Abstract
Hemangiomas are benign tumors representing only 0.7 to 1% of all bone tumors; those that arise in the zygomatic region are rarely described in the literature. Here, we describe the case of a 55-year-old woman with a mass in the right orbitozygomatic region. She was diagnosed on the basis of preoperative clinical manifestations, data from an earlier histopathological examination, and computed tomography (CT). The CT scan revealed a lesion in the right zygomatic region at the level of the cancellous component. This caused thinning and remodeling of the deformed cortex both medially and laterally. Surgery was performed. We describe the clinical characteristics of our case with an emphasis on surgical management of the lesion using a titanium grid prepared by reference to a stereolithographic model.
Keywords: hemangioma, zygoma, reconstruction
A variety of benign tumors arise from bone. Primary intraosseous vascular lesions are slow-growing benign abnormalities that account for less than 1% of all osseous tumors. 1 2 3 4
Intraosseous hemangiomas are uncommon benign tumors arising from bone, and occur principally in the vertebral column and skull bones. 5 Among maxillofacial tumors, most intraosseous hemangiomas develop in the mandible and maxilla, and rarely in the zygoma. Fewer than 40 cases, including our present case, have been reported in the literature to date. 1 Intraosseous venous malformations present a unique clinical challenge to any maxillofacial surgeon interested in facial reconstruction.
We present an uncommon case of a patient diagnosed with an intraosseous hemangioma and swelling of the zygomatic bone; we discuss our surgical and reconstructive procedures.
Case Presentation
