Abstract
Background:
Real-time elastography (RTE) and shear wave elastography (SWE) are noninvasive and easily available imaging techniques that measure the tissue strain, and it has been reported that the sensitivity and the specificity of elastography were better in differentiating between benign and malignant thyroid nodules than conventional technologies.
Methods:
Relevant articles were searched in multiple databases; the comparison of elasticity index (EI) was conducted with the Review Manager 5.0. Forest plots of the sensitivity and specificity and SROC curve of RTE and SWE were performed with STATA 10.0 software. In addition, sensitivity analysis and bias analysis of the studies were conducted to examine the quality of articles; and to estimate possible publication bias, funnel plot was used and the Egger test was conducted.
Results:
Finally 22 articles which eventually satisfied the inclusion criteria were included in this study. After eliminating the inefficient, benign and malignant nodules were 2106 and 613, respectively. The meta-analysis suggested that the difference of EI between benign and malignant nodules was statistically significant (SMD = 2.11, 95% CI [1.67, 2.55], P < .00001). The overall sensitivities of RTE and SWE were roughly comparable, whereas the difference of specificities between these 2 methods was statistically significant. In addition, statistically significant difference of AUC between RTE and SWE was observed between RTE and SWE (P < .01).
Conclusion:
The specificity of RTE was statistically higher than that of SWE; which suggests that compared with SWE, RTE may be more accurate on differentiating benign and malignant thyroid nodules.
Keywords: benign, malignant, real-time elastography (RTE), shear wave elastography (SWE), thyroid nodule
1. Introduction
Thyroid nodules are a common finding in the general population and the number has increased in recent years.[1] Many thyroid nodules in clinical diagnosis are detected incidentally with imaging studies, usually for other reasons. Most thyroid nodules diagnosed are asymptomatic and benign, whereas only about 5% are malignant nodules.[2,3] Diagnosing the benign or malignant of thyroid nodules is the foundation for its subsequent treatment.[4] As guidelines generally recommend, fine-needle aspiration biopsy (FNAB) is the best method to differentiate between benign and malignant thyroid nodules. But FNAB has some limitations, such as being invasive and time-intensive.[5,6] During the last decade, elastography, a novel imaging technique that is noninvasive and easily available, was added to the diagnostic list for the evaluation of thyroid nodules.[7] Elastography is a promising technology based on measuring the tissue strain, and because of the its easy assessment and efficient compressing against underlying anatomic structures, the thyroid gland would be well-positioned.[8]
Real-time elastography (RTE) is a noninvasive diagnostic technique that examines the stiffness and hardness of tissue. With the principle that the softer tissue is easily deformed than the harder tissue under external compression, the deformability of tissue was applied to differentiate malignant from benign lesions.[9,10] The technique of RTE was widely used in the detection of superficial tissues, including neck, prostate, breast, and thyroid, by testing the elasticity.[11] When pathological conditions occurred, the structure and elastic properties of soft tissue may be transformed. Then the stiffness of tissue would be increased and strain ratio of tissues in the region of interest (ROI) would be measured.[12] With the application of RTE, the thyroid gland is well positioned and easily accessed and efficiently compressed with the ultrasound probe.
Another novel, quantitative method is shear wave elastography (SWE), which was first administrated from acoustic radiation force by Nightingale et al.[13] SWE measures the shear wave velocity of the tissue by acoustic radiation force impulse and the velocity reflects the tissue hardness directly with Young modulus. With the image of shear wave propagation velocity through tissues, qualitative and quantitative assessments about the surrounding tissue are performed. The color scale is used to assess tissue stiffness, and each color represents a different level of tissue stiffness: blue represents soft tissues and red represents hard tissues.[14–16] Some studies[17,18] have reported that SWE would increase the specificity of assessment without loss of sensitivity, and the evaluations of thyroid nodules would not be hindered by autoimmune thyroiditis.
Although many studies thought that RTE and SWE seem to be the meaningful measures in differentiation between benign and malignant thyroid nodules, their real effects of diagnosis, including sensitivity and specificity, were controversial. The objective of this meta-analysis was to compare the EI between benign and malignant nodules detected by SWE and prospectively examine the diagnostic performance of RTE and SWE as measures in differentiating benign and malignant thyroid nodules using histopathological diagnosis as the reference standard.
2. Materials and methods
2.1. Search strategy
Comprehensive searches of relevant citations about detecting thyroid nodules using elastography were performed to examine the accuracy of differentiating benign and malignant nodules. The systematic review was undertaken with articles published from inception to July 2016, and all publication statuses, including published, unpublished, in press and in progress were included in this study. To assemble all of the relevant published citations, multiple electronic databases (PubMed, Springer, Embase, OVID, Cochrane Library and China Journal Full-text Database) were searched and no language restriction was set. To maximize the search sensitivity and specificity, the following keywords were used in our search work: “thyroid nodules,” “benign” OR “malignant” OR “cancer,” “elastography” OR “real-time elastography” OR “shear wave elastography” OR “RTE” OR “SWE.” MeSH terms and Boolean operator were selected for each database search. Two members of our team searched the literature and reviewed the titles and abstracts independently. The reference lists should also be reviewed to obtain the additional relevant studies that are not identified through the database searching.
