Abstract
Objective:
Substance use disorders are among the most common and costly health conditions affecting Americans. Despite estimates of national costs exceeding $400 billion annually, individual companies may not see how substance use impacts their bottom lines through lost productivity and absenteeism, turnover, health care expenses, disability, and workers’ compensation.
Methods:
Data on employed adults (18 years and older) from 3 years (2012 to 2014) of the National Survey on Drug Use and Health Public Use Data Files were analyzed.
Results:
The results offer employers an authoritative, free, epidemiologically grounded, and easy-to-use tool that gives specific information about how alcohol, prescription pain medication misuse, and illicit drug use is likely impacting workplaces like theirs.
Conclusion:
Employers have detailed reports of the cost of substance use that can be used to improve workplace policies and health benefits.
Risky use of alcohol, prescription pain medication misuse, and other drug use disorders are among the most common and costly health conditions affecting Americans [Substance use disorder (SUD) is a condition in which the use of one or more substances leads to a clinically significant impairment or distress. SUDs can include any psychoactive drug, for example, alcohol, prescription pain medications, heroin, cocaine, and marijuana.] The Surgeon General reports that in 2015, 66.7 million people in the United States reported drinking more than five drinks on one occasion at least once in the past month and 27.1 million adolescents and adults used illicit drugs or misused prescription drugs.1 The costs to the individuals and families are grave. Alcohol contributes to 88,000 deaths each year in the US; one in 10 deaths among working adults are alcohol-related.2 Added to that, in 2014, there were 47,055 drug overdose deaths: 28,647 of whom died from overdoses from prescription pain relievers or heroin.3
The cost of substance use to employers may not be as apparent. Despite estimates that the national bill for substance use annually is more than $400 billion,4,5 individual companies may not see how substance use impacts their bottom lines through lost productivity and absenteeism, turnover, health care expenses, disability, and workers’ compensation, and increased taxes to pay for law enforcement, criminal justice, and publicly supported medical treatment. Business leaders remain largely in the dark about how substance use impacts their companies and what they can do to reduce their risks and costs.6–8
The Real Costs of Substance Use in Your Workforce (https://www.nsc.org/forms/substance-use-employer-calculator/index.aspx) was designed to be an authoritative, epidemiologically grounded, and easy-to-use tool that provides employers with specific information about how alcohol, prescription pain medication misuse, and illicit drug use impacts their workplaces. It also provides research-proven steps employers can take to help employees and family members of their employees who have substance use problems and, at the same time, increase the safety, health, and productivity of their workforces. The new tool updates an earlier SUD Calculator introduced by this research team in 2003, and most recently refreshed in 2009 (www.alcoholcostcalculator.org, www.alcoholcostcalculator.org/sub). This paper describes the methods used and important results derived from the new tool.
METHODS
Sources of Data
Three years of data from the annual Federal substance use epidemiological survey, the National Survey on Drug Use and Health (NSDUH) 2012 to 2014 are the primary sources for the Calculator [Public use data (PUD) files of the NSDUH were analyzed online at http://pdas.samhsa.gov/#/?_k=m9xwxh.] The Substance Abuse and Mental Health Services Administration (SAMHSA) conducts the NSDUH. Each year, a nationally representative sample of approximately 67,500 persons ages 12 years and above is interviewed. PUD files are made available about 18 months after the annual survey results are released. The PUD files contain weighted, anonymized data from approximately 55,000 adolescents and adults. Questions include lifetime, annual, and past-month usage of alcohol, marijuana, cocaine, hallucinogens, heroin, inhalants, tobacco, pain relievers, tranquilizers, stimulants, and sedatives. The NSDUH survey also covers mental health and physical health symptoms, mental health and substance use treatment history, health care utilization, and health insurance coverage. Demographic data include gender, race, age, ethnicity, educational level, job status, workplace characteristics, and income. The research team separately analyzed the 2012 to 2014 NSDUH PUD and averaged the results. All respondents employed full- or part-time were included in analyses (25,201 in 2012; 25,235 in 2013; 27,030 in 2014). Respondents who did not report paid employment in the prior year were excluded from the analyses. The NSDUH survey is constructed so that Diagnostic and Statistical Manual of Mental Disorders IV diagnoses of SUDs can be derived.9 Nationally, 0.7% of working adults have a pain medication use disorder, 1.7% used a pain reliever nonmedically within the previous 30 days, 7.9% had an alcohol use disorder, 2.5% an illicit drug use disorder, and 1.7% a marijuana use disorder. Overall, 8.6% of adults had a SUD.
The Survey Documentation and Analysis (SDA, version 3.5) was the primary online software to analyze the NSDUH [SDA, an online analysis system was developed and is maintained by the Computer-assisted Survey Methods Program (CSM) at the University of California, Berkeley. SDA results are comparable to SAS, Stata, and SUDAAN. For more information on SDA 3.5: http://sda.berkeley.edu/document.htm.] The data and SDA are part of the Substance Abuse and Mental Health Data Archive maintained by the Inter-University Consortium for Political and Social Research at the University of Michigan and the SAMHDA Public-use Data Analysis System (PDAS; http://datafiles.samhsa.gov/info/analyze-public-data-nid6).
Adjusting Prevalence Estimates: States
There are substantial differences between states in the prevalence of prescription pain medication misuse and SUDs generally. SAMHSA pools several years’ NSDUH data to provide state estimates of substance use (SAMHSA does not report state-specific rates of opioid disorder but does provide state rates of prescription pain medication misuse in previous 30 days.)10,11 In order to account for these differences, the average prevalence of prescription pain medication misuse and SUDs for persons 18 years and older in each state 2012 to 2014 was divided into the national prevalence rate for this age group.
Among employed adults, the prevalence of any SUD, including alcohol use disorder, is 8.6% nationally, ranging from Utah and Tennessee at 7.4% of 18 year olds and above, to Washington, DC (13.4%), Rhode Island (10.8%), and Montana (10.0%). The national prevalence of prescription pain medication misuse in the past 12 months is 4.2%. At the higher end are Arizona (5.2%), Oklahoma (5.1%), Alabama (5.0%), and Oregon (5.0%). At the lower end are Wyoming (3.4%), Florida (3.4%), Maine (3.4%), and Vermont (3.34%).
Adjusting Prevalence Estimates: Industry Sector
Most people with SUDs work (Fig. 1). In the age group between 18 and 64 years, 75% of adults with a SUD are in the workforce. Similarly, 78% of adults with an alcohol use disorder are in the workforce. A smaller proportion of adults who report past month misuse of pain medications are in the workforce (68%), and still fewer who have a pain medication use disorder (60%). Adults with SUDs are about twice as likely to be unemployed (9% vs 5%). Two-thirds (67%) of workers with a SUD are male, a ratio that holds for alcohol, illicit drug, and pain medication use disorders. Workers with a SUD are more likely than their peers to be younger, have a lower family income, and less likely to be married (Table 1).
FIGURE 1.
