Abstract
Autogenous bone grafts are the gold standard for reconstruction of atrophic jaws, pseudoarthroses, alveolar clefts, orthognathic surgery, mandibular discontinuity, and augmentation of sinus maxillary. Bone graft can be harvested from iliac bone, calvarium, tibial bone, rib, and intraoral bone. Proximal tibia is a common donor site with few reported problems compared with other sites. The aim of this study was to evaluate the use of proximal tibia as a donor area for maxillofacial reconstructions, focusing on quantifying the volume of cancellous graft harvested by a lateral approach and to assess the complications of this technique. In a retrospective study, we collected data from 31 patients, 18 women and 13 men (mean age: 36 years, range: 19–64), who were referred to the Department of Oral and Maxillofacial Surgery at the Servidores do Estado Federal Hospital. Patients were treated for sequelae of orthognathic surgery, jaw fracture, nonunion, malunion, pathology, and augmentation of bone volume to oral implant. The technique of choice was lateral access of proximal tibia metaphysis for graft removal from Gerdy tubercle under general anesthesia. The mean volume of bone harvested was 13.0 ± 3.7 mL (ranged: 8–23 mL). Only five patients (16%) had minor complications, which included superficial infection, pain, suture dehiscence, and unwanted scar. However, none of these complications decreases the result and resolved completely. We conclude that proximal tibia metaphysis for harvesting cancellous bone graft provides sufficient volume for procedures in oral and maxillofacial surgery with minimal postoperative morbidity.
Keywords: tibia, cancellous bone graft, complications, volume bone graft, maxillofacial surgery
A variety of bone grafting materials, ranging from autologous bone to bone graft substitutes, are available in the clinical setting to enhance bone regeneration. Autologous cancellous bone grafting is the gold standard in maxillomandibular reconstruction because its properties such as osteoconduction, osteoinduction, and osteogenesis fulfil the requisites for bone repair and regeneration. 1
Bone grafting is performed to stimulate bone healing in various adverse situations, including posttraumatic skeletal complications, such as delayed unions, nonunions, malunions, and traumatic bone defects, as well as other situations, including joint fusions, avascular necrosis, and diverse reconstruction procedures. 2
Several techniques and autogenous bone grafting have been described. Donor sites vary depending on the amount and types of bone available for harvest, and each site has advantages and disadvantages. Regions such as the mandibular symphysis; rib; anterior and posterior iliac crest; and, more recently, the intercalvarial diploic bone have been used as important donor sites for bone grafting. 1 3 4 5 6 7 8
Procurement of cancellous bone from any site is not without relative biological insult to the patient. These include an additional surgical site, possible increased postoperative morbidity, weakened donor site, and potential serious complications from these conditions. 8 Among alternatives, the use of the proximal tibia as a donor site shows minimal complications as well as a satisfactory amount of bone graft.
Use of the proximal tibia as a donor site has been applied in jawbone reconstruction 3 since 1990; thus, the tibia has subsequently been used for grafting in orthognathic surgery, clef surgery, and preprosthetic surgery, and for major jaw reconstruction. 9
Several studies of bone harvesting have compared the complication rate, morbidity, and amount of cancellous bone harvested from the tibia with other donor sites such as the iliac crest. These studies have concluded that in comparison with an iliac crest graft, tibia bone harvesting is easier and quicker, with less blood loss and fewer donor site complications. 10
This article aimed to evaluate the volume of cancellous bone harvested by a lateral approach on proximal metaphysis of tibia in 31 patients at the Department of Oral and Maxillofacial Surgery, Servidores do Estado Federal Hospital (Rio de Janeiro, Brazil) and the associated complications.
Materials and Methods
A retrospective study of 31 patients (18 women and 13 men) with a median age of 35 years (range: 19–64) referred to the Oral and Maxillofacial Surgery Service at Servidores do Estado Federal Hospital (Rio de Janeiro, Brazil) was performed. The study was accepted by the Ethics Committee and Research of the Servidores do Estado Federal Hospital (CEP 731470).