A 55-year-old woman was referred to the Operative Unit for Maxillofacial Surgery, Spedali Civili Brescia, Italy, with a right-sided orbitozygomatic hard swelling that had developed 5 years ago; the pain was not aggravated by palpation. She reported that the lesion was growing. There was no history of trauma or any other event that might explain symptom onset.
On physical examination, neither facial nerve paralysis nor disturbance in facial sensation was apparent. There was no evidence of proptosis or a visual deficit. Anamnesis revealed that, 5 years prior, an incisional biopsy had yielded a diagnosis of an intraosseous hemangioma. Earlier surgery had employed a transconjunctival approach with curettage of the region ( Fig. 1 ).
Fig. 1.

Preoperative clinical view.
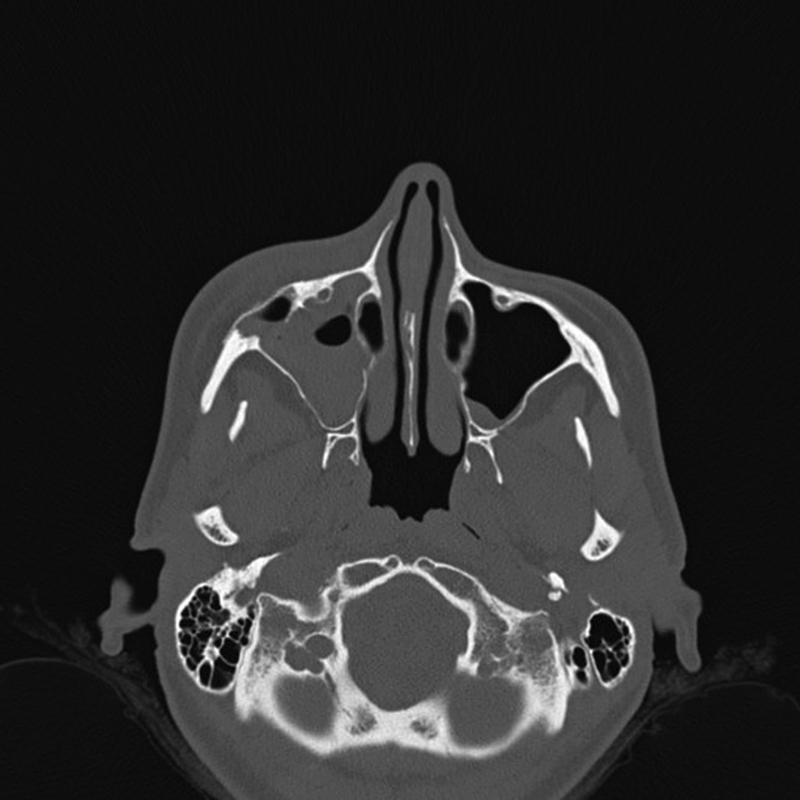
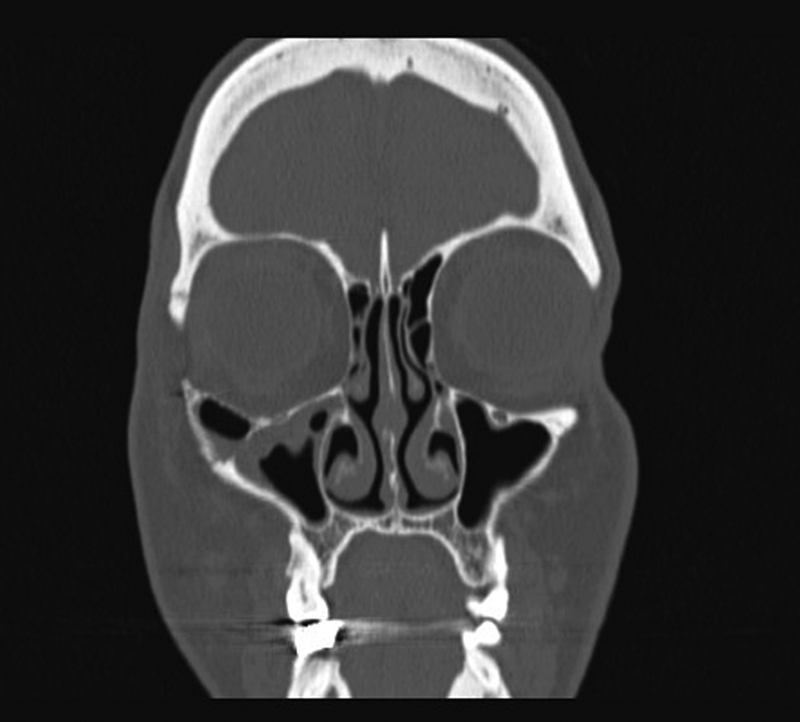
Computed tomography (CT) scans revealed a lesion in the right orbitozygomatic region at the level of the cancellous component, causing thinning and remodeling of the deformed cortex both medially and laterally. On the medial side, the cortical bone was so thin and decalcified (over short stretches) to render it barely recognizable ( Fig. 2 ). We found no sign of infiltration of nearby structures. As both the CT scans and the previous biopsy indicated that the lesion was benign, we did not perform an exploratory biopsy.
Fig. 2.
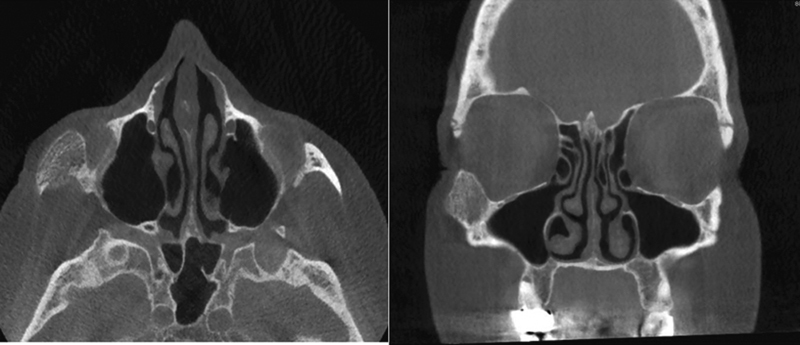
A computed tomography axial and coronal views of the lesion.
Before surgery, we used a stereolithographic model to plan an optimal corrective ostectomy. We constructed a titanium grid with the aid of the model both to facilitate surgery and to achieve an optimal aesthetic outcome.
