Abstract
Background
A bed that is too small to allow patients to turn from supine to side lying increases the difficulty of mobilizing patients, which can increase risk of musculoskeletal injury to caregivers, increase risk of pressure injuries to patients, and reduce patient comfort. Currently, no guidance is available for what patient sizes are accommodated by the standard 91cm (36 in.)-wide hospital bed, and no studies have evaluated the relationship between anthropometric attributes and space required to turn in bed.
Objective
The purpose of this research was to determine how much space individuals occupy when turning from supine to side lying as predicted by their anthropometry (i.e., body dimensions) to establish guidance on selecting the appropriate bed size.
Methods
Forty-seven adult participants (24 female) with body mass index (BMI) from 20 to 76 kg/m2 participated in a laboratory study. Body dimensions were measured, and the envelope of space required to turn was determined using motion capture. Linear regressions estimated the relationship between anthropometric attributes and space occupied when turning.
Results
BMI was strongly correlated (R2 = .88) with the space required to turn. Based on the linear regressions, individuals with BMI up to 35 kg/m2 could turn left and right within 91 cm and individuals with BMI up to 45 kg/m2 could turn one direction within 91 cm.
Discussion
BMI is a good predictor of the space required to turn from supine to lateral. Nurses should consider placing patients that are unable to laterally reposition themselves on a wider bed when BMI is greater than 35 kg/m2 and should consider placing all patients greater than 45 kg/m2 on a wider bed regardless of mobility. Hospital administrators can use historical demographic information about the BMI of their patient populations to plan facility-level equipment procurement for equipment that accommodates their patients.
Key Words: bariatric equipment, caregiver injury, hospital bed, obesity, patient care, patient handling
Over one third of the U.S. population is now obese with a body mass index (BMI) greater than 30 kg/m2 (Ogden, Carroll, Fryar, & Flegal, 2015). As the general population has increased in body size, so too has the hospital population. From 2006 to 2015, the mean patient weight in acute care increased from 80.5 to 83.7 kg (177.5–184.5 lbs; Vangilder, Lachenbruch, Algrim-Boyle, & Meyer, 2017). Over the same period, the mean BMI increased from 29.0 to 29.7 kg/m2 (Vangilder et al., 2017), which is very near the definition of obese. A particular challenge for caregivers is that, although the mean body weight of the population is increasing, the heaviest patients are increasing at an even faster rate. For example, in 2006, 2.5% of patients weighed more than 136 kg (300 lbs), compared with 4.0% in 2015 (unpublished data from Vangilder et al., 2017).
To properly care for a patient of size, caregivers require specialized equipment that can accommodate the dimensions, weight, and specific mobility needs of such patients (Camden, 2006). Matching the patient with the proper size of hospital bed is particularly important for the recovery of the patient and the safety and effectiveness of the care team. The hospital bed is typically the piece of equipment with which the patient has the most contact and is central to most aspects of nursing care. The standard width of a hospital bed is 91 cm (36 in.), although 102-cm (40-in.) and 127-cm (50-in.) widths are also available. Currently, there is no data to support guidance on what size of bed should be selected for a particular patient.
Background
There is little mention in the literature of how to select a bed size for a patient, and none of these recommendations appear to be supported by empirical evidence on patient space requirements. In many cases, the lowest weight capacity of standard equipment appears to drive bariatric protocols, such as using a wider bed for patients weighing greater than 159 kg (350 lbs; Muir & Archer-Heese, 2009). Another source suggests assigning specialized “bariatric” beds for patients heavier than 147 kg (325 lb) or with a BMI greater than 55 kg/m2, although it is unclear how this threshold was determined (Gourash, Rogula, & Schauer, 2007).
Caregivers can experience negative consequences when there is insufficient space to turn a patient in bed who is unable to self-reposition.
Of the many activities performed by patients and caregivers using the hospital bed, moving from supine to side lying is an activity that requires a particularly large amount of space to accommodate the patient. Patients who have insufficient space to turn in bed may have limited ability to reposition the body, which could increase discomfort or negatively impact patient sleep. Many patients, particularly those who have undergone abdominal surgery, must first turn to their side and then push up or rotate about the hips to stand (Zafiropoulos, Alison, & McCarren, 2004). Without space to turn, those patients must flex at the hip, contracting abdominal muscles, which could cause additional pain (Smith-Temple & Johnson, 2006).
