Abstract
The aim of this article is to determine hearing and mortality outcomes following temporal bone fractures. Retrospective chart review was performed of 152 patients diagnosed with a temporal bone fracture presenting to the emergency room at a tertiary care referral center over a 10-year period. Utilizing Patients' previously obtained temporal bone computed tomographic scans and audiograms, fractures were classified based on several classification schemes. Correlations between fracture patterns, mortality, and hearing outcomes were analyzed using χ 2 tests. Ossicular chain disruption was seen in 11.8% of patients, and otic capsule violation was seen in 5.9%; 22.7% of patients presented for audiologic follow-up. Seventeen patients with conductive hearing loss had air–bone gaps of 26 ± 7.5 dB (500 Hz), 27 ± 6.8 dB (1,000 Hz), 18 ± 6.2 dB (2,000 Hz), and 32 ± 7.7 dB (4,000 Hz). Two cases of profound sensorineural hearing loss were associated with otic capsule violation. No fracture classification scheme was predictive of hearing loss, although longitudinal fractures were statistically associated with ossicular chain disruption ( p < 0.01). Temporal bone fractures in patients older than 60 years carried a relative risk of death of 3.15 compared with those younger than 60 years. The average magnitude of conductive hearing loss resulting from temporal bone fracture ranged from 18 to 32 dB in this cohort. Classification of fracture type was not predictive of hearing loss, despite the statistical association between ossicular chain disruption and longitudinal fractures. This finding may be due to the low follow-up rates of this patient population. Physicians should make a concerted effort to ensure that audiological monitoring is executed to prevent and manage long-term hearing impairment.
Keywords: temporal bone, trauma, hearing outcomes
The temporal bone forms a part of the lateral skull base and houses the organs of hearing and balance, as well as the temporal portion of the carotid artery. The temporal bone also transmits the facial nerve from the brainstem to the facial soft tissues. In its role as part of the skull base, it articulates with the sphenoid, parietal, zygomatic, and occipital bones and forms the floor of the middle fossa. Injuries to this critical structure can have multiple consequences, including deficits in hearing and balance and facial nerve paralysis. The bone itself is subdivided into four parts: the mastoid process, the tympanic portion, the squamosa, and the petrous apex.
Fracture patterns of this structure in trauma are complex and can involve any of these structures. Multiple systems have been proposed to classify these in an attempt to correlate them with clinical symptoms. The initial classification system separated fractures into longitudinal, transverse, or oblique depending on the relationship between the long axis of the fracture and of the petrous apex. 1 2 This classification scheme was based on cadaveric studies performed in the 1950s. 3 A longitudinal fracture was more likely to result from a force directed laterally, whereas a transverse fracture was more likely to result from a blow directed in the anteroposterior direction. Longitudinal fractures are generally the more common of the two types, occurring in 70% to 90% of temporal bone trauma. 3 Although this scheme provides a simple means of fracture pattern classification, multiple studies have demonstrated little utility in terms of predicting clinical outcomes. 4 This is primarily attributable to the difficulty of classifying all fractures into one of two geometric configurations, when many fractures are neither purely longitudinal nor purely transverse. The addition of categories such as oblique or mixed to describe more complex fracture patterns has not resulted in significant improvements in the ability to predict clinical outcomes.
A simpler method of classifying fractures proposed by Brodie and Thompson, 5 which has proven more predictive of clinical outcomes, is to separate fractures into otic capsule violating or otic capsule sparing. This system is straightforward and unambiguous to implement, unlike the classification system based on geometry. Otic capsule violating fractures have been noted to convey a fourfold increase in the risk of cerebrospinal fluid (CSF) leak, and a sevenfold increase in the risk of sensorineural hearing loss (SNHL). 6 A further refinement of this system by Ishman and Friedland classifies temporal bone fractures into those which involve the petrous apex and those which spare the petrous apex. This classification system demonstrated that fractures involving the petrous apex are 9.8 times as likely to have a CSF leak, and 3 times as likely to cause facial nerve paralysis compared with fractures not involving the petrous apex. 4 SNHL was not significantly different between the two fracture types, but conductive hearing loss (CHL) was significantly correlated with fractures not involving the petrous apex. 4
Mechanisms of hearing loss following temporal bone trauma are varied. Direct damage to the cochlea or internal auditory canal and disruption of the ossicular chain are the most obvious mechanisms of hearing loss and are apparent radiographically. 7 However, hearing loss can still result from injury to the membranes within the cochlea, or by microfractures of the cochlea which are not apparent on computed tomographic (CT) scans. However, while the relationship between temporal bone fractures and complications such as CSF leak and facial nerve paralysis has been extensively reported, data about longer-term hearing outcomes are scarce. The objective of this study is to present longer-term hearing outcomes following temporal bone fractures.
