Abstract
Bilateral masseter muscle hypertrophy is an alteration in shape and thickness of the masseter muscles that can modify the width of the lower face causing aesthetic and functional problems. A 21-year-old man was referred to the Department of Maxillofacial Surgery at the Civil Hospital in Brescia by his dentist for an evaluation of his facial appearance with a square-face type. To reduce the undesirable facial appearance, a surgical intraoral approach was performed; the procedure includes the bilateral dissection of the masseter muscle, partial lipectomy, and the ostectomy of the mandibular angle assisted by a surgical guide built on a stereolithographic model. The patient was satisfied with the functional and aesthetic outcomes of both the profile and the frontal views. There was no evidence of complication at a 1-year follow-up. This new method yields optimal aesthetic results with an enhanced outline of the lower face.
Keywords: masseter hypertrophy, buccal fat pad, surgical guide
Masseter hypertrophy is a rare condition and the etiology in the majority of the cases is unclear. 1 This condition can cause both functional and aesthetic problems; aesthetic problems consist of the prominent masseter muscle in the face and a square face and with a wide angle so that this type of patient could have psychological problems due to an unappealing face. 2 3 Functional problems lead to malocclusion, bruxism, clenching, and temporomandibular disorders. 4
Masseter muscle hypertrophy was first described by Legg in 1880 5 and since then, many surgeons have been interested in the treatment of this disorder. 6 In 1947, Gurney proposed the first surgical treatment according to an extraoral approach with a submandibular incision and then the removal of a part of all muscle tissue available from the muscle upper aponeurosis to the lower mandibular border. 7
The use of an intraoral approach was first suggested by Ginestet et al 8 and in 1977, Becker reported the intraoral technique in treating 17 patients. 9 Nowadays, the treatment is well known and the different options in managing this pathology comprise botulinum toxin, splint therapy, reduction of the masseter muscle, osteotomy, and ostectomy.
The aim of this article is to present a new treatment of an uncommon case of masseter muscle hypertrophy associated with a mandibular angular overgrowth using masseter muscle reduction, partial lipectomy of the buccal fat pad, and ostectomy of the mandibular angle assisted by a surgical guide built on a stereolithographic model.
Technical Note
A 21-year-old man was referred to the Department of Maxillofacial Surgery at the Civil Hospital in Brescia by his dentist for an evaluation of his facial appearance with square-face type ( Fig. 1 ).
Fig. 1.

Preoperative clinical frontal view.
The extra- and intraoral evaluation revealed a bilateral masseter muscle hypertrophy and a buccal fat pad overgrowth in a square-face type, an increase of the mandibular angle, a class I molar occlusion with a limitation of mouth opening; we noticed even bruxism as an interpretation of his grinded teeth. The methods used for the measurement of the buccal fat pad and masseter muscle were just clinical judgment. There was no history of trauma in this patient and no genetic alteration. The orthopantomography, the computed tomographic scan, and the ultrasound did not reveal any other underlying pathology ( Fig. 2 ).
Fig. 2.
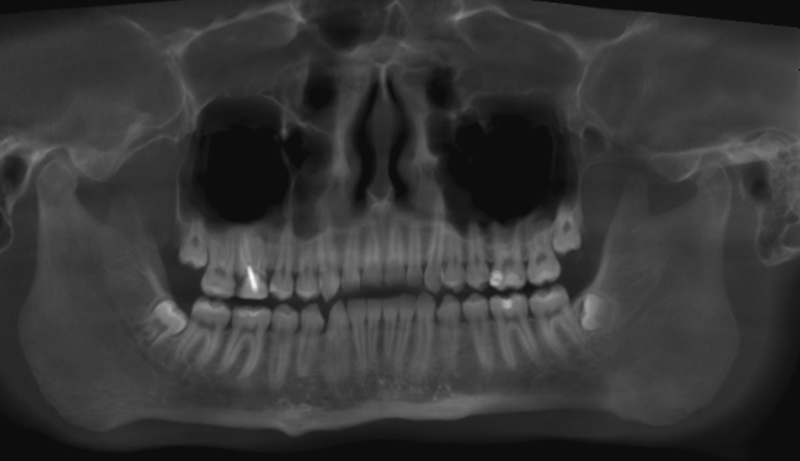
Preoperative mandibular Rx.