In addition to potentially affecting comfort and patient satisfaction, insufficient space to turn in bed may negatively impact patient outcomes. Caregivers must frequently turn patients for a variety of objectives that include wound inspection, dressing changes, repositioning to relieve pain, bed pan placement, linen changes, cleaning or bathing, helping to mobilize patients, or for repositioning to prevent pressure injuries (Smith, Duell, Martin, Gonzalez, & Aebersold, 2017). If a patient is unable to self-reposition or be easily turned by caregivers, that patient may not as frequently off-load parts of the body exposed to sustained pressure that can lead to pressure injuries (Brindle et al., 2013; Oertwich, Kindschuh, & Bergstrom, 1995). Fragala, Perry, and Fragala (2012) have also suggested that in long-term care, a bed that is too narrow may increase the likelihood that patients could roll past the edge of the bed and fall.
Caregivers can experience negative consequences when there is insufficient space to turn a patient in bed who is unable to self-reposition. If a bed is only slightly wider than the space required to turn the patient, caregivers must first laterally reposition the patient to the edge of the bed that is opposite the direction of the turn before turning the patient. Without this lateral repositioning the patient would otherwise roll off the bed or be turned into the opposite side rail resulting in impingement. This lateral repositioning requires high pull forces and exposes caregivers to a greater risk of injury than turning the patient (Wiggermann, 2016). If there is insufficient space for the patient to be turned even once, then caregivers must turn and laterally slide the patient simultaneously, which is physically demanding and requires additional staff.
Although there are many consequences to having a bed that is too narrow, there may also be drawbacks to using beds that are unnecessarily wide. Wider beds tend to cost more, and using a bed that is needlessly wide may incur unnecessary costs for the healthcare institution. Moreover, an unnecessarily wide bed will require caregivers to reach farther as they extend their arms from the edge of the bed to the patient, which could increase the risk of back injury (Waters, 2007).
Purpose
The objective of this study was to determine how much space individuals occupy when turning from supine to side lying as predicted by their anthropometric attributes (i.e., body dimensions). The relationship between anthropometric attributes and space occupied when turning was then used to establish guidance on selecting an appropriate hospital bed width based on the size of the patient.
METHODS
Design
This was an experimental study performed in a laboratory environment, which allowed careful recruitment of participants based on physical attributes, safe execution of the experimental protocol, and precise measurement techniques.
Participants
Forty-seven (47) healthy adult participants (24 female, 23 male) were recruited from the local population by phone and word of mouth. Individuals were ineligible to participate if they were pregnant or had an injury or condition that affected their ability to independently get in and out of bed or roll onto their side. Participants were recruited specifically so that a range of BMI was sampled. Five women and five men were recruited in each BMI category: 18.5–24.9, 25–34.9, and 35–44.9 kg/m2. Because of the difficulty of recruiting high-BMI participants, BMI category limitations were not set for the remaining 17 participants who were all of BMI greater than 45. Participants wore their own form-fitting clothes during the experiment (e.g., knitted leggings, gym shorts, fitted T-shirts). Ethics committee approval was obtained prior to conducting this experiment, and all participants provided informed consent prior to participating.
Equipment
Testing occurred on both a hard, rigid polyethylene surface and a Compella bariatric hospital bed with a therapeutic air mattress (Hill-Rom, Batesville, IN). Hard and very soft surfaces were selected for the study to test whether the type of surface affects the distance occupied when turning in bed. Both surfaces were 127 cm (50 in.) wide to provide enough space for all participants to turn from supine to side lying.