Methods
This retrospective review was conducted across two hospitals associated with the same institution, an academic tertiary care referral center and a community hospital. Academic institutional review board approval was obtained prior to initiation of the study (Pro00058026). Emergency department records were explored for all patients older than 18 years, seen between January 1, 2004, and June 30, 2014, with an associated ICD9 code for skull base fracture (801.xx or 803.xx). Because there is no specific ICD9 code for temporal bone fractures, this subset of records was further refined by filtering for records containing a CT scan report with the phrase “temporal bone fracture.” This group of records was further filtered to exclude those patients whose temporal bone fracture was confined to the squamosal portion of the temporal bone, as squamous temporal bone fractures at this institution are managed by neurosurgery. Furthermore, isolated squamous temporal bone fractures are not known to contribute to hearing deficits. Charts were reviewed to determine demographic data as well as audiometric follow-up.
CT scans were assessed to determine the type and extent of fracture, as well as the presence of hemotympanum, ossicular chain dislocation, or otic capsule violation. Fractures were classified as either longitudinal, transverse, or oblique depending on their orientation with respect to the long axis of the temporal bone. Fractures containing both longitudinal and transverse components were classified as mixed. For patients with audiometric follow-up data, fractures were also classified based on whether the petrous apex was involved or spared.
Statistical analysis was performed using the χ 2 test for comparison of proportions.
Results
A total of 152 patients met inclusion criteria for the study. Bilateral fractures were noted in 19 of 152 patients (12.5%) for a total of 172 temporal bone fractures in the study. Baseline characteristics of the study group are outlined in Table 1 .
Table 1. Study group demographic and etiology data.
| Age | N (%) |
|---|---|
| ≥ 60 y | 26 (17.1) |
| < 60 y | 126 (82.9) |
| Laterality | |
| Right | 74 (48) |
| Left | 60 (39.5) |
| Bilateral | 19 (12.5) |
| Etiology | |
| Vehicular | 78 (51.3) |
| MVC | 57 (37.5) |
| ATV accident | 4 (2.6) |
| Bicycle accident | 2 (1.3) |
| Struck by vehicle | 15 (9.8) |
| Fall | 50 (32.9) |
| Assault | 19 (12.5) |
| Blunt force | 15 (9.8) |
| GSW | 4 (2.6) |
| Unknown | 5 (3.3) |
Abbreviations: ATV, all-terrain vehicle; GSW, gunshot wound; MVC, motor vehicle collision.
Temporal bone fractures carried a relatively high risk of mortality, predominantly due to associated intracranial injuries. In our cohort, 30 of the 152 (19.7%) patients died during admission. This risk was not evenly distributed across age groups. Among patients 60 years or older, 12 of the 26 (42%) patients did not survive their admission, compared with 18 of the 126 (14.0%) patients younger than 60 years who did not survive. This finding was statistically significant ( p < 0.001). Among those patients who died during the same admission as the temporal bone fracture, the cause of death was directly related to sequelae of intracranial injuries in 25 of 29 (86%) patients. Among those patients who died, the most common findings on head CT scan were subarachnoid or subdural hemorrhage, midline shift away from the side of the fracture, and diffuse cerebral edema. For patients 60 years or older, the presence of a temporal bone fracture carried a relative risk of death of 3.15 ([95% confidence interval [CI]: 1.8–5.4]) compared with patients younger than 60 years. Patients 60 years or older were also much more likely to be injured via a fall compared with a vehicular related mechanism ( p < 0.02).
A total of 169 CT scans were analyzed for radiographic abnormalities associated with temporal bone fractures; two scans were not examined due to their removal from the medical record system for unspecified reasons. Hemotympanum was very common and present in 129 of 169 scans (76.3%). Ossicular chain disruption was noted in 20 of 169 scans (11.8%) and otic capsule violation was noted in 10 of 169 scans (5.9%). Ossicular chain disruption was more commonly associated with fractures classified as longitudinal compared with transverse or oblique/mixed fracture patterns ( p < 0.01).