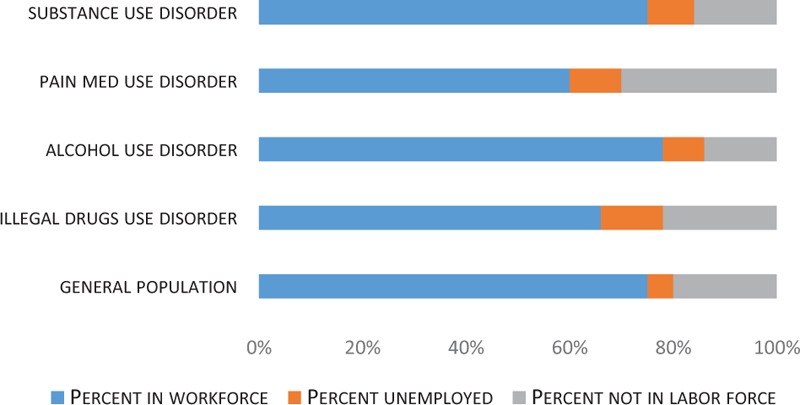
Workforce participation.
TABLE 1.
Demographics of Workers
| Overall US Workforce | Pain Med Use Disorder | Any Substance Use Disorder | |
| Male | 53% | 61% | 67% |
| Married | 54% | 28% | 33% |
| Between 18 and 34 years | 34% | 66% | 55% |
| Family income below $20K | 12% | 24% | 18% |
The NSDUH elicits information about employment status, industry sector, and occupation. Respondents are assigned to one of 14 industry sector based on their current job, and to one of 14 occupational categories. The proportion of NSDUH respondents who report working in specific industries mirrors rates reported by the Bureau of Labor Statistics (The only exceptions are in the categories education and health, which in 2014 composed 14% of the workforce and government, which composed 14%. The comparable NSDUH categories were 12% for education and health, and 5% for public administration. Discrepancies are likely a result of the NSDUH assigning some government worksites to education and health.)12Table 2 compares the proportion of the US workforce employed in 14 industry sectors per the Bureau of Labor Statistics and the corresponding percentage of NSDUH respondents in those industries in the 3 years sampled. The third column shows the total number of NSDUH respondents working in each industry in the 3 years sampled.
TABLE 2.
Industry Representation in the NDSUH
| BLS 2014 (%) | NSDUH (%) | Number in NSDUH | |
| Agriculture, forestry, fishing, and hunting | 1.4 | 1.4 | 1,254 |
| Mining | 0.6 | 0.6 | 605 |
| Construction | 4.1 | 7.5 | 15,357 |
| Manufacturing | 8.1 | 10.5 | 7,380 |
| Utilities and transportation | 3.5 | 5.0 | 3,032 |
| Information | 1.8 | 2.3 | 1,386 |
| Wholesale trade | 3.9 | 2.5 | 1,697 |
| Retail trade | 10.2 | 10.5 | 10,452 |
| Financial activities | 5.3 | 6.5 | 4,022 |
| Professional and business services | 12.7 | 11.9 | 8,214 |
| Educational services, health | 14.3 | 22.3 | 17,294 |
| Leisure and hospitality | 9.8 | 9.3 | 11,125 |
| Government, public administration | 14 | 4.6 | 3,118 |
| Other services | 4.2 | 5.6 | 4,193 |
Work Days Missed
The NSDUH asks respondents two questions about unscheduled leave in the previous 30 days. They are asked about whole days of work missed due to illness and injury. Respondents are also asked how many whole days they missed because they just did not want to be there (not including days missed because of a planned vacation or days missed for illness, injury or care for a sick child or other family member). Responses to these two questions are summed and annualized to measure the total number of missed workdays per year. Many employers provide sick leave or paid time off (PTO) that covers all forms of work absence (vacation, illness, etc). The unscheduled work days missed reported in this study may be covered by employers’ sick leave or PTO benefits. But these absences can be inconveniences and costs for employers who must still get the work done. They may need to hire substitutes or add to other workers’ duties. One study found that one in five workers reports being injured or put in danger on the job because of a coworker's drinking, or having to work harder, redo work, or cover for a coworker as a result of a fellow employee's drinking.13
Health Care Use
Respondents are asked about health care use in the prior 12 months: how many times they had gone to a hospital emergency room, whether they had been hospitalized overnight, and, if so, for how many nights, and the number of outpatient primary care visits. Respondents were also asked about past 12-month and lifetime substance use treatment.
Cost of Health Care
The Surgeon General's 2016 report “Facing Addiction in America” notes that the US spends roughly $35 billion per year to treat SUDs, and another $85 billion to treat the injuries, infections, and illnesses associated with risky and dependent substance use.14,15 If the payment of the combined $120 billion cost was spread evenly across the total US population in 2016, the result would be an annual cost of $370 for each person in the US.
However, those big numbers are difficult for employers to apply to their workforces. To more precisely estimate health care costs for individual employers who are associated with untreated SUDs in their workforce, we calculated from NSDUH the average hospital, emergency department, and ambulatory primary care use by workers with or with no current SUDs. Use by workers’ family members with a SUD was estimated from the overall prevalence of SUDs among NHSDUH respondents aged 12 to 65 years, and the health care use of those with and with no SUD in that age group. Utilization was then multiplied by the most recently available Federal government and health care industry data on average paid claims for hospital nights, ED, and ambulatory care visits. From the Healthcare Cost and Utilization Project (HCUP), average hospital paid claim per day in 2014 was $2553.16 The average emergency department visit cost $1863 in 2013 and ambulatory visit was $103 (Average expense in 2009 was $218.)17,18
Employers that offer health insurance to their employees cover, on average, 79% of individual workers’ premiums and 73% of family premiums (http://kff.org/state-category/health-costs-budgets/employer-based-health-insurance-premiums/). Employers’ costs were discounted by the percentage of employer's premium support for individual workers and for dependents.
Cost of Missed Work Days
For each industry sector, the average number of unscheduled work days missed by a worker with a SUD was compared with the average number of days missed by all workers in that sector. The direct costs of unscheduled leave was computed by multiplying those averages by the fully loaded daily wage data for each sector published by the US Bureau of Labor Statistics (The agricultural wage was derived from Fayer).19–21 The actual cost of unscheduled leave may significantly underestimate the true costs to employers who must cover missed work with substitute personnel.
Cost of Turnover, Replacement, and Other Problems
Substance use is associated with a number of hazardous and costly social consequences that can have negative impacts in the workplace that can be derived from NSDUH responses. Studies place the average cost to employers of recruiting and training replacement workers at 21% of an employee's annual fully loaded salary.22,23 Replacement and retraining costs are greater for workers with more education and training, and lower for workers paid less and with fewer skills. For the Calculator, employers’ turnover costs are computed from the difference in rates of 1-year turnover in each industry sector of workers with and without a SUD and the estimated costs of replacement in that sector (Replacement costs for each sector were figured at 21% of the average annual salary and fringe for that sector.)19
Substance use is associated with other problems that can impact employees’ productivity and safety that have not been monetized. These include inattention while at work (referred to as “presenteeism”), accidents and injuries associated with driving while intoxicated, and workplace and domestic violence.24,25
PRIOR SUBSTANCE USE TREATMENT AND RECOVERY
NSDUH asks detailed questions about prior substance use treatment. Self-reported prior treatment for an SUD among workers is uncommon: only 1.3% report receiving prior treatment. For the present study, we define workers in recovery as individual with no current or previous 12-month diagnosis of any alcohol or drug use disorder who report having received substance use treatment at some point in their lives.
