Supplemental Digital Content is available in the text.
Keywords: cardiovascular, chest pain, primary healthcare, referral, symptom onset, transport to emergency department
Abstract
Background
It is important that patients with symptoms of acute coronary syndrome receive appropriate medical care as soon as possible. Little is known about the preadmission actions that patients with chest pain take before arrival at the Emergency Department (ED).
Objective
This study aimed to describe the actions of patients with chest pain or pressure after onset of symptoms. What is the first action following onset of symptoms? Who is the first lay or professional person to be contacted? Which steps are taken first? How is the patient transported to the hospital?
Methods
Consecutive patients, arriving at the ED of two large hospitals in Belgium, were asked additional questions during the initial assessment.
Results
Overall, 35% of 412 consecutive patients with chest pain admitted to the ED were diagnosed with acute coronary syndrome. A total of 57% contacted a GP between symptom onset and arrival at the ED. Only 32% of the patients were transported to the ED by ambulance, 16% drove themselves and 52% arrived by other means of transport (by family, neighbour, GP, public transport).
Conclusion
In Belgium, the GP is still the first professional to be contacted for most patients. Other patients initially rely on their partner, family or friends when symptoms emerge. Too often, patients with chest pain rely on other transport to get to the ED instead of calling the Emergency Medical Services. This study included only patients who ultimately attended the ED.
Introduction
Early referral of possible acute coronary syndrome (ACS) patients to a hospital is crucial in optimizing survival and subsequent quality of life 1–3. It is very difficult for patients to correctly attribute symptoms to either a cardiac or other cause. Half of all ST segment elevation myocardial infarction patients do not experience a typical episode of acute severe chest pain – the so-called ‘Hollywood heart attack’ – but have atypical symptoms. Patients’ expectations of symptoms are crucial in taking action and contribute considerably towards patient delay 4–10.
Little is known about the actions taken by patients with chest pain in Belgium before assessment at the Emergency Department (ED). Therefore, the aim of this study is to gain insight into the different actions of a patient with chest pain and to examine differences in actions according to sex, level of anxiety, localization and duration of the symptoms and previous experience with similar symptoms.
Methods
Population
The study population included consecutive patients presenting with chest pain or oppression at the ED or chest unit of the University hospital of Leuven (UHL) and the regional hospital of Genk, Belgium, between November 2013 and May 2014. They were 18 years of age or older and did not have any mental impairment. Exclusion criteria were as follows: arrival at more than 24 h after the onset of symptoms, a clear traumatic cause of the complaints and symptoms that were considered a recurrence of known symptoms with a previous noncardiac diagnosis.
Measurements
The questionnaire was completed by the treating physician after a verbal consent was provided by the patient, recorded in the file. The interview consisted of eight questions with predefined multiple choice answers: when did this episode of chest pain or oppression, which has led you to the ED, start? Did you have similar symptoms before? What was your level of anxiety? Where were you when noticing the symptoms? What was your first action when feeling central chest pain (crushing or squeezing) and in case you did not take any action, who was the person taking action and what did he or she do? If you contacted the GP or ambulance service, what did they do? How did you finally go to the hospital?
Study coordinators were trained in clinical data collection.
Anxiety was measured on a Likert scale of 0 to 10 (0 indicated no fear and 10 indicated considerable fear) 11.
Analysis
The initial surveys were completed by a team of GPs, a cardiologist and an emergency physician. The results are presented in a descriptive manner. We described sequences of actions by patients and their caretakers. Differences between groups were tested using the χ2or the Fisher’s exact test (in case of categorical variables) or the Kruskal–Wallis test (in case of continuous variables).
Ethical aspects
The study was approved by the ethical review board of both hospitals (coordinating review board is UHL: no S55411).