Surgery was performed under general anesthesia. We employed a transconjunctival approach with lateral canthotomy to expose the surgical field. Incision was followed by exposure of the mass. The lesion was completely removed from adjacent bone using a 3-mm-wide chisel. The orbitozygomatic region was reconstructed using a titanium grid (Johnson and Johnson, New Brunswick, NJ) to afford support to adjacent structures ( Figs. 3 4 ). The surrounding soft tissues were intact. CT was performed immediately after surgery to evaluate the symmetry of reconstruction ( Figs. 5 6 ).
Fig. 3.
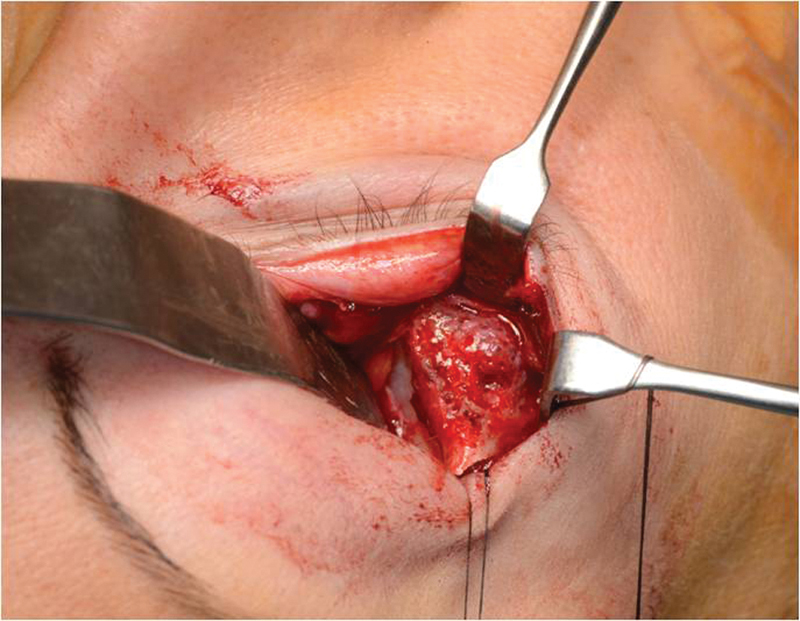
An intraoperative view of the transconjunctival approach employing lateral canthotomy.
Fig. 4.
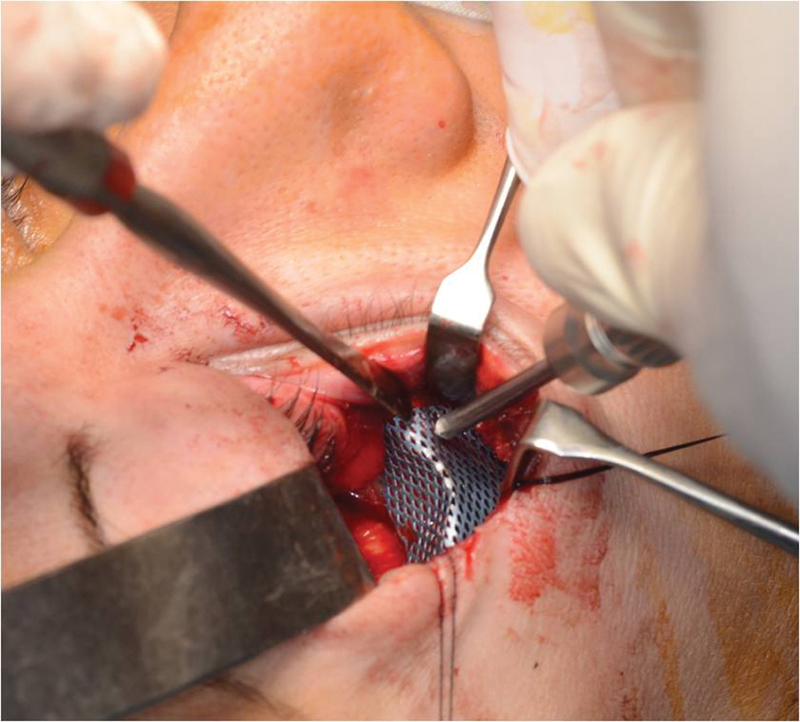
An intraoperative view of reconstruction during positioning of the grid.