2.2. Citation selection
The articles searched out were screened for the further selection. Another 2 authors independently selected the citations in this process, and screened the titles and abstracts of the articles identified previously. Subsequently, the full text of the studies that met the criteria were obtained and reviewed to check whether the study was likely to be relevant. Patients of all age groups were evaluated. The final selection of the target articles were determined by these 2 investigators together.
All the studies included in this study must meet the following inclusion criteria:
-
1.
a randomized trial controlled study;
-
2.
comparison of the EI between benign and malignant nodules detected by SWE;
-
3.
evaluation of RTE or SWE; and
-
4.
availability of full text.
Exclusion criteria were as follows:
-
1.
nonrandomized studies;
-
2.
studies on other detection technology; and
-
3.
studies lacking outcome measures or comparable results.
These 2 authors met and checked their selections for agreement after the primary selection. Disagreements were resolved by reaching a consensus through discussion and a third investigator was involved if necessary.
2.3. Data extraction
Studies that prospectively and simultaneously evaluated RTE and SWE as diagnostic technologies for thyroid nodules were included. Two reviewers independently read the full text of the studies, included and extracted the details from each study in a coding sheet in Microsoft Excel 2010. The data extracted consisted of the first author's name, year of publication, year of onset, age range of patients, sex distribution (male/female), diagnostic methods, sample size (malignant/benign), and outcome parameters. In this study, the parameters included elasticity index (EI) and accuracy of diagnosis. As a diagnostic method, we obtained the true positive (TP), true negative (TN), false positive (FP), and false negative (FN) of RTE and SWE diagnosis in each study, which were used to estimate the sensitivity and specificity.
2.4. Statistical analysis
We performed the meta-analyses with the Review Manager 5.0 (The Cochrane Collaboration, 2011) to estimate the difference of the EI between benign and malignant nodules. As a continuous outcome, standard mean difference (SMD) with 95% confidence intervals (CIs) of EI was calculated by the mean and standard deviation. Heterogeneity was assessed using Q statistics in this study. The value of I2 statistic reflects the levels of heterogeneity. If I2 is >50%, which means significant heterogeneity was present, a random-effect model was adopted. Otherwise a fixed-effect model was chosen.
As diagnostic tests, the overall sensitivity and specificity of RTE and SWE, as well as their corresponding 95% CIs were calculated on the basis of TP, TN, FP, and FN with STATA 10.0 software, and forest plots of the sensitivity and specificity and summary receiver operating characteristic (SROC) curve were performed.
In addition, sensitivity analysis and bias analysis of the studies were conducted to examine the quality of articles. To estimate possible publication bias, funnel plot was used and the Egger test was conducted. A P value <.05 was considered to be statistically significant.
3. Results
3.1. Search results
After the primary selection, 1800 titles and abstracts were initially searched out in these multiple electronic databases, and finally 22 articles[5,19–39] among them eventually satisfied all the inclusion criteria. The other 1778 articles were excluded for duplication, irrelevant studies, inappropriate data, review, without or inappropriate control group, other detection methods, or not a full-text. The flow diagram that reflects the search process and the reasons of exclusion was presented in Figure 1. Among these 22 articles, 12 were involved in the RTE, 9 were involved in the SWE, and 1 study both RTE and SWE. Eight of the SWE studies compared the EI between benign and malignant nodules.
Figure 1.
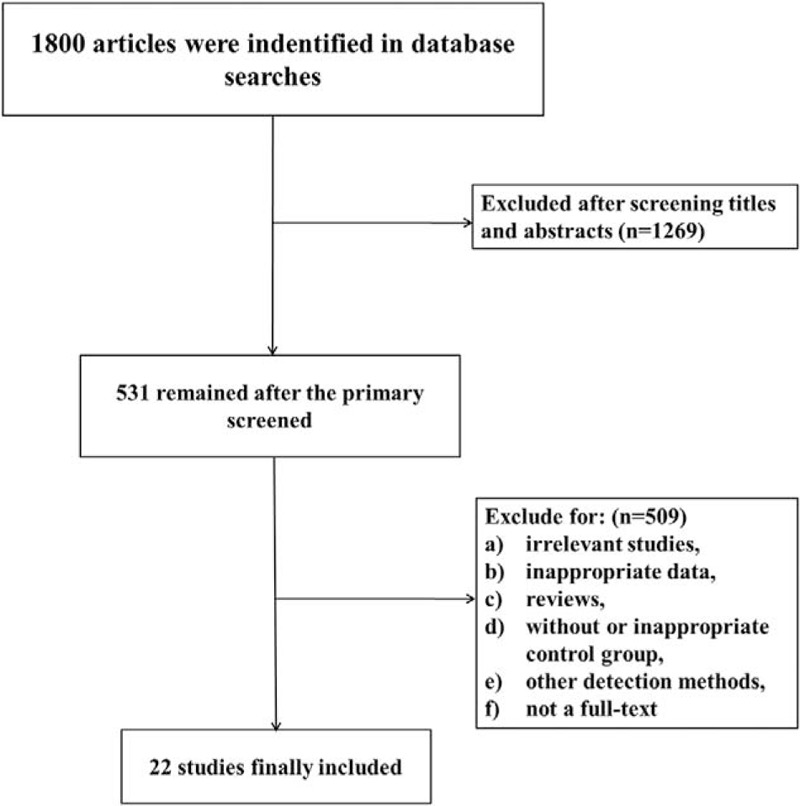
Flow diagram of the study identification and inclusion.