Results
Participants
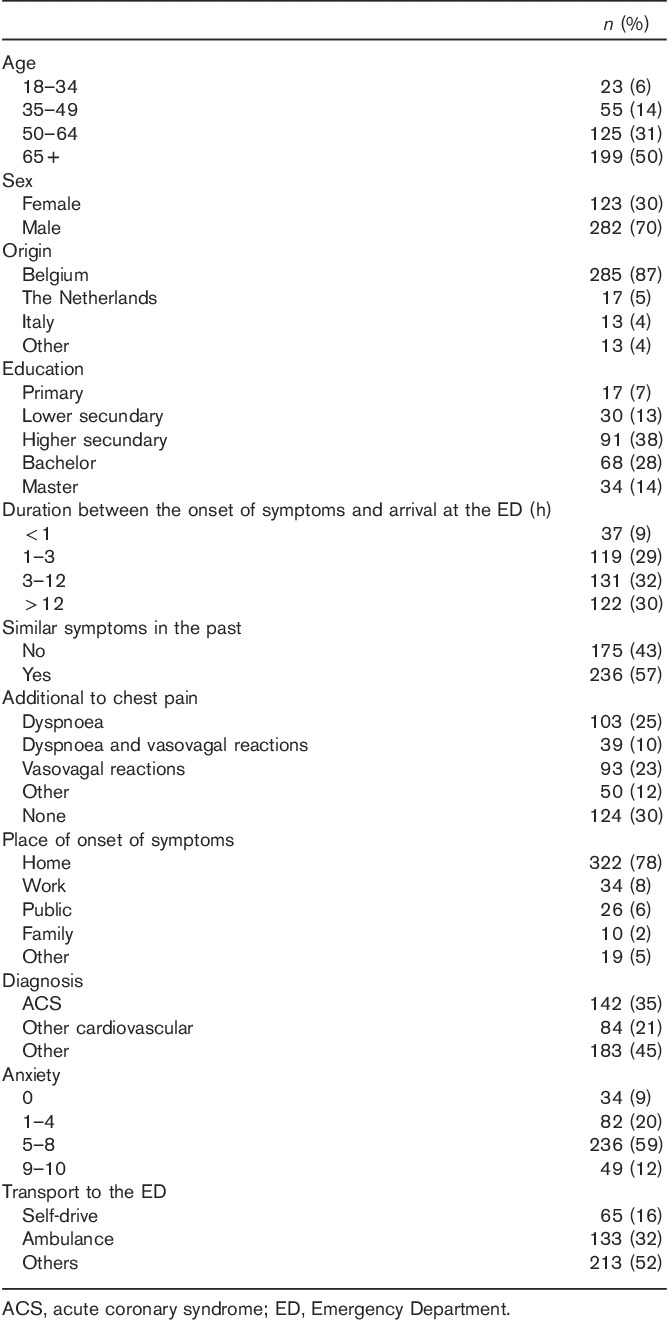
We included 414 patients, 214 in Leuven and 200 in Genk. The average age of the patients was 63 years (18–93) and 70% were men. Overall, 87% were of Belgian origin, 38% had a higher secondary education and 29% a bachelor degree or more. A total of 71% of the patients scored at least 5 on the anxiety scale. Symptoms started when the patient was at home in 78% of the cases. A total of 57% of the patients had already similar symptoms in the past.
A total of 30% of the patients with chest pain initially had no additional symptoms, 35% additionally had dyspnoea, 33% had general vasovagal reactions and 12% had other symptoms.
The final diagnoses in hospital were ACS in 35% of the cases, other cardiovascular events (including pulmonary embolism) in 20% and noncardiovascular events in 45% (Table 1).
Table 1.
Patient characteristics
No patient included in the study died before leaving the ED.
Actions
A total of 45% of patients initially contacted the GP. Only 21% directly contacted the Emergency Medical Services (EMS) and 34% took other action (no action, call a nurse in the nursery home, take medication, call cardiologist). Overall, 56% of the patients with chest pain finally contacted the GP (either their own GP or a GP on duty) before leaving for the ED (Table 2).
Table 2.
Actions taken by a patient with chest pain
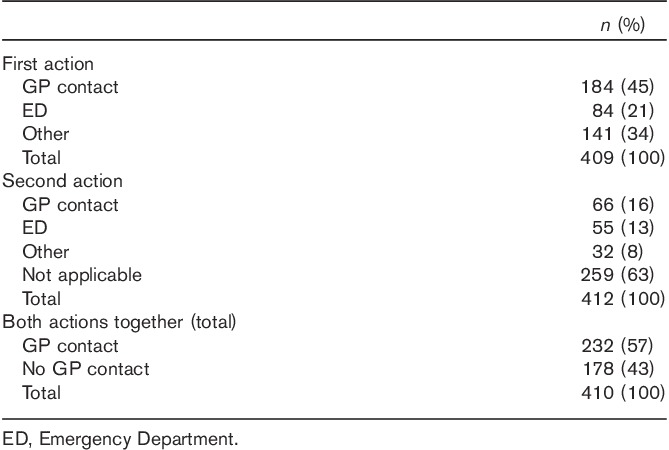
If patients initially took no action (20%), their partner took action in 36%, other family or a neighbour in 23%, caregivers in 26% and other individuals in 15% of cases. Overall, 40% of these persons who took action called the GP and 15% called the EMS. Only 25% of the persons immediately brought the patient to ED by their own means. The remaining 20% could not be categorized (already at the hospital for other reasons, called another specialist, called a taxi).