Fig. 5.
A computed tomography axial view taken immediately postoperatively showing the titanium grid and the symmetry of the zygomatic region.
Fig. 6.
A computed tomography coronal view taken immediately postoperatively showing the symmetry of the orbital floor.
Macroscopically, the specimen was a nodular mass 2.3 × 1.7 × 1.9 cm in dimensions. Microscopically, hemangiomas are characterized by endothelial cell proliferation (without atypia) forming a variable pattern of vascular spaces. The thin walls of these cavernous spaces are lined by a single layer of endothelial cells interspersed with bony trabeculae ( Fig. 7 ).
Fig. 7.
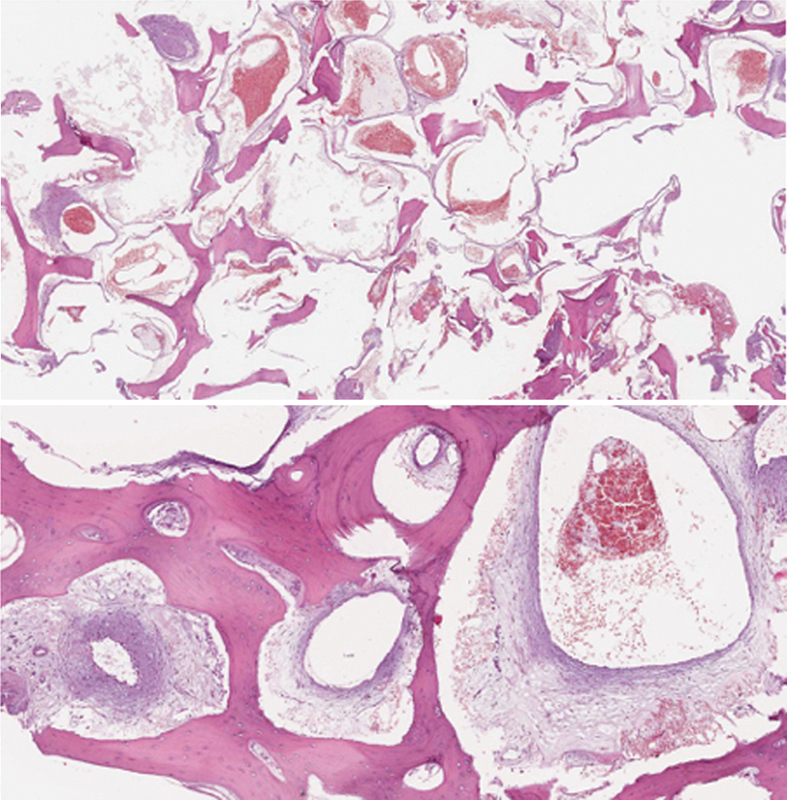
Endothelial cell-lined line vascular spaces lacking atypia interspersed with fibrous connective tissue stroma and bony trabeculae.
Our patient has currently been followed up for 18 months with no evident recurrence ( Fig. 8 ).
Fig. 8.

Postoperative clinical view.
Discussion
An intraosseous hemangioma is a rare, slow-growing tumor arising from a newly formed blood vessel. 6 The tumor was first described in 1845 by Toynbee 7 from the parietal bone. In 1950, Schofield 8 described the first hemangioma of the zygomatic bone.
In 1982, Mulliken and Glowacki 9 developed specific clinical, histochemical, and cellular criteria differentiating the various vascular anomalies into two basic clinical entities: hemangiomas and vascular malformations. The landmark work of Enjolras and Mulliken distinguished vascular tumors from vascular malformations using clinical, radiological, and histopathological features. 10 11 12 This system was adopted by the International Society for the Study of Vascular Anomalies in 1996.
