Abstract
Background
To isolate hospital effects on hospitals’ risk-standardized readmission rates, we examined readmission outcomes among patients with multiple admissions for a similar diagnosis at >1 hospital within a given year.
Methods
We divided the Centers for Medicare & Medicaid Services hospital-wide readmission measure cohort from July 2014–June 2015 into 2 random samples. We used the first sample to calculate each hospital’s risk-standardized readmission rate and classified hospitals into performance quartiles. In the second sample, we identified patients with 2 admissions for similar diagnoses at different hospitals that occurred more than a month and less than a year apart, and compared observed readmission rates for those admitted to hospitals in different performance quartiles.
Results
In the sample used to characterize hospital performance, the median risk-standardized readmission rate was 15.5% (IQR 15.3%–15.8%). The other sample included 37,508 patients with 2 admissions for similar diagnoses at 4,272 different hospitals. The observed readmission rate was consistently higher when patients were admitted to hospitals in the worse performing quartile, but the only statistically significant difference was observed when the same patients were admitted to hospitals in the best and worst performing quartiles, in which the absolute readmission rate difference was 1.95 percentage points (95% CI, 0.39%–3.50%).
Conclusions
When the same patients were admitted with similar diagnoses to hospitals in the best performing quartile compared with the worst performing quartile for hospital readmission performance, there is a significant difference in rates of readmission within 30 days. The findings suggest that hospital quality contributes in part to readmission rates independent of patient factors.
INTRODUCTION
The measurement and reporting of 30-day hospital readmission rates by the Centers for Medicare & Medicaid Services (CMS) has had a major impact on healthcare delivery. These measures, first publicly reported in 2009, were subsequently incorporated into the Hospital Readmission Reduction Program, a quality incentive program mandated by the Affordable Care Act.1 Since the passage of the Affordable Care Act, readmission rates have declined significantly.2–5
Risk-standardized readmission rates, which are the basis of hospital assessment in the Hospital Readmission Reduction Program, are intended to account for hospital case-mix differences and to measure hospital quality of care.6–10 However, researchers and hospital administrators have expressed concerns about the adequacy of risk adjustment, questioning whether the readmission rates are valid estimates of quality and suggesting that they may reflect differences in social and clinical risk.11–17 A recent Department of Health and Human Services report to the US Congress entitled, “Social Risk Factors and Performance under Medicare’s Value-Based Purchasing Programs,” concluded that social factors and provider performance likely account for differences in hospital performance variation, but that evidence is limited and there is “clearly a need for more research in this area.”17
Our objective was to determine if a hospital effect contributes to CMS risk-standardized readmission risk, independent of patient factors. To isolate the effect of hospitals from unmeasured patient factors, we exploited the fact that many patients have multiple admissions for a similar diagnosis at more than 1 hospital within a given year. Accordingly, we identified patients admitted with the same diagnoses to hospitals in different quartiles of 30-day readmission performance within the same year and determined the difference in readmission rates for these patients across hospital quartiles with different risk-standardized readmission rates as measured by the CMS hospital-wide readmission measure.
METHODS
Data and Cohort
The hospital-wide readmission measure as reported by CMS Hospital Compare incorporates most of the hospital admissions. Qualifying hospitalizations included admissions for a broad range of medical, neurological, and surgical conditions, in contrast with the narrow cohorts for disease-specific readmission measures (e.g., heart failure or pneumonia).
To construct the overall study cohort, we applied the cohort definition of the CMS publicly reported, hospital-wide, 30-day readmission measure.6,10 Briefly, we included all discharges from July 1, 2014 through June 30, 2015 from short-term acute care or critical access hospitals in the US of patients who had Medicare Fee-for-Service insurance, were aged ≥65 years, and who were discharged alive and not against medical advice. We excluded patients admitted for medical treatment of cancer or primary psychiatric disease. In addition, we excluded patients without 1 year of pre-hospitalization enrollment in Medicare Fee-for-Service since previous claims are needed to identify comorbidities used in risk adjustment or without 1 month of post-discharge enrollment to capture all 30-day readmissions. We also excluded patients discharged from cancer hospitals exempt from Fee-for-Service. Multiple index admissions by the same patient could be included if each met eligibility criteria.
We obtained post-discharge mortality status from the Medicare Denominator File. We additionally used the 2015 American Hospital Association annual survey database to identify descriptive hospital characteristics.