RESULTS
Prevalence of Prescription Pain Medication, Alcohol, and SUDs by Industry Sector
Industries with younger, male-dominated workforces, and those that have easy access to alcohol have high rates of substance use and alcohol use disorders. Construction, entertainment, recreation, and food service businesses have nearly twice the rates of substance use and alcohol use disorders as the national average (15% compared with 8.6% nationally for SUDs, 12% compared with 7.5% nationally for alcohol use disorders). Pain medication misuse and pain medication use disorders follow a similar pattern, with two to three times higher rates of pain medication problems in these industries than the nation's workforce in general. By contrast, older and more female workforces in public administration, education, and health and social services experience about two-thirds the national rates of substance use (Table 3).
TABLE 3.
Rates of Substance Use Disorders by Industry
| Any SUD | Alcohol Use Disorder | Illicit Drug Use Disorder | Pain Med and Opioid Use Disorder | Marijuana Use Disorder | |
| Entertainment, recreation, food | 15.3 | 12.1 | 5.7 | 1.6 | 3.5 |
| Construction | 15.0 | 12.4 | 4.4 | 1.3 | 2.3 |
| Wholesale, nondurable | 10.6 | 9.4 | 2.4 | 0.7 | 1.2 |
| Professional, mgmt., admin | 10.3 | 8.6 | 2.7 | 0.9 | 1.6 |
| Mining | 10.3 | 9.6 | 1.0 | 1.0 | 0.1 |
| Retail | 9.8 | 7.9 | 3.3 | 0.9 | 2.1 |
| Information, communications | 9.7 | 8.2 | 2.3 | 0.6 | 1.4 |
| Finance, insurance real estate | 9.1 | 8.1 | 1.5 | 0.3 | 1.0 |
| Wholesale, durable | 8.7 | 8.1 | 1.3 | 0.4 | 0.9 |
| Other services except publ. admin | 8.7 | 7.1 | 2.5 | 1.0 | 1.6 |
| Agriculture | 8.6 | 7.5 | 1.7 | 0.4 | 1.2 |
| Manufacturing, durable | 8.4 | 7.5 | 1.5 | 0.8 | 0.6 |
| Manufacturing, nondurable | 8.0 | 6.7 | 2.1 | 0.6 | 1.1 |
| Transportation, utilities | 7.5 | 6.6 | 1.7 | 0.6 | 0.9 |
| Education, health, social services | 6.4 | 5.4 | 1.5 | 0.5 | 1.0 |
| Public administration | 5.7 | 5.0 | 0.9 | 0.5 | 0.5 |
| Overall average all industries | 9.4 | 7.9 | 2.5 | 0.8 | 1.5 |
Although alcohol is the primary contributor to overall rates of SUDs, the addictiveness and lethality of pain medication use disorders make this an important labor force concern. Generally, the industries with more alcohol use disorders in their labor forces have more illicit drug, pain medication, and marijuana use disorders. Industries with relatively low rates of alcohol use disorders have correspondingly low rates of other drug use disorders. The prevalence of pain medication and heroin use disorders is low among working adults, only 0.8% in 2012, 2013, and 2014. Entertainment, recreation, and food service stand out with double the national workforce average of opioid use disorders (1.6% vs 0.8%). Construction, mining, and other services have higher than average opioid use disorders. Marijuana use disorders are relatively uncommon within the labor force. Overall, 1.5% of employees have a marijuana use disorder, but again, workers in the entertainment, recreation, hospitality, and food service sector have rates much higher than average (3.5%), as do construction (2.3%) and retail (2.1%). Mining (0.1%), public administration (0.5%), and durable goods manufacturing (0.6%) have lower rates.
Workplace Absenteeism
Employees with SUDs miss substantially more work days than other employees (Table 4). The typical worker misses an average of 10.5 days annually for illness, injury, or reasons other than vacation and holidays. Workers with SUDs miss nearly 50% more days than their peers, averaging 14.8 days a year of unscheduled leave. Workers with pain medication use disorders miss nearly three times as much work as their peers, 29 days. Most of these extra days of missed work, more than 22 days annually, are associated with illness and injury. Workers in recovery, workers who report receiving substance use treatment at some time in the past and who have not had a SUD within the last 12 months, miss the fewest days of any group. They are less likely than even the general workforce to miss work days (9.5 days for workers in recovery and 10.5 days for other workers).
TABLE 4.
Workers in Recovery Have the Lowest Turnover and Absenteeism Rates
| General Work Force | Any SUD | Alcohol Use Disorder | Illicit Drug Use Disorder | Pain Med Use Disorder | Marijuana Use Disorder | In Recovery | |
| Missed work days for injury, illness past year | 8.4 | 10.2 | 9.4 | 13.0 | 22.2 | 10.6 | 8.3 |
| Missed work days for other reasons past year | 2.1 | 4.7 | 4.7 | 5.4 | 6.8 | 4.8 | 1.2 |
| Total missed work days past year | 10.5 | 14.8 | 14.1 | 18.4 | 29.0 | 15.4 | 9.5 |
| Worked for more than one employer in last year (%) | 25 | 36 | 36 | 42 | 42 | 45 | 23 |
Turnover and Replacement
Table 4 also summarizes differences in job turnover. One-fourth of currently employed workers report having more than one employer in the previous year. Employees with a SUD are much more likely than their peers to report having more than one employer: 36% among workers with any SUD. Workers with a prescription pain medication disorder were even more likely (42%) to have more than one employer. Workers in recovery are the group least likely to leave their employers. Their turnover rate is much lower than workers with untreated substance use, and even lower than their peers with no SUD (21% vs 25%).
Health Care Utilization
Although employees with any SUD report greater health care use than their peers, the big difference between groups, as summarized in Table 5, is that workers who have a pain medication use disorder use health care services much more than their peers. Workers in recovery use health care services at slightly lower rates than their peers and less than workers with an untreated SUD.
TABLE 5.
Health Care Use is Highest for People with a Pain Medication Use Disorder
| General Work Force | Any SUD | Alcohol Use Disorder | Illicit Drug Use Disorder | Pain Med Use Disorder | Marijuana Use Disorder | In Recovery | |
| Hospitalized overnight last year (%) | 7.4 | 7.9 | 7.9 | 9.5 | 17.0 | 8.1 | 7.3 |
| Hospital nights per person last year | 0.3 | 0.3 | 0.3 | 0.5 | 0.6 | 0.5 | 0.2 |
| Emergency room visits last year | 0.4 | 0.6 | 0.5 | 1.0 | 2.0 | 0.8 | 0.4 |
| Outpatient visits last year | 2.6 | 2.3 | 2.4 | 2.7 | 3.9 | 2.5 | 2.6 |
Hospital Use
People with pain medication use disorders are more than twice as likely as their peers to have been hospitalized in the previous 12 months and, when hospitalized, stay more than twice as long. No other substance-using group, including workers who misused pain medications, shows so great a difference in hospital use. Workers in recovery have the lowest hospital use of any group.