The etiology of intraosseous hemangioma remains unclear. 13 The cause may be traumatic or congenital. 14 Histologically, these cases are divided into capillary, cavernous, and mixed types, 5 although most hemangiomas of facial bones are cavernous. 15 Such hemangiomas are composed of thin-walled vascular structures covered by endothelial cells. 16 The capillary type of hemangioma exhibits small-vessel proliferation with a prominent stromal component.
The peak incidence of these bony malformations typically occurs in the fourth or fifth decade of life, with a 3:1 female-to-male predominance. 1 4 17 The lesions may be completely asymptomatic, although some are associated with pain and swelling. 18
The differential diagnoses include osteosarcoma, osteoma, multiple myeloma, intraosseous meningioma, and fibrous dysplasia, 4 13 19 20 as well as metastasis of a renal tumor. 21
CT is the most useful imaging technique, affording excellent trabecular and cortical detail. The CT presentation is variable. The calvaria usually host a characteristic, sharply marginated expansile lesion with intact inner and outer tables and trabeculae radiating in a sunburst pattern. “Soap bubble” and “honeycomb” configurations have also been described.
The magnetic resonance (MR) imaging characteristics of a hemangioma depend on the extent of slow-moving venous blood and the ratio of red to converted fatty marrow within the lesion. Signal intensities may be either low or high on T1-weighted images, but are high on water-sensitive sequences. 22 Small lesions may appear bright on T1-weighted images; however, in larger lesions, the trabeculae are typically of low signal intensity on such images. When a round, potentially benign bone lesion is initially detected on MR images, the lesion may be confused with other diseases, including malignancy. 4
Open surgery with complete excision has always been the therapy of choice, and is associated with a low recurrence rate. 1 Some authors advocate less invasive procedures such as curettage, but these are associated with higher recurrence rates. 23
Full restoration of the maxillary sinus walls after trauma is important to ensure normal sinus function. If bone healing is poor, and bone loss develops even after placement of a titanium grid, sinus function can be disturbed, imparting a predisposition toward sinusitis. 24
Many authors recommend either embolization or external carotid ligation, 4 18 25 26 while others find that proximal vascular control is unnecessary if the margin of normal bone is adequate after resection. 4 25 27
Radiotherapy stops progression of the lesion, but does not address the cosmetic deformity and may cause tissue necrosis, slowing down bone and tooth growth, and causing telangiectasis and malignant degeneration 18 ( Fig. 9 ).
Fig. 9.
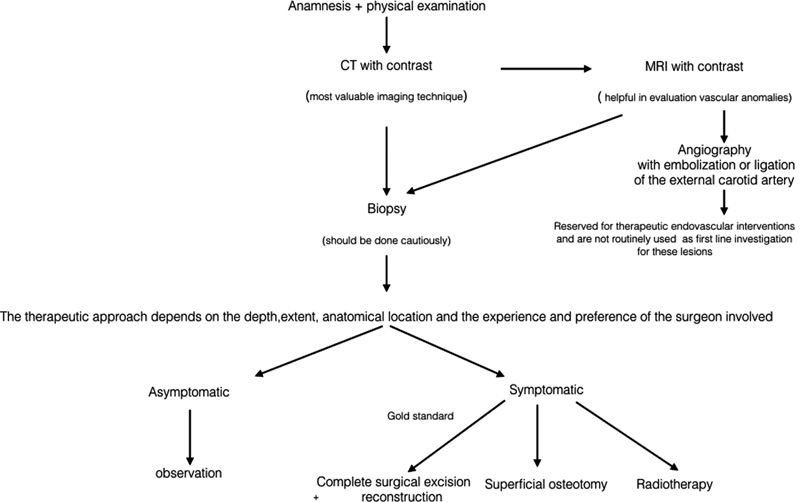
Algorithm of proper diagnostic steps and management.