3.2. Characteristics of included studies
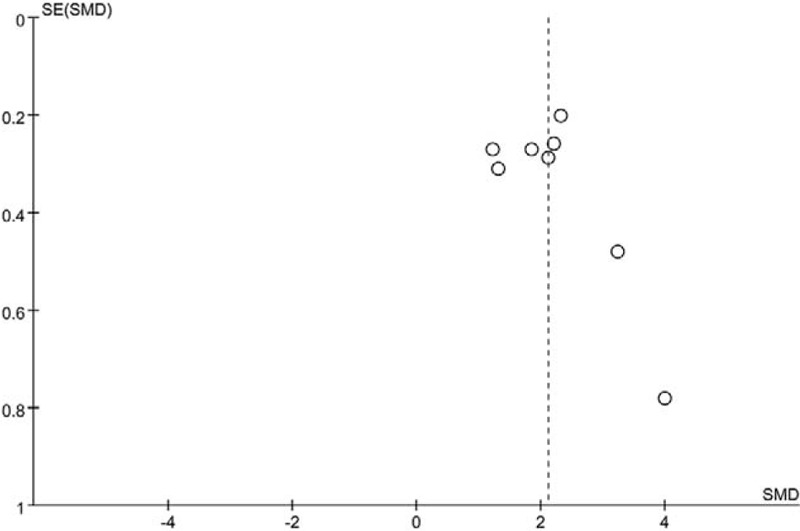
Detailed characteristics of the included studies were presented in Table 1, including the first author's name, year of publication, year of onset, age range of patients, sex distribution (male/female), diagnostic methods, sample size (malignant/benign), and outcome parameters. All these articles were published from 2007 to 2016. The sample size ranges from 26 to 707. In total, 2661 patients were included in these studies, and after eliminating the inefficient, benign and malignant nodules were 2063 and 598, respectively.
Table 1.
Detailed characteristics of the included studies.
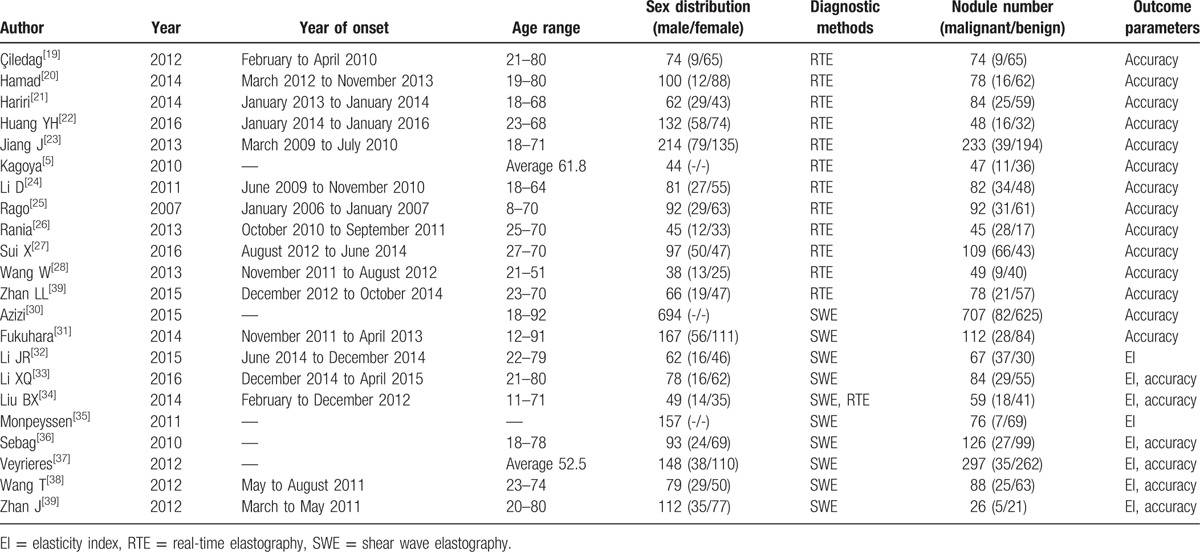
3.3. Meta-analysis about the EI
Eight articles included in this study are involved in the comparison of the EI between benign and malignant nodules detected by SWE. Figure 2 shows the forest plot for EI in different nodules. According to the forest plot, all the 8 studies showed that the EI of malignant nodules was much higher than that of benign nodules. And the overall meta-analysis suggested that the difference between benign and malignant nodules was statistically significant (SMD = 2.11, 95% CI [1.67, 2.55], P < .00001; P for heterogeneity < .0001, I2 = 77%).
Figure 2.
A forest plot for the EI between benign and malignant nodules detected by SWE. EI = elasticity index, SWE= shear wave elastography.