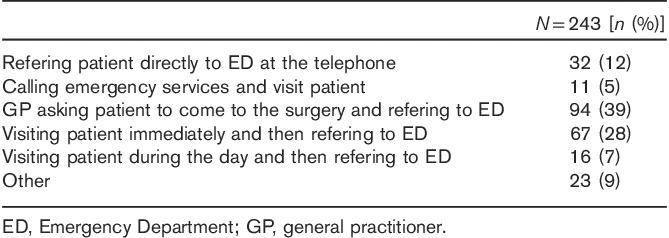
If the GP is involved in the process, 39% of the GPs asked the patient to come over to their practice and then referred them to the ED. A total of 28% of the GPs immediately visited the patient and were referred to the ED. Five percent of the GPs immediately called the EMS and 12% advised the patient to leave for the ED immediately (Table 3).
Table 3.
Action of GP after being called by the patient
Nine percent of all patients arrived at the ED within 1 h after the onset of symptoms and 29% between 1 and 3 h (Table 1).
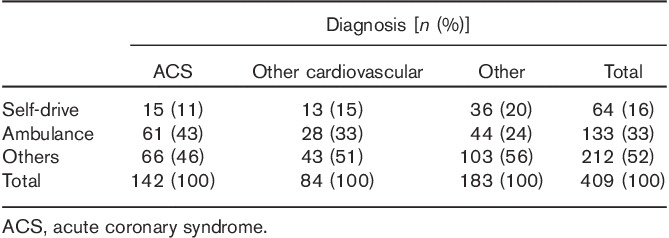
Of the patients, who were eventually diagnosed with ACS, almost half were initially driven to the hospital by a partner, family member or a neighbour (others) (46%). A total of 43% arrived by EMS ambulance and 11% drove to the ED themselves (Table 5).
Table 5.
Means of transport according to diagnosis
Patients driving to the ED by themselves on average were 59 years old, which is slightly lower than the overall average (63 years).
Determinants
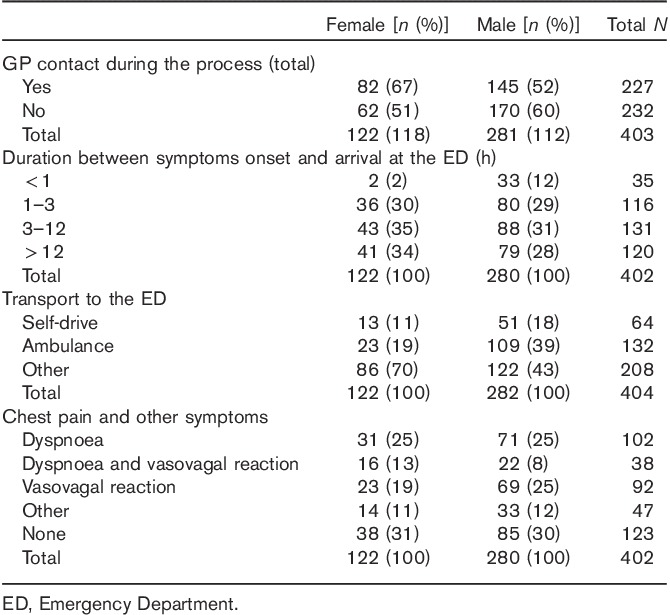
Women (67%) more frequently relied on the GP for an initial opinion versus 52% of men (P=0,02). Two percent of the women and 12% of men arrived at the ED within 1 h after the onset of symptoms. Overall, 70% of the women and 43% of the men were driven to the ED by a neighbour or family member (Table 4).
Table 4.
Differences in action and symptoms by sex
More than half of the patients (54%) brought in by ambulance arrived at the ED within 3 h after the onset of symptoms (14% within 1 h). Of all patients driving themselves, 31% arrived within 3 h (5% within 1 h) (P<0.01) (see Table, Supplemental digital content 1, http://links.lww.com/EJEM/A121, which explains the duration between symptoms onset and arrival at the ED according to patient characteristics).