Hospital Readmission Performance Classification
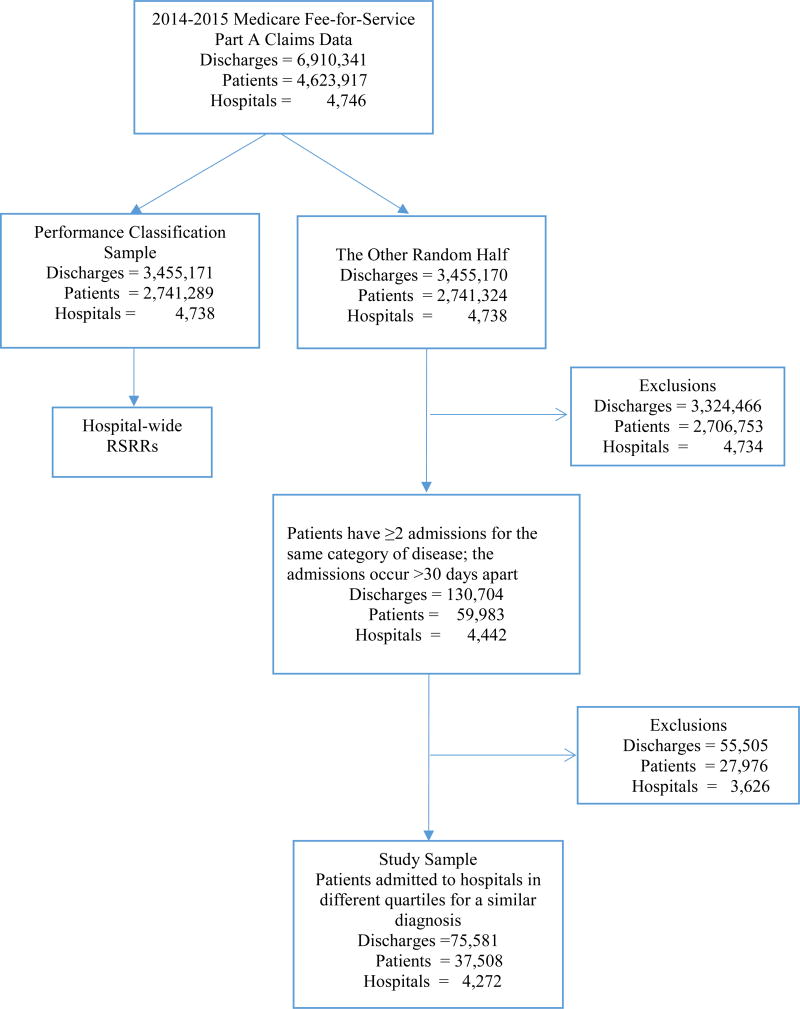
We randomly divided the discharges into 2 groups, which were stratified on hospital and principal diagnosis category (Figure 1). We used one half of the sample (the “performance classification sample”) to calculate hospital risk-standardized all-cause, unplanned readmission rates and classify the hospitals into quartiles of readmission performance. We calculated readmission performance using risk-standardized readmission rates in a manner consistent with the CMS publicly reported, hospital-wide, 30-day readmission measure.6,10,18 The classification of an unplanned readmission is based on the CMS measures.19 In brief, hospital-wide risk-standardized readmission rates are calculated as the ratio of the number of ‘predicted’ readmissions to the number of ‘expected’ readmissions, multiplied by the national observed readmission rate. Specifically, the hospital-wide readmission measure was computed within 5 specialty cohort levels, including surgical/gynecology, cardiovascular, cardiorespiratory, neurological, and medical hospitalizations. Five hierarchical logistic regression models were fitted to estimate the predicted and expected number of readmissions. The approach simultaneously modeled data at the patient and hospital levels to account for the variation in patient readmissions within and between hospitals. Hospitals were classified into quartiles based on their hospital-wide risk-standardized readmission rates from the performance specification sample.
Figure 1.
Flow diagram for the study cohort construction.
RSRR: Risk-standardized readmission rate
Hospital Comparisons
We used the other half of the sample to identify patients who had been admitted to hospitals in different quartiles of risk-standardized readmission rate performance for a similar diagnosis (i.e., within the same diagnostic category of the readmission measure). For these patients, we selected 1 or more pairs of hospitalizations, with 1 hospitalization in each of 2 or more quartiles. If a patient had more than 1 hospitalization in a given quartile, then 1 hospitalization was randomly selected. The result was a group of patients with 1 or more pairs of hospitalizations for similar diagnoses that occurred in hospitals that were in different readmission performance quartiles. The patients and hospitalizations in the quartile-pair comparisons constituted the study sample.