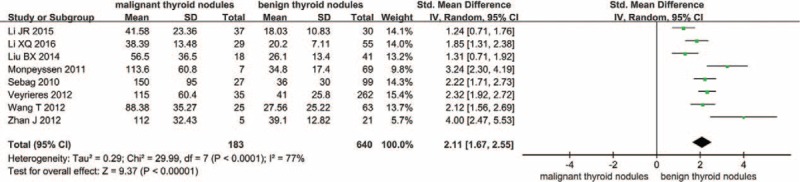
3.4. Bias analysis
Relatively high heterogeneity in the meta-analysis of the EI between benign and malignant nodules was observed (I2 = 77%). Figure 3 was the funnel plot for the studies about the EI, and the Egger test was also conducted. The result of Egger test suggested that no significant evidence of potential publication bias of meta-analysis about the EI between benign and malignant nodules was observed (t = 1.22, P = .267).
Figure 3.
A funnel plot for the studies about the EI between benign and malignant nodules. EI = elasticity index.
3.5. Meta-analyses of diagnostic tests
Forest plots for the combined sensitivity and specificity of diagnosing malignant from benign nodules with RTE and SWE are showed in Figures 4 and 5, respectively. The results showed that the sensitivity and specificity of RTE were 0.84 (95% CI [0.76, 0.90]) and 0.90 (95% CI [0.85, 0.94]), and those of SWE were 0.79 (95% CI [0.73, 0.84]) and 0.87 (95% CI [0.79, 0.92]). The overall sensitivities of these 2 methods were roughly comparable (P > .05), whereas the difference of specificity between RTE and SWE was statistically significant (P < .05)
Figure 4.
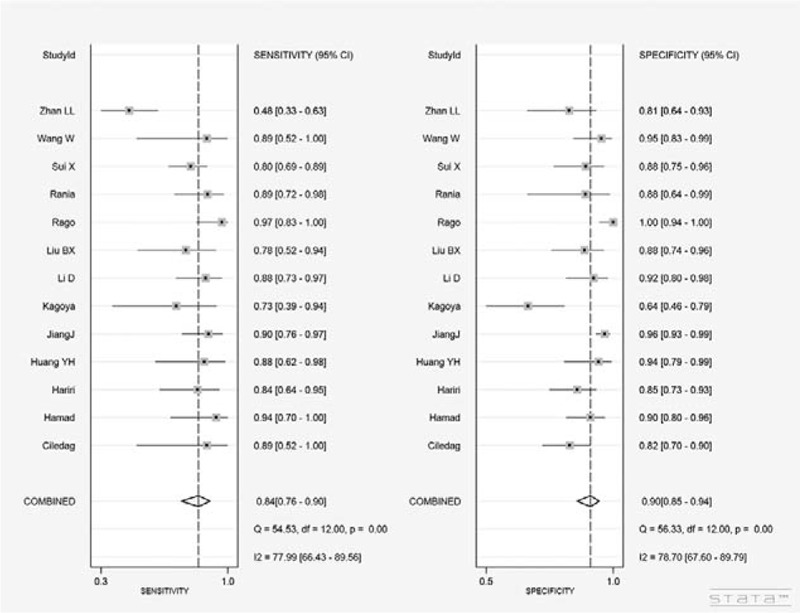
Forest plots for the combined sensitivity and specificity of RTE. RTE = real-time elastography.
Figure 5.
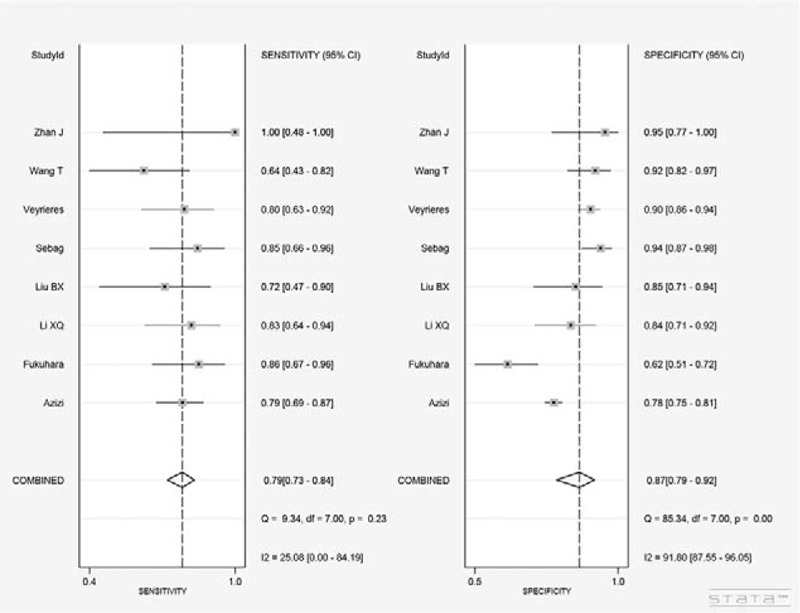
Forest plots for the combined sensitivity and specificity of SWE. SWE= shear wave elastography.
The SROC curves that evaluated these 2 promising technologies for differentiating malignant nodules from benign nodules are presented in Figures 6 and 7, respectively. As shown in these figures, the area under the SROC curve (AUC) was 0.94 (95% CI [0.91, 0.96]) for RTE, and 0.83 (95% CI [0.80, 0.86]) for SWE. Statistically significant difference of AUC was observed between RTE and SWE (P < .01).
Figure 6.