Patterns of hospital use of workers’ families are similar. People with a current or past-year SUD were more likely to be hospitalized and stay longer than either individuals with no current SUD or those in recovery. The average per person number of hospital nights in the previous year were 0.65 nights for individuals with a current SUD, 0.51 for individuals in recovery, and 0.34 nights for individuals with no SUD and no prior SUD treatment.
Emergency Room Use
Workers with pain medication use disorders use hospital emergency services (ED) an average of two visits annually, more than four times as often as workers with no SUDs, or as workers in recovery. Workers with an illicit drug use disorder or who misuse pain medications had twice the rate of ED use as their peers. Family members with an SUD also use more emergency services than individuals with no SUDs (0.81 visits and 0.55 visits, respectively), and more than individuals in recovery (0.77 visits).
Ambulatory Medical Care
Workers with a pain medication use disorder are outliers. They report an average of nearly four primary care visits annually. All other groups clustered around 2.5 visits annually. Family members in recovery used more outpatient services (3.2 annually) than the general population (2.8) or those with an SUD (2.7). Greater ambulatory care use by people in recovery may be associated with demographics. People in the general population who report prior substance use treatment but no current SUD are generally older. Only 10% are younger than 25 years, compared with 27% of people with no SUD and 35% of people with an SUD being under 25 years.
Comorbid Substance Use
Employees who have a SUD often are dependent on more than one drug. Four in 10 workers who had an illicit drug use disorder had comorbid alcohol use disorder. Sixty percent had a comorbid marijuana use disorder, and 28% had a pain medication use disorder. Similarly, 38% of employees with pain medication use disorders have alcohol use disorders, and 16% had marijuana use disorders. A similar pattern of comorbidity is seen among employees with marijuana use disorders. Alcohol use exhibits a different pattern: only 13% had an illicit drug use disorder, 3% were dependent on pain medications, and 8% were dependent on marijuana.
Serious Psychological Distress, Depression, and Anxiety
The NSDUH interview uses a six-item scale to measure respondents’ psychological distress in the prior 12 months. The symptoms assessed include feeling hopeless, feeling nervous, feeling restless or fidgety, feeling sad or depressed, feeling everything was an effort, and feeling worthless. Table 6 highlights the sharp difference between the general workforce and workers in recovery, on the one hand, and workers with current SUDs, especially workers with pain medication use disorders. Fewer than 4 in 100 workers in the general labor force report symptoms of serious psychological distress. Only 3 in 100 workers in recovery report serious distress. Although workers with any SUD and those with alcohol or illicit drug use disorder were more likely to report serious distress than their peers with no current SUD (12%, 11%, and 20%, respectively), it is workers with pain medication disorders who stand out. Workers with pain medication use disorders report serious distress seven times more frequently (28%) than peers without an SUD. A similar pattern, though not as extreme, can be seen in the prevalence of major depressive episodes and anxiety in the previous year. In the general workforce and among workers in recovery, rates of depression and anxiety are similarly low (between 5% and 7%). Among workers with SUDs, and especially among workers with pain medication use disorders, depression and anxiety are much more common. Anxiety and depression are twice as common among workers with any SUD, and four times more likely among those with a pain medication disorder.
TABLE 6.
Behavioral Health and Nicotine
| General Work Force | Any SUD | Alcohol Use Disorder | Illicit Drug Use Disorder | Pain Med Use Disorder | In Recovery | |
| Serious psychological distress past year (%) | 4 | 12 | 11 | 20 | 28 | 3 |
| Anxiety disorder past year (%) | 5 | 11 | 11 | 14 | 20 | 6 |
| Depression past year (%) | 6 | 11 | 11 | 15 | 22 | 7 |
| Percent cigarette use - past 30 days use (%) | 23 | 49 | 44 | 66 | 68 | 19 |
| Percent nicotine dependence past year (%) | 12 | 25 | 22 | 47 | 48 | 10 |
Smoking
Workers with SUDs are much more likely than their peers to smoke cigarettes and to be dependent on nicotine. Compared with their peers without an SUD, twice as many workers who have a SUD, and nearly three times as many workers with a pain medication disorder, marijuana, or illicit drug use disorder, reported smoking in the last 30 days. Twice as many employees with any SUD are dependent on nicotine than are their peers: 25% versus 12%, and nearly half of workers with an illicit drug use disorder or pain medication use disorder are nicotine dependent. Workers in recovery are much less likely to smoke or to be nicotine-dependent than workers with a SUD and have rates even lower than workers who have never had a SUD.
Driving Under the Influence
In 2014, driving while under the influence of alcohol or other drugs was a factor in the deaths of 9967 people, nearly one-third (31%) of all traffic-related fatalities in the U.S.26 The 1.3 million arrests for impaired driving every year may represent only about 1% of the actual alcohol and drug-impaired driving incidents.27–29 The National Highway Traffic Safety Administration (NHTSA) estimates that driving while under the influence of alcohol or drugs (DUI) costs the United States more than $44 billion each year in prosecution, higher insurance rates, higher taxes, medical claims, and property damage.30
Nearly two-thirds (64%) of workers with an alcohol use disorder report DUI at least once in the prior year. Similar high rates of impaired driving are seen among workers with a drug use disorder (61%), and with a pain medication use disorder (54%). In the general population of working adults, 16% report driving while under the influence at least once. Only 11% of workers in recovery reported DUI, the lowest rate of any group studied.
Costs of SUDs to Employers
Cost of Avoidable Health Care Use
Employers who self-insure and provide individual coverage pay $1729 per employee with no SUD each year (Fig. 2; Estimates of the costs of workers’ health care use from the NSDUH are likely to be lower than actual costs because the survey does not inquire about medications or laboratory tests, and 12-month recall may be imprecise.) A worker with an SUD uses health care services that cost his/her employer $2197. The difference is primarily a result of greater emergency department use by the latter. Workers with a pain medication use disorder cost more than twice that much as workers with no SUD: $5586. Emergency department use of workers with a pain medication disorder is four times that of workers with no SUDs and twice that of workers with any other SUD. These differences in health care use are likely reflections of greater illness and injury of workers with SUDs and especially among workers with pain medication disorders. The latter are twice as likely as their peers to report their health status to be fair or poor (14.1% vs 7.0%), and workers with any SUD are nearly half as likely to report fair or poor health (10%).
FIGURE 2.