Statistical Analysis
First, we described the characteristics of the hospitals in the study sample by performance quartile. We reported risk-standardized readmission rates, teaching status, safety-net status, geographic location, urban/rural status, and bed size. Second, we described the patients in each of the quartile-pair comparisons (i.e., quartiles 1 versus 2; 2 versus 3; 3 versus 4; 1 versus 3; 2 versus 4; 1 versus 4). We reported age, race, sex, dual eligibility status, socioeconomic status, geographic location, and time between admissions. Dual beneficiaries were defined as individuals enrolled in both Medicaid and Medicare. Beneficiaries with low socioeconomic status were defined as those in the lowest quartile group of the socioeconomic status index score of the Agency for Healthcare Research and Quality, a composite measure of socioeconomic status that was calculated based on 7 measures from the census data.20 We also report the sequence of admissions to determine if there is an imbalance as to whether the individual went to the higher or lower quality hospital first. Third, for each performance quartile pair (i.e., quartile 1 vs. quartile 2; quartile 1 vs. quartile 3, etc.) we calculated the difference in the observed 30-day, unplanned all-cause readmission rates among patients contributing an admission pair to that quartile pair. To assess the significance of the difference between paired proportions, we calculated the 95% confidence interval using McNemar’s test. Our primary inference involved testing of 6 null hypotheses that for each of the 6 quartile pairs, readmission rates are equal in the 2 paired performing quartiles. To maintain a family-wise error rate of 0.05, we used a Bonferroni adjustment indicating that a statistical significance of 0.0083 would be required. We next compared the patients in the study sample with those who were excluded. To determine the similarity of the diagnoses at the most granular level, we compared the specific International Classification of Diseases, 9th Edition, Clinical Modification (ICD-9-CM) principal discharge diagnosis code for the admissions in each quartile. We identified the top-50 ICD-9-CM diagnosis codes in each quartile and summarized the differences in percentages of top-50 ICD-9-CM diagnosis codes for each quartile pair in histograms. Finally, we compared the admission characteristics for each hospitalization for each quartile pair to provide more information about the comparability of the admissions. We calculated the standardized difference in mean or proportion for each admission characteristic. We used SAS 9.4 (SAS Institute, Cary, NC) for analyses. We obtained institutional review board approval, including waiver of the requirement for participant informed consent, through the Yale University Human Investigation Committee.
RESULTS
Study Cohorts
The study cohort construction is shown in Figure 1. In the study period, there were 7,163,152 hospitalizations, of which 6,910,341 met inclusion criteria for the hospital-wide risk-standardized readmission measure. Of these, 3,455,171 discharges (2,741,289 patients and 4,738 hospitals) were randomly selected to calculate the hospital readmission performance. The second sample was comprised of 3,455,170 discharges in the study sample, of which 130,704 were patients who had 2 or more admissions for similar diagnoses at least 30 days apart. Compared with those excluded, this sample of 130,704 patients was slightly younger (77.5 years versus 78.4 years), more likely to be non-white (19.4% versus 14.1%), less likely to be female (55.8% versus 56.4%), more likely to have lower socioeconomic status (25.2% versus 20.5%), and more likely to be from the South region (42.0% versus 40.6%) (Table S1). Then, at the patient level, for those with multiple admissions to hospitals within a quartile, we randomly selected 1, leaving us with a final study sample that included 75,581 hospitalizations from 37,508 patients and 4,272 hospitals. There is an odd number of hospitalizations because a single hospitalization could be used in more than 1 quartile-pair comparison.
Hospital Readmission Performance Classification
Risk-standardized hospital-wide unplanned all-cause readmission rates were calculated for each institution in the performance classification cohort. The results of specialty cohort-level hierarchical logistic regression models are shown in Table S2. The mean was 15.6%, with a range of 11.7% to 19.6% and an interquartile range of 15.3% to 15.8%. The mean risk-standardized readmission rates for the 4 hospital quartiles were 15.0%, 15.4%, 15.7%, and 16.3% (Table S3). Hospital characteristics by quartile are shown in Table 1.
Table 1.