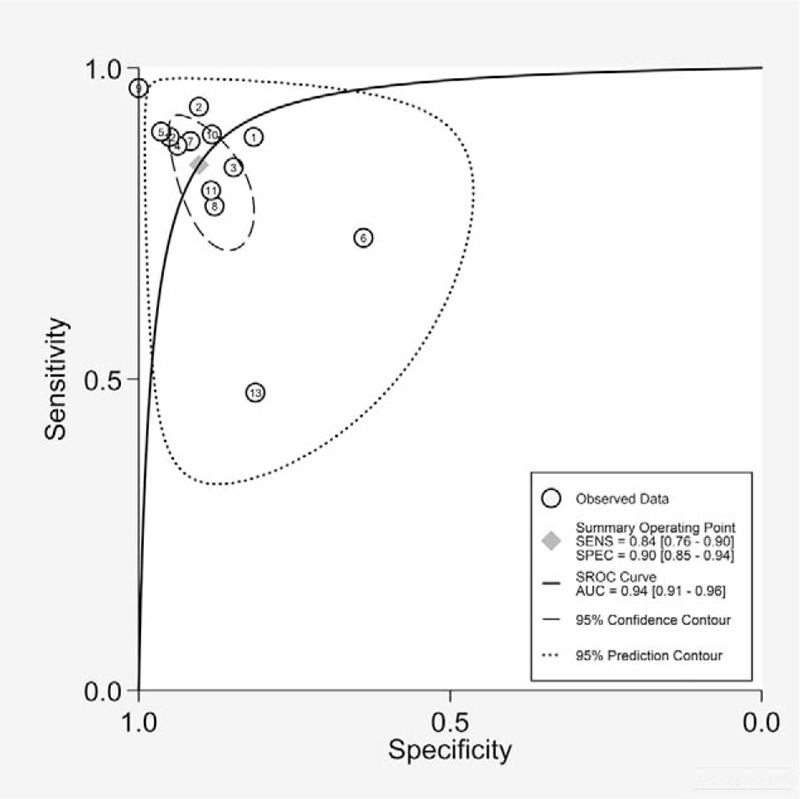
Summary receiver operating characteristic (SROC) curves of RTE. RTE = real-time elastography.
Figure 7.
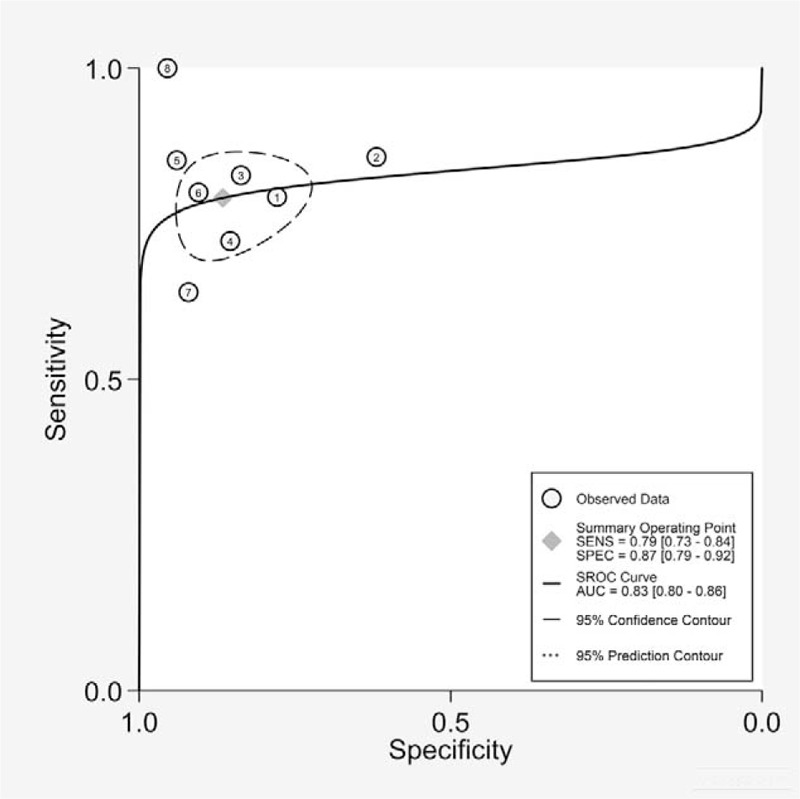
Summary receiver operating characteristic (SROC) curves of SWE. SWE= shear wave elastography.
4. Discussion
Several diagnostic approaches have been proposed for detection of thyroid nodules, including FNAB and ultrasound (US) examination. FNAB suffers the limitations of being invasive and time-intensive as it requires sending and getting the samples evaluated by the pathologist.[6] Ultrasound is a widely accepted diagnostic method of detecting thyroid nodules, and about 41% thyroid nodules are found by ultrasound.[40] But previous studies have found that the assessment of thyroid nodules by US was extreme different.[41] It has been reported that the diagnosis of US lacks sensitivity and is unable to sufficiently differentiate between thyroid follicular carcinoma and follicular adenoma.[6,42] Another problem with using US as diagnosis method is that the morphological changes of malignant nodules <1 cm in diameter are usually lacking.[43]
Currently, elastography has been introduced to augment the diagnostic accuracy of ultrasound.[44] Several studies have reported for better accuracy in differentiating between benign and malignant thyroid nodules with RTE,[45–47] which could directly reveal the physical properties of tissues using conventional US probes. Generally, the stiffness of malignant nodules is increased, and that of benign nodules is decreased. The different color modes of the elastography represent different tissue stiffness, and with these added information, benign and malignant lesions would be differentiated.[46,48] Compared with US, the utility of elastography was independent from the size of thyroid nodules.