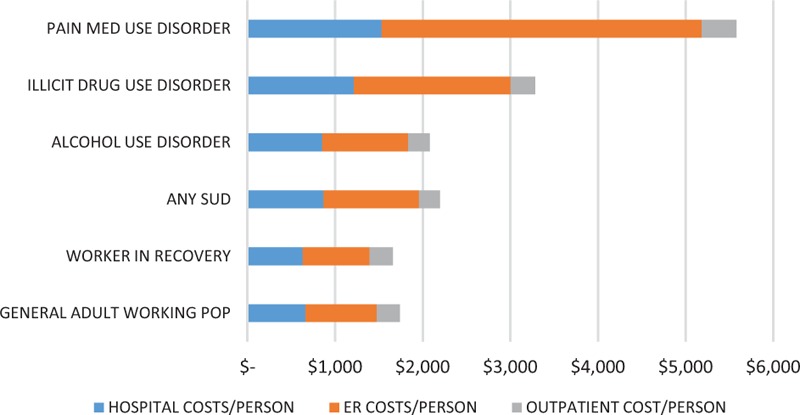
Employers’ per capita health care costs.
Health care costs of workers in recovery are nearly identical with those of workers with no current or past substance use conditions. On the basis of self-reported use, workers in recovery had an average annual cost $91 per year less than their peers who have never had a SUD. The pattern of health care costs of family members are similar to those of workers. Annual hospital, emergency, and outpatient costs for a person with an SUD were $3440, for a person in recovery, $3071, and for an individual with no SUD, $2173. The calculator produces estimates of employers’ costs of health care by multiplying the number of the firm's employees by state and industry sector SUD prevalence rates, the difference in health care use by workers with SUDs and family members with SUDs, published national averages of per day and per visit paid claims amounts,16,31,32 and the national average proportion of individual and family health care premiums generally paid by employers.
Cost of Missed Work
Table 7 illustrates by industry the per capita costs associated with the extra days of unscheduled leave used by workers with any SUD and by workers with a pain medication use disorder. Actual costs for an individual employer of unscheduled leave will vary based on employee wages and fringe, PTO policies, work duties, and substitution costs. The calculator produces estimates of employers’ costs of missed work by multiplying the number of employees by state and industry sector SUD prevalence rates, the difference in the number of work days missed annually, and that industry sector's fully loaded daily wage from the August 2016 Bureau of Labor Statistics.
TABLE 7.
Extra Costs of Missed Work by Industry
| Per Capita Annual Extra Cost of a with an SUD, $ | Per Capita Annual Extra Cost for a Worker with a Pain Medication Use Disorder, $ | Per Capita Annual Costs Avoided for Each Worker in Recovery ($) | |
| Agriculture | $187 | $1,668 | $90 |
| Mining | $881 | $(764) | $422 |
| Construction | $1,040 | $455 | $499 |
| Manufacturing: Durable goods | $1,399 | $14,830 | $671 |
| Manufacturing nondurable goods | $1,692 | $1,677 | $812 |
| Transportation and warehousing | $383 | $3,125 | $184 |
| Information, communications | $3,941 | $27,173 | $1,891 |
| Wholesale durable | $(893) | $2,468 | $(428) |
| Wholesale nondurable | $886 | $2,463 | $425 |
| Retail trade | $1,284 | $225 | $616 |
| Finance, insurance, real estate | $1,169 | $2,373 | $561 |
| Professional, mgmt., admin | $2,604 | $6,057 | $1,250 |
| Education, health, social services | $887 | $5,062 | $425 |
| Entertainment, recreation, food | $795 | $2,490 | $381 |
| Public administration | $1,406 | $(162) | $674 |
| Other services | $945 | $2,417 | $453 |
Negative numbers are likely associated with small numbers of workers in some categories. Mining represents 0.6% of the NSDUH employed respondents, so a small number of workers with an SUD in that sector with unusually high or low absenteeism may skew responses.
Turnover Costs
Replacing workers is expensive, averaging around 21% of the job's annual salary to recruit and retrain for a vacant position.33,34 Costs are greater for workers with greater education and training, and lower for workers paid less and with fewer skills. From the NSDUH interviews, about one in four currently employed adults had more than one employer in the previous 12 months. In some industries, for example, in entertainment, lodging, hospitality, and food service, turnover is greater (36% per year). In others, such as public administration, turnover is less common (18%). Workers with an untreated SUD had much higher rates of turnover. In entertainment, lodging, hospitality, and food service, nearly half (49%) of workers had more than one employer in the prior year. Other sectors also had high turnover rates among workers with SUDs: mining (41%), information and communication (43%), and other services (44%). This sector comprises establishments, not classified to any other sector, primarily engaged in repairing, or performing general or routine maintenance, on motor vehicles, machinery, equipment and other products to ensure that they work efficiently; providing personal care services, funeral services, laundry services and other services to individuals, such as pet care services and photo finishing services; organizing and promoting religious activities; supporting various causes through grant-making, advocating (promoting) various social and political causes, and promoting and defending the interests of their members. Table 8 summarizes the percentage of workers who had more than one employer in the past year. The column on the far right of Table 8 shows the extra costs employers bear for turnover and replacement for each employee with an untreated SUD. In sectors with high average salaries, such as information and communications, and higher than average turnover risk by employees with untreated SUDs, replacement costs are considerably higher than average: more than $4000 for each worker with an untreated SUD. The lower industry wages and smaller turnover differential between the general workforce and workers with a SUD in sectors such as agriculture result in smaller turnover costs per worker with an untreated SUD.
TABLE 8.
Turnover Costs
| Average Sector Turnover rate (%) | Turnover Rate for Workers with SUDs (%) | Workers in Recovery (%) | Per Capita Turnover Costa ($) | Per Capita Turnover Cost if Any SUD | Per Capita Excess Turnover Cost if SUD | Per Capita Savings of Worker in Recovery | |
| Agriculture | 20 | 27 | 20 | $1,535 | $2,046 | $512 | $537 |
| Mining | 27 | 41 | 27 | $5,044 | $7,597 | $2,553 | $2,491 |
| Construction | 27 | 32 | 26 | $4,440 | $5,317 | $877 | $987 |
| Manufacturing, nondurable | 19 | 32 | 19 | $3,085 | $5,052 | $1,968 | $2,074 |
| Manufacturing, durable | 19 | 28 | 18 | $2,601 | $3,947 | $1,347 | $1,393 |
| Transportation, utilities | 21 | 31 | 21 | $2,871 | $4,284 | $1,413 | $1,413 |
| Information, communications | 24 | 43 | 23 | $5,068 | $9,137 | $4,069 | $4,140 |
| Wholesale, durable | 21 | 34 | 21 | $3,681 | $5,924 | $2,243 | $2,301 |
| Wholesale, nondurable | 20 | 26 | 21 | $2,125 | $2,682 | $557 | $488 |
| Retail | 26 | 39 | 26 | $2,682 | $4,075 | $1,393 | $1,393 |
| Finance, insurance real estate | 21 | 28 | 20 | $3,974 | $5,299 | $1,325 | $1,451 |
| Professional, mgmt., admin | 25 | 32 | 25 | $4,506 | $5,767 | $1,262 | $1,322 |
| Education, health, social services | 25 | 36 | 25 | $3,762 | $5,417 | $1,655 | $1,655 |
| Entertainment, recreation, food | 36 | 49 | 36 | $3,167 | $4,271 | $1,104 | $1,133 |
| Public administration | 18 | 25 | 18 | $2,759 | $3,711 | $953 | $953 |
| Other services except publ. admin | 26 | 44 | 27 | $3,490 | $5,862 | $2,372 | $2,282 |
aAverage turnover, recruitment, replacement, and training costs estimated at 21.4% of annual salary.