Characteristics of hospitals, overall and by quartile.
| Quartiles | |||||
|---|---|---|---|---|---|
|
|
|||||
| Study sample | Q1 (lowest) | Q2 | Q3 | Q4 (highest) | |
| Number of hospitals | 4272 | 1101 | 1009 | 1021 | 1141 |
| Risk-standardized readmission rate | |||||
| Mean (SD) | 15.6 (0.6) | 14.9 (0.4) | 15.4 (0.1) | 15.7 (0.1) | 16.3 (0.4) |
| Range | 11.7–19.6 | 11.7–15.3 | 15.3–15.5 | 15.5–15.8 | 15.8–19.6 |
| Median (IQR) | 15.6 (15.3–15.9) | 15.1 (14.8–15.2) | 15.4 (15.4–15.5) | 15.7 (15.6–15.7) | 16.2 (16.0–16.5) |
| Teaching status, n (%) | |||||
| Non-teaching | 2911 (69.6) | 700 (64.6) | 780 (79.3) | 768 (77.5) | 663 (58.8) |
| Teaching | 1273 (30.4) | 383 (35.4) | 203 (20.7) | 223 (22.5) | 464 (41.2) |
| Safety-net hospital, n (%) | |||||
| No | 3019 (72.2) | 864 (79.8) | 652 (66.3) | 670 (67.6) | 833 (73.9) |
| Yes | 1165 (27.8) | 219 (20.2) | 331 (33.7) | 321 (32.4) | 294 (26.1) |
| Geographic location, n (%) | |||||
| Midwest | 1189 (28.4) | 328 (30.3) | 336 (34.2) | 281 (28.4) | 244 (21.7) |
| Northeast | 545 (13.0) | 122 (11.3) | 74 (7.5) | 112 (11.3) | 237 (21.0) |
| South | 1620 (38.7) | 385 (35.5) | 358 (36.4) | 399 (40.3) | 478 (42.4) |
| West | 784 (18.7) | 247 (22.8) | 208 (21.2) | 179 (18.1) | 150 (13.3) |
| Others | 46 (1.1) | 1 (0.1) | 7 (0.7) | 20 (2.0) | 18 (1.6) |
| Core-based statistical area, n (%) | |||||
| Rural | 890 (21.3) | 127 (11.7) | 303 (30.8) | 307 (31.0) | 153 (13.6) |
| Urban | 3294 (78.7) | 956 (88.3) | 680 (69.2) | 684 (69.0) | 974 (86.4) |
| Hospital bed size, n (%) | |||||
| 1–199 beds | 2920 (69.8) | 696 (64.3) | 808 (82.2) | 787 (79.4) | 629 (55.8) |
| 200–299 beds | 510 (12.2) | 176 (16.3) | 80 (8.1) | 77 (7.8) | 177 (15.7) |
| 300–399 beds | 303 (7.2) | 87 (8.0) | 46 (4.7) | 51 (5.1) | 119 (10.6) |
| 400–499 beds | 173 (4.1) | 52 (4.8) | 18 (1.8) | 29 (2.9) | 74 (6.6) |
| ≥500 beds | 278 (6.6) | 72 (6.6) | 31 (3.2) | 47 (4.7) | 128 (11.4) |
Numbers of hospitals may not sum to total due to missing values (88 hospitals cannot be matched with American Hospital Association 2015 survey data); safety-net hospitals are defined as hospitals with an annual Medicaid caseload that was greater than 1 SD above their respective state’s mean private hospital Medicaid caseload;26 A Core Based Statistical Area (CBSA) is a U.S. geographic area defined by the Office of Management and Budget (OMB) that consists of 1 or more counties (or equivalents) anchored by an urban center of at least 10,000 people plus adjacent counties that are socioeconomically tied to the urban center by commuting;27 Quartiles are defined based on the performance classification sample; IQR, interquartile range; Q, quartile; SD, standard deviation
Main Findings
Among the patients who were hospitalized more than once for similar diagnoses at different hospitals that were classified into different performance quartiles, the observed readmission rate was significantly higher in patients admitted to the worst quartile compared with the best quartile (absolute readmission rate difference = 1.95 percentage points; 95% CI, 0.39% to 3.50%) (Table 2). The differences in the comparison of the other quartiles were smaller and not significant.
Table 2.
Difference in observed 30-day readmission rate (%) and 95% confidence interval and number of admissions of each quartile pair.
| Quartile pairs | Number of pairs | Observed 30-day readmission rate, % |
Difference in readmission rate, % |
95% confidence interval, % |
|
|---|---|---|---|---|---|
|
| |||||
| Lower quartile | Higher quartile | ||||
| Q12 | 5649 | 21.26 | 21.65 | 0.39 | (−1.53, 2.31) |
| Q23 | 3472 | 23.10 | 23.85 | 0.75 | (−1.81, 3.30) |
| Q34 | 8049 | 25.78 | 25.98 | 0.20 | (−1.51, 1.91) |
| Q13 | 5781 | 23.11 | 23.53 | 0.42 | (−1.56, 2.39) |
| Q24 | 6035 | 24.09 | 25.34 | 1.25 | (−0.71, 3.20) |
| Q14 | 9355 | 23.13 | 25.08 | 1.95 | (0.39, 3.50) |
Lower quartile and higher quartile represent the 2 groups of each quartile pair; Q, quartile-pair (e.g., Q12, quartile-pair comparison Q1 vs. Q2); the confidence interval for the difference in observed 30-day readmission rate is calculated using McNemar’s test with Bonferroni adjustment (statistical significance level was 0.05/6=0.0083).
