int J Obes Relat Metab Disord. 1995;19:893–901. [PubMed] [Google Scholar]
- 16.Altman R, Asch E, Bloch D, Bole G, Borenstein D, Brandt K, et al. Development of criteria for the classification and reporting of osteoarthritis. Classification of osteoarthritis of the knee. Diagnostic and Therapeutic Criteria Committee of the American Rheumatism Association. Arthritis Rheum. 1986;29:1039–49. doi: 10.1002/art.1780290816. [DOI] [PubMed] [Google Scholar]
- 17.Kellgren J, Lawrence J. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16:494. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Landry SC, McKean KA, Hubley-Kozey CL, Stanish WD, Deluzio KJ. Knee biomechanics of moderate OA patients measured during gait at a self-selected and fast walking speed. J Biomech. 2007;40:1754–61. doi: 10.1016/j.jbiomech.2006.08.010. [DOI] [PubMed] [Google Scholar]
- 19.Zeni JA, Higginson JS. Differences in gait parameters between healthy subjects and persons with moderate and severe knee osteoarthritis: a result of altered walking speed? Clin Biomech. 2009;24:372–8. doi: 10.1016/j.clinbiomech.2009.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Arnold EM, Ward SR, Lieber RL, Delp SL. A model of the lower limb for analysis of human movement. Ann Biomed Eng. 2010;38:269–79. doi: 10.1007/s10439-009-9852-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Delp SL, Anderson FC, Arnold AS, Loan P, Habib A, John CT, et al. OpenSim: open-source software to create and analyze dynamic simulations of movement. IEEE T Bio-Med Eng. 2007;54:1940–50. doi: 10.1109/TBME.2007.901024. [DOI] [PubMed] [Google Scholar]
- 22.Jensen MP, Turner JA, Romano JM. What is the maximum number of levels needed in pain intensity measurement? Pain. 1994;58:387–92. doi: 10.1016/0304-3959(94)90133-3. [DOI] [PubMed] [Google Scholar]
- 23.Jensen MP, Turner JA, Romano JM, Fisher LD. Comparative reliability and validity of chronic pain intensity measures. Pain. 1999;83:157–62. doi: 10.1016/s0304-3959(99)00101-3. [DOI] [PubMed] [Google Scholar]
- 24.Racunica TL, Teichtahl AJ, Wang Y, Wluka AE, English DR, Giles GG, et al. Effect of physical activity on articular knee joint structures in community-based adults. Arthritis Care Res. 2007;57:1261–8. doi: 10.1002/art.22990. [DOI] [PubMed] [Google Scholar]
- 25.Cheng Y, Macera CA, Davis DR, Ainsworth BE, Troped PJ, Blair SN. Physical activity and self-reported, physician-diagnosed osteoarthritis: is physical activity a risk factor? J Clin Epidemiol. 2000;53:315–22. doi: 10.1016/s0895-4356(99)00168-7. [DOI] [PubMed] [Google Scholar]
- 26.Wang Y, Simpson JA, Wluka AE, Teichtahl AJ, English DR, Giles GG, et al. Is physical activity a risk factor for primary knee or hip replacement due to osteoarthritis? A prospective cohort study. J Rheumatol. 2011;38:350–7. doi: 10.3899/jrheum.091138. [DOI] [PubMed] [Google Scholar]
- 27.Robbins SM, Birmingham TB, Callaghan JP, Jones GR, Chesworth BM, Maly MR. Association of pain with frequency and magnitude of knee loading in knee osteoarthritis. Arthritis Care Res. 2011;63:991–7. doi: 10.1002/acr.20476. [DOI] [PubMed] [Google Scholar]
- 28.Rejeski WJ, Gauvin L, Hobson ML, Norris JL. Effects of baseline responses, in-task feelings, and duration of activity on exercise-induced feeling states in women. Health Psychol. 1995;14:350–9. doi: 10.1037//0278-6133.14.4.350. [DOI] [PubMed] [Google Scholar]
- 29.Parvataneni K, Ploeg L, Olney SJ, Brouwer B. Kinematic, kinetic and metabolic parameters of treadmill versus overground walking in healthy older adults. Clin Biomech. 2009;24:95–100. doi: 10.1016/j.clinbiomech.2008.07.002. [DOI] [PubMed] [Google Scholar]