Overall Costs of Untreated SUDs
Employers’ costs for untreated SUDs are substantial. Table 9 summarizes the percentage of each sector's workforce that has an untreated SUD, and the average per capita cost to an employer for each employee who has an SUD. The per capita cost is the sum of employers’ costs for avoidable health care use, absenteeism, and turnover of a worker with an untreated SUD in each industry sector. Information and communications, and professional services employers bear the highest costs. But other sectors with higher than average rates of SUDs in their workforces, such as construction and entertainment, lodging, hospitality, and food service, are exposed to significant costs because SUDs are so common. Greater use of health care by a family member who has an untreated SUD adds an extra $1267 per person annually to the cost of coverage for employers who support a portion of family health insurance premiums (http://kff.org/state-category/health-costs-budgets/employer-based-health-insurance-premiums/).
TABLE 9.
Per Capita Costs to Employers for Each Untreated Worker with an SUD
| Prevalence of SUD (%) | Excess Cost for Each Employee With an SUD ($) | |
| Agriculture | 8.6 | $2,689 |
| Mining | 10.3 | $8,934 |
| Construction | 15.0 | $6,813 |
| Manufacturing, nondurable | 8.0 | $6,907 |
| Manufacturing, durable | 8.4 | $6,096 |
| Transportation, utilities | 7.5 | $5,123 |
| Information, communications | 9.7 | $13,534 |
| Wholesale, durable | 7.4 | $5,487 |
| Wholesale, nondurable | 10.6 | $4,024 |
| Retail | 9.8 | $5,815 |
| Finance, insurance real estate | 9.1 | $6,925 |
| Professional, mgmt., admin | 10.3 | $8,827 |
| Education, health, social services | 6.4 | $6,760 |
| Entertainment, recreation, food | 15.3 | $5,523 |
| Public administration | 5.7 | $5,573 |
| Other services except publ. admin | 8.7 | $7,264 |
| Overall average | 9.4 | $6,643 |
COST AVOIDANCE WHEN WORKERS RECEIVE TREATMENT AND RECOVER FROM ADDICTION
Across the three NSDUH surveys, 7988 currently employed adults (10.3% of the 77,466 working adults in the 3-year NSDUH sample) report receiving substance use treatment at some time in their lives and did not have a SUD at any time in the prior 12 months. From these respondents, it is possible to estimate the costs employers avoid for each worker who receive treatment and recovers.
Health care utilization and costs are lower for workers in recovery than for workers with an untreated SUD, by an average of $536 per year. A family member in recovery costs employers $262 less in health care claims than a family member with an untreated SUD.
Workers in recovery stay with one employer at nearly identical rates as other workers in that sector (Table 8). Compared with the costs of turnover and replacement of workers with a SUD, workers in recovery save employers a substantial amount in every sector. Savings range from more than $4000 for each worker in recovery in information and communications to a little over $500 in agriculture.
Workers in recovery take much less unscheduled leave than their peers with untreated SUDs. In fact, they take even fewer days of unscheduled leave than workers in their industry who have never had a SUD. They miss work a week less than workers with an SUD, and a day less than workers who have never had a SUD. Table 7 summarizes the per capita costs employers avoid from the lower absence rates of a worker in recovery. Note that among employees in recovery in the durable wholesale goods sector, the cost of unscheduled leave is greater than costs of employees with an untreated SUD. The reason for this discrepancy is not apparent from the data.
Employers can avoid a significant amount of unnecessary and unproductive costs if they can assist their employees to receive treatment and recover from their SUDs. Table 10 summarizes that the average costs employers avoid annually for each employee who recovers from an SUD is more than $3200. For some industries, the savings are significantly higher: more than $8400 for each employee in recovery in information and communications industries, and more than $4300 in professional, management, and administrative industries.
TABLE 10.
Employer Costs Avoided for Each Worker in Recovery
| Industry Sector | Savings Per Worker in Recovery |
| Agriculture | $1,155 |
| Mining | $3,890 |
| Construction | $2,373 |
| Manufacturing, nondurable | $3,823 |
| Manufacturing, durable | $3,495 |
| Transportation, utilities | $2,252 |
| Information, communications | $8,466 |
| Wholesale, durable | $1,806 |
| Wholesale, nondurable | $1,900 |
| Retail | $3,134 |
| Finance, insurance real estate | $2,950 |
| Professional, mgmt., admin | $4,322 |
| Education, health, social services | $2,998 |
| Entertainment, recreation, food | $2,356 |
| Public administration | $2,815 |
| Other services except publ. admin | $3,773 |
| Overall average all occupations | $3,219 |
DISCUSSION
Seventy-five percent of adults experiencing an untreated SUD are in the workforce. Few business leaders are aware of the avoidable costs that treatment and recovery from addiction can generate. Employers remain largely in the dark about how substance use—and in particular, prescription drug misuse—impacts their companies and how to reduce their risks and costs. The analyses reported here and the free online tool, The Real Cost of Substance Use in Your Workforce (https://forms.nsc.org/substance-use-employer-calculator/index.aspx), can help individual companies understand how untreated substance use in their workforce can lead to unscheduled leave or missed work, job turnover, and extra health care costs. The annual cost of a single employee with an untreated SUDs ranges from $2600 in agriculture to more than $13,000 in the information and communications sectors.
The prevalence and costs of substance use vary by industry. Four industries—construction, entertainment, recreation, and food service—have twice the national average of employees with untreated SUDs. Industries that have higher proportions of workers with alcohol use disorders also have more workers with illicit drug, pain medication, and marijuana use disorders. Costs for each employee with an untreated SUD are greater in industries with highly skilled or highly compensated employees, such as the information or communications industries, even though the prevalence of SUDs in their workforces may be lower than, for example, construction or mining. To use the Calculator, employers simply input basic information into the online tool: industry sector, worksite location, and number of employees. The online calculator combines that information with prevalence and cost data from the NSDUH to produce an immediate report showing the likely number of their employees and their family members who have any type of SUD, and with specific types of SUDs (alcohol, marijuana, prescription pain, illicit drug). The report shows how much and where untreated SUDs are costing them, and potential costs avoided if their employees and family members get treatment.
Investing in helping workers get effective substance use treatment can, on average, avoid $3200 in costs annually for each worker who recovers. Workers in recovery who have received specialized substance use treatment and who have been in recovery for more than a year are less likely to miss work. They miss 5 days fewer than workers with a SUD and 1 day less than the general workforce. Workers in recovery also have lower turnover rates, are less likely to be hospitalized, and have fewer doctor's visits.