The third molars were asymptomatic and they were controlled in the subsequent clinical checks. Before surgery, a stereolithographic model was used to plan the correct ostectomy; a surgical titanium guide (Johnson & Johnson, New Brunswick, NJ) was built on that model to facilitate the procedure and to gain a better aesthetic result and a similar ostectomy line ( Figs. 3 and 4 ).
Fig. 3.
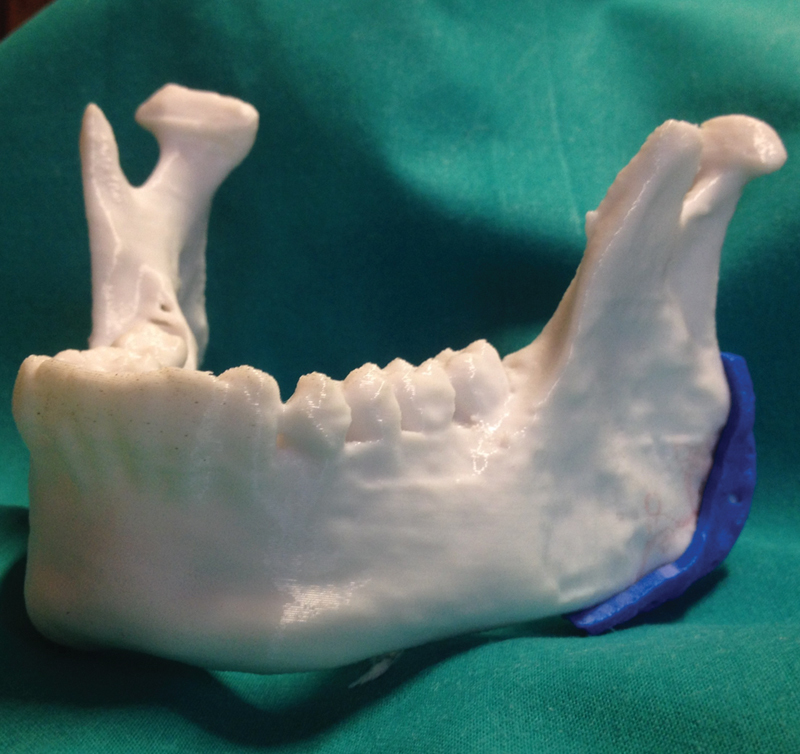
Stereolithographic model with surgical guide.
Fig. 4.
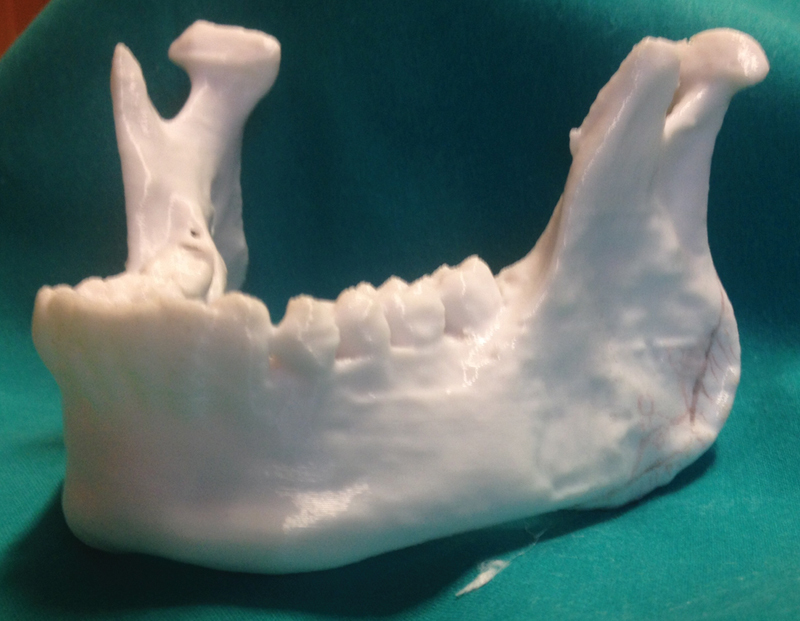
Stereolithographic model with surgical guide (closer view).
Under general anesthesia (mepivacaine 0.2% with 1:100,000 adrenaline), an intraoral approach was performed. Then, an incision along the right external oblique line was made and the periosteum was elevated.