Anthropometric Measurements
To determine physical attributes that could be used to predict the space an individual occupies when turning from supine to side lying, several anthropometric measurements were recorded. The complete list is shown in Table 1. Body weight was measured using a digital scale (Scale-Tronix 5002, Welch Allyn, Skaneateles, NY). Height and all other dimensions taken in the standing posture using the methods of Gordon et al. (1989) were recorded. Supine anthropometric measurements in the current study were recorded with the participant lying on the hard polyethylene surface with the legs at a comfortable spacing. The elbows rested on the surface with the upper arms adducted so that the arms slightly touched against the torso; the upper arms rested on the stomach. The landmarks for all supine measurements were also the same as those used by Gordon et al. (1989), with the exception of supine torso breadth, which was measured as the widest point of the torso anywhere between the chest and knees. All anthropometric measurements of male participants were made by the author (NW), and all measurements of female participants were made by the same female lab assistant. Both measurers practiced before the study to ensure consistency of technique and resulting measurements.
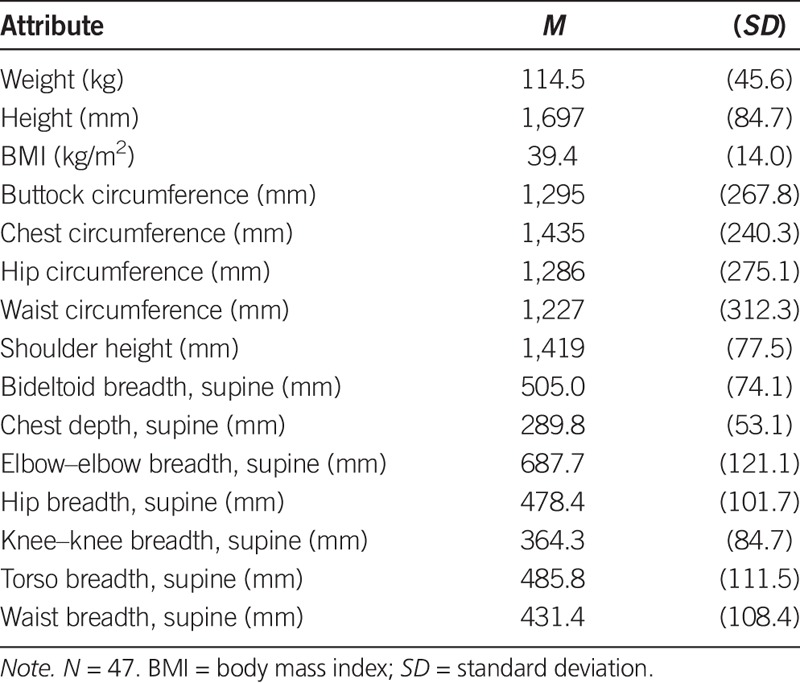
TABLE 1.
Participant Anthropometric Attributes
Motion Capture Measurements
The position of participants in three-dimensional space was quantified using a motion capture system (Motion Analysis, Santa Rosa, CA). The system is capable of measuring the position of reflective markers placed on the participant with a measurement error of less than 1 mm. Markers were placed as shown in Figure 1. The forehead, acromion (shoulder), trochanter, and knee markers were placed consistently for all participants. When supine, two additional makers were placed to characterize the most lateral points on the side opposite the direction of the turn. The lateral torso marker described the most lateral point on the torso, and the lateral arm marker described the most lateral point of the upper arm (between the elbow and shoulder). After the participant turned to side lying, a final marker was placed on the most anterior point of the torso.
FIGURE 1.
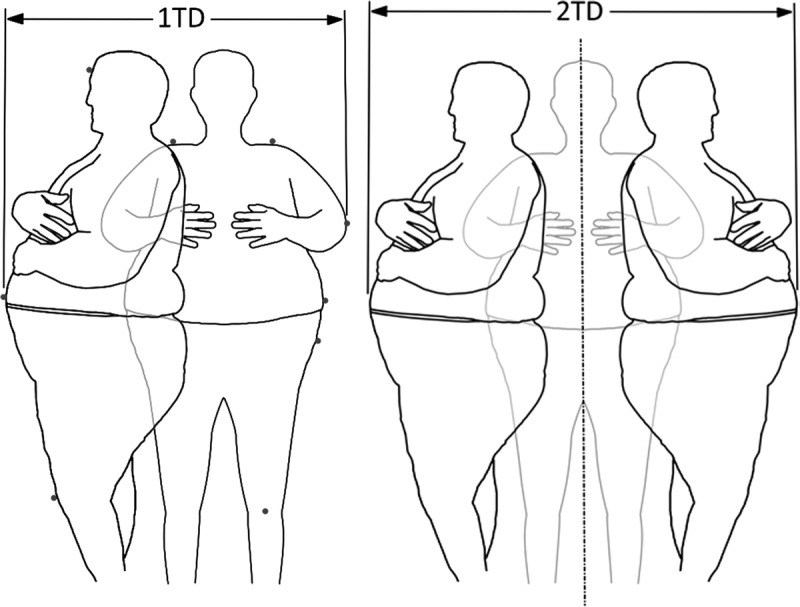
Illustration of single turn distance (1TD, left) and left and right turn distance (2TD, right). The dots on the left image show the placement of the motion capture markers.