A total of 89% of the patients, arriving at the ED within 1 h after the onset of symptoms, presented themselves with an anxiety score of at least 5 (66% more than 6) versus 66% arriving at the ED after more than 3 h after the onset of symptoms (P=0.16).
As mentioned before, there were no marked differences between means of transport and the final diagnosis (Table 5).
Discussion
Of all chest pain patients admitted to the ED, 56% had a serious cardiovascular disease, of whom 35% had ACS. Overall, GPs were involved in the process of diagnosis and referral in 57%. The main first action of the patient with chest pain was calling the GP (30%); only 5% directly called the EMS system and all of these were men.
In Belgium, access to any physician or to the hospital services is free. However, the GP is an established and familiar route to medical care and many patients believe that calling a GP should always be their first course of action. The average GP sees one or two patients with chest pain a week 12.
A number of investigators have reported that calling a physician’s office increases delay in seeking treatment 13–17. This is confirmed in our analysis as 36% of patients with symptoms for over 12 h when arriving at the ED also contacted their GP first versus 7% of the patients with a maximum of 1 h from the onset of symptoms. The increase in delay occurs initially for a variety of reasons including the GP not perceiving the symptoms as cardiac in nature, self-medication by the patient or the inability to contact the GP immediately 18.
It is remarkable that only 33% of these chest pain patients finally arrived at the ED by ambulance, 16% arrived driving their own car and 52% were brought in by their partner, family or neighbours. There was a significant sex difference in ambulance use; 19% of the women and 39% of the men used the EMS. This is not in agreement with previous findings from other countries, where women were more frequently transported by EMS 19,20.
The reason for not using the EMS for transport to the hospital should be examined further using both quantitative and qualitative designs. If the reasoning behind this observation is known, transportation by ambulance can be encouraged and facilitated by public campaigns.
In 62% of cases, the delay for patients in arriving at the ED was more than 3 h. This results from the complex process of decision-making after the onset of chest pain, including cognitive and emotional processes, individual beliefs and values, and the influence of the context of the event 14.
Consistent with previous qualitative research in Belgium, in 46% of the cases, the transport facilitator was a family member or a neighbour. The main reason for this observation could be a time-saving and cost-saving component (in Belgium, the patient has to pay for part of the ambulance services). This kind of use of own transport should be discouraged because transporting patients with a suspected ACS without professional supervision, including the availability of a defibrillator, is not recommended 10,13.
In the UK, the recommendation and the public health campaigns encouraged all patients with chest pain to phone 999 immediately. If the discomfort is only minor or has resolved, it may be more appropriate to either see a GP, call NHS 111 or attend a local walk-in centre http://www.nhs.uk/Conditions/chest-pain/Pages/Introduction.aspx.
Strengths and weaknesses
The strength of this study lies in the fact that it fits with daily life actions of patients and caregivers. We have gathered detailed information on a group of subsequent patients with chest pain admitted to the ED and data were collected in two different hospitals, decreasing the risk of reporting results specific for only one hospital.
The weakness of the study lies in the fact that the answers are provided by the patient instead of being observed by a researcher. Furthermore, we do not know what has happened with patients who had chest pain, but never visited an ED. They were either assessed or treated by the GP, self-medicated or waited for the symptoms to disappear without treatment. However, a study exploring this group is difficult to design and operationalize.
Conclusion
GPs still play a major role in the triage and referral of patients with chest pain in Belgium. However, some of the patients directly contact the EMS without contacting a GP, which may have implications for future training and experience of young GPs.
Supplementary Material
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's website, www.euro-emergencymed.com.
Acknowledgements
Conflicts of interest
There are no conflicts of interest.