Quartile Comparisons
The patient characteristics for the individuals in the quartile comparisons are reported in Table 3. The definition of the quartiles is derived from the performance specification cohort, but the patients and hospitalizations in the quartile comparisons are from a separate study sample. In the quartile comparisons, the median of days between paired admissions for the same patient was from 111 to 118 days. The sequence of the admissions was similar across hospital quartile comparisons, as the percentage of first admissions that occurred at the better performing quartile hospitals was 50.01% for the quartile 1–2 comparison; 48.59% for quartiles 2–3; 50.38% for quartiles 3–4; 48.45% for quartiles 1–3; 51.42% for quartiles 2–4; and 49.64% for quartiles 1–4. For the comparison that was significant, the higher readmission rate for the worst quartile was present in both sequences (Table S4). The principal discharge diagnoses (Table S5) and the patient characteristics (Table S6) that could have changed (e.g., comorbidities, admission source, age) between the quartiles for each quartile-comparison pair were not substantively different. In Figure S1, we summarized the differences in percentages of top-50 ICD-9-CM diagnosis codes for each quartile pair in histograms; the max (min) difference in percentages of top codes is −1.58% (1.03%).
Table 3.
Patient characteristics, overall and by paired quartiles.
| Paired quartiles | |||||||
|---|---|---|---|---|---|---|---|
|
|
|||||||
| Study sample | Q12 | Q23 | Q34 | Q13 | Q24 | Q14 | |
| Number of patients | 37,508 | 5649 | 3472 | 8049 | 5781 | 6035 | 9355 |
| Race, n (%) | |||||||
| White | 30,897 (82.4) | 4874 (86.3) | 2867 (82.6) | 6302 (78.3) | 4878 (84.4) | 4916 (81.5) | 7668 (82.0) |
| Non-white | 6611 (17.6) | 775 (13.7) | 605 (17.4) | 1747 (21.7) | 903 (15.6) | 1119 (18.5) | 1687 (18.0) |
| Gender, n (%) | |||||||
| Female | 20,884 (55.7) | 3187 (56.4) | 1880 (54.1) | 4574 (56.8) | 3208 (55.5) | 3388 (56.1) | 5127 (54.8) |
| Male | 16,624 (44.3) | 2462 (43.6) | 1592 (45.9) | 3475 (43.2) | 2573 (44.5) | 2647 (43.9) | 4228 (45.2) |
| Low socioeconomic status, n (%) | |||||||
| No | 28,191 (75.5) | 4445 (79.0) | 2563 (74.1) | 5791 (72.3) | 4379 (76.2) | 4411 (73.6) | 7145 (76.7) |
| Yes | 9126 (24.5) | 1179 (21.0) | 894 (25.9) | 2219 (27.7) | 1370 (23.8) | 1585 (26.4) | 2167 (23.3) |
| Region, n (%) | |||||||
| Midwest | 8604 (22.9) | 1608 (28.5) | 901 (26.0) | 1641 (20.4) | 1277 (22.1) | 1484 (24.6) | 1871 (20.0) |
| Northeast | 6083 (16.2) | 357 (6.3) | 315 (9.1) | 1852 (23.0) | 699 (12.1) | 941 (15.6) | 2020 (21.6) |
| South | 16,763 (44.7) | 2399 (42.5) | 1734 (49.9) | 3610 (44.9) | 2629 (45.5) | 2572 (42.6) | 4194 (44.8) |
| West | 5849 (15.6) | 1284 (22.7) | 516 (14.9) | 827 (10.3) | 1156 (20.0) | 1014 (16.8) | 1223 (13.1) |
| Other | 209 (0.6) | 1 (0.0) | 6 (0.2) | 119 (1.5) | 20 (0.3) | 24 (0.4) | 47 (0.5) |
| Time between paired admissions (days) | |||||||
| Median | NA | 118.0 | 113.0 | 111.0 | 114.0 | 112.0 | 113.0 |
| IQR | NA | 70.0–184.0 | 68.0–177.0 | 67.0–175.0 | 68.0–182.0 | 69.0–177.0 | 69.0–178.0 |
Number of patients may not sum to total due to missing values (191 patients in the study sample had missing values in the low socioeconomic status variable); NA: In the study sample, patients might have had >2 admissions; the time between paired admissions is not available; IQR, interquartile range; Q, quartile-pair (e.g., Q12, quartile-pair comparison Q1 vs. Q2); Beneficiaries with low socioeconomic status were defined as those in the lowest quartile group of the Agency for Healthcare Research and Quality socioeconomic status index score, a composite measure of socioeconomic status that was calculated based on 7 measures from the census data.20
DISCUSSION
In this study, when the same patients were admitted with similar diagnoses to multiple hospitals in the best and worst performance quartiles based on the CMS readmission measure, they experienced significantly higher rates of readmission after hospitalization at worse performing facilities. This study addresses a persistent concern that national readmission measures may reflect differences in unmeasured factors rather than hospital performance.16,21,22 The findings suggest that hospital quality contributes at least in part to readmission rates independent of patient factors. By studying individuals who are admitted twice within a year with similar diagnoses to different hospitals, this study design is able to isolate hospital signals of performance while minimizing differences among the patients used to estimate performance. In these cases, because the same patients have admissions at 2 hospitals, the patients, including their level of social disadvantage, level of education, or degree of underlying illness, are broadly the same. The alignment of the differences we observed with the CMS hospital-wide readmission measure results also adds to evidence that the readmission measure classifies true differences in performance.