The inclusion criteria were ASA I, II and III patients, without presence of infection, metabolic or metastatic bone disease, or trauma to the extremity that would further compromise the integrity of the leg. Indications for reconstruction using tibial graft were sequelae of orthognathic surgery, jaw fracture, nonunion, pathology, and augmentation of bone volume in oral implantology.
The surgical technique used to harvest the cancellous graft was lateral approach from the Gerdy tubercle on the proximal metaphysis of the tibia. Gerdy tubercle is the insertion site of the iliotibialis tract on the proximal and lateral aspects of the tibia. This bony protuberance is almost subcutaneous and it is exposed with minimal dissection. 11 The major anatomic landmarks are the patella, patellar ligament, tibial tuberosity, and fibular head, which were palpated. The tibial tuberosity is localized below the midline of the knee, and the fibular head is found laterally. The Gerdy tubercle is located between these structures ( Figs. 1 and 2 ).
Fig. 1.
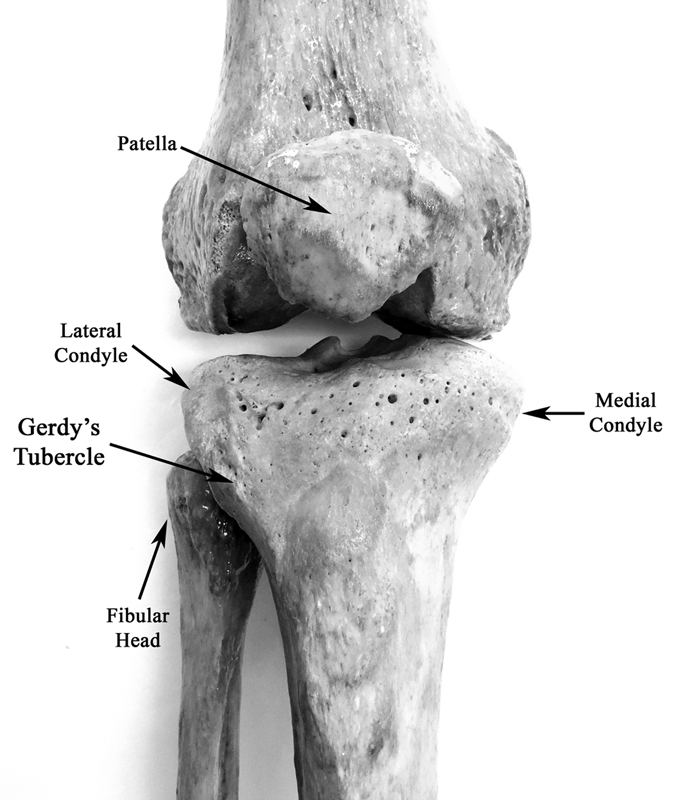
Anterior view of knee showing the anatomic landmarks to access the Gerdy tubercle in the tibia bone.
Fig. 2.
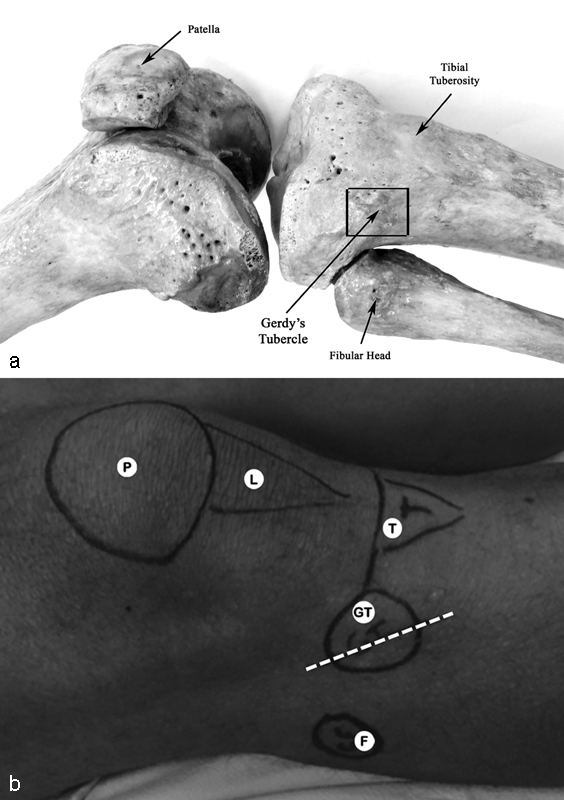
Anterolateral view of knee showing the anatomic landmarks in the bones involved with the access to Gerdy tubercle ( a ) and in the patient during transoperatory period ( b ). P, patella; L, patellar ligament; T, tibial tuberosity; F, fibular head; and GT, Gerdy tubercle. The square in ( a ) marks the location for the osteotomy to create a bony window of 2.0 × 2.0 cm over the Gerdy tubercle with a drill to harvest the cancellous bone with curettes. The interrupted line in ( b ) marks the location of the incision (a 3- to 4-cm oblique skin incision was made superolaterally to inferomedially paralleling the tendinous fibers over the Gerdy tubercle). No tourniquet was used.
