Abstract
Viruses enter host cells via several mechanisms, including endocytosis, macropinocytosis, and phagocytosis. They can also fuse at the plasma membrane and can spread within the host via cell-to-cell fusion or syncytia. The mechanism used by a given viral strain depends on its external topology and proteome and the type of cell being entered. This comparative review discusses the cellular attachment receptors and entry pathways of dsDNA viruses belonging to the families Adenoviridae, Baculoviridae, Herpesviridae and nucleocytoplasmic large DNA viruses (NCLDVs) belonging to the families Ascoviridae, Asfarviridae, Iridoviridae, Phycodnaviridae, and Poxviridae, and giant viruses belonging to the families Mimiviridae and Marseilleviridae as well as the proposed families Pandoraviridae and Pithoviridae. Although these viruses have several common features (e.g., topology, replication and protein sequence similarities) they utilize different entry pathways to infect wide-range of hosts, including humans, other mammals, invertebrates, fish, protozoa and algae. Similarities and differences between the entry methods used by these virus families are highlighted, with particular emphasis on viral topology and proteins that mediate viral attachment and entry. Cell types that are frequently used to study viral entry are also reviewed, along with other factors that affect virus-host cell interactions.
Introduction
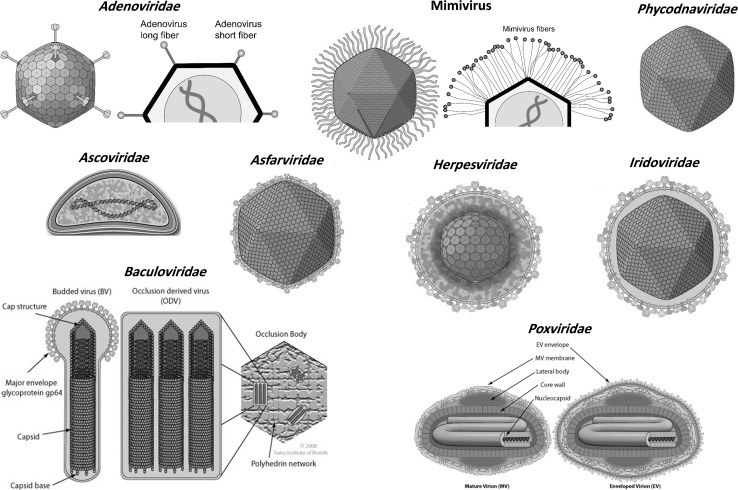
Viruses utilize several mechanisms to enter host cells. This review focuses on the relationships between the external topology of the virions and their entry mechanisms in different cell types, as well as the roles of cellular receptors and viral attachment factors. Ten viral families are discussed, including Adenoviridae, Baculoviridae, Herpesviridae, and nucleocytoplasmic large DNA viruses (NCLDVs). The NCLDVs include large and giant viruses characterized by their large virions and genomes, and can be classified into several distinct families: Ascoviridae, Asfarviridae, Iridoviridae, Mimiviridae, Marseilleviridae, Phycodnaviridae and Poxviridae. They also include members of the proposed families Pandoraviridae and Pithoviridae as well as the recently isolated molivirus and faustovirus [1–4]. They replicate completely or partially in the cytoplasm and are larger than other viruses. They may also have several common traits, including similarities in their protein sequences and topological features. Figure 1 shows the external topology of each viral family. They might be evolutionary related and share a common ancestor [5, 6]. It has been proposed that the NCLDVs be classified into one order, named “Megavirales” [7], whereas, herpesviruses belong to the order Herpesvirales. Generally, mimiviruses and phycodnaviruses are closely related to pandoraviruses and moliviruses, whereas pithoviruses are related to marseilleviruses, iridoviruses and ascoviruses, and faustovirus are closely related to asfarviruses, [1–4, 8, 9].
Fig. 1.
The different virion topologies of the 12 dsDNA large and giant virus families. Image adapted from ViralZone (http://viralzone.expasy.org/) [10]. Schematic representation of the different shapes of adenovirus and mimivirus fibers
Virus attachment and receptors
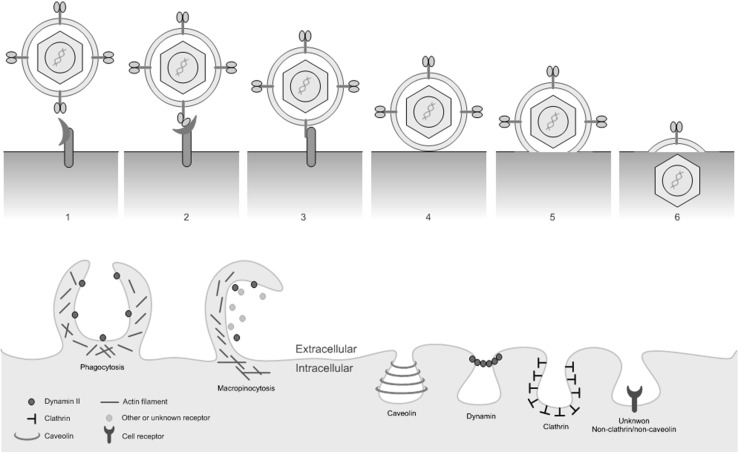
Viruses attach to proteins known as cellular receptors or attachment factors on the surface of the host cell [11, 12]. In addition, certain membrane lipids and glycans may be necessary for viral entry. These factors stabilize the virus on the cell surface and allow it to circumvent the cell’s barriers to entry. High-affinity interactions between viral proteins and cellular receptors drive conformational changes in the proteins’ structures that activate signaling cascades and destabilize the plasma membrane, leading to pore formation and internalization of the virus as shown in Figure 2a [13]. These interactions can be initiated by specific motifs or domains in both viral and host proteins. Notable viral protein motifs that facilitate entry by binding to cellular counterparts include the integrin-binding (RGD), endocytosis (PPxY and Yxx[FILV]), and clathrin endocytosis (PWxxW) motifs, where “x” denotes any residue [14]. It is worth noting that a receptor could be accompanied by an additional co-receptor that triggers a particular entry pathway or stabilizes the virus at plasma membrane.
Fig. 2.
Schematic representation of viral attachment and fusion (upper panel) and entry mechanisms (lower panel)
General mechanisms of virus entry
Cells can internalize viruses by endocytosis, as reviewed elsewhere [11–13, 15–17] and depicted in Figure 2. Alternatively, the virus may fuse with the cell membrane. Several factors determine which entry mechanism will be active, including the cell type and the cellular receptors it displays. Aspects of the virus’ external topology, such as the presence of surface protrusions or glycoproteins, may also affect the entry process. Viruses enter host cells via one of three major pathways:
(A) Fusion: Viral proteins promote the fusion of the virion with the plasma membrane, which then form a pore, and the virion becomes uncoated. Its genomic cargo is then transferred into the cytoplasm [12, 13, 18–21]. The proteins involved in fusion, so-called fusogens, can be divided into three classes: (i) class I fusogens, which are dominated by α-helical coils; (ii) class II fusogens, which consist predominantly of β-sheets; and (iii) class III fusogens, which feature both secondary structure types.
(B) Cell-cell fusion: Some viruses such as vaccinia virus (VV) and herpes simplex virus (HSV) induce the expression of proteins on the surfaces of infected cells that attract uninfected cells and cause them to fuse with the infected cell at low pH values to form a multinuclear cell known as a syncytium [11, 13, 22, 23]. Syncytium formation represents a very efficient way for a virus to spread within a host: it circumvents the immune response and creates a good site of replication for a nuclear-replicating virus. It should be noted that syncytium formation is not always regarded as an entry mechanism per se.
(C) Endocytosis: Once the cell internalizes the virus, it is then delivered to an acidic pit, a so-called early endosome. The virus then may be transferred into a late endosome and then to a lysosome. Alternatively, due to the low pH value in the lumen of endosomes, the viral membrane can fuse with the endosomal membrane, releasing the viral genome into the cytoplasm [12]. After exiting from endosomes, some adenoviruses or poxviruses may use microtubules for transport within the cytoplasm. Once in cytoplasm, some viruses move toward the nucleus to deliver their cargo inside the nucleus, whereas the NCLDVs usually remain in cytoplasm to initiate their replication cycle. Dynamin GTPase may have a key role in regulating most endocytic pathways. During virus entry, dynamin is deposited in the neck of the endocytic pit toward the cytoplasm leading to the excision of the pit [24, 25]. There are several major endocytosis-based pathways that viruses can use to enter cells and evade the host’s immune system. These pathways differ in terms of the types of particles involved and the molecules that are important in the process. The most important viral entry pathways are as follows:
Phagocytosis (cell eating), which occurs in specialized mammalian cells (so-called professional phagocytes, e.g., dendritic cells and macrophages) that engulf large and essential particles. Viral entry by this pathway typically involves the formation of large extracellular projections, and the internalized virus is taken into a phagosome. Actin and RhoA are typically necessary for this process.
Pinocytosis (cell drinking), which is the process by which cells take up solutes and fluids. Pinocytotic processes can be further classified based on the membrane structures and types of molecules they are associated with. Macropinocytosis is a nonspecific process, and particles internalized by this route may not be essential for the cell. When it is exploited by viruses, interactions between viral proteins and cell receptors activate intracellular signaling and actin rearrangements that form ruffles or filopodia on the external surface of the host cell. The ruffles then close up to form a vesicle known as a macropinosome, which carries the virus into the cytosol. Actin, Rho GTPases (Rac and Cdc42), PI3K, and Na+/H+ exchange are usually required for this pathway, and kinases are required to regulate macropinosome formation and closure. Although dynamin might not be required for some viruses to enter via macropinocytosis, some strains of adenoviruses and poxviruses require dynamin to enter the cell.
Clathrin-mediated endocytosis, which is the process by which the cell internalizes the virus in a clathrin-rich flask-shaped invagination/cavity (vesicle) known as a clathrin-coated pit. The virus is then delivered into the cytoplasm via endosomes. Clathrin and cholesterol are required, and dynamin and transferrin are usually involved in pit formation.
Caveolar/raft endocytosis, which is similar to clathrin-mediated endocytosis but involves pits containing caveolin-1 rather than clathrin. The internalized virus is delivered to the cytoplasm in cave-like bodies known as caveolae or caveosomes, whose internal pH is neutral.
Endocytosis based on other routes. These pathways involve vesicles that contain neither clathrin nor caveolin. However, like the clathrin- and caveolin-based pathways, they generally require dynamin, cholesterol and/or lipids. Interestingly, lymphocytic choriomeningitis virus uses a dynamin-, clathrin-, and caveolin-independent route that is also independent of actin, lipid rafts, and the pH [26, 27].
Mechanisms of attachment and entry utilized by large and giant DNA viruses
Members of all ten viral families covered in the review infect a wide range of potential hosts, including humans, other mammals, invertebrates, fish, protozoa, and algae, causing serious problems in public health, livestock farming, and aquaculture (Table 1). As suggested by this diversity of potential hosts, they can use many different mechanisms to enter host cells, and members of the same viral family may use very different mechanisms to enter a given host cell type. To ensure an efficient virus infection, a virus may utilize more than one mechanism to enter a given host cell.
Table 1.
Entry mechanisms utilized by large and giant DNA viruses. I, linear dsDNA; O, circular dsDNA; N, nuclear replication; M, cytoplasmic replication; E, enveloped; D, non-enveloped; S, icosahedral virus
| Features/replication | Genus or subgroup | Host | Topology | Entry |
|---|---|---|---|---|
| Adenoviridae: N; I; S; E; ~70–90 nm | Mastadenovirus | Mammals | S; D; contains long or short fibers | Endocytosis or macropinocytosis |
| Aviadenovirus | Birds | |||
| Atadenovirus | Birds, ruminants, squamata, marsupial | |||
| Siadenovirus | Frog, birds, turtle | |||
| Ichtadenovirus | Fish | |||
| Ascoviridae: N; O; 130 diameter × 200–400 nm length |
Diadromus spp., Heliothis spp, Spodoptera spp. Trichoplusia spp. |
Insects | E; no protrusions | - |
| Asfarviridae: M and N; I; E; 175–215 nm | African swine fever virus | Swine | E; short protrusions | Endocytosis or macropinocytosis |
| Baculoviridae: E; N; O; E; the nucleocapsid is ~21 × 260 nm | Alphabaculovirus | Lepidopteran | E; gp64 at surface | Fusion or endocytosis |
| Betabaculovirus | Lepidopteran-specific | |||
| Gammabaculovirus | Hymenopteran-specific | |||
| Deltabaculovirus | Culex nigripalpus | |||
| Herpesviridae: N; I; E; 150–200 nm | Alphaherpesvirinae (5 Genera) | Human or vertebrates (mammals, birds, fish, reptiles, and amphibians) | S; E; short protrusions (short envelope protein and phage-like tail) | Fusion, endocytosis or macropinocytosis |
| Betaherpesvirinae (4 Genera) | ||||
| Gammaherpesvirinae (4 Genera) | ||||
| Ictalurivirus | Fish | |||
| Iridoviridae: M; I; E and D; 120–350 nm | Ranavirus | Amphibians, reptiles | S; E and D; short surface protein | Fusion or endocytosis |
| Megalocytivirus | Fish | |||
| Lymphocystivirus | Fish | |||
| Iridovirus | Crustaceans, insects | |||
| Chloriridovirus | Mosquitos | |||
| Mimiviridae / Marseilleviridae: M; O / I; D; 200–600 nm | Mimivirus, Mamavirus, Megavirus, Moumouvirus, etc. | Mostly Protozoa; many viruses are isolated from environmental samples and the original host is unknown. | S; D; Long fibers, Marseilleviruses usually harbor short or no fibers | Phagocytosis-like |
| Marseillevirus, Lausannevirus, etc. | ||||
| Phycodnaviridae: N; I; E; 100–220 nm | Chlorovirus, Prasinovirus, Prymnesiovirus and Phaeovirus | Marine protozoa and Algae | S; E; no fiber | Cell wall degradation or fusion |
| Poxviridae: M; I; E; 220–450 nm long and 140–260 nm wide | Orthopoxvirus | Human, primates, camels, rodent | E; short surface proteins | Fusion or macropinocytosis |
| Leporipoxvirus | Rabbit | |||
| Squirrelpox virus species | Squirrel | |||
| Crocodylidpoxvirus | Nile crocodile | |||
| Molluscipoxvirus | Immunosuppressed human | |||
| Parapoxvirus | Superorder Laurasiatheria | |||
| Yatapoxvirus | Primate | |||
| Suipoxvirus | Swine | |||
| Cervidpoxvirus | Deer |
Adenoviridae
Adenoviruses (Ad) are non-enveloped icosahedral viruses with diameters of 70-90 nm (Fig. 1) that can be divided into seven groups and 50+ serotypes. They harbor 30 to 40-kb linear dsDNA genomes encoding around 45 proteins, and they replicate in the nucleus. Their genomes encode fiber proteins with a conserved N-terminal tail, a shaft, and a globular knob domain. The lengths of these fibers are similar within a serotype, but Ad-F and Ad-G encode two fiber proteins: short and long [28, 29]. The fibers bind to a wide range of cell receptors [30]; upon binding at the plasma membrane, the fibers become detached from the viral core and remain at the surface, while the core enters the cell [30–32]. The coxsackie-adenovirus receptor (CAR) is a functional receptor for most Ad strains [33]; it is expressed in the tight junctions in the epithelial cells of some human tissues (brain, heart and pancreas) and various tumor cells, but not in mice or primates [34, 35] (Table 2). The long viral fibers are flexible enough to permit the fiber knob to interact with CAR, bringing the penton base of the viral capsid into contact with integrins in the host cell membrane. Other cellular receptors targeted by adenoviruses include CD46, CD80, CD86, desmoglein-2, heparan sulphate, sialic acid, major histocompatibility complex-1-α2, and vascular cell adhesion molecule-1. Ad-2, Ad-5 and egg drop syndrome virus enter host cells via clathrin-mediated endocytosis [36–38], whereas Ad-3, Ad-5 and Ad-35 enter via macropinocytosis [37, 39]. Longer lists of cellular receptors and entry pathways exploited by adenoviruses are given in Tables 2 and 3.