There may be some factors that could change over time for individual patients. We sought to evaluate whether any of those factors, such as comorbidities, sequence of the admissions, and specific principal discharge diagnoses may have influenced the outcomes at the respective hospitals. We could find no evidence of systemic differences in factors that could have been different in the 2 hospitalizations. Moreover, we conducted the study so that hospitalizations used to characterize hospital readmission performance were not used in the evaluation of risk for patients who were admitted to hospitals categorized as having different levels of performance. This separation of the hospitalizations was intended to ensure independence of hospital performance evaluation and readmission risk determination for individual patients.
Of note, the study was not designed to determine whether particular patient factors currently not included in the measure are an important indicator of an individual’s risk of readmission. Several studies have indicated that sociodemographic characteristics are associated with readmission for at least some conditions at the patient level.23,24 The root cause of that risk deserves continued scrutiny and not all studies agree.25 Moreover, there is a difference between patient-level prediction and risk adjustment at the hospital level. Several studies indicate that adding information about social factors to the CMS readmission measures has little impact on the characterization of hospital performance.12–14,17
Nor was the study designed to determine the contribution of the hospital effect relative to other factors. Nevertheless, the magnitude of the difference in readmission risk among the same patients admitted to the best and worst quartile is similar to the difference in the risk-standardized readmission rates in the CMS measure. If unmeasured patient factors were confounding the assessment of readmission performance, we would expect the difference to be smaller than that reported by the public measures. The difference is actually larger than the mean risk-standardized readmission rate quartile differences from the performance specification sample, perhaps owing to the study sample being, overall, a higher risk group given that it comprised individuals who experienced at least 2 admissions within a year. An absolute difference of 2% may seem small relative to the overall readmission risk, but it indicates that for every 50 patients admitted to a hospital in the lowest performing, rather than highest performing, quartile, there is 1 additional readmission.
The study has several limitations. First, it focused on the subset of patients seen in more than 1 hospital with different readmission performance. These patients have a higher risk of readmission and have more comorbidities than the other patients. Nevertheless, they are an ideal population in which to test the validity of the readmission measures. In particular, the factors that could vary by hospitalization, i.e., the sequence of the admissions and the diagnoses, were quite comparable. Second, this study focused on hospital-wide readmission because of the larger sample it afforded rather than readmission performance for individual admitting conditions. Third, we did not evaluate particular hospitals, but rather groups of hospitals because paired admissions were infrequent among individual hospital pairs. We cannot exclude that there may be exceptions for certain individual hospitals. Fourth, the 2 admissions were matched for similar, but not exactly the same, diagnoses. Nevertheless, we did evaluate the specific principal diagnoses and admission characteristics and we did not detect an important difference (Figure S1 and Table S3). Finally, only the first and fourth quartiles had significant differences. However, given that each RSRR is associated with some uncertainty and the hospitals in closer quartiles likely have overlapping interval estimates, it is not surprising that there are not entirely consistent differences. Since these differences are not statistically different, what we observe may be a result of the play of chance among hospitals that are not so different in their true rates.
In conclusion, we report evidence that the same patients admitted to hospitals with different levels of readmission performance, as classified by risk-standardized readmission rates, have different risk of outcomes. This result should reassure the public, policymakers and health care professionals that the signal of quality from the hospital-wide readmission measure is valid and can be used as a means to benchmark performance. Moreover, there are opportunities for worse performing hospitals to improve their care and avert potentially preventable readmissions.