The body of the buccal fat pad was located and a partial lipectomy was performed, then the masseter muscle was carefully detached with an elevator throughout the inferior and the posterior border of the angle of the mandible and the surgical reduction was performed. After that the surgical titanium guide was inserted along the mandibular border in the angular region and the ostectomy was performed. The incision was closed in a single plan with a 4–0 absorbable suture and a compressive external bandage was put in place for 3 days. During the procedure, a dose of 1 g of Solu-Medrol (Pfizer, New York, NY) was intravenously managed. Amoxicillin 1 g two times a day for 1 week was prescribed after surgery. After surgery, an orthopantomography (Rx Opt) and a 3d computed tomography (3d Tc) mandibular scan were performed to demonstrate the good aesthetic result and the symmetry of the ostectomy ( Fig. 5 ).
Fig. 5.

Postoperative clinical frontal view.
The patient was satisfied with the functional and aesthetic outcomes of both the profile and the frontal views. There was no evidence of complication at a 1-year follow-up ( Fig. 6 ). No complication was observed during this period.
Fig. 6.
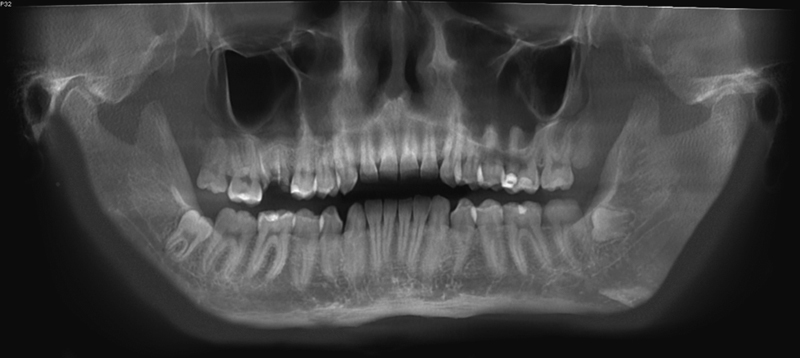
Postoperative mandibular Rx.
Discussion
According to Poch classification, there are 10 face types. 10 The masseter muscle plays an important role in facial aesthetics so that a hypertrophy of this muscle leads to an unwanted shape of the face. The etiology is not clearly understood; theories such as emotional stress, chronic bruxism, microtrauma, masseteric hyper- or parafunction have been proposed. 4 Diagnosis cannot only be based on clinical findings and there are conflicting recommendations in the literature for investigating patients presenting bilateral masseter hypertrophy. 4 Differential diagnosis must include muscle tumor, salivary gland disease, parotid tumors, parotid inflammatory diseases, and masseter muscle miopathy. 11 The traditional method of treatment for masseteric hypertrophy is the surgical partial excision of masseteric muscle under general anesthesia. 12
Currently, an intraoral approach is preferred to primarily avoid facial nerve damage and scar formation; other complications from surgical excision of the masseter include hematoma formation, facial nerve paralysis, infection, mouth opening limitation, and sequelae from general anesthesia. 12
Nonsurgical treatment can take the form of an injection of botulinum toxin type A described in 1994 by Smyth 13 and Moore and Wood 14 ; an injection in the masseter muscle inhibits acetylcholine release at the neuromuscular terminals resulting in muscle relaxation for 6 months. Reduced muscle activity leads to the reduced muscular tone and volume of the affected muscle. Complications include reduced masticatory force, facial paralysis, localized facial bruising, and pain at the injection side. The limitation of this procedure is that the effect wears off in 6 months. 12 In 2009, Ham described the use of radiofrequency coagulation for this disease to achieve the cosmetic effect results of the botulinum toxin therapy even if a surgical procedure was performed. 12
In 2013, Xu and Yu stated that the dissection of the masseter muscle from the point of attachment to the bone surface can result in a cosmetic effect as well 6 ; in fact, some animal models have shown that the masseter muscle will atrophy and the volume of the masseter muscle will reduce after dissection. 15
This article reports a new method that uses an intraoral approach associated with a titanium surgical guide built on the stereolithographic model to best perform the ostectomy and the partial removal of the buccal fat pad combined with the surgical reduction of the muscle.