The power of RTE to examine malignant thyroid nodules has been reported in many studies,[49,50] and these articles generally described RTE to be relatively more accurate. In our study, the combined sensitivity and specificity of RTE were 0.84 (95% CI [0.76, 0.90]) and 0.90 (95% CI [0.85, 0.94]), respectively, which were much higher than those of conventional US.[23,29,30] Because RTE is an operator-dependent technique, measurement bias resulting from different radiologists definitely exists in clinical practice. Besides, the evaluation of RTE is limited to the ROI on only 1 side of the neck. Compared with RTE, SWE is a more independent technique and quantitative analysis that avoids the limitation of RTE, and this promising technology is expected to provide more information.[51,52] The meta-analysis provides a comparison of EI between benign and malignant nodules. The EI of malignant nodules is much higher than that of benign nodules, which means that SWE could be a great method to detect thyroid nodules. Based on the results, we observed that the difference of sensitivity was not significant, while the combined specificity of RTE was much higher than that of SWE. Besides, the AUC of RTE was also much larger than that of SWE. These results suggested that compared with SWE, RTE was a demonstrably superior method on accuracy. While considering the technical advantages of SWE, the diagnostic methods should be selected with comprehensive balance.
Although the meta-analyses suggested that RTE and SWE could be diagnostic approach to diagnose benign and malignant thyroid nodules, as we expected, there are some potential biases and limitations in our study. One of the major limiting factors is the selection bias.[7] Some studies that were included in our meta-analysis enrolled the patients who have already been suspected with malignant nodules for cytological results or large nodular size, and this could amplify the predictive value of elastography. In the meta-analysis of comparison of the EI between benign and malignant nodules, we selected a random-effect model for a relatively high heterogeneity (I2 > 50%). The reasons for high heterogeneity were complex and we believe that different test technologies and small sample size may be 2 of them. Because elastography is an operator-dependent technique, measurement bias resulting from different radiologists definitely exists in clinical practice. Besides, the poor quality of some studies indicates that further well-designed and prospective studies are needed to verify our results.
5. Conclusion
The present study evaluated the clinical value of RTE and SWE in differentiating between benign and malignant thyroid nodules. Based on the results reported in the present meta-analyses, both RTE and SWE seem to have a great diagnostic potential to differentiate benign and malignant solitary thyroid nodules, and RTE seems to be more specific. Thus we support the recommendation that RTE and SWE could be used in clinical diagnosis as a noninvasive diagnostic approach, which may lead to a great improvement in accurate diagnosis, and for benign thyroid nodules, the number of unnecessary surgical procedures could be reduced.
Footnotes
Abbreviations: CIs = confidence intervals, EI = elasticity index, FN = false negative, FNAB = fine-needle aspiration biopsy, FP = false positive, ROI = the region of interest, RTE = real-time elastography, SMD = standard mean difference, SWE = shear wave elastography, TN = true negative, TP = true positive.
This study was funded by Project of High-level Personnel in the Beijing Health System (no. 2014–3–009) And Basic-Clinical Cooperation Program from Capital Medical University (no. 15JL10).
The authors report no conflicts of interest.
References
- [1].Knox MA. Thyroid nodules. Am Fam Physician 2013;88:193–6. [PubMed] [Google Scholar]
- [2].Lim DJ, Luo S, Kim MH, et al. Interobserver agreement and intraobserver reproducibility in thyroid ultrasound elastography. Am J Roenthenol 2012;198:896–901. [DOI] [PubMed] [Google Scholar]
- [3].Hegedus L. Clinical practice. The thyroid nodule. N Engl J Med 2004;351:1764–71. [DOI] [PubMed] [Google Scholar]
- [4].Hegedus L, Bonnema SJ, Bennedbaek FN. Management of simple nodular goiter: current status and future perspectives. Endocr Rev 2003;24:102–32. [DOI] [PubMed] [Google Scholar]
- [5].Kagoya R, Monobe H, Tojima H. Utility of elastography for differential diagnosis of benign and malignant thyroid nodules. Otolaryngol Head Neck Surg 2010;143:230–4. [DOI] [PubMed] [Google Scholar]
- [6].Vorlander C, Wolff J, Saalabian S, et al. Real-time ultrasound elastography—a noninvasive diagnostic procedure for evaluating dominant thyroid nodules. Langenbecks Arch Surg 2010;395:865–71. [DOI] [PubMed] [Google Scholar]