The coordinates from motion capture were used to calculate the main dependent variables (see Figure 1). Single turn distance (1TD) was the distance along the width of the bed of the most lateral point of the arm when supine to the most anterior point on the body when side lying. Left and right turn distance (2TD) was the distance occupied when turning both left and right. This was calculated as twice the distance of a stationary plane coincident with the sagittal plane of the supine participant (midpoint of the trochanters) to the most anterior point when side lying. Whereas 2TD was intended to define the distance a patient required when turning from the center of the bed, 1TD was the absolute minimum distance a patient would require if turning from one edge of the bed to the opposite edge. Lateral migration was an estimate of how far the body moved after turning and returning back to supine. It was calculated as the distance moved by the lateral point of the torso when supine before turning compared to when supine after turning.
Procedure
After providing informed consent, anthropometric measurements were recorded, and motion capture markers were placed on the participant. Participants lay on either the hard surface or mattress and practiced turning. To minimize variation, a standardized turning procedure was followed. Participants began by abducting the arm on the side of the intended turn 60° from the body and crossing the other arm over the body. They then bent the knee of the leg on the opposite side of the turn, placed the foot flat on the surface, and pushed with the leg to turn approximately 90° until they were on their side. For trials on the hard surface, a right-angle steel brace that stood 18 in. wide × 14 in. tall perpendicular to the surface was lightly placed against the back of the participant to standardize the position. On the mattress, no positioning aids were used to test a purely natural posture.
Participants were instructed strictly to roll and not to scoot, drag, or reposition their hips. The purpose of this instruction was to ensure that the maximal space occupied when turning was captured; if a caregiver was turning a patient or a deconditioned patient was turning independently, this hip movement would not be possible. After turning to side lying, participants paused so that the anterior point marker could be placed on the most anterior part of the torso. Participants then slowly rolled back to supine, again without scooting, dragging, or repositioning.
Participants turned to the left and right once on each surface for a total of four trials per participant. Motion capture data were collected during each trial. Two study administrators watched the participant, and trials were repeated if the procedure was not followed.
Data Analysis
General linear regression models were used to estimate the relationship between each main dependent variable (i.e., 1TD and 2TD) and each of the anthropometric variables. Analysis of variance was used to test the effect of surface type on 1TD, 2TD, and lateral migration, with surface as a fixed effect and participant as a random effect. Analyses were performed using Minitab software (Minitab, State College, PA).
RESULTS
The anthropometric attributes of the study participants are shown in Table 1. The BMI of participants ranged from 20.4 to 76.4 kg/m2 (M = 39.4 kg/m2).