Table 2.
Attachment cellular receptors used by adenoviruses
| Cellular receptor | Adenovirus strains |
|---|---|
| CAR | Ad-12, 31, 2, 5, 9, 19a, 19p, 4 and 41; but not Ad-3, 7, 21, 11, 14, 35 nor 30; due to the structure conformation of the fiber protein [34, 40–42] |
| CD46 | Ad-16, 21, 50, 11, 14, 34, 35, 19a and 37; but not Ad-3 or 7 [40–46] |
| CD80 & 86 | Ad-3 and 7 [47] |
| DSG2 | Ad-3, 7, 11 and 14 (only human DSG, but not mouse homolog) [48] |
| HSPG | Ad-2 and 5; but not Ad-35 [49] |
| Integrins | Ad-3, 35, 2, 5 and D60 through YGD motif instead of RGD [50] |
| MHC1-α2 | Ad-5 utilizes α2 domain of MHC-I (MHC-I-α2) [51] |
| Sialic acid | Ad-8, 19a and 37; but not Ad-9 or 19p [52] |
| VCAM-1 | Ad-5 [53] |
| GD1a glycan | Ad-8, 19a and 37; but not Ad-5, 9 or 19p [54] |
Table 3.
Entry mechanism and/or cellular receptors used by viruses. The cell types used in entry assay are mentioned whenever possible; otherwise, multiple cells might be used. “∞” means “interacts with”
| Virus | Cells | Entry method and/or attachment receptors |
|---|---|---|
| Adenoviruses | ||
| Ad-2/5 | – | Clathrin, myeloid, and αvβ3- and αvβ5-integrins-mediated endocytosis [36, 90] |
| Ad-2 | – | Macropinocytosis [90] |
| Ad-5 | Afferent lymph DCs | Actin-dependent macropinocytosis [39] |
| Ad-3/35 | EpC and haematopoietic | PI3K, Rho GTPases and dynamin-dependent macropinocytosis [37, 91] |
| Egg drop syndrome virus | Duck embryonic FbCs | Low pH, clathrin-mediated endocytosis [38] |
| Herpesviruses | ||
| HSV-1 | HeLa, CHO and keratinocytes, but not neuroblastoma | Low-pH endocytosis [92–94] |
| Vero cells | Fusion [92] | |
| CHO | Viral gB and gD, and cellular Nectin-1, HVEM and PILR-α are required for infection; gD ∞ Nectin-1 and gB ∞ PILR-α [95]; gD ∞ Nectin-1 and gB ∞ PILR-α [96–99] | |
| EpC, neuron and keratinocytes | gH/gL (RGD motif) ∞ αvβ6- and αvβ8-integrins [100]; gH/gL binds to αvβ3-integrin activating IFN-I and NF-κB [101] | |
| CHO, HeLa, Vero | gD ∞ HVEM [102, 103] | |
| HeLa | Syndecan-1 and syndecan-2 [104] | |
| Nectin-1 or HVEM-deficient murine dermal FbCs | Delayed virus entry; HS could be an alternative receptorl; dynamin and cholesterol could be involved [105] | |
| Murine cornea | HVEM and nectin-1 are crucial for infection [106] | |
| Human oligodendrocytic cells | Proteolipid protein is required in entry [107] | |
| – | gD triggers fusion by forming complexes with gB or gH/gL [108]; gB ∞ non-muscle myosin heavy chain IIA [109] | |
| CHO and fibroblasts | gC, gB and gD are required for entry [110]; gD ∞ 3-O-sulfated HS [111] | |
| HSV-2 | Retinal EpCs | Nectin-1, HVEM and PILR-α [95]; gD ∞ Nectin-1 and PILR-α and gB ∞ PILR-α [96–99] |
| HSV-6 | – | gH/gL/gQ ∞ CD46 [112–114]; gB and the gH/gL/gQ complex are required for cell-cell fusion [115] |
| HSV-7 | CHO | gB ∞ HS [116] |
| CMV | Fibroblast, EnC and retinal EpC | Fusion or endocytosis [78, 117] |
| Multiple cells, e.g. CHO, myeloid, EpC, EnC and FbC | gB ∞ epidermal growth factor receptor [118] or integrins (does not depend on RGD motif) [119]; gH ∞ αvβ3 integrin as a co-receptor [120]; gB or gH/gL are required for syncytium [121, 122]. gH/gL/UL128/130/131 and gH/gL/gO complexes are essential for fusion [123] | |
| EBV | B lymphocytes | Endocytosis [124, 125]; gp350/220 ∞ complement receptor 2 (CR2, CD21) [126, 127]. gH/gL (KGD motif) ∞ αvβ6- and αvβ8-integrins [128, 79]; gp42 ∞ HLA to induce membrane fusion through gH/gL and gB [, 80, 81, 110, 126]. |
| EpCs | Fusion [125]; macropinocytosis and lipid raft-dependent endocytosis [82] | |
| B cells, but not EpC | gp42/gH/gL complex mediates fusion [83] | |
| Nasopharyngeal EpC | gB ∞ Neuropilin-1 [82] | |
| Polarized cells | BMRF2 protein ∞ integrins [84] | |
| KSHV (HHV-8) | EnC and FbC | DC-SIGN, pH and clathrin mediated endocytosis [85–87] |
| Endothelial cells | Macropinocytosis [88] | |
| Monocytic THP-1 cells | Endocytosis; clathrin, caveolin, HS, DC-SIGN, integrins, NF-κB, Src, and PI3K signaling are involved [89]. | |
| Human dermal microvascular EnC | gB ∞ ESCRT-0 component Hrs (hepatocyte growth factor-regulated tyrosine kinase substrate) promoting macropinocytosis [129] | |
| – | gB (RGD motif) ∞ integrins [130, 57]. gB, gH/gL and K8.1 ∞ HSPG induces fusion [58, 59, 60]. | |
| VZV | B cells | Endocytosis [61] |
| VZV-permissive human melanoma cells expressing integrins | gB and gH-gL ∞ αV integrins [62] | |
| Ovine herpesvirus 2 | – | gB and gH/gL induce cell-cell fusion [131] |
| Poxviruses | ||
| VV MV / EV | HeLa | Low-pH, dynamin, actin, and cholesterol-dependent macropinocytosis [132–137] |
| VV MV | HeLa cells | Bind to CD98 and enters via endocytosis [138] |
| VV MV / EV | DCs | Dynamin and pH-independent macropinocytosis [139], cholesterol (lipid raft), PS, actin, kinases, GTPases, integrins and Na+/H+ exchangers are required [134, 140, 141]. |
| VV-MV | HeLa or A549 | Low-pH, and serine/threonine kinase PAK1 and tyrosine kinase [142]. |
| VV | Human pancreatic carcinoma cell lines | Entry enhanced by vascular endothelial growth factor A and Akt signaling pathway [143]. |
| VV | Leukocytes | Attach to heparin and laminin [144, 145] |
| VV | Fibroblast or HeLa | Tumor necrosis factor receptor associated factor 2 [146] |
| VV | Drosophila DL1 cells | Macropinocytosis [147] |
| VV | Drosophila S2 cells | Low-pH endocytic pathway that requires EFC proteins [148] |
| Myxoma virus | Leukocytes | Attach to heparin [144] |
| VV and myxoma virus | FbCs BSC-40 | Inhibition of HS affects entry, but laminin blocks binding of VV [144]. |
| WR and IHD-J | HeLa | PS, kinases and actin macropinocytosis; IHD-J MV induces filopodia; WR utilizes tyrosine kinase, PI3K and Rac1 to activate blebs [136]. |
| HeLa, B78H1 and L cells | Inhibited by soluble heparin [149, 150] | |
| B78H1 and BSC-1 | Require endosomal acidification [149, 150] | |
| WR, monkeypox virus and cowpox virus | – | Low-pH [150, 151] |
| IHD-J, Copenhagen and Elstree strains | – | A pH-independent fusion [150, 151] |
| WR EV | – | Gas6 protein enhances entry by bridging viral PS to TAM (Tyro3/Axl/Mer) receptor tyrosine kinases [152]. |
| EVs | – | Expression of A33 and A36 at plasma membrane of the infected cells mediates the repulsion between EVs toward uninfected cells leading to rapid spread of virus [153]. A56 (hemagglutinin) interact with K2 (serine proteinase inhibitors) forming A56-K2 complex that co-localizes at the cell surface blocking the superinfection and fusion [154–157]. A56-K2 complex interacts with A16 and G9 subunits and prevents the superinfection [158]. |
| Iridoviruses | ||
| Tiger frog virus, Ranavirus genus | HepG2 cells | pH, cholesterol, dynamin, actin and caveolin-mediated endocytosis [159] |
| Frog virus 3, Ranavirus genus | BHK-21 cells | Low pH and clathrin-mediated endocytosis [160] |
| ISKNV, Megalocytivirus | Mandarin fish fry cells | Major capsid protein ∞ caveolin-1 and induces caveolin-endocytosis [161, 162] |
| SGIV | Grouper spleen cell line | pH-dependent clathrin-endocytosis and macropinocytosis [163]; the deletion of VP088 envelope protein inhibits viral entry [164]. |
| Large yellow croaker iridovirus | Bluegill fry (BF-2) cells | 037L (RGD motif) ∞ integrins inducing fusion [165, 166] |
Herpesviridae (order Herpesvirales)
Herpesviruses (HVs) have an enveloped icosahedral virion (150-200 nm) containing a 120 to 240-kb linear dsDNA genome encoding 100-200 proteins (see Figure 1 and Table 1). They replicate in the nucleus. The >70 known members of this family include eight human pathogens: HSV-1, HSV-2, CMV, EBV, KSHV, VZV, HHV-6 and HHV-7. HVs are rich in glycoproteins (GPs) that can form heterodimeric complexes to facilitate attachment and entry [55, 56]. Several proteins are involved in their attachment, including viral GPs (gB, gC, gD, gH/gL, and the gH/gL/gO complex) and host cell proteins such as HVEM, integrins, heparan sulphate, syndecan, and neuropilin [57–62]. HVEM was the first recognized receptor for HSV-1/2 gD (see Table 3). HV has a bacteriophage-like short tail whose role in entry is currently unknown [63]. Interestingly, an analysis of cytomegalovirus (CMV) showed that the genomes of clinical samples contain at least 19 genes that are absent in laboratory-acclimated strains [64]. Three of these missing proteins, UL128, UL130 and UL131, contribute to viral entry by binding to gH/gL [64–69]. HVs generally enter host cells by endocytosis or fusion with the plasma membrane [149, 71–77]. HSV-1, CMV, EBV, KSHV and VZV enter via endocytosis [78, 61, 79–87]. KSHV has been observed to enter endothelial cells by pinocytosis [88] but enters monocytes via some other mechanism that may involve heparan sulphate, integrins, and the induction of Src and PI3 K signaling [89]. Details on the entry mechanisms of HVs and receptors mediating their attachment and entry can be found in Table 3.
Baculoviridae
Baculoviruses are arthropod-specific enveloped virus with nucleocapsid dimensions of 21 × 260 nm (Fig. 1). They have circular dsDNA genomes of 80-180 kb that encode 100-180 proteins and replicate in the nucleus. They are used in biocontrol against insects, and as vectors for gene transfer and protein expression. Consequently, their entry into insect, human, and cancer cells has an increasing biological impact (see Tables 1 and 3). Two baculovirus phenotypes have been characterized: budded and occlusion-derived. Viruses of this family express two crucial fusogens, gp64 (class III) and F (class I), which are functionally analogous and can both trigger low-pH membrane fusion during endocytosis. There are evidences that gp64 facilitate virus entry and fusion with the plasma membrane [167–170]. Bombyx mori nucleopolyhedrovirus (BmNPV) enters Bombyx mori (BmN) cells via cholesterol-dependent macropinocytosis [171], while Autographa californica multiple nucleopolyhedrovirus (AcMNPV) grown in Spodoptera frugiperda (sf9) cells enters human hepatocarcinoma (HepG2) and embryonic kidney (293) cell lines via a dynamin-, raft- and RhoA-dependent phagocytosis-like mechanism [172], but clathrin-mediated endocytosis or macropinocytosis may not be involved in the virus uptake. However, recombinant AcMNPV from sf21 cells enters BHK-21 cells via low-pH clathrin-mediated endocytosis [173]. Additionally, a pseudotyped vesicular stomatitis virus (VSV) encoding gp64 grown in Sf9 cells enters the Huh7 and 293 cells via macropinocytosis and endocytosis, which is mediated by viral gp64, and cellular cholesterol, dynamin and clathrin [169]. This process also requires the host cell proteins HSPG and syndecan-1 [174], as well as cholesterol [169, 175].