Surgical procedures were performed under general anesthesia, and Cefazolin 2 g (Kefazol, ABL LTDA., Cosmópolis, SP, Brazil) was used preoperatively and intraoperatively. Patients were positioned supine with the knee flexed to approximately 45degrees to elevate the anterolateral surface of the tibia. Antisepsis with povidone-iodine solution was then conducted to obtain a sterilized field. Anatomic bony landmarks were palpated and highlighted with a sterile skin marker pen. The midpoint of a line from the fibular head to the anterior tibial tuberosity reveals the location of the Gerdy tubercle, which was palpated and marked ( Figs. 1 and 2 ). Once the Gerdy tubercle was localized, the soft tissue was infiltrated with 2% xylocaine with 1:100.000 epinephrine to promote proper vasoconstriction and facilitate the incision.
A 3- to 4-cm oblique skin incision was made superolaterally to inferomedially paralleling the tendinous fibers over the Gerdy tubercle. Dissection was performed through the subcutaneous tissue and iliotibial tract to expose the bony prominence. Then, the periosteum was incised and elevated. The correct identification of bony landmarks is essential to avoid neurovascular structures during dissection, which is relatively safe. Electrocoagulation was utilized to manage any hemorrhage.
Osteotomy using a drill bit was performed to create a bony window of 2.0 × 2.0 cm square over the Gerdy tubercle. Cancellous bone was harvested with curettes medially to laterally until cortical bone was reached and inferiorly. Thus, the maximum possible amount of cancellous marrow bone was harvested from the proximal tibial metaphysis ( Fig. 3 ). Caution was taken superiorly to avoid the tibial plateau and joint space. The cancellous bone graft was placed into a 20-mL syringe to measure the bone volume ( Fig. 4 ).
Fig. 3.
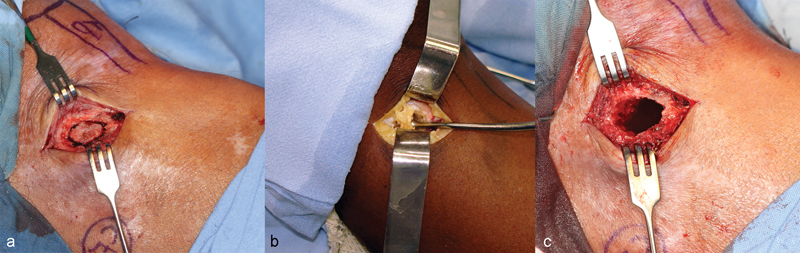
( a ) The window formed over the Gerdy tubercle during osteotomy. ( b ) Cancellous tibial bone harvested with curettes. ( c ) The aspect of bone after the curettage.
Fig. 4.

Cancellous bone graft into a 20-mL syringe to measure the bone volume. Note a volume of 15 mL harvested in this case.
After bone graft removal, the area was irrigated with sterile saline. The closure of the iliotibial tract and subcutaneous tissue was performed with 3.0 polyglactin (Vicryl, Ethicon, LLC, Somerville, NJ). Skin was closed with 3.0 nylon (Mononylon, Ethicon, M & I Medical) and a bulky gauze dressing was placed on the wound with a light-pressure bandage.