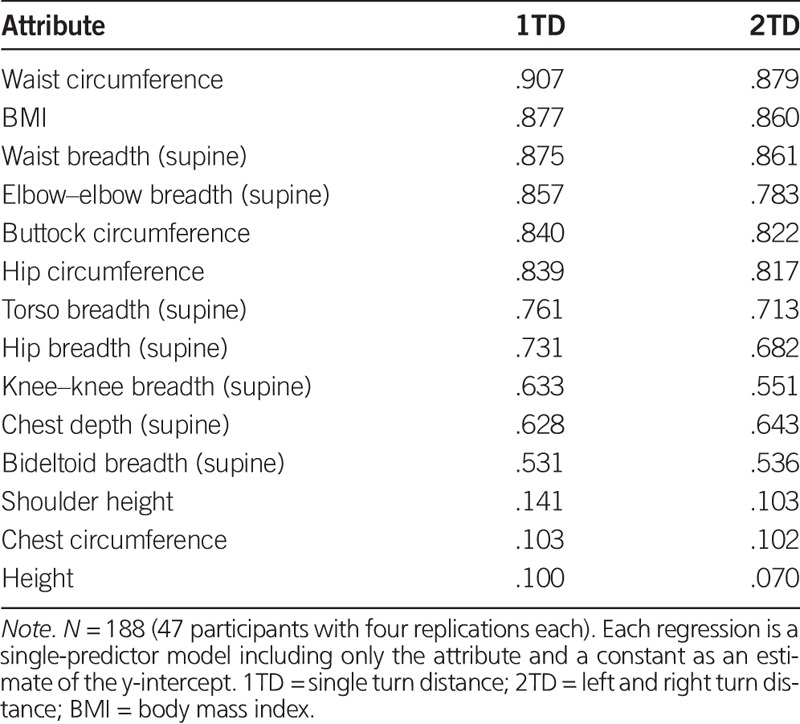
Correlation coefficients for single-predictor models for each anthropometric attribute on 1TD and 2TD are shown in Table 2. BMI, waist circumference, and waist breadth were most strongly correlated to 1TD and 2TD. In general, most circumference and breadth measurements were well correlated with 1TD and 2TD, but height measurements and chest circumference were poorly correlated with 1TD and 2TD. Specifically, the correlation of BMI with 1TD was strong and significant (adjusted R2 = .88, p < .001), as was the relationship between BMI and 2TD (adjusted R2 = .86, p < .001).
TABLE 2.
Adjusted R2: Regressions of Turn Distance on Each Anthropometric Attribute Under 1TD and 2TD Conditions
Because observations were clustered within participants, we also ran a sensitivity analysis using a mixed effects model with participants as random factors. The results were very similar to the original single-predictor simple model. The p-values were <.001 for both the mixed models and simple models. A drawback of the mixed model is that it does not return R2 values, which are useful for interpreting the fit of the model. Given that the results were very similar between the two model types and that the original single-predictor simple models are conservative, we presented them here. We also averaged the dependent variable (i.e., 1TD and 2TD) for each subject and ran the regressions of patient average on the single predictor. Again, the results were very similar (p < .001, R2 similar). This suggests that the results are robust to the consideration of the participant as a factor in the model.
A scatter plot with a line fit is shown for the relationship between BMI and 1TD (Figure 2A) and BMI and 2TD (Figure 2B). Overlaid on these figures are the widths of hospital beds currently available to caregivers.
FIGURE 2.
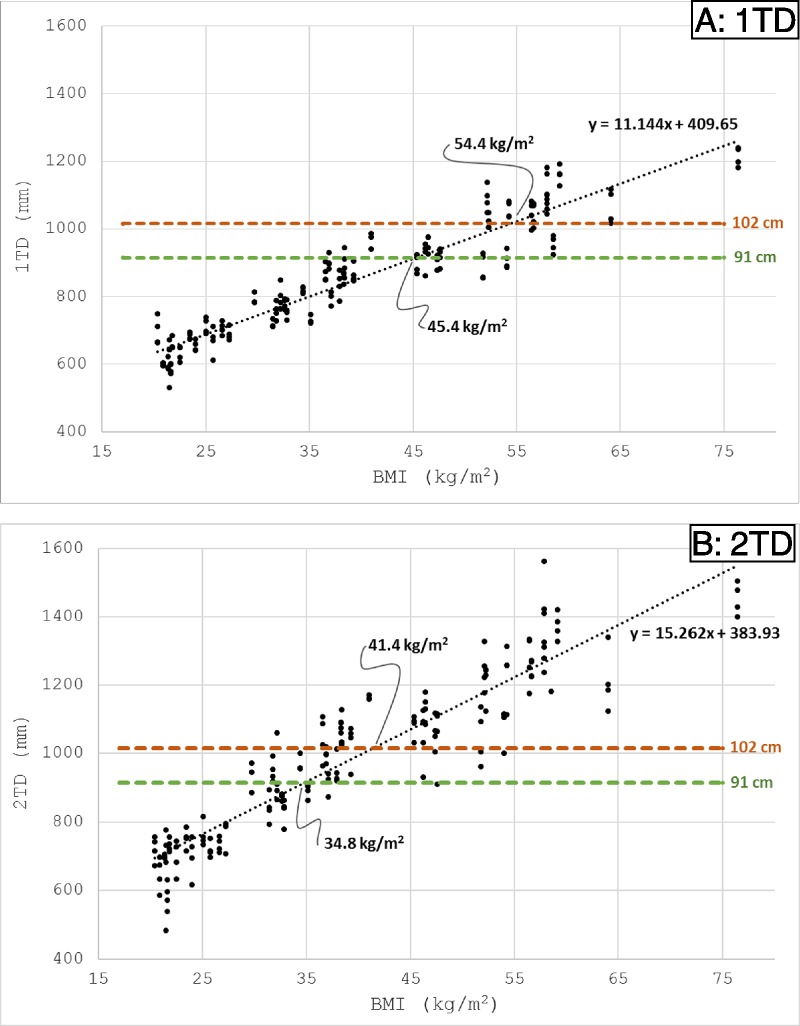
(A) Scatter plot of body mass index (BMI) versus space occupied when turning one direction (1TD) for all experimental trials. The horizontal lines represent common hospital bed widths. The BMI values for the intersection of the line fit and hospital bed widths are labeled. (B) Scatter plot of BMI versus space occupied when turning both directions (2TD) for all experimental trials. The horizontal lines represent common hospital bed widths. The BMI values for the intersection of the line fit and hospital bed widths are labeled.
Lateral migration averaged 15.4 mm (SD = 15.7 mm). The effect of surface on 1TD and 2TD was not significant. Lateral migration was significantly greater on the air surface than the hard surface, but the difference was only 5 mm. These results suggest that findings from the current study are likely generalizable to any hospital bed mattress.
DISCUSSION