Of a total of 119 patients who survived their hospitalization, 27 presented for audiologic follow-up (22.7%). Initial audiometric follow-up was performed, on average, 43 days after initial injury ([range: 3–316 days]). The various types of hearing loss observed are shown in Fig. 1 . For patients with a conductive component to their hearing loss, air–bone gaps were noted between 15 and 35 dB, with the breakdown by frequency shown in Fig. 2 . Five patients were noted to have hemotympanum on their initial visit, which had resolved in all cases by the second visit which was between 21 and 40 days after the initial visit. Of the four patients with mixed-type hearing loss, three had documented resolution of the conductive component by their second visit, with the remaining patient having continued CHL at the time of the latest audiogram. Of the eight patients with a pure SNHL, two patients with otic capsule violating fractures experienced a profound loss with lack of response to auditory stimuli at any hearing level. The remaining six patients with SNHL had mild to moderate levels of hearing loss. No fracture classification scheme utilized was predictive of hearing loss in those patients who presented for audiologic follow-up.
Fig. 1.
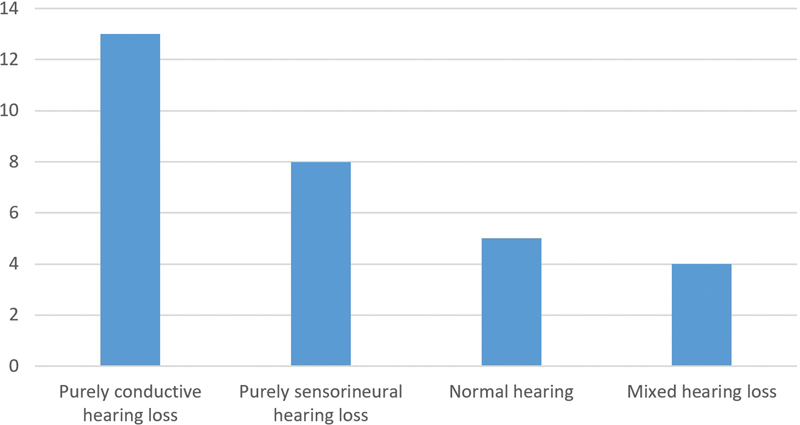
Types of hearing loss observed.
Fig. 2.
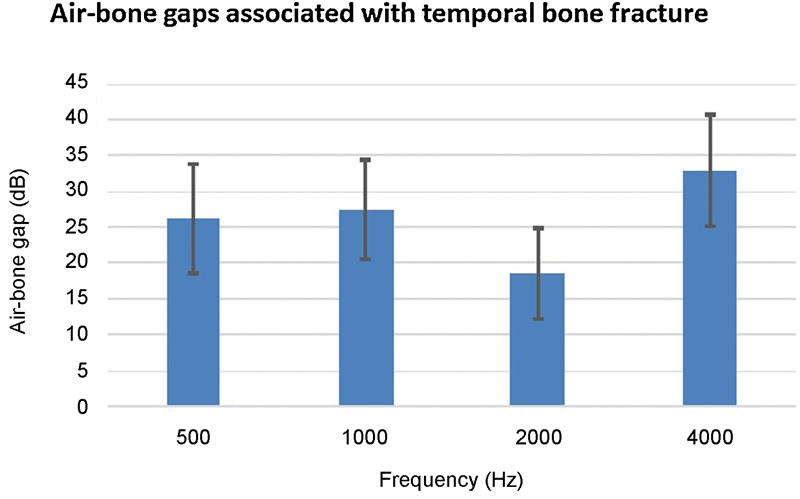
Air–bone gaps associated with temporal bone fracture.