LIMITATIONS
Study findings should be interpreted in the context of several limitations. First, the NSDUH is based on respondent self-report. Self-report is easy to implement, affordable, and provides immediate results. It is thus relied upon for national public health surveys.35 However, the validity of self-report as a screening method for stigmatized health behaviors is complex.36,37 Self-report of substance use was not validated with a urine or blood test. Social desirability bias, patient characteristics, interview setting, population, interviewer traits, and sensitivity of subject matter can influence the validity of self-report.38,39 The NSDUH attempts to reduce these biases by administering most questions with audio computer-assisted self-interviewing (ACASI) to provide the respondent with a highly private and confidential mode for responding to questions in order to increase the level of honest responses to questions about illicit drug use and other sensitive behaviors. Less sensitive items are administered by interviewers using computer-assisted personal interviewing (CAPI). Reports on results from NSDUH data are available on the SAMHSA web site (http://www.samhsa.gov/data/NSDUH.aspx).40 But, studies have demonstrated that subjects often under-report substance use, based on perceived stigma associated with use.41 Thus, estimates derived from this as well as previous studies may be considered conservative. Second, the NSDUH is a cross-sectional study. We are unable to assess any causal relationships between substance use and work status or performance. A third limitation is that NSDUH data for 2012, 2013, and 2014 were pooled to increase the analytic sample size. As such, the prevalence estimates for alcohol and drug use may not account for possible time trends and cohort effects from different survey years. Of particular concern is the very rapid increase in opioid deaths in the last few years, which may represent increases in the prevalence of prescription opioid, heroin, and fentanyl use too recent to be picked up in our sample.42 However, the self-reported prevalence of pain medication use disorders among working adults was flat across the 3 years (0.7%; 0.7%; and 0.6%) as were self-reported last month misuse of pain medications (2.0%; 1.6%; 1.6%). Finally, the NSDUH does not ask questions about some key interpersonal (eg, temperament and personality), contextual (eg, neighborhood and worksite), or work-performance (presenteeism, job stress, and conflict) factors that may be of relevance to interpreting the impact of alcohol and drug use on employment.
CONCLUSION
Despite these limitations, this study contributes understanding the occupational impact of substance use by presenting a simple estimate of the financial toll faced by individual businesses, illuminating an area with significant potential for cost reduction and improved productivity. It provides employers tools to identify opportunities for health and productivity savings while also improving the health of employees and their families. Most importantly, it demonstrates the significant costs that employers can avoid if their employee gets treated for their SUDs.
Footnotes
Funding for this study was provided by a contract from the National Safety Council. All sources of support were provided by National Safety Council, Shatterproof.
Saira Huq, MPH, and Danielle Noriega, BA, of NORC, and Christopher Sanew, MFA, Zachary Davis, MBA, and Matt Bohlman, BA, of the National Safety Council contributed valuable analytic, editorial, and data visualization expertise throughout the project.
The authors have no conflicts of interest.
REFERENCES
- 1.Murthy VH. Facing Addiction in America: Surgeon General's Report on Alcohol, Drugs, and Health. Available at: https://addiction.surgeongeneral.gov/surgeon-generals-report.pdf Accessed September 4, 2017. [DOI] [PubMed] [Google Scholar]
- 2.Stahre M, Roeber J, Kanny D, Brewer RD, Zhang X. Contribution of excessive alcohol consumption to deaths and years of potential life lost in the United States. Prev Chronic Dis 2014; 11:E109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rudd RA, Aleshire N, Zibbel JE, Gladden RM. Increases in drug and opioid overdose deaths—United States, 2000–2014. MMWR Morb Mortal Wkly Rep 2016; 64:1378–1382. [DOI] [PubMed] [Google Scholar]
- 4.Sacks J, Gonzales KR, Bouchery EE, Tomedi LE, Brewer RD. 2010 national and state costs of excessive alcohol consumption. Am J Prev Med 2015; 49:e73–e79. [DOI] [PubMed] [Google Scholar]
- 5.National Drug Intelligence Center. National Drug Threat Assessment. Washington, DC: U.S. Department of Justice; 2011. [Google Scholar]
- 6.Harwood HJ, Reichman MB. The cost to employers of employee alcohol abuse: a review of the literature in the United States of America. United Nations Office on Drugs and Crime. Bull Narcotics 2000. [Google Scholar]
- 7.Harwood HJ, Malhotra D, Villarivera C, et al. Cost Effectiveness and Cost Benefit Analysis of Substance Abuse Treatment: An Annotated Bibliography. U.S. Department of Health and Human Services. Substance Abuse and Mental Health Services Administration. Center for Substance Abuse Treatment; 2002. [Google Scholar]
- 8.Holder HD, Lennox RD, Blose JO. The economic benefits of alcoholism treatment: a summary of twenty years of research. J Employee Assist Res 1992; 1:63–82. [Google Scholar]
- 9.Center for Behavioral Health Statistics Quality. Impact of the DSM-IV to DSM-5 Changes on the National Survey on Drug Use and Health. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2016. [PubMed] [Google Scholar]
- 10.Substance Abuse and Mental Health Services Administration. Behavioral Health Barometer: United States, 2014. HHS Publication No. SMA-15-4895. Rockville, MD: SAMHSA; 2015. [PubMed] [Google Scholar]
- 11.Substance Abuse and Mental Health Services Administration. National Survey on Drug Use and Health: Comparison of 2012–2013 and 2013–2014 Population Percentages (50 States and the District of Columbia). 2015. Available at: http://www.samhsa.gov/data/sites/default/files/NSDUHsaeShortTermCHG2014/NSDUHsaeShortTermCHG2014.htm Accessed September 4, 2017. [Google Scholar]
- 12.Henderson R. Industry employment and output projections to 2024. Monthly Lab Rev 2015; 138:1. [Google Scholar]
- 13.Mangione TW, Howland J, Lee M. New Perspectives for Worksite Alcohol Strategies: Results from a Corporate Drinking Study. 1998; Boston, MA: JSI Research and Training Institute, Available at: http://www.rwjf.org/files/publications/books/1999/chapter_04.html. Accessed September 4, 2017. [Google Scholar]
- 14.Murthy VH. Facing Addiction in America: Surgeon General's Report on Alcohol, Drugs, and Health. 2016. Substance Abuse and Mental Health Services Administration. Behavioral Health Spending and Use Accounts, 1986–2014. HHS Publication No. SMA-16-4975. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2016. Available at: https://addiction.surgeongeneral.gov/surgeon-generals-report.pdf Accessed September 4, 2017. [Google Scholar]