During postoperative care, the patients were instructed to keep the site of incision dry for 48 hours, to avoid weight bearing on the operated leg for 3 weeks, and to always use a stick to walk. Sutures were removed after 10 to 14 days. Analgesia was achieved with metamizole (Novalgina, Sanofi-Aventis Farmacêutica Ltda, Suzano, São Paulo, Brazil), and ibuprofen was used as a nonsteroidal anti-inflammatory drug (Alivium; Mantecorp LTDA, Rio de Janeiro, Brazil).
Results
A total of 18 women (average age: 37, age range: 21–64 years) and 13 men (average age: 35, age range: 19–57 years) were included in the study. We used a lateral approach to remove a cancellous tibial bone graft from the Gerdy tubercle on the proximal metaphysis of the tibia on the upper extremity. Indications for reconstruction using a tibial graft were sequelae of orthognathic surgery ( n = 1), jaw fracture ( n = 8), nonunion of the jaw fracture ( n = 2), pathology ( n = 12), and bone volume augmentation in oral implantology ( n = 8) ( Table 1 ).
Table 1. Distribution of patients, the volume of graft harvested from the proximal tibial site by lateral approach, and complications.
| Gender | Age | Indication | Volume | Complication |
|---|---|---|---|---|
| F | 21 | Orthognathic sequel | 14 | No |
| F | 22 | Pathology | 15 | Local pain |
| F | 22 | Pathology | 15 | Superficial infection |
| F | 24 | Implantology | 12 | No |
| F | 24 | Fracture sequel | 18 | No |
| F | 31 | Pathology | 14 | No |
| F | 33 | Pathology | 17 | No |
| F | 34 | Fracture sequel | 8 | No |
| F | 64 | Pathology | 11 | No |
| F | 35 | Pathology | 9 | No |
| F | 38 | Implantology | 9 | No |
| F | 38 | Fracture sequel | 10 | No |
| F | 41 | Implantology | 20 | No |
| F | 43 | Fracture sequel | 9 | No |
| F | 43 | Fracture sequel | 13 | Suture dehiscence |
| F | 48 | Pathology | 16 | No |
| F | 48 | Pathology | 16 | No |
| F | 49 | Pathology | 12 | No |
| Mean | 37 | 13.5 | ||
| SD | 12 | 3.4 | ||
| Min | 21 | 8 | ||
| Max | 64 | 20 | ||
| Gender | Age | Indication | Volume | Complication |
| M | 19 | Fracture sequel | 9 | No |
| M | 22 | Pathology | 15 | No |
| M | 23 | Fracture sequel | 8 | No |
| M | 23 | Fracture sequel | 10 | No |
| M | 25 | Pathology | 15 | Local pain |
| M | 28 | Implantology | 13 | No |
| M | 33 | Nonunion | 10 | No |
| M | 36 | Implantology | 9 | No |
| M | 40 | Implantology | 23 | No |
| M | 44 | Implantology | 10 | No |
| M | 45 | Nonunion | 10 | Unaesthetic scar |
| M | 56 | Pathology | 15 | No |
| M | 57 | Implantology | 14 | No |
| Mean | 35 | 12.4 | ||
| SD | 13 | 4.1 | ||
| Min | 19 | 8 | ||
| Max | 57 | 23 |
Abbreviations: F, female; M, man; m, media; max, maximal; min, minimal; SD, standard deviation.
The mean amount of graft harvested from the tibial site by the lateral approach was 13.0 ± 3.7 mL (range: 8–23 mL) ( Table 1 ). This volume was sufficient in all surgical procedures.
At the donor site, only five patients (16%) exhibited minor morbidity, and all complications were resolved during outpatient care ( Table 1 ). In three cases, whose indications for graft harvesting were pathology and fracture sequel, local pain and suture dehiscence occurred. Pain was managed with oral analgesics for 1 week, and no debridement was necessary for dehiscence. In another case whose indication for graft harvesting was a sequela of jaw fracture, an unaesthetic scar could be noted at the donor site. Infiltration with corticosteroids for 2 weeks was performed successfully. Finally, one patient who received a graft for nonunion of a jaw fracture had a superficial infection. Antisepsis with local chlorhexidine 2% for 2 weeks and oral antibiotics for 1 week reversed the case. Follow-up of approximately 6 months was performed, and all complications resolved in approximately 3 weeks.