Various reconstructive methods have been proposed, including resection without repair, or repair using a surgical pack, silicone implant, hydroxyapatite, autogenous rib graft, pedicled flap from the infratemporal fossa, or autogenous free iliac bone grafts. 27
The best therapeutic approach toward correction of a venous malformation depends on the depth, extent, and anatomical location of the lesion, and on the experience and preference of the surgeon. 28 We decided to use a stereolithographic model to prepare a titanium grid. Placement of this grid allowed us to completely excise the lesion, obtain an optimal reconstructive result, reduce the surgical time, and minimize the complications (including recurrence) that can develop after curettage.
Conclusion
The zygoma is critical to facial aesthetics. We removed the lesion and replaced the bone with a titanium grid constructed with the aid of a stereolithographic model. This afforded optimal aesthetic and reconstructive results.
Note
The English in this document has been checked by at least two professional editors, both native speakers of English. For a certificate, please see: http://www.textcheck.com/certificate/MSHGYj
References
- 1.Srinivasan B, Ethunandan M, Van der Horst C, Markus A F. Intraosseous ‘haemangioma’ of the zygoma: more appropriately termed a venous malformation. Int J Oral Maxillofac Surg. 2009;38(10):1066–1070. doi: 10.1016/j.ijom.2009.05.010. [DOI] [PubMed] [Google Scholar]
- 2.Yu M S, Kim H C, Jang Y J. Removal of a nasal bone intraosseous venous malformation and primary reconstruction of the surgical defect using open rhinoplasty. Int J Oral Maxillofac Surg. 2010;39(04):394–396. doi: 10.1016/j.ijom.2009.12.016. [DOI] [PubMed] [Google Scholar]
- 3.Wassef M, Vanwijck R, Clapuyt P, Boon L, Magalon G.Vascular tumours and malformations, classification, pathology and imaging [in French] Ann Chir Plast Esthet 200651(4–5):263–281. [DOI] [PubMed] [Google Scholar]
- 4.Moore S L, Chun J K, Mitre S A, Som P M. Intraosseous hemangioma of the zygoma: CT and MR findings. AJNR Am J Neuroradiol. 2001;22(07):1383–1385. [PMC free article] [PubMed] [Google Scholar]
- 5.Kim T H, Lim E J, Lee J K, Lee J G, Han M H. Intraosseous hemangioma of the middle turbinate misdiagnosed as a nasal polyp. Case Rep Otolaryngol. 2014;2014:217349. doi: 10.1155/2014/217349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dhupar V, Yadav S, Dhupar A, Akkara F. Cavernous hemangioma--uncommon presentation in zygomatic bone. J Craniofac Surg. 2012;23(02):607–609. doi: 10.1097/SCS.0b013e31824cd7c4. [DOI] [PubMed] [Google Scholar]
- 7.Toynbee J. An account of two vascular tumors developed in the substance of bone. Lancet. 1845;2:676. [Google Scholar]
- 8.Schofield A L. Primary hemangioma of the malar bone. Br J Plast Surg. 1950;3(02):136–140. doi: 10.1016/s0007-1226(50)80021-8. [DOI] [PubMed] [Google Scholar]
- 9.Mulliken J B, Glowacki J. Hemangiomas and vascular malformations in infants and children: a classification based on endothelial characteristics. Plast Reconstr Surg. 1982;69(03):412–422. doi: 10.1097/00006534-198203000-00002. [DOI] [PubMed] [Google Scholar]
- 10.Mulliken J B, Fishman S J, Burrows P E. Vascular anomalies. Curr Probl Surg. 2000;37(08):517–584. doi: 10.1016/s0011-3840(00)80013-1. [DOI] [PubMed] [Google Scholar]