The current study was the first of its kind to quantify the space occupied when turning from supine to side lying and to correlate this measurement to anthropometric dimensions. The findings from this study have clear implications for selecting hospital beds that will appropriately accommodate patients.
The findings from this study have clear implications for selecting hospital beds that will appropriately accommodate patients.
For many aspects of care, such as changing linens, cleaning patients, or turning to prevent pressure injuries, caregivers need to turn a patient both left and right. Assuming that turning from supine to side lying represents the maximum space that a patient needs to occupy in bed, the 1TD and 2TD measurements can be used to provide guidance for selecting hospital bed sizes depending on the condition of the patient. For patients that are unable to self-reposition, 2TD represents the amount of space required in bed to allow a patient who is centered in the bed to be turned both directions without lateral repositioning by caregivers. However, for patients who are able to self-reposition, 1TD can serve as a minimum requirement. These patients can move themselves laterally to either edge of the bed to allow the space to turn the opposite direction. In this manner, a patient with the ability to self-reposition would still be able to turn either direction within the 1TD dimension.
Waist circumference was the best predictor of 1TD and 2TD (adjusted R2 = .91 and .88, respectively). However, the correlation of BMI to 1TD and 2TD was nearly as strong (adjusted R2 = .88 and .86) and is much more practical to use than waist circumference when selecting hospital beds. Measuring waist circumference takes additional time and requires a patient to stand, which may be impossible in many circumstances. Alternatively, BMI for an individual patient can be estimated using medical records. For facility planning, BMI can also be easily referenced from hospital historical data or population statistics, whereas such data are not as readily available for waist circumference.
Based on the linear regression of BMI and 2TD, patients who are unable to self-reposition with a BMI up to 35 kg/m2 could be placed on a 91-cm (36-in.)-wide bed, patients up to 40 kg/m2 could be placed on a 102-cm (40-in.)-wide bed, and patients with a BMI greater than 40 kg/m2 should be on a 127-cm (50-in.)-wide bariatric bed. However, for patients who are able to slide side-to-side in bed or lift their hips to turn while staying centered in the bed, 1TD appears to represent the minimum space required for the patient in bed. For patients with the ability to self-reposition, those with BMI up to 45 kg/m2 could be placed on a 91-cm-wide bed, up to 55 kg/m2 could be placed on a 102-cm-wide bed, and those with BMI greater than 55 kg/m2 should be placed on a bariatric bed. These minimum requirements are summarized in Table 3.