No patients had hard infection, gait disturbance, hematoma formation, fractures, paresthesia, or other donor site complications. In general, all patients were satisfied with the surgical procedure and exhibited excellent recovery of the donor site.
Discussion
Autologous bone graft is the gold standard for reconstructions in maxillofacial surgeries because these grafts possess properties required for grafting success, such as osteoconduction, osteoinduction, and osteogenesis. The physiological process of bone reconstruction involves the union of these three processes. Cancellous tibial bone possesses all of these characteristics and is therefore an excellent graft for orofacial procedures. Cancellous bone grafts harvested from the proximal tibia are used in oral and maxillofacial surgery for filling the osteotomy gap in orthognathic surgery, alveolar cleft bone grafting, alveolar ridge augmentation, maxillary sinus grafting, and other maxillomandibular reconstructions. 3 4 8
Using the lateral approach, Catone and colleagues 8 obtained a noncompressed volume of 25 mL of cancellous bone from the proximal tibial metaphysis in 21 cases. Other studies of cadavers yielded similar amounts of bone. 12 A retrospective study of 78 patients who underwent 80 cancellous tibial graft procurements as part of their maxillofacial procedures revealed a mean graft volume of 17.8 ± 5.3 mL (range: 8–32 mL). 3 In our study, the amount of proximal tibial bone harvested by the lateral approach from the 31 patients was satisfactory for all procedures, with a mean volume of 13.0 ± 3.7 mL (range: 8–23 mL). Correlations with quantity, degree of morbidity, operating time, postoperative complications, surgical complexity, and removal of cancellous bone graft are more attractive for the proximal tibial bone than for other sites.
Equal amounts of bone graft material are procurable from the medial and lateral aspects of the proximal tibia. 7 Some authors prefer the medial approach to the proximal tibia because medial approach offers an easily palpable bone plane and avoids potential injury to important structures, such as detachment of the anterior tibial muscle and trauma of the anterior tibial recurrent artery, which decreases surgical trauma. 13 14 A study suggested that the medial proximal tibial bone harvest approach had fewer serious structures in harm's way compared with the lateral; however, the lateral approach would have the benefit of muscle coverage and therefore healing might be expedited in particular patient sub-groups. 15 Thus, each approach can benefit different patient subgroups ( Fig. 5 ).
Fig. 5.
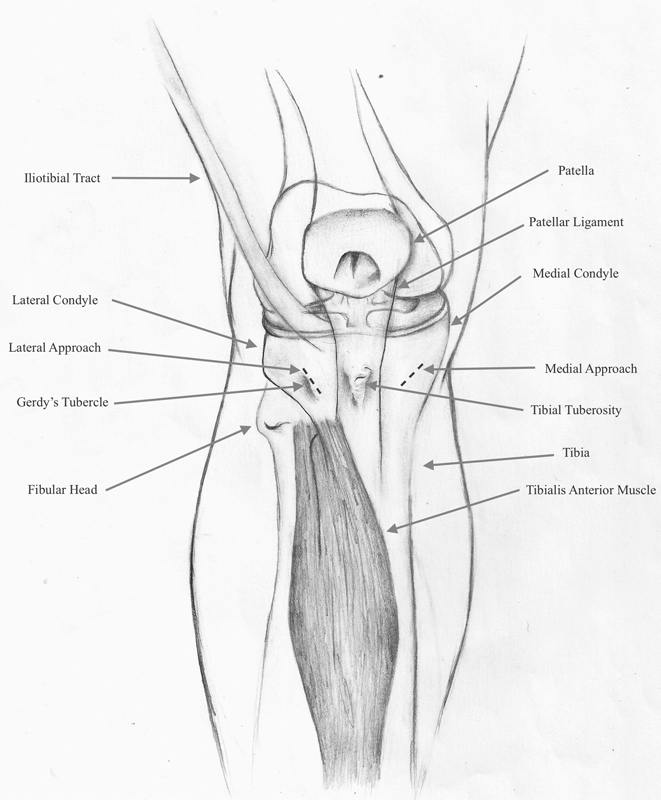
Anterior view of knee to show anatomic landmarks and incisions to lateral and medial approaches.