Poxviridae
Poxviruses are widely distributed enveloped viruses (∼360 × 270 × 250 nm) that replicate in the cytoplasm (Fig. 1) [176]. They harbor a 130 to 375-kb linear genome that encodes ~200 proteins. Vaccinia virus (VV) is a prototypic virus of this class that was used as a smallpox vaccine. It exists in three forms [177, 178]. The first is the mature virion (MVs, also known as the intracellular mature virus, IMV or INV), which has a brick-shaped structure; it is the most abundant, stable and simple form and is active in host-host transmission. The second form is the wrapped virion (WV or intracellular enveloped virus, IEV), which contains an MV core wrapped in two membranes. WVs travel to the cell periphery via microtubules and fuse with the plasma membrane, and they are then released by exocytosis as the third form, the extracellular virion (EV, or cell-associated extracellular enveloped virus, CEV, or extracellular enveloped virus, EEV), which is specialized for exiting and cell-to-cell transmission within the host.
Four proteins are used for attachment to the cell surface (A26, A27, D8 and H3), and the MV displays the so-called entry-fusion complex (EFC), which consists of 11 proteins (A16L, A21L, A28L, F9, G3L, G9R, H2, J5, L1R, L5R and O3L). These proteins interact with one another and mediate virus-cell fusion, membrane disruption, and cell-to-cell fusion [176, 179, 180] (Tables 3 and 4). Inhibition of any of these proteins destabilizes the complex and hence perturbs viral entry. MV enters host cells via endocytosis or fusion with the plasma membrane, leaving the virus in endosomes [179–184] (see Table 3). Notably, the mechanisms of fusion for MVs and EVs at the plasma membrane and endosome are identical, and both require EFC proteins. VV (MV/EV), WR, and IHD-J enter HeLa cells via macropinocytosis [132, 134–139] and have also been suggested to enter via a parallel endocytotic mechanism [138]. In Drosophila, VV enters DL1 cells by macropinocytosis [147], but it enters S2 cells via endocytosis [148].
Table 4.
Poxviruses entry proteins, cellular receptors and functions. 1, N-terminal, 2, C-terminal transmembrane domain
| Protein | Roles |
|---|---|
| Attachment | |
| A26 | Binds to laminin [185]; A25 and A26 may act as fusion suppressors [180, 186]. |
| A27 | Binds to heparan sulfate, but not chondroitin [187]; binds with A17 protein forming a complex that mediates pH-dependent cell-to-cell fusion and syncytium formation [188]. |
| D8 | Binds to chondroitin sulfate and mediates the adsorption of MV [189] |
| H3 | Binds to heparan sulfate [190] |
| Entry (entry-fusion complex, EFC) | |
| A16L | 2; interacts with G9 and with A56/K2 to prevent superinfection; A16-deficient virion fails to induce syncytia [191]. |
| A21L | 1; interacts with H2; [192] |
| A28L | 1; interacts with H2 and both are required for entry and cell-cell fusion [177, 179, 193–195]. |
| F9 | 2; important for entry; F9-deficient virus binds to the cell, but the core fails to penetrate into the inside [177, 196]. |
| G3L | 1 [197] |
| G9R | 2; binds to A16 and A26 suppressing fusion [198, 199]. |
| H2 | 1, binds to A28 and both are required for entry and cell-cell fusion [177, 179, 194, 195]. |
| J5 | 2 [200] |
| L1R | 2; binds with uninfected cell receptors; L1 mutant virus is lethal, as it is required in assembly and fusion [177, 196, 201] |
| L5R | 2 [202] |
| O3L | 1 [203] |
Giant viruses (Mimiviridae and Marseilleviridae)
These families comprise the largest known viruses, so-called giant viruses (GVs). They have genomes of ~0.5-2.5 Mb that encode 400-2500 proteins, and they replicate in the cytoplasm. Representatives of these families have been isolated from diverse habitats, including bronchoalveolar lavage fluid [204] and stools [205] from patients with pneumonia, insects [206], and leeches [207] (for a detailed review, see reference [208], [209]). The nature of the relationship between giant viruses and pneumonia remains to be elucidated [209–212]. Briefly, the giant viruses were detected by serological and genomic methods in patients with respiratory symptoms. Moreover, recent images show giant virus- and virus factory-like structures in number of human cells [213].
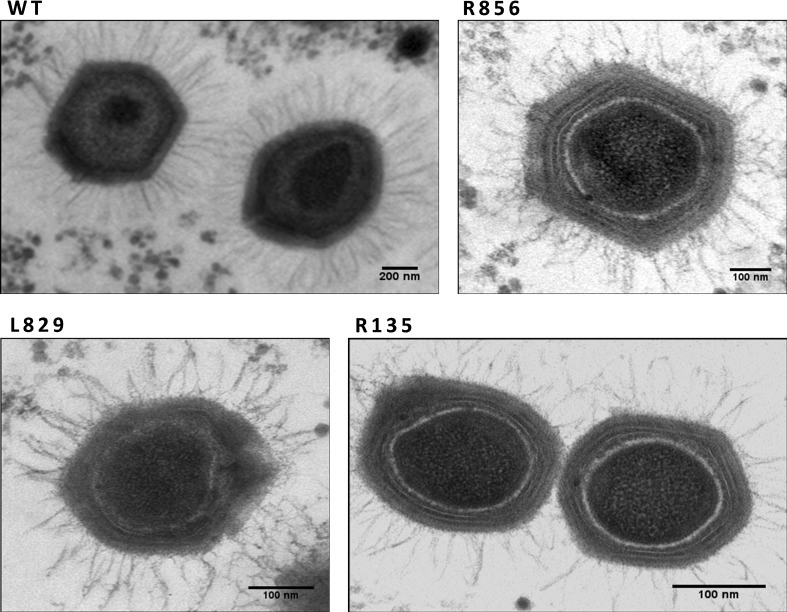
Mimivirus virions are 500 nm in diameter, with a 1 Mb dsDNA genome encoding 900 proteins. Their surfaces are completely covered with fibers (120 nm long) attached to the capsid via a disc-shaped feature except at one capsid vertex (Fig. 1). The outer fibers may play some role in the virus’ attachment to or entry into host cells [214, 215], but the details of its mechanisms of attachment and entry are unknown. Proteomic and gene silencing experiments revealed that the fibres consist of at least four proteins (R135, L725, L829, and R856); viruses in which any of these proteins are silenced exhibit short and deformed fibers [214, 216–219], as shown in Figure 3. Further structural analysis showed that R135 is a component of the fibers and is required for host cell entry [219]. In addition, a electron microscopy showed that L725 aggregates form fibre-like architectures [217]. The fibers’ shape differs from that in other viruses, and the fiber proteins exhibit no sequence similarity to proteins encoded by other viruses. It should be noted that some giant viruses lack external fibers – for instance, marseilleviruses (which are 200 nm in diameter with 350-kb circular dsDNA genomes) have topologies similar to those of mimiviruses but have only short (12 nm) or no fibers [216].
Fig. 3.
Silencing any one of the four fiber-associated proteins in mimivirus produces viruses bearing short and deformed fibers compared to the wild-type control (WT). The images are adapted from reference [216]
Mimiviruses enter amoebae or macrophages via a phagocytosis-like mechanism that depends on dynamin, actin and PI3-K [220, 221]. Unlike poxviruses, the entire virion with fiber can be seen inside the host. Further analyses showed that individual Marseillevirus virions enter A. castellanii cells via phagocytosis or in vesicles, endocytosis and micropinocytosis, were also suggested, but remain to be investigated [222]. Because the closely related Mimiviruses enter cells via phagocytosis, it seems very plausible that Marseillevirus could also enter via such a mechanism. It should be noted that the original host of most giant virus strains, including APMV, is not known; neither amoebae nor macrophages are their natural hosts. The tropism of these viruses and their interactions with their natural host cells thus remain to be elucidated.
Phycodnaviridae
The Phycodnaviridae are marine enveloped viruses with dimensions of 100-220 nm that have 330 to 560-kb linear dsDNA genomes and replicate in the cytoplasm of algae (Fig. 1). Despite having algal hosts, their entry pathways resemble those used by bacteriophages and animal viruses. Paramecium bursaria chlorella virus (PBCV-1) attaches to host cells via a viral vertex and degrades the host cell wall at the site of attachment like a bacteriophage [223]. To this end, it encodes chitinases, chitosanase, β -1,3-glucanase, and alginase enzymes that catalyze cell wall lysis [224]; it also encodes potassium ion channel proteins, which have a putative role in entry [225, 226]. After entry, PBCV leaves an empty shell at the cell surface. Another member of this family, Emiliania huxleyi virus 86, enters host cells via endocytosis or fusion of the outer lipid membrane surrounding the capsid, which is similar to animal virus entry [227]. The intact virion can be seen in the cytoplasm before the capsid breaks down to release the genome. Ectocarpus fasciculatus virus infects zoospores or gametes of brown algae that lack cell walls [228]. It fuses with the outer plasma membrane of the host cell, leaving the capsid outside the cell surface, and injects its genomic cargo into the cytoplasm.
Asfarviridae
These are enveloped viruses (175-215 nm, see Figure 1) with 170 to 190-kb linear dsDNA genomes encoding around 150 genes. They infect macrophages and monocytes of pigs and argasid ticks, and they replicate in the nucleus and/or cytoplasm. The early steps in the binding and entry of African swine fever virus (ASFV) into host cells are largely unknown [229]. The ASFV-E70 and Ba71V strains enter Vero cells and macrophages by low-pH-, dynamin-, and clathrin-dependent endocytosis, which requires actin, small GTPase Rab7 and PI3-K. Additionally, cholesterol may be needed to liberate the virus from endosomes into the cytoplasm [230–234]. There is also evidence that ASFV can enter via macropinocytosis, which requires actin, kinases and Na+/H+ exchange [235].
Iridoviridae
The iridoviruses include both enveloped and non-enveloped viruses with dimensions of 120-350 nm that replicate in the cytoplasm of insect and fish cells (Fig. 1). They harbor 100 to 200-kb linear dsDNA genomes with circularly permuted and redundant termini. The enveloped viruses fuse with the cell membrane of the host cell, whereas the non-enveloped viruses enter via endocytic pathways [236] (see Table 3). Frog virus 3, tiger frog virus, and infectious spleen and kidney necrosis virus enter BHK-21, HepG2 and Mandarin fish fry cells, respectively, by endocytosis [159–162]. The VP088 protein encoded by SGIV facilitates both endocytosis and macropinocytosis into a grouper spleen cell line [163, 164].
Ascoviridae
These viruses (~130 nm diameter, 200-400 nm in length) infect invertebrates; they replicate in the nucleus and harbor 150 to 190-kb circular dsDNA genomes that encode 180 proteins (Fig. 1). They are phylogenetically related to iridoviruses, and their entry mechanisms are obscure. However, Heliothis virescens ascovirus-3e infections are known to require actin rearrangement [237].
Conclusion and future perspectives
Viruses enter host cells via several mechanisms, depending on the host cell type and viral strain. Concerns about the risks of viral outbreaks have prompted efforts to characterize emerging pathogens and predict the emergence and properties of new viruses. A further motivating factor for such studies is the possibility of developing non-cytotoxic antiviral drugs that act outside host cells by preventing viral attachment or entry rather than disrupting viral replication inside cells. This review details the entry pathways exploited by large dsDNA viruses. Their entry pathways are affected by several factors, including the external topology of the virions (particularly the presence of surface protrusions and their topology), the targeted cell type, the cellular receptors that are present, and the viral protein content.
While viruses from the same viral family often have similar topologies and encode proteins with similar sequences and structures, they may still use different entry mechanisms. As mentioned in Table 3, the virus protein(s) may bind to one or more receptors and co-receptors (see herpesviruses for examples). The binding may activate number of factors (proteins/pathways) that are relevant to infection. These factors could be characteristics of other entry pathways (see, for example, entry of KSHV). Additionally, the MV form of vaccinia virus can enter cells by direct fusion with either the plasma membrane or the membrane of a vesicle after endocytosis.
It is worth emphasizing that additional factors could affect the entry mechanism. Among these factors is protein sequence similarity; some viral proteins exhibit functional and structural similarities despite having little or no sequence similarity. For example, the HSV-1 protein gB is a class III fusogen that resembles (especially in its post-fusion conformation) the gG protein of the RNA rhabdovirus VSV and the baculovirus protein gp64 [72, 238–241]. Additionally, the EBV protein gp42 is a functional homolog of HSV gD, but the two share no sequence similarity [110]. The functional motifs of viral proteins appear to play central roles in determining the entry pathways available to specific viruses, so their analysis could enable prediction of entry pathways and virus-host cell interactions [14, 242]. Closely related viruses that infect the same host generally have similar functional motif profiles [242]. Another factor that may be important is ubiquitination of viral proteins inside host cells, which can affect infection and microtubule trafficking. For instance, the adenovirus protein VI recruits Nedd4 E3 ubiquitin ligases via interactions involving its PPxY motif [14, 61, 243, 244]. Biophysical factors may also affect viral entry. For example, the entry of CMV into vascular endothelial cells is promoted by low levels of shear stress [245]. Similarly, the fusion of the enveloped HSV requires a negative curvature of the lipid bilayer and can thus be suppressed by factors that prevent the formation of such negative curvature [246].
Differences in observed entry pathways for different strains or different samples of the same viral strain may be due to differences in experimental design and conditions [61], the use of a non-physiological host in vitro (e.g., non-wild-type cells), or the use of a laboratory strain whose gene content differs from that of the wild-type virus, as in the case of CMV [64]. It is generally accepted that cell lines (i.e., immortalized cells) often differ genetically and phenotypically from cells in native tissues (or primary cells). Consequently, the type of cell used when studying viral entry may profoundly affect the results obtained. It has also been shown that baculoviruses grown in different insect cell types enter mammalian cells via different mechanisms [247]. These results clearly show that there are several aspects of viral entry into host cells that are very poorly understood. Comparative studies could potentially shed important light on this topic and help to clarify unknown aspects of virus-host cell interactions. In addition, more comprehensive information on viral topology and protein sequences will help to understand virus tropism. Further studies in this area should focus on predicting viral entry mechanisms and the evolution of interactions between host cells and viruses. Efforts should also be made to identify optimal experimental conditions for viral entry in different cell types and for different viral families.
Acknowledgements
I would like to thank professors Philippe Colson (Univ. Aix-Marseille), Bruno Pozzetto (Univ. Jean Monnet), and Bernard Moss (NIAID-NIH).