Supplementary Material
Acknowledgments
Support
Harlan Krumholz, Kun Wang, Zhenqiu Lin, Kumar Dharmarajan, Leora Horwitz, Joseph Ross, Elizabeth Drye, and Susannah Bernheim receive support from contracts with the Centers for Medicare & Medicaid Services (CMS) to develop and maintain performance measures that are used for public reporting. Susannah Bernheim, Leora Horwitz and Joseph Ross receive support (grant R01HS022882) from the Agency for Healthcare Research and Quality; Elizabeth Drye also receives support (contract 6081485-104939) from the Agency for Healthcare Research and Quality for the reevaluation of quality indicators.
Disclosures
Sharon-Lise Normand was involved in the creation of several CMS measures, including those discussed in this manuscript.
Harlan Krumholz and Joseph Ross have research agreements with Medtronic and Johnson & Johnson (Janssen), through Yale University, to develop methods of clinical trial data sharing, and a grant from Medtronic and the Food and Drug Administration, through Yale University, to develop methods for post-market surveillance of medical devices.
Harlan Krumholz chairs a cardiac scientific advisory board for UnitedHealth; is a participant/participant representative of the IBM Watson Health Life Sciences Board; is a member of the Advisory Boards of Element Science and Aetna; and is the founder of Hugo, a personal health information platform.
Joseph Ross receives support from the Food and Drug Administration to establish a Center for Excellence in Regulatory Science and Innovation at Yale and Mayo Clinic; from the Blue Cross-Blue Shield Association to better understand medical technology evaluation; and from the Laura and John Arnold Foundation to support the Collaboration on Research Integrity and Transparency at Yale.
Kumar Dharmarajan is a member of the Advisory Board and a consultant for Clover Health.
References
- 1.Hospital Readmission Reduction Program. Patient Protection and Affordable Care Act, 2124 Stat. 119 §3025. 2010 [Google Scholar]
- 2.Desai NR, Ross JS, Kwon JY, et al. Association between hospital penalty status under the Hospital Readmission Reduction Program and readmission rates for target and nontarget conditions. JAMA. 2016;316:2647–56. doi: 10.1001/jama.2016.18533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gerhardt G, Yemane A, Hickman P, et al. Medicare readmission rates showed meaningful decline in 2012. MMRR. 2013;3 doi: 10.5600/mmrr.003.02.b01. mmrr.003.02.b01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wasfy JH, Zigler CM, Choirat C, et al. Readmission rates after passage of the Hospital Readmissions Reduction Program: A pre-post analysis. Ann Intern Med. 2017;166:324–331. doi: 10.7326/M16-0185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zuckerman RB, Sheingold SH, Orav EJ, Ruhter J, Epstein AM. Readmissions, observation, and the Hospital Readmissions Reduction Program. N Engl J Med. 2016;374:1543–51. doi: 10.1056/NEJMsa1513024. [DOI] [PubMed] [Google Scholar]
- 6.Horwitz LI, Partovian C, Lin Z, et al. Development and use of an administrative claims measure for profiling hospital-wide performance on 30-day unplanned readmission. Ann Intern Med. 2014;161:S66–75. doi: 10.7326/M13-3000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Keenan PS, Normand SL, Lin Z, et al. An administrative claims measure suitable for profiling hospital performance on the basis of 30-day all-cause readmission rates among patients with heart failure. Circ Cardiovasc Qual Outcomes. 2008;1:29–37. doi: 10.1161/CIRCOUTCOMES.108.802686. [DOI] [PubMed] [Google Scholar]
- 8.Krumholz HM, Lin Z, Drye EE, et al. An administrative claims measure suitable for profiling hospital performance based on 30-day all-cause readmission rates among patients with acute myocardial infarction. Circ Cardiovasc Qual Outcomes. 2011;4:243–52. doi: 10.1161/CIRCOUTCOMES.110.957498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lindenauer PK, Normand SL, Drye EE, et al. Development, validation, and results of a measure of 30-day readmission following hospitalization for pneumonia. J Hosp Med. 2011;6:142–50. doi: 10.1002/jhm.890. [DOI] [PubMed] [Google Scholar]
- 10.Horwitz LI, Partovian C, Lin Z, et al. Hospital-wide all-cause unplanned readmission measure. [Accessed May 25, 2017];Final technical report. 2012 Jul; at: https://www.cms.gov/medicare/quality-initiatives-patient-assessment-instruments/hospitalqualityinits/measure-methodology.html.