In accordance with many authors, 5 8 11 16 we consider that the lateral approach has advantages over the medial approach because the Gerdy tubercle is a prominent anatomic landmark to perform a safe skin incision that avoids the anterior tibial muscle and local vessels and nerves. The lateral approach also features a smaller required angle of hand instrumentation to access nearly all the procurable area of the tibial plateau. Thus, less effort and time are expended. 17
Engelstad et al performed a study of 10 fresh frozen cadavers to compare the amount of volume of cancellous bone harvested from donor sites (anterior iliac crest, posterior iliac crest, and proximal tibia) within the same cadaver. The results showed that the bone volumes from the proximal tibia (11.3 mL) and posterior iliac crest (10.1 mL) were significantly greater than those from the anterior iliac crest (7.0 mL). In uncompressed volume groups, the mean volume of cancellous bone from the proximal tibia (15.2 mL) was higher than that from the anterior and posterior iliac crests. The mean volume of uncompressed cancellous bone from the posterior iliac crest (11.7 mL) was greater than that from the anterior iliac crest (10.4 mL), but the difference was not statistically significant. 18
Many studies have reported significant complications when the iliac crest is removed compared with tibia bone grafts. Studies reported that 25% of patients who have been treated with autogenous bone harvested from the iliac crest experience postoperative pain at an average of 5 years after surgery. 19 Furthermore, in addition to pain, 6 to 20% of patients experience hypersensitivity or numbness in the buttocks, and 3 to 9% of patients report major complications with hernia or even peritoneal perforation. 20 Thus, compared with iliac crest harvesting, tibia bone removal is easier and quicker, is associated with less blood loss and fewer donor site complications, and offers a source of low–to-moderate volumes of autologous bone. 21
Harvesting bone grafts from the proximal tibia is safe, effective, and with a relatively low amount of adverse outcomes, but should be careful while using because it is not completely without adverse outcomes. Schmidt and Townsend described a case of a 47-year-old patient with a medical history of controlled hypertension, asthma, osteoporosis, and osteoarthritis of the hands and knees and using alendronate. After the surgery to augmentation maxillary sinus using tibial bone graft, the tibial bone progressed with osteomyelitis that was treated with appropriate antibiotics and debridement. 22 Possible causes of infection in this case might include the fact that the patient was taking alendronate, an oral bisphosphonate that is known to produce localized bone vascular insufficiency and inhibit normal bone turnover remodeling. 23 This fact serves to alert clinicians about these kind of patients.
In this article, 5 of 31 patients had minor complications that did not impair the outcome and were resolved in a few weeks. In three cases, local pain and suture dehiscence were observed. In another case, an unaesthetic scar was noted. Finally, one patient had a superficial infection. All complications resolved in approximately 3 weeks with appropriate management. No patients exhibited hard infection, hematoma formation, fractures, paresthesia, or other donor site complications.
O'Keeffe et al reported 230 cases of bone grafts harvested from the proximal tibia. One case of fracture occurred in a patient who, despite being non weight bearing for 6 weeks, experienced an undisplaced fracture on the tibia eminence. 24 Hughes and Revington reported 2 proximal tibia fractures among 75 cases. One case (a displaced fracture) occurred during a school sport 3 months following the harvest; the second (an undisplaced stress fracture) was noted 9 days postoperatively following a fall. 4 Ohya et al reported a case of a woman who fell while removing her slacks 3 months after tibia bone harvesting and suffered spontaneous pain in the left tibia at the site of bone removal. 25
There is no difference in the force required to induce a tibial plateau fracture between the intact and decancellated proximal tibia. Cases of fracture have occurred when patients performed weight bearing. 4 16 24 Our patients were instructed to avoid weight bearing for 3 weeks and to avoid contact with sports for 6 months. No cases of fracture occurred. In a study conducted by Kim et al, only 4 of 105 tibial graft patients experienced tibial fracture, and all fractures occurred between 2 and 7 weeks after surgery and were caused by external trauma. Because tibial fractures occurred only during this specific period, the authors concluded that patient education is a very important factor to prevent tibial fractures. The authors assumed that tibial fractures are vulnerable to direct or indirect external trauma rather than physical condition, such as body weight or age. 26
Conclusion
We conclude that proximal tibia metaphysis for harvesting cancellous bone graft provides sufficient volume for maxillofacial surgery procedures with minimal postoperative morbidity.