- [7].Hegedus L. Can elastography stretch our understanding of thyroid histomorphology? J Clin Endocrinol Metab 2010;95:5213–5. [DOI] [PubMed] [Google Scholar]
- [8].Kim JY, Lee CH, Kim SY, et al. Radiologic and pathologic findings of nonpalpable thyroid carcinomas detected by ultrasonography in a medical screening center. J Ultrasound Med 2008;27:215–23. [DOI] [PubMed] [Google Scholar]
- [9].Lyshchik A, Higashi T, Asato R, et al. Cervical lymph node metastases: diagnosis at sonoelastography—initial experience. Radiology 2007;243:258–67. [DOI] [PubMed] [Google Scholar]
- [10].Thomas A, Fischer T, Frey H, et al. Real-time elastography—an advanced method of ultrasound: first results in 108 patients with breast lesions. Ultrasound Obstet Gynecol 2006;28:335–40. [DOI] [PubMed] [Google Scholar]
- [11].Ophir J, Alam SK, Garra B, et al. Elastography: ultrasonic estimation and imaging of the elastic properties of tissues. Proc Inst Mech Eng H 1999;213:203–33. [DOI] [PubMed] [Google Scholar]
- [12].Reading CC, Charboneau JW, Hay ID, et al. Sonography of thyroid nodules: a “classic pattern” diagnostic approach. Ultrasound Q 2005;21:157–65. [DOI] [PubMed] [Google Scholar]
- [13].Nightingale K, McAleavey S, Trahey G. Shear-wave generation using acoustic radiation force: in vivo and ex vivo results. Ultrasound Med Biol 2003;29:1715–23. [DOI] [PubMed] [Google Scholar]
- [14].Asteria C, Giovanardi A, Pizzocaro A, et al. US-elastography in the differential diagnosis of benign and malignant thyroid nodules. Thyroid 2008;18:523–31. [DOI] [PubMed] [Google Scholar]
- [15].Trimboli P, Guglielmi R, Monti S, et al. Ultrasound sensitivity for thyroid malignancy is increased by real-time elastography: a prospective multicenter study. J Clin Endocrinol Metab 2012;97:4524–30. [DOI] [PubMed] [Google Scholar]
- [16].Azizi G, Keller J, Lewis M, et al. Performance of elastography for the evaluation of thyroid nodules: a prospective study. Thyroid 2013;23:734–40. [DOI] [PubMed] [Google Scholar]
- [17].Cosgrove DO, Berg WA, Doré CJ. Shear wave elastography for breast masses is highly reproducible. Eur Radiol 2012;22:1023–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Berg WA, Cosgrove DO, Dore CJ, et al. Shear-wave elastography improves the specificity of breast US: the BE1 multinational study of 939 masses. Radiology 2012;262:435–49. [DOI] [PubMed] [Google Scholar]
- [19].Çiledag N, Arda K, Aribas BK, et al. The utility of ultrasound elastography and MicroPure imaging in the differentiation of benign and malignant thyroid nodules. AJR Am J Roentgenol 2012;198:W244–9. [DOI] [PubMed] [Google Scholar]
- [20].Eltyib HEH, Awad IA, Elsayed NM, et al. Real time ultrasound elastography for the differentiation of benign and malignant thyroid nodules. Open J Med Imaging 2014;4:38–47. [Google Scholar]
- [21].El-Hariri MA, Taha Ali TF, Tawab MA, et al. The clinical value of ultrasound elastography in predicting malignant thyroid nodules. Egyptian J Radiol Nucl Med 2014;45:353–9. [Google Scholar]
- [22].Hang YH, Chen WJ, Liang QS, et al. Diagnostic value of conventional ultrasound combined with elastography in thyroid microcarcinoma. China Med Herald 2016;13:112–5. [Google Scholar]
- [23].Jiang J, Li D, Zhou Q, et al. Comparative analysis of ultrasonic elastography and conventional ultrasound for thyroid nodules. J Clin Ultrasound Med 2013;15:186–8. [Google Scholar]
- [24].Li D, Liu N, Bai YL, et al. Value of contrast enhanced ultrasound and ultrasonic elastography in differential diagnosis of benign and malignant thyroid nodules. J Clin Ultrasound Med 2011;13:516–20. [Google Scholar]
- [25].Rago T, Santini F, Scutari M, et al. Elastography: new developments in ultrasound for predicting malignancy in thyroid nodules. J Clin Endocrinol Metab 2007;92:2917–22. [DOI] [PubMed] [Google Scholar]
- [26].Mohamed RE, Abodewan KA. Diagnostic utility of real-time ultrasound elastography for prediction of malignancy in solid thyroid nodules. Egyptian J Radiol Nucl Med 2013;44:33–43. [Google Scholar]
- [27].Sui X, Liu HJ, Jia HL, et al. Contrast-enhanced ultrasound and real-time elastography in the differential diagnosis of malignant and benign thyroid nodules. Exp Ther Med 2016;12:783–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Wang W, Jin ZJ, Tang B, et al. Value of ultrasonic elasticity imaging and conventional ultrasonography to the diagnosis of benign and malignant thyroid nodules. J Chin Pract Diagn Ther 2013;27:467–9. [Google Scholar]
- [29].Zhan LL, Liu ST. Combination of conventional ultrasound and elastography in the diagnosis of small thyroid nodules. Chin J Oper Proc Gen Surg 2015;9:56–8. [Google Scholar]