Abbreviations
- dsDNA
double-stranded DNA
- CHO
Chinese hamster ovary
- DC
dendritic cell
- EnC
endothelial cell
- EpC
epithelial cell
- FbC
fibroblast cell
- VV
vaccinia virus
- WR
VV Western Reserve
- IHD-J
International Health Department-J
- AcMNPV
Autographa californica multiple nucleopolyhedrovirus
- BmNPV
Bombyx mori nucleopolyhedrovirus
- ISKNV
infectious spleen and kidney necrosis virus
- SGIV
Singapore grouper iridovirus
- ASFV
African swine fever virus
- HHV
Human herpesvirus
- HSV
herpes simplex virus type 1 or 2 (HSV-1 or HSV-2, also known as HHV-1 and HHV-2, respectively)
- VZV
varicella-zoster virus (or HHV-3)
- EBV
Epstein-Barr virus (or HHV-4)
- CMV
cytomegalovirus or human CMV (HCMV or HHV-5)
- KSHV
Kaposi’s sarcoma-associated HV (HHV-8)
- VSV
vesicular stomatitis virus
- CAR
coxsackie-adenovirus receptor
- DSG2
desmoglein-2
- ESCRT
endosomal sorting complexes required for transport
- GAGs
glycosaminoglycan
- GD1a
disialogangliotetraosylceramide
- HLA
human leukocyte antigen
- HS
heparan sulphate
- HSPG
heparan sulphate proteoglycans
- HVEM
herpesvirus entry mediator
- IFN
interferon
- MHC
major histocompatibility complex
- PGs
proteoglycans
- PI3-K
phosphatidylinositol 3-kinase
- PILR-α
paired immunoglobulin-like receptor alpha
- PS
phosphatidylserine
- VCAM-1
vascular cell adhesion molecule 1
Author contribution
HS analysed the data and wrote the manuscript.
Compliance with ethical standards
Conflicts of interest
No known conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by the author.
Informed consent
Not applicable.
References
- 1.Philippe N, Legendre M, Doutre G, Coute Y, Poirot O, Lescot M, Arslan D, Seltzer V, Bertaux L, Bruley C, Garin J, Claverie JM, Abergel C. Pandoraviruses: amoeba viruses with genomes up to 2.5 Mb reaching that of parasitic eukaryotes. Science. 2013;341(6143):281–286. doi: 10.1126/science.1239181. [DOI] [PubMed] [Google Scholar]
- 2.Legendre M, Bartoli J, Shmakova L, Jeudy S, Labadie K, Adrait A, Lescot M, Poirot O, Bertaux L, Bruley C, Coute Y, Rivkina E, Abergel C, Claverie JM. Thirty-thousand-year-old distant relative of giant icosahedral DNA viruses with a pandoravirus morphology. Proc Natl Acad Sci USA. 2014;111(11):4274–4279. doi: 10.1073/pnas.1320670111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Legendre M, Lartigue A, Bertaux L, Jeudy S, Bartoli J, Lescot M, Alempic JM, Ramus C, Bruley C, Labadie K, Shmakova L, Rivkina E, Coute Y, Abergel C, Claverie JM. In-depth study of Mollivirus sibericum, a new 30,000-year-old giant virus infecting Acanthamoeba. Proc Natl Acad Sci USA. 2015;112(38):E5327–E5335. doi: 10.1073/pnas.1510795112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Reteno DG, Benamar S, Khalil JB, Andreani J, Armstrong N, Klose T, Rossmann M, Colson P, Raoult D, La Scola B. Faustovirus, an asfarvirus-related new lineage of giant viruses infecting amoebae. J Virol. 2015;89(13):6585–6594. doi: 10.1128/JVI.00115-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nasir A, Caetano-Anolles G. A phylogenomic data-driven exploration of viral origins and evolution. Sci Adv. 2015;1(8):e1500527. doi: 10.1126/sciadv.1500527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Aherfi S, Colson P, La Scola B, Raoult D. Giant viruses of amoebas: an update. Front Microbiol. 2016;7:349. doi: 10.3389/fmicb.2016.00349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Colson P, De Lamballerie X, Yutin N, Asgari S, Bigot Y, Bideshi DK, Cheng XW, Federici BA, Van Etten JL, Koonin EV, La Scola B, Raoult D. “Megavirales”, a proposed new order for eukaryotic nucleocytoplasmic large DNA viruses. Arch Virol. 2013;158(12):2517–2521. doi: 10.1007/s00705-013-1768-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yutin N, Koonin EV. Pandoraviruses are highly derived phycodnaviruses. Biol Direct. 2013;8:25. doi: 10.1186/1745-6150-8-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fischer MG, Allen MJ, Wilson WH, Suttle CA. Giant virus with a remarkable complement of genes infects marine zooplankton. Proc Natl Acad Sci USA. 2010;107(45):19508–19513. doi: 10.1073/pnas.1007615107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hulo C, de Castro E, Masson P, Bougueleret L, Bairoch A, Xenarios I, Le Mercier P. ViralZone: a knowledge resource to understand virus diversity. Nucleic Acids Res. 2011;39(Database issue):D576–D582. doi: 10.1093/nar/gkq901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Marsh M, Helenius A. Virus entry: open sesame. Cell. 2006;124(4):729–740. doi: 10.1016/j.cell.2006.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Grove J, Marsh M. The cell biology of receptor-mediated virus entry. J Cell Biol. 2011;195(7):1071–1082. doi: 10.1083/jcb.201108131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dimitrov DS. Virus entry: molecular mechanisms and biomedical applications. Nat Rev Microbiol. 2004;2(2):109–122. doi: 10.1038/nrmicro817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sobhy H. A review of functional motifs utilized by viruses. Proteomes. 2016;4(1):3. doi: 10.3390/proteomes4010003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Conner SD, Schmid SL. Regulated portals of entry into the cell. Nature. 2003;422(6927):37–44. doi: 10.1038/nature01451. [DOI] [PubMed] [Google Scholar]
- 16.Mercer J, Helenius A. Virus entry by macropinocytosis. Nat Cell Biol. 2009;11(5):510–520. doi: 10.1038/ncb0509-510. [DOI] [PubMed] [Google Scholar]
- 17.Vazquez-Calvo A, Saiz JC, McCullough KC, Sobrino F, Martin-Acebes MA. Acid-dependent viral entry. Virus Res. 2012;167(2):125–137. doi: 10.1016/j.virusres.2012.05.024. [DOI] [PubMed] [Google Scholar]
- 18.Kielian M, Rey FA. Virus membrane-fusion proteins: more than one way to make a hairpin. Nat Rev Microbiol. 2006;4(1):67–76. doi: 10.1038/nrmicro1326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Harrison SC. Viral membrane fusion. Nat Struct Mol Biol. 2008;15(7):690–698. doi: 10.1038/nsmb.1456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.White JM, Delos SE, Brecher M, Schornberg K. Structures and mechanisms of viral membrane fusion proteins: multiple variations on a common theme. Crit Rev Biochem Mol Biol. 2008;43(3):189–219. doi: 10.1080/10409230802058320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Backovic M, Jardetzky TS. Class III viral membrane fusion proteins. Curr Opin Struct Biol. 2009;19(2):189–196. doi: 10.1016/j.sbi.2009.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sattentau Q. Avoiding the void: cell-to-cell spread of human viruses. Nat Rev Microbiol. 2008;6(11):815–826. doi: 10.1038/nrmicro1972. [DOI] [PubMed] [Google Scholar]
- 23.Zhong P, Agosto LM, Munro JB, Mothes W. Cell-to-cell transmission of viruses. Curr Opin Virol. 2013;3(1):44–50. doi: 10.1016/j.coviro.2012.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ramachandran R. Vesicle scission: dynamin. Semin Cell Dev Biol. 2011;22(1):10–17. doi: 10.1016/j.semcdb.2010.09.001. [DOI] [PubMed] [Google Scholar]
- 25.Cocucci E, Gaudin R, Kirchhausen T. Dynamin recruitment and membrane scission at the neck of a clathrin-coated pit. Mol Biol Cell. 2014;25(22):3595–3609. doi: 10.1091/mbc.E14-07-1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rojek JM, Perez M, Kunz S. Cellular entry of lymphocytic choriomeningitis virus. J Virol. 2008;82(3):1505–1517. doi: 10.1128/JVI.01331-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Quirin K, Eschli B, Scheu I, Poort L, Kartenbeck J, Helenius A. Lymphocytic choriomeningitis virus uses a novel endocytic pathway for infectious entry via late endosomes. Virology. 2008;378(1):21–33. doi: 10.1016/j.virol.2008.04.046. [DOI] [PubMed] [Google Scholar]
- 28.Yeh HY, Pieniazek N, Pieniazek D, Gelderblom H, Luftig RB. Human adenovirus type 41 contains two fibers. Virus Res. 1994;33(2):179–198. doi: 10.1016/0168-1702(94)90054-X. [DOI] [PubMed] [Google Scholar]
- 29.Jones MS, 2nd, Harrach B, Ganac RD, Gozum MM, Dela Cruz WP, Riedel B, Pan C, Delwart EL, Schnurr DP. New adenovirus species found in a patient presenting with gastroenteritis. J Virol. 2007;81(11):5978–5984. doi: 10.1128/JVI.02650-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wolfrum N, Greber UF. Adenovirus signalling in entry. Cell Microbiol. 2013;15(1):53–62. doi: 10.1111/cmi.12053. [DOI] [PubMed] [Google Scholar]
- 31.Moyer CL, Wiethoff CM, Maier O, Smith JG, Nemerow GR. Functional genetic and biophysical analyses of membrane disruption by human adenovirus. J Virol. 2011;85(6):2631–2641. doi: 10.1128/JVI.02321-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Corjon S, Gonzalez G, Henning P, Grichine A, Lindholm L, Boulanger P, Fender P, Hong SS. Cell entry and trafficking of human adenovirus bound to blood factor X is determined by the fiber serotype and not hexon:heparan sulfate interaction. PLoS One. 2011;6(5):e18205. doi: 10.1371/journal.pone.0018205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Roelvink PW, Lizonova A, Lee JG, Li Y, Bergelson JM, Finberg RW, Brough DE, Kovesdi I, Wickham TJ. The coxsackievirus–adenovirus receptor protein can function as a cellular attachment protein for adenovirus serotypes from subgroups A, C, D, E, and F. J Virol. 1998;72(10):7909–7915. doi: 10.1128/jvi.72.10.7909-7915.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Law LK, Davidson BL. What does it take to bind CAR? Mol Ther. 2005;12(4):599–609. doi: 10.1016/j.ymthe.2005.05.017. [DOI] [PubMed] [Google Scholar]
- 35.Seiradake E, Henaff D, Wodrich H, Billet O, Perreau M, Hippert C, Mennechet F, Schoehn G, Lortat-Jacob H, Dreja H, Ibanes S, Kalatzis V, Wang JP, Finberg RW, Cusack S, Kremer EJ. The cell adhesion molecule “CAR” and sialic acid on human erythrocytes influence adenovirus in vivo biodistribution. PLoS Pathog. 2009;5(1):e1000277. doi: 10.1371/journal.ppat.1000277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wickham TJ, Mathias P, Cheresh DA, Nemerow GR. Integrins alpha v beta 3 and alpha v beta 5 promote adenovirus internalization but not virus attachment. Cell. 1993;73(2):309–319. doi: 10.1016/0092-8674(93)90231-E. [DOI] [PubMed] [Google Scholar]
- 37.Amstutz B, Gastaldelli M, Kalin S, Imelli N, Boucke K, Wandeler E, Mercer J, Hemmi S, Greber UF. Subversion of CtBP1-controlled macropinocytosis by human adenovirus serotype 3. EMBO J. 2008;27(7):956–969. doi: 10.1038/emboj.2008.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Huang J, Tan D, Wang Y, Liu C, Xu J, Wang J. Egg drop syndrome virus enters duck embryonic fibroblast cells via clathrin-mediated endocytosis. Virus Res. 2015;210:69–76. doi: 10.1016/j.virusres.2015.07.014. [DOI] [PubMed] [Google Scholar]
- 39.Guzman E, Taylor G, Hope J, Herbert R, Cubillos-Zapata C, Charleston B. Transduction of skin-migrating dendritic cells by human adenovirus 5 occurs via an actin-dependent phagocytic pathway. J Gen Virol. 2016 doi: 10.1099/jgv.0.000581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wang H, Liaw YC, Stone D, Kalyuzhniy O, Amiraslanov I, Tuve S, Verlinde CL, Shayakhmetov D, Stehle T, Roffler S, Lieber A. Identification of CD46 binding sites within the adenovirus serotype 35 fiber knob. J Virol. 2007;81(23):12785–12792. doi: 10.1128/JVI.01732-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Persson BD, Muller S, Reiter DM, Schmitt BB, Marttila M, Sumowski CV, Schweizer S, Scheu U, Ochsenfeld C, Arnberg N, Stehle T. An arginine switch in the species B adenovirus knob determines high-affinity engagement of cellular receptor CD46. J Virol. 2009;83(2):673–686. doi: 10.1128/JVI.01967-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cupelli K, Muller S, Persson BD, Jost M, Arnberg N, Stehle T. Structure of adenovirus type 21 knob in complex with CD46 reveals key differences in receptor contacts among species B adenoviruses. J Virol. 2010;84(7):3189–3200. doi: 10.1128/JVI.01964-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sirena D, Lilienfeld B, Eisenhut M, Kalin S, Boucke K, Beerli RR, Vogt L, Ruedl C, Bachmann MF, Greber UF, Hemmi S. The human membrane cofactor CD46 is a receptor for species B adenovirus serotype 3. J Virol. 2004;78(9):4454–4462. doi: 10.1128/JVI.78.9.4454-4462.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Fleischli C, Verhaagh S, Havenga M, Sirena D, Schaffner W, Cattaneo R, Greber UF, Hemmi S. The distal short consensus repeats 1 and 2 of the membrane cofactor protein CD46 and their distance from the cell membrane determine productive entry of species B adenovirus serotype 35. J Virol. 2005;79(15):10013–10022. doi: 10.1128/JVI.79.15.10013-10022.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Marttila M, Persson D, Gustafsson D, Liszewski MK, Atkinson JP, Wadell G, Arnberg N. CD46 is a cellular receptor for all species B adenoviruses except types 3 and 7. J Virol. 2005;79(22):14429–14436. doi: 10.1128/JVI.79.22.14429-14436.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Fleischli C, Sirena D, Lesage G, Havenga MJ, Cattaneo R, Greber UF, Hemmi S. Species B adenovirus serotypes 3, 7, 11 and 35 share similar binding sites on the membrane cofactor protein CD46 receptor. J Gen Virol. 2007;88(Pt 11):2925–2934. doi: 10.1099/vir.0.83142-0. [DOI] [PubMed] [Google Scholar]