Footnotes
Conflict of Interest None.
References
- 1.Vittayakittipong P, Nurit W, Kirirat P. Proximal tibial bone graft: the volume of cancellous bone, and strength of decancellated tibias by the medial approach. Int J Oral Maxillofac Surg. 2012;41(04):531–536. doi: 10.1016/j.ijom.2011.10.023. [DOI] [PubMed] [Google Scholar]
- 2.De Long W G, Jr, Einhorn T A, Koval K et al. Bone grafts and bone graft substitutes in orthopaedic trauma surgery. A critical analysis. J Bone Joint Surg Am. 2007;89(03):649–658. doi: 10.2106/JBJS.F.00465. [DOI] [PubMed] [Google Scholar]
- 3.Ko E C, Chang C M, Chang P et al. Tibial cancellous bone grafting in jaw reconstruction: 10 years of experience in Taiwan. Clin Implant Dent Relat Res. 2015;17 01:e321–e331. doi: 10.1111/cid.12150. [DOI] [PubMed] [Google Scholar]
- 4.Hughes C W, Revington P J.The proximal tibia donor site in cleft alveolar bone grafting: experience of 75 consecutive cases J Craniomaxillofac Surg 2002300112–16., discussion 17 [DOI] [PubMed] [Google Scholar]
- 5.Mazock J B, Schow S R, Triplett R G. Proximal tibia bone harvest: review of technique, complications, and use in maxillofacial surgery. Int J Oral Maxillofac Implants. 2004;19(04):586–593. [PubMed] [Google Scholar]
- 6.Gerressen M, Riediger D, Marx R, Saxe J, Ghassemi A. Stability behavior of human tibias after bone removal—comparative examination in 15 cadaver tibia pairs. J Oral Maxillofac Surg. 2010;68(01):60–67. doi: 10.1016/j.joms.2009.03.058. [DOI] [PubMed] [Google Scholar]
- 7.Herford A S, King B J, Audia F, Becktor J. Medial approach for tibial bone graft: anatomic study and clinical technique. J Oral Maxillofac Surg. 2003;61(03):358–363. doi: 10.1053/joms.2003.50071. [DOI] [PubMed] [Google Scholar]
- 8.Catone G A, Reimer B L, McNeir D, Ray R. Tibial autogenous cancellous bone as an alternative donor site in maxillofacial surgery: a preliminary report. J Oral Maxillofac Surg. 1992;50(12):1258–1263. doi: 10.1016/0278-2391(92)90223-m. [DOI] [PubMed] [Google Scholar]
- 9.Besly W, Ward Booth P. Technique for harvesting tibial cancellous bone modified for use in children. Br J Oral Maxillofac Surg. 1999;37(02):129–133. doi: 10.1054/bjom.1998.0433. [DOI] [PubMed] [Google Scholar]
- 10.Ilankovan V, Stronczek M, Telfer M, Peterson L J, Stassen L F, Ward-Booth P. A prospective study of trephined bone grafts of the tibial shaft and iliac crest. Br J Oral Maxillofac Surg. 1998;36(06):434–439. doi: 10.1016/s0266-4356(98)90459-4. [DOI] [PubMed] [Google Scholar]
- 11.Brutus J P, Loftus J B. Gerdy's tubercle as a source of cancellous bone graft for surgery of the upper extremity: description of technique. J Hand Surg Am. 2006;31(01):147–149. doi: 10.1016/j.jhsa.2005.07.011. [DOI] [PubMed] [Google Scholar]
- 12.Gerressen M, Prescher A, Riediger D, van der Ven D, Ghassemi A. Tibial versus iliac bone grafts: a comparative examination in 15 freshly preserved adult cadavers. Clin Oral Implants Res. 2008;19(12):1270–1275. doi: 10.1111/j.1600-0501.2008.01621.x. [DOI] [PubMed] [Google Scholar]
- 13.Hernández-Alfaro F, Martí C, Biosca M J, Gimeno J. Minimally invasive tibial bone harvesting under intravenous sedation. J Oral Maxillofac Surg. 2005;63(04):464–470. doi: 10.1016/j.joms.2004.07.020. [DOI] [PubMed] [Google Scholar]