TABLE 3.
Recommendations: Bed Widths Based on Patient Mobility and Body Mass Index
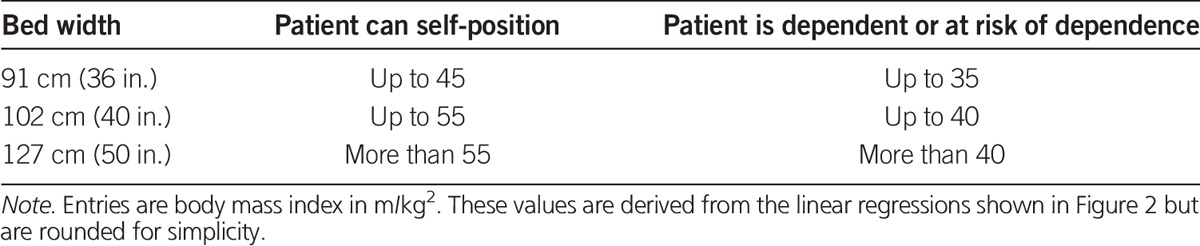
The BMI distribution of 58,149 patients in the acute care population from the 2016 International Pressure Ulcer Prevalence Survey (unpublished data from Vangilder et al., 2017) can be used to provide some indication of a minimum of how many specialized beds may be needed at a facility level. Population percentiles for patients with BMI of 35, 40, 45, and 55 kg/m2 are 79%, 88%, 93%, and 96%, respectively. Based on the 2TD estimates in the current study, for patients that are unable to self-reposition, a 36-in.-wide bed should accommodate 79% of patients and a 40-in.-wide bed should accommodate 88% of patients. For patients who are able to self-reposition (1TD) a 36-in.-wide bed should accommodate 93% and a 40-in.-wide bed should accommodate 96%.
Limitations
When applying the findings of the current study, it should be noted that the requirements for bed sizing are based on population averages determined by linear regression. There will be some patients who may occupy more space when turning than is predicted by the linear regression for their BMI. Alternatively, some patients may require less space than predicted by the linear regression.
The recommendations in the current study do not consider additional space that may be required as patients shift in bed. Although the lateral migration of 15.4 mm determined in the current study is small, this distance could add up as patients turn repeatedly, which could increase the space required by the patient. These recommendations also consider only the space occupied when turning and do not consider other activities such as physical therapy. The 1TD and 2TD measurements do not consider braces or other medical equipment that may increase the space needed for mobility. In addition, these recommendations only consider the physical space to accommodate a patient and did not evaluate the relationship between bed width and patient satisfaction or comfort.
Although recruiting healthy participants in the current study afforded several methodological strengths that include a large sample size, a diverse participant population, and a precise measurement methodology, the healthy population is also a limitation. Despite the participant population representing a wide range of ages, the patient population is older and more deconditioned than the study population. This means that a patient with a given BMI may occupy slightly more or less space than a healthy patient in the current study with the same BMI. It is possible that these differences could affect the coefficients of the line fits that were used to develop these bed sizing recommendations, but the impact should be modest.
Conclusions
BMI is a good predictor of the space an individual requires to move from supine to side lying. The findings from this study suggest that, when lying in the center of a standard 91-cm-wide hospital bed, a patient with a BMI greater than 35 kg/m2 would have insufficient space to be turned in either direction within the bed without lateral repositioning. Furthermore, a patient with a BMI greater than 45 kg/m2 would have insufficient space to be turned at all, even if repositioned to one edge of the surface before being turned. Nurses should consider placing patients that are unable to laterally reposition themselves on a wider bed when BMI is greater than 35 kg/m2 and should consider placing all patients greater than 45 kg/m2 on a wider bed regardless of mobility. Hospital administrators can use historical demographic information about the BMI of their patient populations to plan facility-level equipment procurement for equipment that accommodates their patients.
Figure.
No caption available.