Discussion
Head trauma continues to be a major cause of morbidity and mortality. The literature reports motor vehicle accidents (MVAs) are the primary mechanism for injury 8 which is confirmed in our series as 78% of cases were secondary to MVAs. Based on retrospective review of the medical records, we aimed to investigate and present long-term hearing outcomes following temporal bone fractures. Of what limited data currently exists in the literature, the reported incidence rates for CHL following temporal bone fracture are 10 to 57% 6 8 and from our current understanding CHL generally resolves over time, usually within 3 to 4 weeks. SNHL rates post–temporal bone trauma are reported as 0 to 14%. 6 9
In our study, of those patients for whom audiograms were available, only 17% had grossly normal hearing. Unfortunately, no preinjury audiograms were available for any patients in this study. At a mean of 43 days post–temporal bone injury, we observed an incidence of 43% CHL, 27% SNHL, and 13% mixed hearing loss. All patients with SNHL not attributable to an otic capsule fracture were found to have symmetric SNHL, suggesting this was likely a preexisting condition. Out of 17 patients with some component of CHL, 5 were found to have hemotympanum on exam. All five patients had resolution of their hemotympanum on a subsequent exam, with a range between 21 and 40 days after the initial injury. This is concordant with previous estimates of ~approximately 6 weeks for resolution of hemotympanum. However, there were 13 patients with a documented CHL and a well-aerated middle ear space. This may be the result of blood clots which are not evident on exam, or due to subtle dislocations of the ossicular chain which may not have been evident on CT scan.
It is interesting to note the low proportion (22.7%) of patients who presented for audiologic follow-up after temporal bone trauma. To our knowledge, this finding of low follow-up rates has not been previously reported. It is unclear whether this is due to lack of follow-up referrals being made, or lack of patient compliance with follow-up. Low follow-up may also be due to the fact that temporal bone fractures rarely occur in isolation. Approximately 1,875 lb of force is required to fracture the temporal bone, 6 and as a result there are frequently concordant intracranial and spinal injuries associated with temporal bone fractures. With altered mental status, patients may be unable to communicate that they have a hearing loss. Therefore, hearing loss may go unrecognized, or may be considered a lower priority than other injuries which are acutely life threatening.
Our study does likely underestimate the true audiologic follow-up rate, as our institution is a level 1 trauma center with a large catchment area. It is possible that many of the patients who did not present for follow-up at our institution actually sought evaluation by local otolaryngologists and audiologists. It is also possible that some patients choose not to follow-up because their hearing loss was due to hemotympanum and resolved spontaneously. However, among the 20 patients with radiographically evident ossicular chain disruption, only 3 had subsequent follow-up audiograms, and of the 10 patients with otic capsule violation, only 2 appeared for a postinjury hearing evaluation. It is not reasonable to conclude that these patients had hearing loss which would have resolved on its own without some form of intervention.
There is evidence to suggest that our study cohort has patients with missed ossicular chain disruption. First, the proportion of otic capsule disruption in our study is somewhat lower than the 15% to 37% previously reported in the literature. 10 11 Second, some patients underwent only a standard noncontrast head CT as part of their trauma workup as opposed to a dedicated petrous temporal bone CT scan, and subtle otic capsule injuries may have been missed due to the thicker CT slices. Third, among the 14 patients who followed up and had no radiographically evident otic capsule disruption, the magnitude of conductive loss was similar to the three patients with known otic capsule disruption, and also with previously reported values in the literature for traumatic dissociation of the ossicles. 12 If indeed patients with ossicular chain disruption are being missed for treatment, it would represent a significant problem as temporal bone injuries have been demonstrated to have significant detrimental effects on functional status and quality of life. 13 14
Our study was not able to show that any particular system of characterizing temporal bone fractures is predictive of long-term hearing loss. However, longitudinal fractures were more frequently associated with ossicular chain disruption ( p < 0.01) than oblique or mixed-type fractures. This can be accounted for by the fact that longitudinal fractures pass from lateral to medial and cross the trajectory of the ossicular chain. It is difficult to explain why longitudinal fractures are not associated with CHL in our study, but this may be due to the fact that of 20 patients with ossicular chain disruption, only 3 have follow-up audiograms in our medical record system.
The main weakness of this study is the retrospective design. Furthermore, this study does not account for patients who may have followed up outside of our institution for their audiologic care which may have contributed to the low rates of audiologic follow-up. The low follow-up rate does make it challenging to generalize and suggest that the results discovered in this cohort apply to the entire population of patients with temporal bone fractures. However, this study does represent an important contribution to improving our understanding of longer-term hearing outcomes in patients with temporal bone fractures.