- 11.American Hospital Association. The evolution of quality in Medicare Part A. [Accessed May 25, 2017];Statement of the American Hospital Association before the Subcommittee on Ways and Means of the US House of Representatives. 2016 Sep 7; at: http://www.aha.org/advocacy-issues/testimony/2016/160907-statement-postacute.pdf.
- 12.Bernheim SM, Parzynski CS, Horwitz L, et al. Accounting for patients' socioeconomic status does not change hospital readmission rates. Health Aff (Millwood) 2016;35:1461–70. doi: 10.1377/hlthaff.2015.0394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Blum AB, Egorova NN, Sosunov EA, et al. Impact of socioeconomic status measures on hospital profiling in New York City. Circ Cardiovasc Qual Outcomes. 2014;7:391–7. doi: 10.1161/CIRCOUTCOMES.113.000520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Glance LG, Kellermann AL, Osler TM, et al. Impact of risk adjustment for socioeconomic status on risk-adjusted surgical readmission rates. Ann Surg. 2016;263:698–704. doi: 10.1097/SLA.0000000000001363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Joynt KE, DeLew N, Sheingold SH, et al. Should Medicare value-based purchasing take social risk into account? N Engl J Med. 2017;376:510–3. doi: 10.1056/NEJMp1616278. [DOI] [PubMed] [Google Scholar]
- 16.Lipstein SH, Dunagan WC. The risks of not adjusting performance measures for sociodemographic factors. Ann Intern Med. 2014;161:594–6. doi: 10.7326/M14-1601. [DOI] [PubMed] [Google Scholar]
- 17.U.S. Department of Health and Human Services Office of the Assistant Secretary for Planning and Evaluation. A report required by the Improving Medicare Post-Acute Care Transformation (IMPACT) Act of 2014. Washington, DC: 2016. Report to Congress: Social risk factors and performance under Medicare's value-based purchasing programs. [Google Scholar]
- 18.Horwitz LI, Grady JN, Cohen DB, et al. Development and validation of an algorithm to identify planned readmissions from claims data. J Hosp Med. 2015;10:670–7. doi: 10.1002/jhm.2416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yale New Haven Health Services Corporation/Center for Outcomes Research and Evaluation. 2016 Measure Updates and Specification Report: Hospital-Wide All-Cause Risk-Standardized Readmission Measure–Version 5.0. 2016 [Google Scholar]
- 20.Bonito AJ, Bann C, Eicheldinger C, Carpenter L, RTI International Creating and validating an index of socioeconomic status. Creation of new race-ethnicity codes and socioeconomic status (SES) indicators for Medicare beneficiaries: Final report. 2008 Jan; AHRQ Publication Number 08-0029-EF. [Google Scholar]
- 21.Joynt KE, Jha AK. A path forward on Medicare readmissions. N Engl J Med. 2013;368:1175–7. doi: 10.1056/NEJMp1300122. [DOI] [PubMed] [Google Scholar]
- 22.Konstam MA, Upshaw J. Sisyphus and 30-day heart failure readmissions: Futility in predicting a flawed outcome metric. JACC Heart Fail. 2016;4:21–3. doi: 10.1016/j.jchf.2015.10.002. [DOI] [PubMed] [Google Scholar]
- 23.Rahimi AR, Spertus JA, Reid KJ, Bernheim SM, Krumholz HM. Financial barriers to health care and outcomes after acute myocardial infarction. JAMA. 2007;297:1063–72. doi: 10.1001/jama.297.10.1063. [DOI] [PubMed] [Google Scholar]
- 24.Rathore SS, Foody JM, Wang Y, et al. Race, quality of care, and outcomes of elderly patients hospitalized with heart failure. JAMA. 2003;289:2517–24. doi: 10.1001/jama.289.19.2517. [DOI] [PubMed] [Google Scholar]
- 25.Krumholz HM, Chaudhry SI, Spertus JA, et al. Do non-clinical factors improve prediction of readmission risk?: Results from the Tele-HF Study. JACC Heart Fail. 2016;4:12–20. doi: 10.1016/j.jchf.2015.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ross JS, Bernheim SM, Lin Z, et al. Based on key measures, care quality for Medicare enrollees at safety-net and non-safety-net hospitals was almost equal. Health Aff (Millwood) 2012;31:1739–48. doi: 10.1377/hlthaff.2011.1028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.US Census Bureau. 2010 Census Summary File 1: 2010 Census of Population and Housing, Technical Documentation. [Accessed May 25, 2017];2012 Sep;:619. at: https://www.census.gov/prod/cen2010/doc/sf1.pdf.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.