- [30].Azizi G, Keller JM, Mayo ML, et al. Thyroid nodules and shear wave elastography: a new tool in thyroid cancer detection. Ultrasound Med Biol 2015;41:2855–65. [DOI] [PubMed] [Google Scholar]
- [31].Fukuhara T, Matsuda E, Fujiwara K, et al. Phantom experiment and clinical utility of quantitative shear wave elastography for differentiating thyroid nodules. Endocr J 2014;61:615–21. [DOI] [PubMed] [Google Scholar]
- [32].Li JR, Luo YK, Li YM, et al. Application of real-time shear wave elastography in diagnosis of thyroid micro carcinoma. Acad J Chin PLA Med Sch 2015;36:892–5. [Google Scholar]
- [33].Li XQ, Chen HN, Yang Z, et al. Differential diagnostic value of benign and malignant thyroid nodules by real-time shear wave elastography. J Clin Ultrasound Med 2016;18:233–6. [Google Scholar]
- [34].Liu BX, Liang JY, Xie XY, et al. Preliminary comparative study of shear wave elastography versus quasi-static elastography on evaluation of thyroid nodules. Chin J Med Ultrasound 2014;11:925–31. [Google Scholar]
- [35].Monpeyssen H, Correas JM, Tramalloni J, et al. Correlations between shear wave elastography of thyroid nodules and cytological data: study about 157 patients. Ultrasound Med Biol 2011;37:S8–9. [Google Scholar]
- [36].Sebag F, Vaillant-Lombard J, Berbis J, et al. Shear wave elastography: a new ultrasound imaging mode for the differential diagnosis of benign and malignant thyroid nodules. J Clin Endocrinol Metab 2010;95:5281–8. [DOI] [PubMed] [Google Scholar]
- [37].Veyrieres JB, Albarel F, Lombard JV, et al. A threshold value in shear wave elastography to rule out malignant thyroid nodules: A reality? Eur J Radiol 2012;81:3965–72. [DOI] [PubMed] [Google Scholar]
- [38].Wang T, Wang XM, Zhang YX, et al. Quantitative assessment of real-time shear wave elastography imaging in differentiating benign and malignant thyroid nodules. Chin J Med Imaging 2012;9:684–7. [Google Scholar]
- [39].Zhan J, Chen Y, Chai QL, et al. Primary application of shear wave elastography in quantitative differential diagnosis of benign and malignant thyroid nodules. Chin J Ultrasound Med 2012;28:274–7. [Google Scholar]
- [40].Tamsel S, Demirpolat G, Erdogan M, et al. Power Doppler US patterns of vascularity and spectral Doppler US parameters in predicting malignancy in thyroid nodules. Clin Radiol 2007;62:245–51. [DOI] [PubMed] [Google Scholar]
- [41].Algin O, Algin E, Gokalp G, et al. Role of duplex power Doppler ultrasound in differentiation between malignant and benign thyroid nodules. Korean J Radiol 2010;11:594–602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Zhou Q, Xu YB, Jiang J, et al. Differential diagnostic value of contrast-enhanced ultrasound in calcified thyroid nodules. Zhong hua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi 2013;48:726–9. [PubMed] [Google Scholar]
- [43].Rago T, Vitti P, Chiovato L, et al. Role of conventional ultrasonography and color flow-Doppler sonography in predicting malignancy in “cold” thyroid nodules. Eur J Endocrinol 1998;138:41–6. [DOI] [PubMed] [Google Scholar]
- [44].Gao L, Parker KJ, Lerner RM, et al. Imaging of the elastic properties of tissue—a review. Ultrasound Med Biol 1996;22:959–77. [DOI] [PubMed] [Google Scholar]
- [45].Friedrich-Rust M, Sperber A, Holzer K, et al. Real-time elastography and contrast-enhanced ultrasound for the assessment of thyroid nodules. Exp Clin Endocrinol Diabetes 2010;118:602–9. [DOI] [PubMed] [Google Scholar]
- [46].Wang Y, Dan HJ, Dan HY, et al. Differential diagnosis of small single solid thyroid nodules using real-time ultrasound elastography. J Int Med Res 2010;38:466–72. [DOI] [PubMed] [Google Scholar]
- [47].Moon WJ, Jung SL, Lee JH, et al. Benign and malignant thyroid nodules: US differentiation multicenter retrospective study. Radiology 2008;247:762–70. [DOI] [PubMed] [Google Scholar]
- [48].Tanaka K, Fukunari N, Igarashi Y, et al. Evaluation of thyroid malignancy using real-time tissue elastography. Eur Radiol 2006;16:547. [Google Scholar]
- [49].El Hag IA, Kollur SM. Benign follicular thyroid lesions versus follicular variant of papillary carcinoma: differentiation by architectural pattern. Cytopathology 2004;15:200–5. [DOI] [PubMed] [Google Scholar]
- [50].Das DK, Sheikh ZA, George SS, et al. Papillary thyroid carcinoma: evidence for intracytoplasmic formation of precursor substance for calcification and its release from well-preserved neoplastic cells. Diagn Cytopathol 2008;36:809–12. [DOI] [PubMed] [Google Scholar]
- [51].Lyshchik A, Higashi T, Asato R, et al. Thyroid gland tumor diagnosis at US elastography. Radiology 2005;237:202–11. [DOI] [PubMed] [Google Scholar]
- [52].Bojunga J, Dauth N, Berner C, et al. Acoustic radiation force impulse imaging for differentiation of thyroid nodules. PLoS One 2012;7:e42735. [DOI] [PMC free article] [PubMed] [Google Scholar]