- 11.Enjolras O, Mulliken J B. Vascular tumors and vascular malformations (new issues) Adv Dermatol. 1997;13:375–423. [PubMed] [Google Scholar]
- 12.New York, NY: Cambridge University Press; 2007. Introduction: ISSVA classification; pp. 1–11. [Google Scholar]
- 13.Kaya B, Işılgan S E, Cerkez C, Otrakçı V, Serel S. Intraosseous cavernous hemangioma: a rare presentation in maxilla. Eplasty. 2014;14:e35. [PMC free article] [PubMed] [Google Scholar]
- 14.Park B H, Hwang E, Kim C H. Primary intraosseous hemangioma in the frontal bone. Arch Plast Surg. 2013;40(03):283–285. doi: 10.5999/aps.2013.40.3.283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Aykan A, Keleş M K, Bayram Y et al. Hemangioma of the zygomatic bone. J Craniofac Surg. 2016;27(02):e200–e202. doi: 10.1097/SCS.0000000000002457. [DOI] [PubMed] [Google Scholar]
- 16.Liu J K, Burger P C, Harnsberger H R, Couldwell W T. Primary intraosseous skull base cavernous hemangioma. Skull Base. 2003;13(04):219–228. doi: 10.1055/s-2004-817698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cheng N C, Lai D M, Hsie M H, Liao S L, Chen Y B. Intraosseous hemangiomas of the facial bone. Plast Reconstr Surg. 2006;117(07):2366–2372. doi: 10.1097/01.prs.0000218818.16811.9b. [DOI] [PubMed] [Google Scholar]
- 18.Warman S, Myssiorek D.Hemangioma of the zygomatic bone Ann Otol Rhinol Laryngol 198998(8, Pt 1):655–658. [DOI] [PubMed] [Google Scholar]
- 19.Razek A A. Imaging appearance of bone tumors of the maxillofacial region. World J Radiol. 2011;3(05):125–134. doi: 10.4329/wjr.v3.i5.125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gonçalves F G, Rojas J P, Hanagandi P B et al. Case report: periorbital intraosseous hemangiomas. Indian J Radiol Imaging. 2011;21(04):287–290. doi: 10.4103/0971-3026.90691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ramchandani P L, Sabesan T, Mellor T K. Intraosseous vascular anomaly (haemangioma) of the zygoma. Br J Oral Maxillofac Surg. 2004;42(06):583–586. doi: 10.1016/j.bjoms.2004.06.016. [DOI] [PubMed] [Google Scholar]
- 22.Firooznia H, Golimbu C, Rafii M, Rauchning W, Weinreb J. St. Louis, MO: Mosby; 1992. MRI and CT of the musculoskeletal system; p. 63. [Google Scholar]
- 23.Dogan S, Kocaeli H, Sahin S, Korfali E, Saraydaroglu O. Large cavernous hemangioma of the frontal bone. Neurol Med Chir (Tokyo) 2005;45(05):264–267. doi: 10.2176/nmc.45.264. [DOI] [PubMed] [Google Scholar]
- 24.Top H, Aygit C, Sarikaya A, Karaman D, Firat M F. Evaluation of maxillary sinus after treatment of midfacial fractures. J Oral Maxillofac Surg. 2004;62(10):1229–1236. doi: 10.1016/j.joms.2003.12.034. [DOI] [PubMed] [Google Scholar]
- 25.Marshak G. Hemangioma of the zygomatic bone. Arch Otolaryngol. 1980;106(09):581–582. doi: 10.1001/archotol.1980.00790330061017. [DOI] [PubMed] [Google Scholar]
- 26.Clauser L, Meneghini F, Riga M, Rigo L. Haemangioma of the zygoma. Report of two cases with a review of the literature. J Craniomaxillofac Surg. 1991;19(08):353–358. doi: 10.1016/s1010-5182(05)80278-1. [DOI] [PubMed] [Google Scholar]
- 27.Konior R J, Kelley T F, Hemmer D. Intraosseus zygomatic hemangioma. Otolaryngol Head Neck Surg. 1999;121(01):122–125. doi: 10.1016/s0194-5998(99)70138-5. [DOI] [PubMed] [Google Scholar]
- 28.Ethunandan M, Mellor T K. Haemangiomas and vascular malformations of the maxillofacial region--a review. Br J Oral Maxillofac Surg. 2006;44(04):263–272. doi: 10.1016/j.bjoms.2005.06.032. [DOI] [PubMed] [Google Scholar]