Footnotes
Conflicts of interest: All authors are employees of Hill-Rom, a manufacturer of hospital beds. Kathryn Smith also owns stock in Hill-Rom.
Funding statement: This research was funded by Hill-Rom.
REFERENCES
- Brindle C. T., Malhotra R., O'Rourke S., Currie L., Chadwik D., Falls P., … Creehan S. (2013). Turning and repositioning the critically ill patient with hemodynamic instability: A literature review and consensus recommendations. Journal of Wound Ostomy & Continence Nursing, 40, 254–267. doi:10.1097/WON.0b013e318290448f [DOI] [PubMed] [Google Scholar]
- Camden S. G. (2006). Nursing care of the bariatric patient. Bariatric Nursing and Surgical Patient Care, 1(1), 21–30. doi:10.1089/bar.2006.1.21 [Google Scholar]
- Fragala G., Perry B., & Fragala M. (2012). Examining bed width as a contributor to risk of falls from bed in long-term care. Annals of Long-Term Care: Clinical Care and Aging, 20(6), 35–38. [Google Scholar]
- Gordon C. C., Churchill T., Clauser C. E., Bradtmiller B., McConville J. T., Tebbetts I., & Walker R. A. (1989). 1988 Anthropometric Survey of US Army Personnel: Methods and Summary Statistics. Tech Report Natick/TR-89/044 Natick, MA: U.S. Army Natick Research, Development, and Engineering Center. [Google Scholar]
- Gourash W., Rogula T., & Schauer P. R. (2007). Essential bariatric equipment: Making your facility more accommodating to bariatric surgical patients. In Schauer P. R., Schirmer B. D., Brethauer S. (Eds.), Minimally invasive bariatric surgery (pp. 37–49). New York, NY: Springer. [Google Scholar]
- Muir M., & Archer-Heese G. (2009). Essentials of a bariatric patient handling program. OJIN: The Online Journal of Issues in Nursing, 14(1), Manuscript 5 doi:10.3912/OJIN.Vol14No1Man05 [Google Scholar]
- Oertwich P. A., Kindschuh A. M., & Bergstrom N. (1995). The effects of small shifts in body weight on blood flow and interface pressure. Research in Nursing & Health, 18, 481–488. [DOI] [PubMed] [Google Scholar]
- Ogden C. L., Carroll M. D., Fryar C. D., & Flegal K. M. (2015). Prevalence of obesity among adults and youth: United States, 2011–2014. NCHS Data Brief, 219, 1–8. Retrieved from https://www.cdc.gov/nchs/data/databriefs/db219.pdf [PubMed] [Google Scholar]
- Smith S. F., Duell D. J., Martin B. C., Gonzalez L., & Aebersold M. (2017). Exercise and ambulation. Clinical nursing skills: Basic to advanced skills (9th ed). New York, NY: Pearson. [Google Scholar]
- Smith-Temple J., & Johnson J. Y. (2006). Nurses' guide to clinical procedures (5th ed). Philadelphia, PA: Lippincott Williams & Wilkins. [Google Scholar]
- VanGilder C., Lachenbruch C., Algrim-Boyle C., & Meyer S. (2017). The International Pressure Ulcer Prevalence™ Survey: 2006–2015: A 10-year pressure injury prevalence and demographic trend analysis by care setting. Journal of Wound Ostomy & Continence Nursing, 44, 20–28. doi:10.1097/WON.0000000000000292 [DOI] [PubMed] [Google Scholar]
- Waters T. R. (2007). When is it safe to manually lift a patient? American Journal of Nursing, 107, 53–58. [DOI] [PubMed] [Google Scholar]
- Wiggermann N. (2016). Biomechanical evaluation of a bed feature to assist in turning and laterally repositioning patients. Human Factors, 58, 748–757. doi:10.1177/0018720815612625 [DOI] [PubMed] [Google Scholar]
- Zafiropoulos B., Alison J. A., & McCarren B. (2004). Physiological responses to the early mobilisation of the intubated, ventilated abdominal surgery patient. Australian Journal of Physiotherapy, 50, 95–100. doi:10.1016/S0004-9514(14)60101-X [DOI] [PubMed] [Google Scholar]