- 47.Short JJ, Vasu C, Holterman MJ, Curiel DT, Pereboev A. Members of adenovirus species B utilize CD80 and CD86 as cellular attachment receptors. Virus Res. 2006;122(1–2):144–153. doi: 10.1016/j.virusres.2006.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wang H, Li ZY, Liu Y, Persson J, Beyer I, Moller T, Koyuncu D, Drescher MR, Strauss R, Zhang XB, Wahl JK, 3rd, Urban N, Drescher C, Hemminki A, Fender P, Lieber A. Desmoglein 2 is a receptor for adenovirus serotypes 3, 7, 11 and 14. Nat Med. 2011;17(1):96–104. doi: 10.1038/nm.2270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Dechecchi MC, Tamanini A, Bonizzato A, Cabrini G. Heparan sulfate glycosaminoglycans are involved in adenovirus type 5 and 2-host cell interactions. Virology. 2000;268(2):382–390. doi: 10.1006/viro.1999.0171. [DOI] [PubMed] [Google Scholar]
- 50.Robinson CM, Zhou X, Rajaiya J, Yousuf MA, Singh G, Deserres JJ, Walsh MP, Wong S, Seto D, Dyer DW, Chodosh J, Jones MS (2013) Predicting the next eye pathogen: analysis of a novel adenovirus. MBio 4(2):e00595-00512. doi:10.1128/mBio.00595-12 [DOI] [PMC free article] [PubMed]
- 51.Hong SS, Karayan L, Tournier J, Curiel DT, Boulanger PA. Adenovirus type 5 fiber knob binds to MHC class I alpha2 domain at the surface of human epithelial and B lymphoblastoid cells. EMBO J. 1997;16(9):2294–2306. doi: 10.1093/emboj/16.9.2294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Burmeister WP, Guilligay D, Cusack S, Wadell G, Arnberg N. Crystal structure of species D adenovirus fiber knobs and their sialic acid binding sites. J Virol. 2004;78(14):7727–7736. doi: 10.1128/JVI.78.14.7727-7736.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Chu Y, Heistad D, Cybulsky MI, Davidson BL. Vascular cell adhesion molecule-1 augments adenovirus-mediated gene transfer. Arterioscler Thromb Vasc Biol. 2001;21(2):238–242. doi: 10.1161/01.ATV.21.2.238. [DOI] [PubMed] [Google Scholar]
- 54.Nilsson EC, Storm RJ, Bauer J, Johansson SM, Lookene A, Angstrom J, Hedenstrom M, Eriksson TL, Frangsmyr L, Rinaldi S, Willison HJ, Pedrosa Domellof F, Stehle T, Arnberg N. The GD1a glycan is a cellular receptor for adenoviruses causing epidemic keratoconjunctivitis. Nat Med. 2011;17(1):105–109. doi: 10.1038/nm.2267. [DOI] [PubMed] [Google Scholar]
- 55.Cooper RS, Heldwein EE. Herpesvirus gB: a finely tuned fusion machine. Viruses. 2015;7(12):6552–6569. doi: 10.3390/v7122957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Heldwein EE. gH/gL supercomplexes at early stages of herpesvirus entry. Curr Opin Virol. 2016;18:1–8. doi: 10.1016/j.coviro.2016.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Akula SM, Pramod NP, Wang FZ, Chandran B. Integrin alpha3beta1 (CD 49c/29) is a cellular receptor for Kaposi’s sarcoma-associated herpesvirus (KSHV/HHV-8) entry into the target cells. Cell. 2002;108(3):407–419. doi: 10.1016/S0092-8674(02)00628-1. [DOI] [PubMed] [Google Scholar]
- 58.Pertel PE. Human herpesvirus 8 glycoprotein B (gB), gH, and gL can mediate cell fusion. J Virol. 2002;76(9):4390–4400. doi: 10.1128/JVI.76.9.4390-4400.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Wang FZ, Akula SM, Pramod NP, Zeng L, Chandran B. Human herpesvirus 8 envelope glycoprotein K8.1A interaction with the target cells involves heparan sulfate. J Virol. 2001;75(16):7517–7527. doi: 10.1128/JVI.75.16.7517-7527.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Birkmann A, Mahr K, Ensser A, Yaguboglu S, Titgemeyer F, Fleckenstein B, Neipel F. Cell surface heparan sulfate is a receptor for human herpesvirus 8 and interacts with envelope glycoprotein K8.1. J Virol. 2001;75(23):11583–11593. doi: 10.1128/JVI.75.23.11583-11593.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Chakraborty S, Veettil MV, Chandran B. Kaposi’s sarcoma associated herpesvirus entry into target cells. Front Microbiol. 2012;3:6. doi: 10.3389/fmicb.2012.00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Yang E, Arvin AM, Oliver SL. Role for the alphaV integrin subunit in Varicella–Zoster virus-mediated fusion and infection. J Virol. 2016;90(16):7567–7578. doi: 10.1128/JVI.00792-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Schmid MF, Hecksel CW, Rochat RH, Bhella D, Chiu W, Rixon FJ. A tail-like assembly at the portal vertex in intact herpes simplex type-1 virions. PLoS Pathog. 2012;8(10):e1002961. doi: 10.1371/journal.ppat.1002961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Cha TA, Tom E, Kemble GW, Duke GM, Mocarski ES, Spaete RR. Human cytomegalovirus clinical isolates carry at least 19 genes not found in laboratory strains. J Virol. 1996;70(1):78–83. doi: 10.1128/jvi.70.1.78-83.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Adler B, Scrivano L, Ruzcics Z, Rupp B, Sinzger C, Koszinowski U. Role of human cytomegalovirus UL131A in cell type-specific virus entry and release. J Gen Virol. 2006;87(Pt 9):2451–2460. doi: 10.1099/vir.0.81921-0. [DOI] [PubMed] [Google Scholar]
- 66.Ryckman BJ, Rainish BL, Chase MC, Borton JA, Nelson JA, Jarvis MA, Johnson DC. Characterization of the human cytomegalovirus gH/gL/UL128-131 complex that mediates entry into epithelial and endothelial cells. J Virol. 2008;82(1):60–70. doi: 10.1128/JVI.01910-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Hahn G, Revello MG, Patrone M, Percivalle E, Campanini G, Sarasini A, Wagner M, Gallina A, Milanesi G, Koszinowski U, Baldanti F, Gerna G. Human cytomegalovirus UL131-128 genes are indispensable for virus growth in endothelial cells and virus transfer to leukocytes. J Virol. 2004;78(18):10023–10033. doi: 10.1128/JVI.78.18.10023-10033.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Wang D, Shenk T. Human cytomegalovirus virion protein complex required for epithelial and endothelial cell tropism. Proc Natl Acad Sci USA. 2005;102(50):18153–18158. doi: 10.1073/pnas.0509201102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Patrone M, Secchi M, Fiorina L, Ierardi M, Milanesi G, Gallina A. Human cytomegalovirus UL130 protein promotes endothelial cell infection through a producer cell modification of the virion. J Virol. 2005;79(13):8361–8373. doi: 10.1128/JVI.79.13.8361-8373.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Heldwein EE, Krummenacher C. Entry of herpesviruses into mammalian cells. Cell Mol Life Sci. 2008;65(11):1653–1668. doi: 10.1007/s00018-008-7570-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Connolly SA, Jackson JO, Jardetzky TS, Longnecker R. Fusing structure and function: a structural view of the herpesvirus entry machinery. Nat Rev Microbiol. 2011;9(5):369–381. doi: 10.1038/nrmicro2548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Eisenberg RJ, Atanasiu D, Cairns TM, Gallagher JR, Krummenacher C, Cohen GH. Herpes virus fusion and entry: a story with many characters. Viruses. 2012;4(5):800–832. doi: 10.3390/v4050800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Salameh S, Sheth U, Shukla D. Early events in herpes simplex virus lifecycle with implications for an infection of lifetime. Open Virol J. 2012;6:1–6. doi: 10.2174/1874357901206010001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Gardner TJ, Tortorella D. Virion glycoprotein-mediated immune evasion by human cytomegalovirus: a sticky virus makes a slick getaway. Microbiol Mol Biol Rev. 2016;80(3):663–677. doi: 10.1128/MMBR.00018-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Shannon-Lowe C, Rowe M. Epstein Barr virus entry; kissing and conjugation. Curr Opin Virol. 2014;4:78–84. doi: 10.1016/j.coviro.2013.12.001. [DOI] [PubMed] [Google Scholar]
- 76.Agelidis AM, Shukla D. Cell entry mechanisms of HSV: what we have learned in recent years. Future Virol. 2015;10(10):1145–1154. doi: 10.2217/fvl.15.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Gillet L, Frederico B, Stevenson PG. Host entry by gamma-herpesviruses—lessons from animal viruses? Curr Opin Virol. 2015;15:34–40. doi: 10.1016/j.coviro.2015.07.007. [DOI] [PubMed] [Google Scholar]
- 78.Ryckman BJ, Jarvis MA, Drummond DD, Nelson JA, Johnson DC. Human cytomegalovirus entry into epithelial and endothelial cells depends on genes UL128 to UL150 and occurs by endocytosis and low-pH fusion. J Virol. 2006;80(2):710–722. doi: 10.1128/JVI.80.2.710-722.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Chen J, Rowe CL, Jardetzky TS, Longnecker R (2012) The KGD motif of Epstein–Barr virus gH/gL is bifunctional, orchestrating infection of B cells and epithelial cells. MBio 3(1). doi:10.1128/mBio.00290-11 [DOI] [PMC free article] [PubMed]
- 80.Li Q, Spriggs MK, Kovats S, Turk SM, Comeau MR, Nepom B, Hutt-Fletcher LM. Epstein–Barr virus uses HLA class II as a cofactor for infection of B lymphocytes. J Virol. 1997;71(6):4657–4662. doi: 10.1128/jvi.71.6.4657-4662.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Wang X, Hutt-Fletcher LM. Epstein–Barr virus lacking glycoprotein gp42 can bind to B cells but is not able to infect. J Virol. 1998;72(1):158–163. doi: 10.1128/jvi.72.1.158-163.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Wang HB, Zhang H, Zhang JP, Li Y, Zhao B, Feng GK, Du Y, Xiong D, Zhong Q, Liu WL, Du H, Li MZ, Huang WL, Tsao SW, Hutt-Fletcher L, Zeng YX, Kieff E, Zeng MS. Neuropilin 1 is an entry factor that promotes EBV infection of nasopharyngeal epithelial cells. Nat Commun. 2015;6:6240. doi: 10.1038/ncomms7240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Kirschner AN, Omerovic J, Popov B, Longnecker R, Jardetzky TS. Soluble Epstein–Barr virus glycoproteins gH, gL, and gp42 form a 1:1:1 stable complex that acts like soluble gp42 in B-cell fusion but not in epithelial cell fusion. J Virol. 2006;80(19):9444–9454. doi: 10.1128/JVI.00572-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Tugizov SM, Berline JW, Palefsky JM. Epstein–Barr virus infection of polarized tongue and nasopharyngeal epithelial cells. Nat Med. 2003;9(3):307–314. doi: 10.1038/nm830. [DOI] [PubMed] [Google Scholar]
- 85.Inoue N, Winter J, Lal RB, Offermann MK, Koyano S. Characterization of entry mechanisms of human herpesvirus 8 by using an Rta-dependent reporter cell line. J Virol. 2003;77(14):8147–8152. doi: 10.1128/JVI.77.14.8147-8152.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Akula SM, Naranatt PP, Walia NS, Wang FZ, Fegley B, Chandran B. Kaposi’s sarcoma-associated herpesvirus (human herpesvirus 8) infection of human fibroblast cells occurs through endocytosis. J Virol. 2003;77(14):7978–7990. doi: 10.1128/JVI.77.14.7978-7990.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Rappocciolo G, Hensler HR, Jais M, Reinhart TA, Pegu A, Jenkins FJ, Rinaldo CR. Human herpesvirus 8 infects and replicates in primary cultures of activated B lymphocytes through DC-SIGN. J Virol. 2008;82(10):4793–4806. doi: 10.1128/JVI.01587-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Raghu H, Sharma-Walia N, Veettil MV, Sadagopan S, Chandran B. Kaposi’s sarcoma-associated herpesvirus utilizes an actin polymerization-dependent macropinocytic pathway to enter human dermal microvascular endothelial and human umbilical vein endothelial cells. J Virol. 2009;83(10):4895–4911. doi: 10.1128/JVI.02498-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Kerur N, Veettil MV, Sharma-Walia N, Sadagopan S, Bottero V, Paul AG, Chandran B. Characterization of entry and infection of monocytic THP-1 cells by Kaposi’s Sarcoma Associated Herpesvirus (KSHV): role of heparan sulfate, DC-SIGN, integrins and signaling. Virology. 2010;406(1):103–116. doi: 10.1016/j.virol.2010.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Meier O, Boucke K, Hammer SV, Keller S, Stidwill RP, Hemmi S, Greber UF. Adenovirus triggers macropinocytosis and endosomal leakage together with its clathrin-mediated uptake. J Cell Biol. 2002;158(6):1119–1131. doi: 10.1083/jcb.200112067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Kalin S, Amstutz B, Gastaldelli M, Wolfrum N, Boucke K, Havenga M, DiGennaro F, Liska N, Hemmi S, Greber UF. Macropinocytotic uptake and infection of human epithelial cells with species B2 adenovirus type 35. J Virol. 2010;84(10):5336–5350. doi: 10.1128/JVI.02494-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Nicola AV, McEvoy AM, Straus SE. Roles for endocytosis and low pH in herpes simplex virus entry into HeLa and Chinese hamster ovary cells. J Virol. 2003;77(9):5324–5332. doi: 10.1128/JVI.77.9.5324-5332.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Nicola AV, Hou J, Major EO, Straus SE. Herpes simplex virus type 1 enters human epidermal keratinocytes, but not neurons, via a pH-dependent endocytic pathway. J Virol. 2005;79(12):7609–7616. doi: 10.1128/JVI.79.12.7609-7616.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Nicola AV, Straus SE (2004) Cellular and viral requirements for rapid endocytic entry of herpes simplex virus. J Virol 78 (14):7508-7517. doi:10.1128/JVI.78.14.7508-7517.2004 [DOI] [PMC free article] [PubMed]
- 95.Shukla SY, Singh YK, Shukla D. Role of nectin-1, HVEM, and PILR-alpha in HSV-2 entry into human retinal pigment epithelial cells. Invest Ophthalmol Vis Sci. 2009;50(6):2878–2887. doi: 10.1167/iovs.08-2981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Satoh T, Arii J, Suenaga T, Wang J, Kogure A, Uehori J, Arase N, Shiratori I, Tanaka S, Kawaguchi Y, Spear PG, Lanier LL, Arase H. PILRalpha is a herpes simplex virus-1 entry coreceptor that associates with glycoprotein B. Cell. 2008;132(6):935–944. doi: 10.1016/j.cell.2008.01.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Geraghty RJ, Krummenacher C, Cohen GH, Eisenberg RJ, Spear PG. Entry of alphaherpesviruses mediated by poliovirus receptor-related protein 1 and poliovirus receptor. Science. 1998;280(5369):1618–1620. doi: 10.1126/science.280.5369.1618. [DOI] [PubMed] [Google Scholar]