Our method proposes several advantages: all procedures are performed through an intraoral incision with no external scar and a better symmetry in the ostectomy performed with the preoperatively designed titanium guide.
Conclusion
The approach presented in this article can obtain optimal aesthetic and functional results with few complications in selected patients. Even though the manipulation of the ostectomy could be improved, the aesthetic and functional results were satisfactory and the introduction of the preoperative study to provide a better ostectomy is mandatory nowadays to reach the best symmetrical outcome for the width of the lower face.
References
- 1.Addante R R. Masseter muscle hypertrophy: report of case and literature review. J Oral Maxillofac Surg. 1994;52(11):1199–1202. doi: 10.1016/0278-2391(94)90546-0. [DOI] [PubMed] [Google Scholar]
- 2.Tabrizi R, Ozkan B T, Zare S. Correction of lower facial wideness due to masseter hypertrophy. J Craniofac Surg. 2010;21(04):1096–1097. doi: 10.1097/SCS.0b013e3181e1b29b. [DOI] [PubMed] [Google Scholar]
- 3.Yoda T, Sato T, Abe T et al. Long-term results of surgical therapy for masticatory muscle tendon-aponeurosis hyperplasia accompanied by limited mouth opening. Int J Oral Maxillofac Surg. 2009;38(11):1143–1147. doi: 10.1016/j.ijom.2009.07.002. [DOI] [PubMed] [Google Scholar]
- 4.Özkan B T, Tabrizi R, Cigerim L. Management of bilateral masseter muscle hypertrophy. J Craniofac Surg. 2012;23(01):e14–e16. doi: 10.1097/SCS.0b013e31824207a2. [DOI] [PubMed] [Google Scholar]
- 5.Legg J W. Enlargement of the temporal and masseter muscles on both sides. Tr Path Soc London. 1880;31:361–366. [Google Scholar]
- 6.Xu J, Yu Y. A modified surgical method of lower-face recontouring. Aesthetic Plast Surg. 2013;37(02):216–221. doi: 10.1007/s00266-013-0080-x. [DOI] [PubMed] [Google Scholar]
- 7.Gurney C E. Chronic bilateral benign hypertrophy of the masseter muscles. Am J Surg. 1947;73(01):137–139. doi: 10.1016/0002-9610(47)90304-8. [DOI] [PubMed] [Google Scholar]
- 8.Ginestet G, Frezieres H, Merville L. [Surgical correction of hypertrophy of the masseter muscle] Ann Chir Plast. 1959;4:187–195. [PubMed] [Google Scholar]
- 9.Beckers H L. Masseteric muscle hypertrophy and its intraoral surgical correction. J Maxillofac Surg. 1977;5(01):28–35. doi: 10.1016/s0301-0503(77)80072-6. [DOI] [PubMed] [Google Scholar]
- 10.Poch H R. Bericht über die von der Wiener anthropologischen Gesellschaft in den K.u.k. Kriegsgefangenenlagern veranlassten. Studien Mitteil Anthrop Ges In Wien. 1916;46:107–131. [Google Scholar]
- 11.Rispoli D Z, Camargo P M, Pires J L, Jr, Fonseca V R, Mandelli K K, Pereira M A. Benign masseter muscle hypertrophy. Braz J Otorhinolaryngol. 2008;74(05):790–793. doi: 10.1016/S1808-8694(15)31393-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ham J W. Masseter muscle reduction procedure with radiofrequency coagulation. J Oral Maxillofac Surg. 2009;67(02):457–463. doi: 10.1016/j.joms.2006.04.012. [DOI] [PubMed] [Google Scholar]
- 13.Smyth A G. Botulinum toxin treatment of bilateral masseteric hypertrophy. Br J Oral Maxillofac Surg. 1994;32(01):29–33. doi: 10.1016/0266-4356(94)90169-4. [DOI] [PubMed] [Google Scholar]
- 14.Moore A P, Wood G D. The medical management of masseteric hypertrophy with botulinum toxin type A. Br J Oral Maxillofac Surg. 1994;32(01):26–28. doi: 10.1016/0266-4356(94)90168-6. [DOI] [PubMed] [Google Scholar]
- 15.Du B J, Liu Y S, Zheng J S, Su B. Establishment of animal model selectively denervated masseter in rabbits. J Fourth Mil Med Univ China. 2006;27(10):890–893. [Google Scholar]