- 14.Jakse N, Seibert F J, Lorenzoni M, Eskici A, Pertl C. A modified technique of harvesting tibial cancellous bone and its use for sinus grafting. Clin Oral Implants Res. 2001;12(05):488–494. doi: 10.1034/j.1600-0501.2001.120509.x. [DOI] [PubMed] [Google Scholar]
- 15.Benninger B, Ross A, Delamarter T. Approaches to proximal tibial bone harvest techniques. J Oral Maxillofac Res. 2012;3(02):e2. doi: 10.5037/jomr.2012.3202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Thor A, Farzad P, Larsson S. Fracture of the tibia: complication of bone grafting to the anterior maxilla. Br J Oral Maxillofac Surg. 2006;44(01):46–48. doi: 10.1016/j.bjoms.2005.02.011. [DOI] [PubMed] [Google Scholar]
- 17.Kushner G M. Tibia bone graft harvest technique. Atlas Oral Maxillofac Surg Clin North Am. 2005;13(02):119–126. doi: 10.1016/j.cxom.2005.05.001. [DOI] [PubMed] [Google Scholar]
- 18.Engelstad M E, Morse T. Anterior iliac crest, posterior iliac crest, and proximal tibia donor sites: a comparison of cancellous bone volumes in fresh cadavers. J Oral Maxillofac Surg. 2010;68(12):3015–3021. doi: 10.1016/j.joms.2010.07.056. [DOI] [PubMed] [Google Scholar]
- 19.Leonetti J A, Koup R. Localized maxillary ridge augmentation with a block allograft for dental implant placement: case reports. Implant Dent. 2003;12(03):217–226. doi: 10.1097/01.id.0000078233.89631.f8. [DOI] [PubMed] [Google Scholar]
- 20.Zemann W, Feichtinger M, Kowatsch E, Kärcher H. Extensive ameloblastoma of the jaws: surgical management and immediate reconstruction using microvascular flaps. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103(02):190–196. doi: 10.1016/j.tripleo.2006.05.004. [DOI] [PubMed] [Google Scholar]
- 21.Wang K, Almeida L E, Olsson A B. Volume analysis of the proximal tibial metaphysis. J Oral Maxillofac Surg. 2007;65(12):2425–2429. doi: 10.1016/j.joms.2007.04.009. [DOI] [PubMed] [Google Scholar]
- 22.Schmidt E R, Townsend J. Unusual complication of subacute osteomyelitis following tibial bone graft: report of a case. J Oral Maxillofac Surg. 2008;66(06):1290–1293. doi: 10.1016/j.joms.2007.04.036. [DOI] [PubMed] [Google Scholar]
- 23.Ruggiero S L, Mehrotra B, Rosenberg T J, Engroff S L. Osteonecrosis of the jaws associated with the use of bisphosphonates: a review of 63 cases. J Oral Maxillofac Surg. 2004;62(05):527–534. doi: 10.1016/j.joms.2004.02.004. [DOI] [PubMed] [Google Scholar]
- 24.O'Keeffe R M, Jr, Riemer B L, Butterfield S L. Harvesting of autogenous cancellous bone graft from the proximal tibial metaphysis. A review of 230 cases. J Orthop Trauma. 1991;5(04):469–474. doi: 10.1097/00005131-199112000-00014. [DOI] [PubMed] [Google Scholar]
- 25.Ohya M, Fujimoto T, Ito Y, Watabe M, Yamamoto N, Ueda M. Tibial bone fracture after bone harvesting from the tibia. Asian J Oral Maxillofac Surg. 2008;20:106–109. [Google Scholar]
- 26.Kim I K, Cho H Y, Pae S P, Jung B S, Cho H W, Seo J H. Tibial bone fractures occurring after medioproximal tibial bone grafts for oral and maxillofacial reconstruction. J Korean Assoc Oral Maxillofac Surg. 2013;39(06):257–262. doi: 10.5125/jkaoms.2013.39.6.257. [DOI] [PMC free article] [PubMed] [Google Scholar]