- 98.Cocchi F, Menotti L, Mirandola P, Lopez M, Campadelli-Fiume G. The ectodomain of a novel member of the immunoglobulin subfamily related to the poliovirus receptor has the attributes of a bona fide receptor for herpes simplex virus types 1 and 2 in human cells. J Virol. 1998;72(12):9992–10002. doi: 10.1128/jvi.72.12.9992-10002.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Zhang N, Yan J, Lu G, Guo Z, Fan Z, Wang J, Shi Y, Qi J, Gao GF. Binding of herpes simplex virus glycoprotein D to nectin-1 exploits host cell adhesion. Nat Commun. 2011;2:577. doi: 10.1038/ncomms1571. [DOI] [PubMed] [Google Scholar]
- 100.Gianni T, Salvioli S, Chesnokova LS, Hutt-Fletcher LM, Campadelli-Fiume G. alphavbeta6- and alphavbeta8-integrins serve as interchangeable receptors for HSV gH/gL to promote endocytosis and activation of membrane fusion. PLoS Pathog. 2013;9(12):e1003806. doi: 10.1371/journal.ppat.1003806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Gianni T, Leoni V, Campadelli-Fiume G. Type I interferon and NF-kappaB activation elicited by herpes simplex virus gH/gL via alphavbeta3 integrin in epithelial and neuronal cell lines. J Virol. 2013;87(24):13911–13916. doi: 10.1128/JVI.01894-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Montgomery RI, Warner MS, Lum BJ, Spear PG. Herpes simplex virus-1 entry into cells mediated by a novel member of the TNF/NGF receptor family. Cell. 1996;87(3):427–436. doi: 10.1016/S0092-8674(00)81363-X. [DOI] [PubMed] [Google Scholar]
- 103.Stiles KM, Whitbeck JC, Lou H, Cohen GH, Eisenberg RJ, Krummenacher C. Herpes simplex virus glycoprotein D interferes with binding of herpesvirus entry mediator to its ligands through downregulation and direct competition. J Virol. 2010;84(22):11646–11660. doi: 10.1128/JVI.01550-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Bacsa S, Karasneh G, Dosa S, Liu J, Valyi-Nagy T, Shukla D. Syndecan-1 and syndecan-2 play key roles in herpes simplex virus type-1 infection. J Gen Virol. 2011;92(Pt 4):733–743. doi: 10.1099/vir.0.027052-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Petermann P, Rahn E, Thier K, Hsu MJ, Rixon FJ, Kopp SJ, Knebel-Morsdorf D. Role of nectin-1 and herpesvirus entry mediator as cellular receptors for herpes simplex virus 1 on primary murine dermal fibroblasts. J Virol. 2015;89(18):9407–9416. doi: 10.1128/JVI.01415-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Karaba AH, Kopp SJ, Longnecker R. Herpesvirus entry mediator and nectin-1 mediate herpes simplex virus 1 infection of the murine cornea. J Virol. 2011;85(19):10041–10047. doi: 10.1128/JVI.05445-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Bello-Morales R, Crespillo AJ, Praena B, Tabares E, Revilla Y, Garcia E, Fraile-Ramos A, Baron W, Krummenacher C, Lopez-Guerrero JA. Role of proteolipid protein in HSV-1 entry in oligodendrocytic cells. PLoS One. 2016;11(1):e0147885. doi: 10.1371/journal.pone.0147885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Gianni T, Amasio M, Campadelli-Fiume G. Herpes simplex virus gD forms distinct complexes with fusion executors gB and gH/gL in part through the C-terminal profusion domain. J Biol Chem. 2009;284(26):17370–17382. doi: 10.1074/jbc.M109.005728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Arii J, Goto H, Suenaga T, Oyama M, Kozuka-Hata H, Imai T, Minowa A, Akashi H, Arase H, Kawaoka Y, Kawaguchi Y. Non-muscle myosin IIA is a functional entry receptor for herpes simplex virus-1. Nature. 2010;467(7317):859–862. doi: 10.1038/nature09420. [DOI] [PubMed] [Google Scholar]
- 110.Kirschner AN, Sorem J, Longnecker R, Jardetzky TS. Structure of Epstein–Barr virus glycoprotein 42 suggests a mechanism for triggering receptor-activated virus entry. Structure. 2009;17(2):223–233. doi: 10.1016/j.str.2008.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Tiwari V, Clement C, Xu D, Valyi-Nagy T, Yue BY, Liu J, Shukla D. Role for 3-O-sulfated heparan sulfate as the receptor for herpes simplex virus type 1 entry into primary human corneal fibroblasts. J Virol. 2006;80(18):8970–8980. doi: 10.1128/JVI.00296-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Santoro F, Kennedy PE, Locatelli G, Malnati MS, Berger EA, Lusso P. CD46 is a cellular receptor for human herpesvirus 6. Cell. 1999;99(7):817–827. doi: 10.1016/S0092-8674(00)81678-5. [DOI] [PubMed] [Google Scholar]
- 113.Mori Y, Yang X, Akkapaiboon P, Okuno T, Yamanishi K. Human herpesvirus 6 variant A glycoprotein H-glycoprotein L-glycoprotein Q complex associates with human CD46. J Virol. 2003;77(8):4992–4999. doi: 10.1128/JVI.77.8.4992-4999.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Santoro F, Greenstone HL, Insinga A, Liszewski MK, Atkinson JP, Lusso P, Berger EA. Interaction of glycoprotein H of human herpesvirus 6 with the cellular receptor CD46. J Biol Chem. 2003;278(28):25964–25969. doi: 10.1074/jbc.M302373200. [DOI] [PubMed] [Google Scholar]
- 115.Tanaka Y, Suenaga T, Matsumoto M, Seya T, Arase H (2013) Herpesvirus 6 glycoproteins B (gB), gH, gL, and gQ are necessary and sufficient for cell-to-cell fusion. J Virol 87 (19):10900-10903. doi:10.1128/JVI.01427-13 [DOI] [PMC free article] [PubMed]
- 116.Secchiero P, Sun D, De Vico AL, Crowley RW, Reitz MS, Jr, Zauli G, Lusso P, Gallo RC. Role of the extracellular domain of human herpesvirus 7 glycoprotein B in virus binding to cell surface heparan sulfate proteoglycans. J Virol. 1997;71(6):4571–4580. doi: 10.1128/jvi.71.6.4571-4580.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Compton T, Nepomuceno RR, Nowlin DM. Human cytomegalovirus penetrates host cells by pH-independent fusion at the cell surface. Virology. 1992;191(1):387–395. doi: 10.1016/0042-6822(92)90200-9. [DOI] [PubMed] [Google Scholar]
- 118.Wang X, Huong SM, Chiu ML, Raab-Traub N, Huang ES. Epidermal growth factor receptor is a cellular receptor for human cytomegalovirus. Nature. 2003;424(6947):456–461. doi: 10.1038/nature01818. [DOI] [PubMed] [Google Scholar]
- 119.Feire AL, Koss H, Compton T. Cellular integrins function as entry receptors for human cytomegalovirus via a highly conserved disintegrin-like domain. Proc Natl Acad Sci USA. 2004;101(43):15470–15475. doi: 10.1073/pnas.0406821101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Wang X, Huang DY, Huong SM, Huang ES. Integrin alphavbeta3 is a coreceptor for human cytomegalovirus. Nat Med. 2005;11(5):515–521. doi: 10.1038/nm1236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Tugizov S, Navarro D, Paz P, Wang Y, Qadri I, Pereira L. Function of human cytomegalovirus glycoprotein B: syncytium formation in cells constitutively expressing gB is blocked by virus-neutralizing antibodies. Virology. 1994;201(2):263–276. doi: 10.1006/viro.1994.1291. [DOI] [PubMed] [Google Scholar]
- 122.Kinzler ER, Compton T. Characterization of human cytomegalovirus glycoprotein-induced cell–cell fusion. J Virol. 2005;79(12):7827–7837. doi: 10.1128/JVI.79.12.7827-7837.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Zhou M, Lanchy JM, Ryckman BJ. Human cytomegalovirus gH/gL/gO promotes the fusion step of entry into all cell types, whereas gH/gL/UL128-131 broadens virus tropism through a distinct mechanism. J Virol. 2015;89(17):8999–9009. doi: 10.1128/JVI.01325-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Tanner J, Weis J, Fearon D, Whang Y, Kieff E. Epstein–Barr virus gp350/220 binding to the B lymphocyte C3d receptor mediates adsorption, capping, and endocytosis. Cell. 1987;50(2):203–213. doi: 10.1016/0092-8674(87)90216-9. [DOI] [PubMed] [Google Scholar]
- 125.Miller N, Hutt-Fletcher LM. Epstein–Barr virus enters B cells and epithelial cells by different routes. J Virol. 1992;66(6):3409–3414. doi: 10.1128/jvi.66.6.3409-3414.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Speck P, Haan KM, Longnecker R. Epstein–Barr virus entry into cells. Virology. 2000;277(1):1–5. doi: 10.1006/viro.2000.0624. [DOI] [PubMed] [Google Scholar]
- 127.Nemerow GR, Wolfert R, McNaughton ME, Cooper NR. Identification and characterization of the Epstein–Barr virus receptor on human B lymphocytes and its relationship to the C3d complement receptor (CR2) J Virol. 1985;55(2):347–351. doi: 10.1128/jvi.55.2.347-351.1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Chesnokova LS, Nishimura SL, Hutt-Fletcher LM. Fusion of epithelial cells by Epstein–Barr virus proteins is triggered by binding of viral glycoproteins gHgL to integrins alphavbeta6 or alphavbeta8. Proc Natl Acad Sci USA. 2009;106(48):20464–20469. doi: 10.1073/pnas.0907508106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Veettil MV, Kumar B, Ansari MA, Dutta D, Iqbal J, Gjyshi O, Bottero V, Chandran B. ESCRT-0 component Hrs promotes macropinocytosis of Kaposi’s Sarcoma-Associated Herpesvirus in human dermal microvascular endothelial cells. J Virol. 2016;90(8):3860–3872. doi: 10.1128/JVI.02704-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Wang FZ, Akula SM, Sharma-Walia N, Zeng L, Chandran B. Human herpesvirus 8 envelope glycoprotein B mediates cell adhesion via its RGD sequence. J Virol. 2003;77(5):3131–3147. doi: 10.1128/JVI.77.5.3131-3147.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.AlHajri SM, Cunha CW, Nicola AV, Aguilar HC, Li H, Taus NS (2017) Ovine Herpesvirus 2 Glycoproteins B, H, and L Are Sufficient for, and Viral Glycoprotein Ov8 Can Enhance, Cell-Cell Membrane Fusion. J Virol 91 (6). doi:10.1128/JVI.02454-16 [DOI] [PMC free article] [PubMed]
- 132.Townsley AC, Weisberg AS, Wagenaar TR, Moss B. Vaccinia virus entry into cells via a low-pH-dependent endosomal pathway. J Virol. 2006;80(18):8899–8908. doi: 10.1128/JVI.01053-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Locker JK, Kuehn A, Schleich S, Rutter G, Hohenberg H, Wepf R, Griffiths G. Entry of the two infectious forms of vaccinia virus at the plasma membrane is signaling-dependent for the IMV but not the EEV. Mol Biol Cell. 2000;11(7):2497–2511. doi: 10.1091/mbc.11.7.2497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Mercer J, Helenius A. Vaccinia virus uses macropinocytosis and apoptotic mimicry to enter host cells. Science. 2008;320(5875):531–535. doi: 10.1126/science.1155164. [DOI] [PubMed] [Google Scholar]
- 135.Huang CY, Lu TY, Bair CH, Chang YS, Jwo JK, Chang W. A novel cellular protein, VPEF, facilitates vaccinia virus penetration into HeLa cells through fluid phase endocytosis. J Virol. 2008;82(16):7988–7999. doi: 10.1128/JVI.00894-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Mercer J, Knebel S, Schmidt FI, Crouse J, Burkard C, Helenius A. Vaccinia virus strains use distinct forms of macropinocytosis for host-cell entry. Proc Natl Acad Sci USA. 2010;107(20):9346–9351. doi: 10.1073/pnas.1004618107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Schmidt FI, Bleck CK, Helenius A, Mercer J. Vaccinia extracellular virions enter cells by macropinocytosis and acid-activated membrane rupture. EMBO J. 2011;30(17):3647–3661. doi: 10.1038/emboj.2011.245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Schroeder N, Chung CS, Chen CH, Liao CL, Chang W. The lipid raft-associated protein CD98 is required for vaccinia virus endocytosis. J Virol. 2012;86(9):4868–4882. doi: 10.1128/JVI.06610-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Sandgren KJ, Wilkinson J, Miranda-Saksena M, McInerney GM, Byth-Wilson K, Robinson PJ, Cunningham AL. A differential role for macropinocytosis in mediating entry of the two forms of vaccinia virus into dendritic cells. PLoS Pathog. 2010;6(4):e1000866. doi: 10.1371/journal.ppat.1000866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Izmailyan R, Hsao JC, Chung CS, Chen CH, Hsu PW, Liao CL, Chang W. Integrin beta1 mediates vaccinia virus entry through activation of PI3K/Akt signaling. J Virol. 2012;86(12):6677–6687. doi: 10.1128/JVI.06860-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Laliberte JP, Moss B. Lipid membranes in poxvirus replication. Viruses. 2010;2(4):972–986. doi: 10.3390/v2040972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Villa NY, Bartee E, Mohamed MR, Rahman MM, Barrett JW, McFadden G. Myxoma and vaccinia viruses exploit different mechanisms to enter and infect human cancer cells. Virology. 2010;401(2):266–279. doi: 10.1016/j.virol.2010.02.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Hiley CT, Chard LS, Gangeswaran R, Tysome JR, Briat A, Lemoine NR, Wang Y (2013) Vascular endothelial growth factor A promotes vaccinia virus entry into host cells via activation of the Akt pathway. J Virol 87 (5):2781-2790 [DOI] [PMC free article] [PubMed]
- 144.Chan WM, Bartee EC, Moreb JS, Dower K, Connor JH, McFadden G (2013) Myxoma and vaccinia viruses bind differentially to human leukocytes. J Virol 87 (8):4445-4460 [DOI] [PMC free article] [PubMed]