- 15.Levit K, Kassed C, Coffey R, Mark T, McKusick D, King E, Stranges E. Projections of National Expenditures for Mental Health Services and Substance Abuse Treatment, 2004–2014. (SAMHSA Publication No. SMA 08-4326). Rockville, MD: SAMHSA; 2008. [Google Scholar]
- 16.HCUPnet, Healthcare Cost and Utilization Project (HCUP). Hospital Charges and Costs. Available at: http://hcupnet.ahrq.gov/HCUPnet.jsp?Id=54D6E094A91AF8EC&Form=DispTab&JS=Y&Action=Accept Accessed September 4, 2017. [Google Scholar]
- 17.Agency for Healthcare Research and Quality. Emergency Room Services-Mean and Median Expenses per Person With Expense and Distribution of Expenses by Source of Payment: United States, 2014. Medical Expenditure Panel Survey Household Component Data. Generated interactively. Available at: https://meps.ahrq.gov/data_stats/tables_compendia_hh_interactive.jsp?_SERVICE=MEPSSocket0&_PROGRAM=MEPSPGM.TC.SAS&File=HCFY2014&Table=HCFY2014_PLEXP_E&VAR1=AGE&VAR2=SEX&VAR3=RACETH5C&VAR4=INSURCOV&VAR5=POVCAT14&VAR6=REGION&VAR7=HEALTH&VARO1=4+17+44+64&VARO2=1&VARO3=1&VARO4=1&VARO5=1&VARO6=1&VARO7=1&_Debug=) Accessed September 4, 2017. [Google Scholar]
- 18.Davis K, Carper K. Use and Expenses for Office-Based Physician Visits by Specialty, 2009: Estimates for the US Civilian Noninstitutionalized Population. Rockville, MD: Agency for Healthcare Research and Quality, Statistical Brief; 2012 Aug. 381. [Google Scholar]
- 19.Bureau of Labor Statistics Economic News Release: Table B-3 Average Hourly and Weekly Earnings of all Employees on Private Nonfarm Payrolls by Industry Sector, Seasonally Adjusted. Available at: http://www.bls.gov/news.release/empsit.t19.htm Accessed September 4, 2017. [Google Scholar]
- 20.Bureau of Labor Statistics Economic News Release. Table 6. Employer Costs per Hour Worked for Employee Compensation and Costs as a Percent of Total Compensation: Private Industry Workers, by Major Industry Group, June 2016. Available at: http://www.bls.gov/news.release/ecec.t06.htm Accessed September 4, 2017. [Google Scholar]
- 21.Fayer SD. Agriculture: occupational employment and wages. Monthly Lab Rev 2014; 137:1. Available at: http://www.bls.gov/opub/mlr/2014/article/agriculture-occupational-employment-and-wages.htm Accessed September 4, 2017. [Google Scholar]
- 22.Boushey H, Glynn S. There are Significant Business Costs to Replacing Employees. Center for American Progress. 2012. Available at: https://cdn.americanprogress.org/wp-content/uploads/2012/11/16084443/CostofTurnover0815.pdf Accessed December 9, 2016. [Google Scholar]
- 23.Tracey JB, Hinkin TR. Contextual factors and cost profiles associated with employee turnover. Cornell Hosp Quart 2008; 49:12–27. [Google Scholar]
- 24.Chestnut Global Partners, EAPs Can and Do Achieve Positive Outcomes: Workplace Outcome Suite Annual Report 2016. 2016. Available at: http://www.eapassn.org Accessed September 4, 2017. [Google Scholar]
- 25.Richmond M, Pampel F, Wood R, Nunes A. Impact of Employee Assistance Services on Depression, Anxiety, and Risky Alcohol Use: A Quasi Experimental Study. J Occ Env Med 2016; 58:641–650. [DOI] [PubMed] [Google Scholar]
- 26.Department of Transportation, National Highway Traffic Safety Administration. Traffic Safety Facts 2014 Data: Alcohol-Impaired Driving. Washington, DC: NHTSA; 2015. [Google Scholar]
- 27.National Highway Traffic Safety Administration. Traffic Safety Facts 2014 Data: Alcohol Impaired Driving (DOT HS 812 231). Washington, DC: U.S. Department of Transportation; 2015. [Google Scholar]
- 28.Compton R, Berning A. Drug and Alcohol Crash Risk (DOT HS 812 117). Washington, DC: National Highway Traffic Safety Administration; 2015. [Google Scholar]
- 29.Federal Bureau of Investigation. Estimated Number of Arrests: United States, 2012 Crime in the United States 2012: Uniform Crime Reports. 2012. Available at: https://ucr.fbi.gov/crime-in-the-u.s/2012/crime-in-the-u.s.-2012/persons-arrested/persons-arrested Accessed September 4, 2017. [Google Scholar]
- 30.Blincoe L, Miller T, Zaloshnja E, Lawrence B. The Economic and Societal Impact of Motor Vehicle Crashes, 2010 (Revised). (DOT HS 812 013). Washington, DC: National Highway Traffic Safety Administration; 2015. [Google Scholar]
- 31.Emergency Department Visits. MEPS Table 6: Emergency Room Services-Median and Mean Expenses per Person with Expense and Distribution of Expenses by Source of Payment. United States; 2013. [Google Scholar]
- 32.Davis K, Carper K. Use and Expenses for Office-Based Physician Visits by Specialty, 2009: Estimates for the US Civilian Noninstitutionalized Population. Rockville, MD: Agency for Healthcare Research and Quality, Statistical Brief; August 2012. p. 381. [Google Scholar]
- 33.Boushey H, Glynn S. There are Significant Business Costs to Replacing Employees. Center for American Progress; 2012. Available at: https://cdn.americanprogress.org/wp-content/uploads/2012/11/16084443/CostofTurnover0815.pdf Accessed December 9, 2016. [Google Scholar]
- 34.Tracey JB, Hinkin TR. Contextual factors and cost profiles associated with employee turnover. Cornell Hosp Quart 2008; 49:12–27. [Google Scholar]
- 35.Tourangeau R, Yan T. Sensitive questions in surveys. Psychol Bull 2007; 133:859. [DOI] [PubMed] [Google Scholar]
- 36.Greenfield TK, Nayak MB, Bond J, Kerr WC, Ye Y. Test-retest reliability and validity of life-course alcohol consumption measures: the 2005 National Alcohol Survey follow-up. Alcohol Clin Exp Res 2014; 38:2479–2487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jain R, Quraishi R, Majumder P, Pattanayak RD. Comparison of self-report and biological measures for alcohol, tobacco and illicit drug use in consecutive alcohol-dependent patients visiting a tertiary care centre. J Subst Use 2013; 18:302–310. [Google Scholar]
- 38.Babor TF, Steinberg K, Anton R, Del Boca F. Talk is cheap: measuring drinking outcomes in clinical trials. J Stud Alcohol 2000; 61:55–63. [DOI] [PubMed] [Google Scholar]
- 39.Del Boca FK, Noll JA. Truth or consequences: the validity of self-report data in health services research on addictions. Addiction 2000; 95 suppl 3:S347–S360. [DOI] [PubMed] [Google Scholar]
- 40.Harrell AV. The validity of self-reported drug use data: the accuracy of responses on confidential self-administered answered sheets. NIDA Res Monogr 1997; 167:37–58. [PubMed] [Google Scholar]
- 41.Harrison L. The validity of self-reported drug use in survey research: an overview and critique of research methods. NIDA Res Monogr 1997; 167:17–36. [PubMed] [Google Scholar]
- 42.Rudd RA. Increases in drug and opioid-involved overdose deaths—United States, 2010–2015. MMWR Morb Mortal Wkly Rep 2016; 65:1445–1452. [DOI] [PubMed] [Google Scholar]