Conclusion
Classification of temporal bone fracture type was not predictive of hearing loss in our cohort, despite the association between ossicular chain disruption and longitudinal fractures. For those who presented for audiologic follow-up at a mean of 43 days postinjury, we observed an incidence of 43% CHL, 27% SNHL, and 13% mixed hearing loss and the average magnitude of CHL ranged from 18 to 32 dB. Mortality was largely secondary to intracranial injuries sustained at the same time as the temporal bone fracture. Audiologic follow-up rates were poor within this cohort, which may affect the overall results. The low rates of audiologic follow-up observed should alert clinicians to make a concerted effort to ensure that audiological monitoring is executed to prevent and manage long-term hearing impairment in patients with temporal bone injuries. This may require a coordinated care approach to improve follow-up rates.
References
- 1.Kennedy T A, Avey G D, Gentry L R.Imaging of temporal bone trauma Neuroimaging Clin N Am 20142403467–486., viii [DOI] [PubMed] [Google Scholar]
- 2.Kang H M, Kim M G, Boo S H et al. Comparison of the clinical relevance of traditional and new classification systems of temporal bone fractures. Eur Arch Otorhinolaryngol. 2012;269(08):1893–1899. doi: 10.1007/s00405-011-1849-7. [DOI] [PubMed] [Google Scholar]
- 3.Collins J M, Krishnamoorthy A K, Kubal W S, Johnson M H, Poon C S. Multidetector CT of temporal bone fractures. Semin Ultrasound CT MR. 2012;33(05):418–431. doi: 10.1053/j.sult.2012.06.006. [DOI] [PubMed] [Google Scholar]
- 4.Ishman S L, Friedland D R. Temporal bone fractures: traditional classification and clinical relevance. Laryngoscope. 2004;114(10):1734–1741. doi: 10.1097/00005537-200410000-00011. [DOI] [PubMed] [Google Scholar]
- 5.Brodie H A, Thompson T C. Management of complications from 820 temporal bone fractures. Am J Otol. 1997;18(02):188–197. [PubMed] [Google Scholar]
- 6.Johnson F, Semaan M T, Megerian C A.Temporal bone fracture: evaluation and management in the modern era Otolaryngol Clin North Am 20084103597–618., x [DOI] [PubMed] [Google Scholar]
- 7.Saraiya P V, Aygun N. Temporal bone fractures. Emerg Radiol. 2009;16(04):255–265. doi: 10.1007/s10140-008-0777-3. [DOI] [PubMed] [Google Scholar]
- 8.Amin Z, Sayuti R, Kahairi A, Islah W, Ahmad R. Head injury with temporal bone fracture: one year review of case incidence, causes, clinical features and outcome. Med J Malaysia. 2008;63(05):373–376. [PubMed] [Google Scholar]
- 9.Gladwell M, Viozzi C. Temporal bone fractures: a review for the oral and maxillofacial surgeon. J Oral Maxillofac Surg. 2008;66(03):513–522. doi: 10.1016/j.joms.2007.08.039. [DOI] [PubMed] [Google Scholar]
- 10.Cvorovic L, Jovanovic M B, Markovic M, Milutinovic Z, Strbac M. Management of complication from temporal bone fractures. Eur Arch Otorhinolaryngol. 2012;269(02):399–403. doi: 10.1007/s00405-011-1641-8. [DOI] [PubMed] [Google Scholar]
- 11.Wood C P, Hunt C H, Bergen D C et al. Tympanic plate fractures in temporal bone trauma: prevalence and associated injuries. AJNR Am J Neuroradiol. 2014;35(01):186–190. doi: 10.3174/ajnr.A3609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yetiser S, Hidir Y, Birkent H, Satar B, Durmaz A. Traumatic ossicular dislocations: etiology and management. Am J Otolaryngol. 2008;29(01):31–36. doi: 10.1016/j.amjoto.2007.01.001. [DOI] [PubMed] [Google Scholar]
- 13.Gupta N, Varshney S, Bist S S, Bhatia R. A study of temporal bone fractures. Indian J Otolaryngol Head Neck Surg. 2008;60(03):223–226. doi: 10.1007/s12070-008-0082-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Montava M, Mancini J, Masson C, Collin M, Chaumoitre K, Lavieille J P. Temporal bone fractures: sequelae and their impact on quality of life. Am J Otolaryngol. 2015;36(03):364–370. doi: 10.1016/j.amjoto.2014.12.011. [DOI] [PubMed] [Google Scholar]