- 145.Byrd D, Amet T, Hu N, Lan J, Hu S, Yu Q. Primary human leukocyte subsets differentially express vaccinia virus receptors enriched in lipid rafts. J Virol. 2013;87(16):9301–9312. doi: 10.1128/JVI.01545-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Haga IR, Pechenick Jowers T, Griffiths SJ, Haas J, Beard PM. TRAF2 facilitates vaccinia virus replication by promoting rapid virus entry. J Virol. 2014;88(7):3664–3677. doi: 10.1128/JVI.03013-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Moser TS, Jones RG, Thompson CB, Coyne CB, Cherry S. A kinome RNAi screen identified AMPK as promoting poxvirus entry through the control of actin dynamics. PLoS Pathog. 2010;6(6):e1000954. doi: 10.1371/journal.ppat.1000954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Bengali Z, Satheshkumar PS, Yang Z, Weisberg AS, Paran N, Moss B. Drosophila S2 cells are non-permissive for vaccinia virus DNA replication following entry via low pH-dependent endocytosis and early transcription. PLoS One. 2011;6(2):e17248. doi: 10.1371/journal.pone.0017248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Whitbeck JC, Foo CH, Ponce de Leon M, Eisenberg RJ, Cohen GH. Vaccinia virus exhibits cell-type-dependent entry characteristics. Virology. 2009;385(2):383–391. doi: 10.1016/j.virol.2008.12.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Bengali Z, Townsley AC, Moss B. Vaccinia virus strain differences in cell attachment and entry. Virology. 2009;389(1–2):132–140. doi: 10.1016/j.virol.2009.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Bengali Z, Satheshkumar PS, Moss B. Orthopoxvirus species and strain differences in cell entry. Virology. 2012;433(2):506–512. doi: 10.1016/j.virol.2012.08.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Morizono K, Xie Y, Olafsen T, Lee B, Dasgupta A, Wu AM, Chen IS. The soluble serum protein Gas6 bridges virion envelope phosphatidylserine to the TAM receptor tyrosine kinase Axl to mediate viral entry. Cell Host Microbe. 2011;9(4):286–298. doi: 10.1016/j.chom.2011.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Doceul V, Hollinshead M, van der Linden L, Smith GL. Repulsion of superinfecting virions: a mechanism for rapid virus spread. Science. 2010;327(5967):873–876. doi: 10.1126/science.1183173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Turner PC, Moyer RW. The cowpox virus fusion regulator proteins SPI-3 and hemagglutinin interact in infected and uninfected cells. Virology. 2006;347(1):88–99. doi: 10.1016/j.virol.2005.11.012. [DOI] [PubMed] [Google Scholar]
- 155.Wagenaar TR, Moss B. Association of vaccinia virus fusion regulatory proteins with the multicomponent entry/fusion complex. J Virol. 2007;81(12):6286–6293. doi: 10.1128/JVI.00274-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Turner PC, Moyer RW. The vaccinia virus fusion inhibitor proteins SPI-3 (K2) and HA (A56) expressed by infected cells reduce the entry of superinfecting virus. Virology. 2008;380(2):226–233. doi: 10.1016/j.virol.2008.07.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Laliberte JP, Moss B. A novel mode of poxvirus superinfection exclusion that prevents fusion of the lipid bilayers of viral and cellular membranes. J Virol. 2014;88(17):9751–9768. doi: 10.1128/JVI.00816-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Wagenaar TR, Ojeda S, Moss B. Vaccinia virus A56/K2 fusion regulatory protein interacts with the A16 and G9 subunits of the entry fusion complex. J Virol. 2008;82(11):5153–5160. doi: 10.1128/JVI.00162-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Guo CJ, Liu D, Wu YY, Yang XB, Yang LS, Mi S, Huang YX, Luo YW, Jia KT, Liu ZY, Chen WJ, Weng SP, Yu XQ, He JG. Entry of tiger frog virus (an Iridovirus) into HepG2 cells via a pH-dependent, atypical, caveola-mediated endocytosis pathway. J Virol. 2011;85(13):6416–6426. doi: 10.1128/JVI.01500-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Braunwald J, Nonnenmacher H, Tripier-Darcy F (1985) Ultrastructural and biochemical study of frog virus 3 uptake by BHK-21 cells. J Gen Virol 66 ( Pt 2):283-293 [DOI] [PubMed]
- 161.Guo CJ, Wu YY, Yang LS, Yang XB, He J, Mi S, Jia KT, Weng SP, Yu XQ, He JG. Infectious spleen and kidney necrosis virus (a fish iridovirus) enters Mandarin fish fry cells via caveola-dependent endocytosis. J Virol. 2012;86(5):2621–2631. doi: 10.1128/JVI.06947-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Jia KT, Wu YY, Liu ZY, Mi S, Zheng YW, He J, Weng SP, Li SC, He JG, Guo CJ. Mandarin fish caveolin 1 interaction with major capsid protein of infectious spleen and kidney necrosis virus and its role in early stages of infection. J Virol. 2013;87(6):3027–3038. doi: 10.1128/JVI.00552-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Wang S, Huang X, Huang Y, Hao X, Xu H, Cai M, Wang H, Qin Q. Entry of a novel marine DNA virus, Singapore grouper iridovirus, into host cells occurs via clathrin-mediated endocytosis and macropinocytosis in a pH-dependent manner. J Virol. 2014;88(22):13047–13063. doi: 10.1128/JVI.01744-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Yuan Y, Wang Y, Liu Q, Zhu F, Hong Y. Singapore grouper iridovirus protein VP088 is essential for viral infectivity. Sci Rep. 2016;6:31170. doi: 10.1038/srep31170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Ao J, Chen X. Identification and characterization of a novel gene encoding an RGD-containing protein in large yellow croaker iridovirus. Virology. 2006;355(2):213–222. doi: 10.1016/j.virol.2006.07.004. [DOI] [PubMed] [Google Scholar]
- 166.Wu J, Chan R, Wenk MR, Hew CL. Lipidomic study of intracellular Singapore grouper iridovirus. Virology. 2010;399(2):248–256. doi: 10.1016/j.virol.2010.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Blissard GW, Wenz JR. Baculovirus gp64 envelope glycoprotein is sufficient to mediate pH-dependent membrane fusion. J Virol. 1992;66(11):6829–6835. doi: 10.1128/jvi.66.11.6829-6835.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Dong S, Wang M, Qiu Z, Deng F, Vlak JM, Hu Z, Wang H. Autographa californica multicapsid nucleopolyhedrovirus efficiently infects Sf9 cells and transduces mammalian cells via direct fusion with the plasma membrane at low pH. J Virol. 2010;84(10):5351–5359. doi: 10.1128/JVI.02517-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Kataoka C, Kaname Y, Taguwa S, Abe T, Fukuhara T, Tani H, Moriishi K, Matsuura Y. Baculovirus GP64-mediated entry into mammalian cells. J Virol. 2012;86(5):2610–2620. doi: 10.1128/JVI.06704-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Kato T, Sugioka S, Itagaki K, Park EY. Gene transduction in mammalian cells using Bombyx mori nucleopolyhedrovirus assisted by glycoprotein 64 of Autographa californica multiple nucleopolyhedrovirus. Sci Rep. 2016;6:32283. doi: 10.1038/srep32283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Huang J, Hao B, Cheng C, Liang F, Shen X, Cheng X. Entry of Bombyx mori nucleopolyhedrovirus into BmN cells by cholesterol-dependent macropinocytic endocytosis. Biochem Biophys Res Commun. 2014;453(1):166–171. doi: 10.1016/j.bbrc.2014.09.073. [DOI] [PubMed] [Google Scholar]
- 172.Laakkonen JP, Makela AR, Kakkonen E, Turkki P, Kukkonen S, Peranen J, Yla-Herttuala S, Airenne KJ, Oker-Blom C, Vihinen-Ranta M, Marjomaki V. Clathrin-independent entry of baculovirus triggers uptake of E. coli in non-phagocytic human cells. PLoS One. 2009;4(4):e5093. doi: 10.1371/journal.pone.0005093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Long G, Pan X, Kormelink R, Vlak JM. Functional entry of baculovirus into insect and mammalian cells is dependent on clathrin-mediated endocytosis. J Virol. 2006;80(17):8830–8833. doi: 10.1128/JVI.00880-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Makkonen KE, Turkki P, Laakkonen JP, Yla-Herttuala S, Marjomaki V, Airenne KJ. 6-o- and N-sulfated syndecan-1 promotes baculovirus binding and entry into mammalian cells. J Virol. 2013;87(20):11148–11159. doi: 10.1128/JVI.01919-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Luz-Madrigal A, Asanov A, Camacho-Zarco AR, Sampieri A, Vaca L. A cholesterol recognition amino acid consensus domain in GP64 fusion protein facilitates anchoring of baculovirus to mammalian cells. J Virol. 2013;87(21):11894–11907. doi: 10.1128/JVI.01356-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Moss B. Membrane fusion during poxvirus entry. Semin Cell Dev Biol. 2016 doi: 10.1016/j.semcdb.2016.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Moss B. Poxvirus entry and membrane fusion. Virology. 2006;344(1):48–54. doi: 10.1016/j.virol.2005.09.037. [DOI] [PubMed] [Google Scholar]
- 178.Smith GL, Vanderplasschen A, Law M. The formation and function of extracellular enveloped vaccinia virus. J Gen Virol. 2002;83(Pt 12):2915–2931. doi: 10.1099/0022-1317-83-12-2915. [DOI] [PubMed] [Google Scholar]
- 179.Senkevich TG, Moss B. Vaccinia virus H2 protein is an essential component of a complex involved in virus entry and cell–cell fusion. J Virol. 2005;79(8):4744–4754. doi: 10.1128/JVI.79.8.4744-4754.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Moss B. Poxvirus cell entry: how many proteins does it take? Viruses. 2012;4(5):688–707. doi: 10.3390/v4050688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Laliberte JP, Weisberg AS, Moss B. The membrane fusion step of vaccinia virus entry is cooperatively mediated by multiple viral proteins and host cell components. PLoS Pathog. 2011;7(12):e1002446. doi: 10.1371/journal.ppat.1002446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Vanderplasschen A, Hollinshead M, Smith GL. Intracellular and extracellular vaccinia virions enter cells by different mechanisms. J Gen Virol. 1998;79(Pt 4):877–887. doi: 10.1099/0022-1317-79-4-877. [DOI] [PubMed] [Google Scholar]
- 183.Sodeik B, Krijnse-Locker J. Assembly of vaccinia virus revisited: de novo membrane synthesis or acquisition from the host? Trends Microbiol. 2002;10(1):15–24. doi: 10.1016/S0966-842X(01)02256-9. [DOI] [PubMed] [Google Scholar]
- 184.Schmidt FI, Bleck CK, Reh L, Novy K, Wollscheid B, Helenius A, Stahlberg H, Mercer J. Vaccinia virus entry is followed by core activation and proteasome-mediated release of the immunomodulatory effector VH1 from lateral bodies. Cell Rep. 2013;4(3):464–476. doi: 10.1016/j.celrep.2013.06.028. [DOI] [PubMed] [Google Scholar]
- 185.Chiu WL, Lin CL, Yang MH, Tzou DL, Chang W. Vaccinia virus 4c (A26L) protein on intracellular mature virus binds to the extracellular cellular matrix laminin. J Virol. 2007;81(5):2149–2157. doi: 10.1128/JVI.02302-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Chang SJ, Chang YX, Izmailyan R, Tang YL, Chang W. Vaccinia virus A25 and A26 proteins are fusion suppressors for mature virions and determine strain-specific virus entry pathways into HeLa, CHO-K1, and L cells. J Virol. 2010;84(17):8422–8432. doi: 10.1128/JVI.00599-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Chung CS, Hsiao JC, Chang YS, Chang W. A27L protein mediates vaccinia virus interaction with cell surface heparan sulfate. J Virol. 1998;72(2):1577–1585. doi: 10.1128/jvi.72.2.1577-1585.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Kochan G, Escors D, Gonzalez JM, Casasnovas JM, Esteban M. Membrane cell fusion activity of the vaccinia virus A17-A27 protein complex. Cell Microbiol. 2008;10(1):149–164. doi: 10.1111/j.1462-5822.2007.01026.x. [DOI] [PubMed] [Google Scholar]
- 189.Hsiao JC, Chung CS, Chang W. Vaccinia virus envelope D8L protein binds to cell surface chondroitin sulfate and mediates the adsorption of intracellular mature virions to cells. J Virol. 1999;73(10):8750–8761. doi: 10.1128/jvi.73.10.8750-8761.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Lin CL, Chung CS, Heine HG, Chang W. Vaccinia virus envelope H3L protein binds to cell surface heparan sulfate and is important for intracellular mature virion morphogenesis and virus infection in vitro and in vivo. J Virol. 2000;74(7):3353–3365. doi: 10.1128/JVI.74.7.3353-3365.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Ojeda S, Senkevich TG, Moss B. Entry of vaccinia virus and cell–cell fusion require a highly conserved cysteine-rich membrane protein encoded by the A16L gene. J Virol. 2006;80(1):51–61. doi: 10.1128/JVI.80.1.51-61.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Townsley AC, Senkevich TG, Moss B. Vaccinia virus A21 virion membrane protein is required for cell entry and fusion. J Virol. 2005;79(15):9458–9469. doi: 10.1128/JVI.79.15.9458-9469.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Senkevich TG, Ward BM, Moss B. Vaccinia virus entry into cells is dependent on a virion surface protein encoded by the A28L gene. J Virol. 2004;78(5):2357–2366. doi: 10.1128/JVI.78.5.2357-2366.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Nelson GE, Wagenaar TR, Moss B. A conserved sequence within the H2 subunit of the vaccinia virus entry/fusion complex is important for interaction with the A28 subunit and infectivity. J Virol. 2008;82(13):6244–6250. doi: 10.1128/JVI.00434-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Shinoda K, Wyatt LS, Moss B. The neutralizing antibody response to the vaccinia virus A28 protein is specifically enhanced by its association with the H2 protein. Virology. 2010;405(1):41–49. doi: 10.1016/j.virol.2010.05.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Brown E, Senkevich TG, Moss B. Vaccinia virus F9 virion membrane protein is required for entry but not virus assembly, in contrast to the related L1 protein. J Virol. 2006;80(19):9455–9464. doi: 10.1128/JVI.01149-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Izmailyan RA, Huang CY, Mohammad S, Isaacs SN, Chang W. The envelope G3L protein is essential for entry of vaccinia virus into host cells. J Virol. 2006;80(17):8402–8410. doi: 10.1128/JVI.00624-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Ojeda S, Domi A, Moss B. Vaccinia virus G9 protein is an essential component of the poxvirus entry-fusion complex. J Virol. 2006;80(19):9822–9830. doi: 10.1128/JVI.00987-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Chang SJ, Shih AC, Tang YL, Chang W. Vaccinia mature virus fusion regulator A26 protein binds to A16 and G9 proteins of the viral entry fusion complex and dissociates from mature virions at low pH. J Virol. 2012;86(7):3809–3818. doi: 10.1128/JVI.06081-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Senkevich TG, Ojeda S, Townsley A, Nelson GE, Moss B. Poxvirus multiprotein entry-fusion complex. Proc Natl Acad Sci USA. 2005;102(51):18572–18577. doi: 10.1073/pnas.0509239102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Bisht H, Weisberg AS, Moss B. Vaccinia virus L1 protein is required for cell entry and membrane fusion. J Virol. 2008;82(17):8687–8694. doi: 10.1128/JVI.00852-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Townsley AC, Senkevich TG, Moss B. The product of the vaccinia virus L5R gene is a fourth membrane protein encoded by all poxviruses that is required for cell entry and cell–cell fusion. J Virol. 2005;79(17):10988–10998. doi: 10.1128/JVI.79.17.10988-10998.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Satheshkumar PS, Moss B. Sequence-divergent chordopoxvirus homologs of the O3 protein maintain functional interactions with components of the vaccinia virus entry-fusion complex. J Virol. 2012;86(3):1696–1705. doi: 10.1128/JVI.06069-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Saadi H, Pagnier I, Colson P, Cherif JK, Beji M, Boughalmi M, Azza S, Armstrong N, Robert C, Fournous G, La Scola B, Raoult D. First isolation of mimivirus in a patient with pneumonia. Clin Infect Dis. 2013;57(4):e127–e134. doi: 10.1093/cid/cit354. [DOI] [PubMed] [Google Scholar]