References
- 1.Reimer KA, Jennings RB. The ‘wavefront phenomenon’ of myocardial ischemic cell death. II Transmural progression of necrosis within the framework of ischemic bed size (myocardium at risk) and collateral flow. Lab Invest 1979; 40:633–644. [PubMed] [Google Scholar]
- 2.Gersh BJ, Stone GW, White HD, Holmes DR., Jr Pharmacological facilitation of primary percutaneous coronary intervention for acute myocardial infarction: is the slope of the curve the shape of the future? JAMA 2005; 293:979–986. [DOI] [PubMed] [Google Scholar]
- 3.Moser DK, Kimble LP, Alberts MJ, Alonzo A, Croft JB, Dracup K, et al. Reducing delay in seeking treatment by patients with acute coronary syndrome and stroke: a scientific statement from the American Heart Association Council on cardiovascular nursing and stroke council. Circulation 2006; 114:168–182. [DOI] [PubMed] [Google Scholar]
- 4.Horne R, James D, Petrie K, Weinman J, Vincent R. Patients’ interpretation of symptoms as a cause of delay in reaching hospital during acute myocardial infarction. Heart 2000; 83:388–393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dracup K, Moser DK. Beyond sociodemographics: factors influencing the decision to seek treatment for symptoms of acute myocardial infarction. Heart Lung 1997; 26:253–262. [DOI] [PubMed] [Google Scholar]
- 6.Johansson I, Stromberg A, Swahn E. Factors related to delay times in patients with suspected acute myocardial infarction. Heart Lung 2004; 33:291–300. [DOI] [PubMed] [Google Scholar]
- 7.O’Donnell S, McKee G, Mooney M, O’Brien F, Moser DK. Slow-onset and fast-onset symptom presentations in acute coronary syndrome (ACS): new perspectives on prehospital delay in patients with ACS. J Emerg Med 2013; 46:507–515. [DOI] [PubMed] [Google Scholar]
- 8.Johnson JA, King KB. Influence of expectations about symptoms on delay in seeking treatment during myocardial infarction. Am J Crit Care 1995; 4:29–35. [PubMed] [Google Scholar]
- 9.Zerwic JJ. Symptoms of acute myocardial infarction: expectations of a community sample. Heart Lung 1998; 27:75–81. [DOI] [PubMed] [Google Scholar]
- 10.Ruston A, Clayton J, Calnan M. Patients’ action during their cardiac event: qualitative study exploring differences and modifiable factors. BMJ 1998; 316:1060–1065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Likert R. A technique for the measurement of attitudes. Arch Psychol 1932; 140:1–55. [Google Scholar]
- 12.Buntinx F. Chest pain: an evaluation of the initial diagnosis made by 25 Flemish practitioners. Fam Pract 1991; 8:121–124. [DOI] [PubMed] [Google Scholar]
- 13.Bruyninckx R, Van den Bruel A, Aertgeerts B, Van Casteren V, Buntinx F. Half of the patients with chest pain that are urgently referred are transported in unsafe conditions. Eur J Emerg Med 2008; 15:330–333. [DOI] [PubMed] [Google Scholar]
- 14.Wallbridge DR, Tweddel AC, Martin W, Cobbe SM. The potential impact of patient self-referral on mortality in acute myocardial infarction. Q J Med 1992; 85:901–909. [PubMed] [Google Scholar]
- 15.Gray D, Keating NA, Murdock J, Skene AM, Hampton JR. Impact of hospital thrombolysis policy on out-of-hospital response to suspected myocardial infarction. Lancet 1993; 341:654–657. [DOI] [PubMed] [Google Scholar]
- 16.Leslie WS, Urie A, Hooper J, Morrison C. Delay in calling for help during myocardial infarction: reasons for the delay and subsequent pattern of accessing care. Heart 2000; 84:137–141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pattenden J, Watt I, Lewin RJP, Stanford N. Decision making processes in people with symptoms of acute myocardial infarction: qualitative study. BMJ 2002; 324:1006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dracup K, Moser DK, Eisenberg M, Meischke H, Alonzo AA, Braslow A. Causes of delay in seeking treatment for heart attack symptoms. Soc Sci Med 1995; 40:379–392. [DOI] [PubMed] [Google Scholar]
- 19.Canto JG, Zalenski RJ, Ornato JP, Rogers WJ, Kiefe CI, Magid D, et al. Use of emergency medical services in acute myocardial infarction and subsequent quality of care: observations from the National Registry of Myocardial Infarction 2. Circulation 2002; 106:3018–3023. [DOI] [PubMed] [Google Scholar]
- 20.Lambrew CT, Bowlby LJ, Rogers WJ, Chandra NC, Weaver WD. Factors influencing the time to thrombolysis in acute myocardial infarction. Time to Thrombolysis Substudy of the National Registry of Myocardial Infarction-1. Arch Intern Med 1997; 157:2577–2582. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's website, www.euro-emergencymed.com.