- 205.Saadi H, Reteno DG, Colson P, Aherfi S, Minodier P, Pagnier I, Raoult D, La Scola B. Shan virus: a new Mimivirus isolated from the stool of a Tunisian patient with pneumonia. Intervirology. 2013;56(6):424–429. doi: 10.1159/000354564. [DOI] [PubMed] [Google Scholar]
- 206.Boughalmi M, Pagnier I, Aherfi S, Colson P, Raoult D, La Scola B. First isolation of a Marseillevirus in the diptera Syrphidae Eristalis tenax. Intervirology. 2013;56(6):386–394. doi: 10.1159/000354560. [DOI] [PubMed] [Google Scholar]
- 207.Boughalmi M, Pagnier I, Aherfi S, Colson P, Raoult D, La Scola B. First isolation of a giant virus from wild Hirudo medicinalis leech: Mimiviridae isolation in Hirudo medicinalis. Viruses. 2013;5(12):2920–2930. doi: 10.3390/v5122920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Pagnier I, Reteno DG, Saadi H, Boughalmi M, Gaia M, Slimani M, Ngounga T, Bekliz M, Colson P, Raoult D, La Scola B. A decade of improvements in Mimiviridae and Marseilleviridae isolation from amoeba. Intervirology. 2013;56(6):354–363. doi: 10.1159/000354556. [DOI] [PubMed] [Google Scholar]
- 209.Kutikhin AG, Yuzhalin AE, Brusina EB. Mimiviridae, Marseilleviridae, and virophages as emerging human pathogens causing healthcare-associated infections. GMS Hyg Infect Control. 2014;9(2):Doc16. doi: 10.3205/dgkh000236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Zhang XA, Zhu T, Zhang PH, Li H, Li Y, Liu EM, Liu W, Cao WC. Lack of Mimivirus detection in patients with respiratory disease, China. Emerg Infect Dis. 2016 doi: 10.3201/eid2211.160687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Raoult D, Levasseur A, La Scola B. PCR detection of Mimivirus. Emerg Infect Dis. 2017;23(6):1044–1045. doi: 10.3201/eid2306.161896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Dornas FP, Boratto PVM, Costa GB, Silva LCF, Kroon EG, La Scola B, Trindade G, Abrahao JS. Detection of mimivirus genome and neutralizing antibodies in humans from Brazil. Arch Virol. 2017 doi: 10.1007/s00705-017-3455-5. [DOI] [PubMed] [Google Scholar]
- 213.Lusi EA, Maloney D, Caicci F, Guarascio P. Questions on unusual Mimivirus-like structures observed in human cells. F1000Res. 2017;6:262. doi: 10.12688/f1000research.11007.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Boyer M, Azza S, Barrassi L, Klose T, Campocasso A, Pagnier I, Fournous G, Borg A, Robert C, Zhang X, Desnues C, Henrissat B, Rossmann MG, La Scola B, Raoult D. Mimivirus shows dramatic genome reduction after intraamoebal culture. Proc Natl Acad Sci. 2011;108(25):10296–10301. doi: 10.1073/pnas.1101118108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Rodrigues RA, dos Santos Silva LK, Dornas FP, de Oliveira DB, Magalhaes TF, Santos DA, Costa AO, de Macedo Farias L, Magalhaes PP, Bonjardim CA, Kroon EG, La Scola B, Cortines JR, Abrahao JS. Mimivirus fibrils are important for viral attachment to the microbial world by a diverse glycoside interaction repertoire. J Virol. 2015;89(23):11812–11819. doi: 10.1128/JVI.01976-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Sobhy H, Scola BL, Pagnier I, Raoult D, Colson P. Identification of giant Mimivirus protein functions using RNA interference. Front Microbiol. 2015;6:345. doi: 10.3389/fmicb.2015.00345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Sobhy H (2014) Characterization of protein involved in the fibers of Mimivirus. PhD thesis, Universite d’Aix-Marseille, http://www.theses.fr/2014AIXM5029
- 218.Sobhy H, Gotthard G, Chabriere E, Raoult D, Colson P. Recombinant expression of Mimivirus L725 ORFan gene product. Acta Virol. 2017 doi: 10.4149/av_2017_01_116. [DOI] [PubMed] [Google Scholar]
- 219.Klose T, Herbst Dominik A, Zhu H, Max Joann P, Kenttämaa Hilkka I, Rossmann Michael G. A Mimivirus enzyme that participates in viral entry. Structure. 2015;23(6):1058–1065. doi: 10.1016/j.str.2015.03.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Ghigo E, Kartenbeck J, Lien P, Pelkmans L, Capo C, Mege JL, Raoult D. Ameobal pathogen mimivirus infects macrophages through phagocytosis. PLoS Pathog. 2008;4(6):e1000087. doi: 10.1371/journal.ppat.1000087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Suzan-Monti M, La Scola B, Barrassi L, Espinosa L, Raoult D. Ultrastructural characterization of the giant volcano-like virus factory of Acanthamoeba polyphaga Mimivirus. PLoS One. 2007;2(3):e328. doi: 10.1371/journal.pone.0000328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Arantes TS, Rodrigues RA, Dos Santos Silva LK, Oliveira GP, de Souza HL, Khalil JY, de Oliveira DB, Torres AA, da Silva LL, Colson P, Kroon EG, da Fonseca FG, Bonjardim CA, La Scola B, Abrahao JS. The large Marseillevirus explores different entry pathways by forming giant infectious vesicles. J Virol. 2016;90(11):5246–5255. doi: 10.1128/JVI.00177-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Meints RH, Lee K, Burbank DE, Van Etten JL. Infection of a chlorella-like alga with the virus, PBCV-1: ultrastructural studies. Virology. 1984;138(2):341–346. doi: 10.1016/0042-6822(84)90358-1. [DOI] [PubMed] [Google Scholar]
- 224.Yanai-Balser GM, Duncan GA, Eudy JD, Wang D, Li X, Agarkova IV, Dunigan DD, Van Etten JL. Microarray analysis of Paramecium bursaria chlorella virus 1 transcription. J Virol. 2010;84(1):532–542. doi: 10.1128/JVI.01698-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Wang K, Xie S, Sun B. Viral proteins function as ion channels. Biochim Biophys Acta 1808. 2011;2:510–515. doi: 10.1016/j.bbamem.2010.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Romani G, Piotrowski A, Hillmer S, Gurnon J, Van Etten JL, Moroni A, Thiel G, Hertel B. A virus-encoded potassium ion channel is a structural protein in the chlorovirus Paramecium bursaria chlorella virus 1 virion. J Gen Virol. 2013;94(Pt 11):2549–2556. doi: 10.1099/vir.0.055251-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Mackinder LC, Worthy CA, Biggi G, Hall M, Ryan KP, Varsani A, Harper GM, Wilson WH, Brownlee C, Schroeder DC. A unicellular algal virus, Emiliania huxleyi virus 86, exploits an animal-like infection strategy. J Gen Virol. 2009;90(Pt 9):2306–2316. doi: 10.1099/vir.0.011635-0. [DOI] [PubMed] [Google Scholar]
- 228.Maier I, Müller DG, Katsaros C. Entry of the DNA virus, Ectocarpus fasciculatus virus type 1 (Phycodnaviridae), into host cell cytosol and nucleus. Phycol Res. 2002;50(3):227–231. doi: 10.1111/j.1440-1835.2002.tb00155.x. [DOI] [Google Scholar]
- 229.Alonso C, Galindo I, Cuesta-Geijo MA, Cabezas M, Hernaez B, Munoz-Moreno R. African swine fever virus-cell interactions: from virus entry to cell survival. Virus Res. 2013;173(1):42–57. doi: 10.1016/j.virusres.2012.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Hernaez B, Alonso C. Dynamin- and clathrin-dependent endocytosis in African swine fever virus entry. J Virol. 2010;84(4):2100–2109. doi: 10.1128/JVI.01557-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Cuesta-Geijo MA, Galindo I, Hernaez B, Quetglas JI, Dalmau-Mena I, Alonso C. Endosomal maturation, Rab7 GTPase and phosphoinositides in African swine fever virus entry. PLoS One. 2012;7(11):e48853. doi: 10.1371/journal.pone.0048853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Galindo I, Cuesta-Geijo MA, Hlavova K, Munoz-Moreno R, Barrado-Gil L, Dominguez J, Alonso C. African swine fever virus infects macrophages, the natural host cells, via clathrin- and cholesterol-dependent endocytosis. Virus Res. 2015;200:45–55. doi: 10.1016/j.virusres.2015.01.022. [DOI] [PubMed] [Google Scholar]
- 233.Cuesta-Geijo MA, Chiappi M, Galindo I, Barrado-Gil L, Munoz-Moreno R, Carrascosa JL, Alonso C. Cholesterol flux is required for endosomal progression of African swine fever virions during the initial establishment of infection. J Virol. 2016;90(3):1534–1543. doi: 10.1128/JVI.02694-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Hernaez B, Guerra M, Salas ML, Andres G. African swine fever virus undergoes outer envelope disruption, capsid disassembly and inner envelope fusion before core release from multivesicular endosomes. PLoS Pathog. 2016;12(4):e1005595. doi: 10.1371/journal.ppat.1005595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Sanchez EG, Quintas A, Perez-Nunez D, Nogal M, Barroso S, Carrascosa AL, Revilla Y. African swine fever virus uses macropinocytosis to enter host cells. PLoS Pathog. 2012;8(6):e1002754. doi: 10.1371/journal.ppat.1002754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Chinchar VG, Yu KH, Jancovich JK. The molecular biology of frog virus 3 and other iridoviruses infecting cold-blooded vertebrates. Viruses. 2011;3(10):1959–1985. doi: 10.3390/v3101959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Hussain M, Garrad S, Asgari S. The role of actin filaments in ascovirus replication and pathology. Arch Virol. 2009;154(11):1737–1743. doi: 10.1007/s00705-009-0512-8. [DOI] [PubMed] [Google Scholar]
- 238.Kadlec J, Loureiro S, Abrescia NG, Stuart DI, Jones IM. The postfusion structure of baculovirus gp64 supports a unified view of viral fusion machines. Nat Struct Mol Biol. 2008;15(10):1024–1030. doi: 10.1038/nsmb.1484. [DOI] [PubMed] [Google Scholar]
- 239.Heldwein EE, Lou H, Bender FC, Cohen GH, Eisenberg RJ, Harrison SC. Crystal structure of glycoprotein B from herpes simplex virus 1. Science. 2006;313(5784):217–220. doi: 10.1126/science.1126548. [DOI] [PubMed] [Google Scholar]
- 240.Muggeridge MI. Glycoprotein B of herpes simplex virus 2 has more than one intracellular conformation and is altered by low pH. J Virol. 2012;86(12):6444–6456. doi: 10.1128/JVI.06668-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Vitu E, Sharma S, Stampfer SD, Heldwein EE. Extensive mutagenesis of the HSV-1 gB ectodomain reveals remarkable stability of its postfusion form. J Mol Biol. 2013;2836(13):00142–00147. doi: 10.1016/j.jmb.2013.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Sobhy H. A bioinformatics pipeline to search functional motifs within whole-proteome data: a case study of poxviruses. Virus Genes. 2016 doi: 10.1007/s11262-016-1416-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Wodrich H, Henaff D, Jammart B, Segura-Morales C, Seelmeir S, Coux O, Ruzsics Z, Wiethoff CM, Kremer EJ. A capsid-encoded PPxY-motif facilitates adenovirus entry. PLoS Pathog. 2010;6(3):e1000808. doi: 10.1371/journal.ppat.1000808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Marvin SA, Wiethoff CM. Emerging roles for ubiquitin in adenovirus cell entry. Biol Cell. 2012;104(3):188–198. doi: 10.1111/boc.201100096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.DuRose JB, Li J, Chien S, Spector DH. Infection of vascular endothelial cells with human cytomegalovirus under fluid shear stress reveals preferential entry and spread of virus in flow conditions simulating atheroprone regions of the artery. J Virol. 2012;86(24):13745–13755. doi: 10.1128/JVI.02244-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.Colpitts CC, Ustinov AV, Epand RF, Epand RM, Korshun VA, Schang LM. 5-(Perylen-3-yl)ethynyl-arabino-uridine (aUY11), an arabino-based rigid amphipathic fusion inhibitor, targets virion envelope lipids to inhibit fusion of influenza virus, hepatitis C virus, and other enveloped viruses. J Virol. 2013;87(7):3640–3654. doi: 10.1128/JVI.02882-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.O’Flynn NM, Patel A, Kadlec J, Jones IM. Improving promiscuous mammalian cell entry by the baculovirus AcMNPV. Biosci Rep. 2012;2012:4. doi: 10.1042/BSR20120093. [DOI] [PMC free article] [PubMed] [Google Scholar]